Key message
Granulomatosis with polyangiitis (GPA) is a potentially life‐threatening disease that affects all ages. As the disease may be rapidly progressive, the undelayed recognition of its inflammatory activity is critical. This is especially important in central airway involvement, which contributes to morbidity and mortality.
Keywords: Airway, bronchoscopy, granulomatosis with polyangiitis, inflammation, vasculitis
We present the case of a 17‐year‐old boy with granulomatosis with polyangiitis (GPA) with central airway involvement.

Clinical Image
A 17‐year‐old boy with granulomatosis with polyangiitis (GPA) was hospitalized with severe hypoxaemic respiratory failure requiring intubation, invasive ventilation, and extracorporeal lung support. GPA had been diagnosed 15 months earlier presenting with recurrent rhinosinusitis and the course had been stable under treatment with low‐dose prednisolone and methotrexate to this point. Bronchoscopy now visualized acute inflammation affecting the tracheobronchial mucosa and underlying wall (Fig. 1). Severe acute inflammatory activity in GPA was diagnosed. Therapy including high‐dose prednisolone, cyclophosphamide, rituximab, immunoglobulins, and plasmapheresis was effective in controlling airway inflammation; however, extensive damage to the airway remained (Fig. 2).
Figure 1.
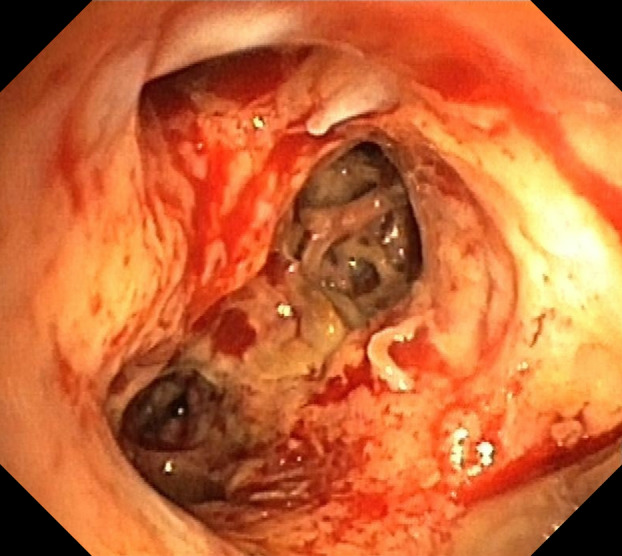
Bronchoscopic image of severe acute destructive inflammation of the airways of the right lower lobe in granulomatosis with polyangiitis depicting oedema, erythema, and hypervascularity of the mucosa as well as exposure and damage of the underlying bronchial wall and cartilage.
Figure 2.
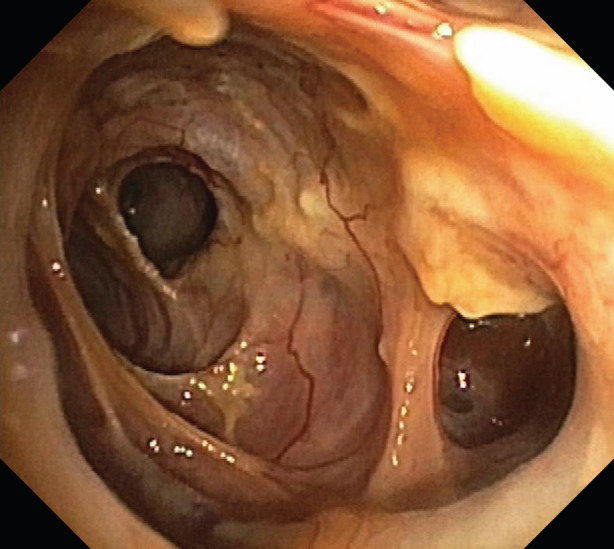
Bronchoscopic image of the remaining structural damage to the airways of the basal segments of the right lower lobe after five weeks of treatment for acute inflammation depicting cavernous neoairways following the destruction of the original bronchial wall and cartilage.
Involvement of lung parenchyma is a well‐recognized pulmonary manifestation of GPA. Involvement of the central airway [1, 2] is however less recognized, but contributes to morbidity and mortality and the correct interpretation of the bronchoscopic image is key to its detection. The bronchoscopic image not only assists in diagnosis, but also in follow‐up as the inner surface may still sensitively or exclusively exhibit acute inflammation while there may be no other pulmonary or extrapulmonary manifestations of acute vasculitis detectable by clinical, radiological, or laboratory tests. It is therefore critical to be aware of airway manifestations in GPA including light to moderate acute inflammation with mucosal oedema, erythema and granularity, severe acute destructive inflammation with deep damage to the airway wall as exhibited unusually extensive in this case, as well as post‐inflammatory scarring and stenosis.
Disclosure Statement
Appropriate written informed consent was obtained for publication of this case report and accompanying images.
Oqueka, T , Klose, H , Iking‐Konert, C , Schnoor, U , Kluge, S , Simon, M . (2021) Granulomatosis with polyangiitis: mind the airway. Respirology Case Reports, 9(1), e00702 10.1002/rcr2.702
Associate Editor: Yet Hong Khor
References
- 1. Polychronopoulos VS, Prakash UB, Golbin JM, et al. 2007. Airway involvement in Wegener's granulomatosis. Rheum. Dis. Clin. North Am. 33:755–775. [DOI] [PubMed] [Google Scholar]
- 2. Daum TE, Specks U, Colby TV, et al. 1995. Tracheobronchial involvement in Wegener's granulomatosis. Am. J. Respir. Crit. Care Med. 151:522–526. [DOI] [PubMed] [Google Scholar]


