Abstract
Purpose
Low birth weight (BW) individuals have an increased risk for myopic refractive error. However, it is unclear which ocular geometric alterations lead to an increase in myopic refractive error. This study aims to evaluate the impact of ocular biometry in interaction with BW on refractive error.
Methods
Participants of the prospective, observational, population-based Gutenberg Health Study (GHS) with self-reported BW aged 40–80 years and objective refraction and optical biometry were included. Linear regression analyses were conducted to evaluate associations between spherical equivalent with corneal power, anterior chamber depth, lens thickness and axial length and its interaction with BW adjusted for age and sex. Low BW was defined as BW<2500 g and normal BW between 2500−4000 g.
Results
Overall, 5123 participants were included. Linear regression showed an interaction of axial length (B = 0.009/100 g, p = 0.002) with BW on spherical equivalent while corneal power, anterior chamber depth and lens thickness revealed no interaction with BW on refractive error. Furthermore, linear regression analysis revealed, that axial length explains 58% of variance of spherical equivalent in low BW subjects, and 54% in normal BW subjects. In contrast, corneal power explained 1% of variance of spherical equivalent in both groups.
Conclusions
Our results indicate that axial length variation explains the majority of variance in refractive error, while steeper corneal shape has no conclusive effects on refractive error. Low BW is not linked to effects of steeper corneal shape on myopic refractive error, while the effect of axial length on myopia is fractionally enlarged in those subjects.
Keywords: Axial length, Birth weight, Corneal curvature, Epidemiology, Myopia, Refraction
Introduction
Low birth weight is often associated with prenatal malnutrition and preterm birth. In former preterm infants an increased risk for the development of myopia in childhood was observed independently of postnatal occurrence of retinopathy of prematurity (ROP).1, 2, 3, 4, 5, 6, 7 Authors have described myopia that develops in people with a history of prematurity as having different ocular features like a steeper corneal curvature, smaller anterior chamber depth and thicker lens accompanied by a smaller axial length in relation to the dioptric value8 with an earlier onset of myopia compared to those born full term.9
As origin for these morphological changes an arrested anterior eye segment development is assumed and probably caused by the differences between the higher intrauterine and the lower extrauterine temperature after preterm birth.10 These authors measured that preterm newborns suffer a thermal deficit of around 1–2 degree of the corneal surface which is never caught up in postnatal development leading to a less flattening of corneal geometry resulting in a steeper corneal shape contributing to myopia. This hypothesis was supported by animal studies where thermal gradients of the eye surface were a factor contributing to myopia.11
Retinopathy of prematurity as complication of preterm birth and its treatment were detected to be other important factors for myopia development. Various reports could demonstrate that particularly advanced stages and treatment with laser or cryotherapy of ROP are important factors contributing to myopia in these children.3, 4, 12, 13 Furthermore, ROP is accompanied by characteristic biometric alterations contributing to an altered ocular and refractive error development which has also to be considered as origin for myopic refractive changes in former preterm individuals. Anatomic sequelae for ROP are particularly a steeper cornea, a shorter axial length and a thicker and more power full lens.14, 15, 16
Several studies describe the association of low birth weight and preterm birth with myopic refractive error in childhood.1, 2, 3, 4, 5, 6 However, no population-based data exist investigating the long-term effects in middle and late adulthood on the association of ocular biometry and refractive error. As preterm infants have usually a low birth weight, this parameter may be used as a surrogate to analyze this association. We recently described that low birth weight is associated with increased myopic refractive error17 and altered ocular biometry such as a steeper corneal geometry and a smaller axial length in adults aged 40–80 years.18
However, it is unclear which ocular geometric alterations lead to an increase in myopic refractive error in these adults. Therefore, we now move one step further and analyze whether refractive error in low birth weight subjects is due to changes of axial length or of biometric alterations like steeper anterior segment. We will explore via linear regression analyses associations between spherical equivalent with corneal power, anterior chamber depth, lens thickness and axial length and its interaction with BW. Our hypothesis is that myopic refractive error in low birth weight adults is linked to alterations of the steeper cornea rather than to axial length.
Methods
Study population
The population-based GHS is an observational, single-center cohort study from the Mainz Bingen region in Germany (Rhineland-Palatinate).19 The population sample includes 15,010 persons aged between 35 and 74 years at baseline examination. Participants were randomly chosen from the database of the local governmental registry in which every inhabitant of the Mainz/Mainz-Bingen region is registered. The sample was stratified for sex, decade of age and residency (Mainz/Mainz-Bingen) containing equal proportions. Our present analysis contains data of the participants of the 5-year follow-up examination which was conducted between 2012 and 2017 in which every participant underwent a detailed ophthalmic examination as reported earlier.18
Written informed consent was obtained from all study participants and the GHS complies with Good Clinical Practice (GCP), Good Epidemiological Practice (GEP), and the ethical principles of the Declaration of Helsinki. The study protocol and study documents were approved by the local ethics committee of the Medical Chamber of Rhineland-Palatinate, Germany (reference no. 837.020.07).
Birth weight
At study invitation every participant was requested to look up personal birth documents or family albums for documented birth weight information. Low birth weight was defined as < 2500 g, normal birth weight as 2500 g–4000 g and high birth weight as > 4000 g. Furthermore, individuals with self-reported birth weight < 1000 g and > 6000 g were excluded from our analysis, because this data was suspected to be unreliable as reported earlier.17, 18, 20, 21 Furthermore, we excluded pseudophakic eyes as refractive error after cataract surgery may be different from preoperative refractive status.
Ophthalmological examination
A precise description of the ophthalmological examinations of the GHS was reported previously.22 In short, objective refraction and consecutive distant-corrected visual acuity were examined in both eyes (Humphrey Automated Refractor / Keratometer (HARK) 599; Carl Zeiss AG, Jena, Germany). Visual acuity was assessed with the built-in Snellen charts, ranging from 20/400 to 20/10 (decimal 0.05–2.0). Calculation of the spherical equivalent was carried out as the spherical correction value plus half the cylindrical power.22 As reported earlier,18 ocular biometry was conducted using the LenStar 900 (Haag Streit, Köniz, Switzerland). For these measurements, every participant was guided to fixate on the center of the LenStar´s internal fixation target, and directional arrows of the machine supported the study personnel to get an optimal focus. This process was performed to achieve high measurement correctness and to reduce and avoid measurement errors. Overall, the LenStar device conducts three single measurements per eye and then calculates the average value. The following parameters were part of the LenStar measurement: corneal radius, corneal power, white-to-white distance as a parameter for corneal diameter (measurement of the horizontal diameter of a best-fitted circle to the outer border of the iris), central corneal thickness, anterior chamber depth, lens thickness and axial length, and axial length-to-corneal power-ratio (ACPR) was computed. Every parameter was controlled for outliers. We validated these measurements against Scheimpflug images recorded with the Oculus Pentacam HR (Oculus, Wetzlar, Germany) and to anterior segment photographs.
Statistical analysis
An item non-responder analysis was carried out and study participants with and without self-reported birth weight were compared with respect to general characteristics and ocular geometry. Validation of self-reported birth weight of our cohort was previously reported and compared to data of the German Federal Statistical Office.17, 23 Data of both eyes were included into linear regression models. Furthermore, the distribution of birth weight data was compared to the medical literature.17 The relationship between refractive error and corneal power, axial length and axial length-to-corneal power-ratio was analyzed for the total study sample in scatter plots. Descriptive statistics were calculated for all parameters and absolute and relative frequencies were computed for dichotomous parameters. Mean and standard deviation were calculated for approximately normally distributed data, and the median and interquartile range were calculated for the remaining variables. Linear regression analyses with generalized estimating equations to account for the inter-eye correlation in one individual were conducted to evaluate associations of spherical equivalent and corneal power, anterior chamber depth, lens thickness and axial length and, in addition, effect modification of these parameters with BW adjusted for age, sex and birth weight. A sensitivity analysis was carried out including only myopic (≤ -1.0D) subjects in these analyses. In another sensitivity analyses these associations were calculated separately for low and normal birth weight subjects. Data were analyzed with R version 3.5.1 (R Core Team (2018). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/).
Results
Participant characteristics
Within the five-year follow-up examination of the GHS, 12,423 participants were examined, including 5123 participants, who were phakic, reported birth weight and had successful refractive and biometric measurements. Of these participants, 263 reported a birth weight below 2500 g (group 1) and 4232 reported a normal birth weight between 2500 g and 4000 g (group 2) and 628 a birth weight above 4000 g. Baseline characteristics are presented in Table 1.
Table 1.
Characteristics of the analysis sample. GHS participants with refractive and biometric measurements and self-reported birth weight data (n = 5123).
| Variable | All (5123) | Men (2449) | Women (2674) |
|---|---|---|---|
| Sex (Women) [% (n)] | 52.2% (2674) | 0% (0) | 100.0% (2674) |
| Age [y] | 55.1 ± 9.7 | 55.3 ± 9.8 | 54.9 ± 9.7 |
| SES index | 13.90 ± 4.23 | 14.52 ± 4.23 | 13.33 ± 4.15 |
| Self-reported eye diseases: | |||
| Glaucoma (yes) [% (n)] | 2.7% (137) | 2.6% (64) | 2.7% (73) |
| AMD (yes) [% (n)] | 1.1% (55) | 0.8% (20) | 1.3% (35) |
| Severe eye injury (yes) [% (n)] | 5.0% (258) | 3.6% (89) | 6.3% (169) |
| Cataract (self-reported) (yes) [% (n)] | 5.0% (258) | 3.6% (89) | 6.3% (169) |
| Sphere and visual acuity | |||
| Sphere (dpt) [Median(Q1/Q3] | 0 (-1.250/0.875) | 0 (-1.250/0.875) | 0 (-1.250/1.000) |
| Astigmatism (dpt) [Median(Q1/Q3] | −0.375 (-0.750/-0.125) | −0.458 (-0.750/-0.250) | −0.375 (-0.750/-0.125) |
| LogMAR [Median(Q1/Q3] | 0.046 (0/0.125) | 0.046 (0/0.097) | 0.046 (0/0.155) |
| Myopia (-3 dpt) (yes) [% (n)] | 12.1% (619) | 11.8% (289) | 12.4% (330) |
| Myopia (-6 dpt) (yes) [% (n)] | 2.8% (143) | 2.5% (62) | 3.0% (81) |
| Hyperopia (3 dpt) (yes) [% (n)] | 2.5% (129) | 2.5% (60) | 2.6% (69) |
| Hyperopia (6 dpt) (yes) [% (n)] | 0.3% (14) | 0.4% (9) | 0.2% (5) |
| Birth weight: | |||
| Birth weight [g] ± SD | 3412 ± 635 | 3538 ± 642 | 3295 ± 606 |
| Lenstar: | |||
| Astigmatism [dpt] (dpt) [Median(Q1/Q3] | 0.765 (0.480/1.140) | 0.700 (0.445/1.055) | 0.825 (0.520/1.210) |
| Corneal radius [mm] | 7.77 ± 0.27 | 7.83 ± 0.27 | 7.71 ± 0.26 |
| White to white distance [mm] | 12.2 ± 0.4 | 12.3 ± 0.4 | 12.2 ± 0.4 |
| Central corneal thickness [mm] | 550 ± 34 | 553 ± 34 | 547 ± 34 |
| Anterior chamber depth [mm] | 3.27 ± 0.35 | 3.33 ± 0.35 | 3.22 ± 0.34 |
| Lens thickness [mm] | 4.34 ± 0.35 | 4.35 ± 0.36 | 4.32 ± 0.33 |
| Axial length [mm] | 23.8 ± 1.2 | 24.1 ± 1.2 | 23.5 ± 1.2 |
| Mean Corneal power [dpt] | 43.5 ± 1.5 | 43.1 ± 1.5 | 43.8 ± 1.5 |
| ACPR | 0.548 ± 0.041 | 0.560 ± 0.040 | 0.537 ± 0.038 |
g – gram; n - number of participants; y – years; dpt – diopter; SEQ - spherical equivalent; mm - millimeter, ACPR – axial length to corneal power ratio, SES index – socioeconomic status using the German Health Update 2009 which ranges from 3 (lowest SES) to 21 (highest SES).36.
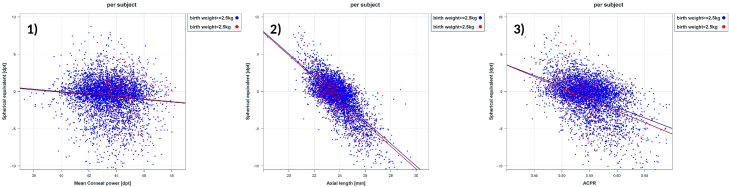
The scatter plots of corneal power and spherical equivalent, axial length and spherical equivalent, and axial length-to-corneal power-ratio with spherical equivalent are presented in Fig. 1. Linear regression analysis revealed, that axial length explains 58% of variance of spherical equivalent in low birth weight subjects, and 54% in normal birth weight subjects. In contrast, corneal power explained only 1% of variance of spherical equivalent in both groups.
Fig. 1.
Scatterplots of (1) corneal power, (2) axial length, and (3) axial length-to-corneal power-ratio (ACPR) of all participants of the Gutenberg Health Study with self-reported birth weight stratified for birth weight < 2.5 kg and ≥ 2.5 kg.
Association of refractive error and ocular geometry considering birth weight
Linear regression analyses showed an association of each ocular geometric segment namely corneal power, anterior chamber depth, lens thickness and axial length with refractive error (see Table 2). When controlling for birth weight, we found no effect of corneal power with higher birth weight on refractive error, while the negative effect size of axial length decreases with higher birth weight (B = 0.009 per 100 g, p = 0.002). The effect of anterior chamber depth and lens thickness on refractive error revealed no modification by birth weight. Associations of spherical equivalent with sex, age, corneal power, anterior chamber depth, lens thickness, axial length separated for low and normal birth weight individuals are presented in supplementary Table 1 and 2.
Table 2.
Associations of spherical equivalent with sex, age, corneal power, anterior chamber depth, lens thickness, axial length and consideration of birth weight as effect modification in the Gutenberg Health Study.
| Model 1 | Model 2 |
|||||
|---|---|---|---|---|---|---|
| B (95% CI) | p | R2 | B (95% CI) | p | R2a | |
| Sex (female) | −0.46 (−0.50; 0.42) | <0.001 | 0.848a | |||
| Age (years) | 0.67 (0.64; 0.69) | <0.001 | ||||
| Birth weight (100 g) | −0.35 (−0.61; −0.09) | 0.008 | ||||
| Mean corneal power (Diopter) | −0.17 (−0.20; −0.14) | <0.001 | 0.001 | −0.95 (−0.97; −0.92) | <0.001 | |
| Mean corneal power x birth weight (100 g) | 0.003 (−0.001; 0.007) | 0.13 | ||||
| Anterior chamber depth (mm) | −2.78 (−2.92; −2.64) | <0.001 | 0.150 | 1.70 (1.58; 1.81) | <0.001 | |
| Anterior chamber depth x birth weight (100 g) | −0.01 (−0.03; 0.01) | 0.30 | ||||
| Lens thickness (mm) | 1.36 (1.22; 1.50) | <0.001 | 0.037 | −0.20 (−0.28; −0.11) | <0.001 | |
| Lens thickness x birth weight (100 g) | 0.003 (−0.008; 0.015) | 0.55 | ||||
| Axial length (mm) | −1.50 (−1.54; −1.46) | <0.001 | 0.548 | −2.26 (−2.29; −2.22) | <0.001 | |
| Axial length x birth weight (100 g) | 0.009 (0.004; 0.02) | 0.002 | ||||
Model 1: Linear regression using generalized estimating equations to control for correlations between right and left eyes as crude model for each presented parameter.
Model 2: Linear regression using generalized estimating equations to control for correlations between right and left eyes with inclusion of sex, age, birth weight, mean corneal power, mean corneal power x birth weight, anterior chamber depth, anterior chamber depth x birth weight, lens thickness, lens thickness x birth weight, axial length, axial length thickness x birth weight.
R2 of the multivariable model with inclusion of all presented parameters.
Non responder analyses
Of all 12,423 study subjects, 5240 did not report birth weight data. Furthermore, 41 participants were excluded with self-reported birth weight < 1000 g or > 6000 g and 22 were excluded because of a history of corneal surgery. Furthermore, 1997 were excluded because of missing data about refractive error and / or ocular biometry and / or previous cataract surgery.
The item non-responder analysis of participants with and without self-reported birth weight showed that participants with self-reported birth weight were younger (56.2 ± 10.3 years versus 64.0 ± 9.9 years) and more often female (52.2% versus 44.2% female). There were only small differences in ocular geometry after adjusting for sex and age apart from axial length which was in participants with self-reported birth weight 0.14 mm (OD) and 0.13 mm (OS) longer.
Discussion
This study presents new results on the relation of refractive error and corneal power, anterior chamber depth, lens thickness and axial length considering effect modification by birth weight. Our results show that axial length variation explains the majority of variance in refractive error. Low birth weight is not linked to larger effects of steeper corneal shape on myopic refractive error, while the effect of axial length on myopia is enlarged in those subjects compared to newborns with normal birth weight.
Low birth weight is regarded as proxy for intrauterine malnutrition and/or preterm birth. These parameters are strong related with each other because the more premature the infants are born the lower is the birth weight.24 Furthermore, adverse intrauterine nutrition is also associated with low birth weight. All these parameters have frequently common origins in maternal nutritional and health status24 and several studies showed a relationship of these parameters on both, myopia1, 2, 3, 4, 5 and ocular shape25 development in childhood. The mechanism of developing myopia in this population is not well understood and there has been conflicting evidence in the literature.26 Only few population-based studies exist assessing the association of low birth weight with altered ocular geometry in childhood. They found in low birth weight children a steeper corneal curvature27, 28 and smaller axial length.27 In congruence, in our recent report18 and data of Sun and colleagues of the Australian Twin Study29 it was demonstrated that steeper corneal shape and smaller axial length in former low birth weight individuals seem to persist until adulthood. In contrast to our results, no association between low birth weight and refraction was reported in a twin study in participants aged from 18 to 86 years30 and in another study in participants aged 5–80 years.29 The authors hypothesized that compensatory emmetropization processes are leading to a normal refraction in later life in former low birth weight newborns despite the alterations of ocular geometry like a steeper cornea and a smaller axial length. In our recent report of the GHS, we could show that former low birth weight individuals have a slightly higher myopic refractive error in middle and late adulthood.17 We could previously demonstrate that low birth weight adults wear more frequently glasses for distance vision and had more frequently a myopic refractive error above 3 and 6 diopter17; these results may underline the clinical importance of our findings. However, with this analysis we want to close the gap of missing data about the correlation of ocular geometry and refractive error.
Fielder et al.26 categorized three different types of myopia in former preterm infants: 1) physiological and temporary myopia, 2) myopia of prematurity, and 3) myopia induced by severe ROP. As anatomic characteristics for this type of myopia, a flatter anterior chamber, more spherical lens, and a shorter axial length9 were described. In contrast to theses alterations, myopia of prematurity describes an earlier development of myopia as an abnormal refractive condition compared to full-term myopes with different anatomic features, like a steeper corneal curvature, smaller anterior chamber depth, and thicker lens accompanied by a smaller axial length in relation to the dioptric value.8 Various theories have been postulated to explain myopia development in former preterm infants. One theory discussed that lower ambient temperature after preterm birth (in comparison to intrauterine temperature) contributes to a less flattening of the cornea.10 Other theories were alterations of bone deficiency, light perception, visual deprivation and abnormal retinal function, or the occurrence and treatment of postnatal ROP.26 Particularly low birth weight newborns are at increased risk for ROP. In several studies strong associations between retinopathy of prematurity and its treatment with the development of significant refractive error could be observed explaining these by an anterior segment arrest.25, 31, 32, 33 Unfortunately, no data was available about postnatal occurrence of ROP which is a major flaw in our study and has to be considered at data interpretation.
Our data extends these previous reports17, 18 indicating that axial length variation explains the majority of variance in refractive error, while steeper corneal shape has no effects on refractive error. Low birth weight is not linked to slightly larger effects of steeper corneal shape on myopic refractive error, while the effect of axial length on myopia is fractionally enlarged in those subjects. Additional factors such as crystalline lens position and sphericity were not measured and could have played a role in the development of myopic refractive error in our subjects. In a previous report Barker et al. described that prenatal adverse growth during important organ developmental periods affects various organs morphology and functioning life-long.34, 35 Supporting this hypothesis, we could show in a recent report that there are fetal origins for adult eye disease because we found an increased risk for age related macular degeneration in low birth weight individuals.20 Consequently, one may speculate that our results of a more myopic refractive error and different ocular biometry compared to normal birth weight individuals are in line with these previous results. Refractive development is a visually guided process, and its components grow in relationship to each other at least until early adulthood. Our data could be potentially a hint that low birth weight affects the emmetropization process.
Strengths and limitations
One major strength of the presented study is the population-based study design with a large sample size. As study staff were masked to birth weight data, an investigator-dependent bias could be excluded.
There are several limitations. First, about 44% of the GHS study participants did not report their birth weight.17 Another limitation is that birth weight was self-reported and not obtained from birth records. We reported earlier, that the birth weight distribution of our cohort was comparable to governmental reports of the early 1970s.17, 23 In a previous report of a population-based study, a high reliability of self-reported birth weight was observed comparing self-reported birth weight to medical record data (intra-class correlation coefficient of 0.98; 95% CI 0.97– 0.98),29 which underlines the validity of birth weight self-reports. However, we cannot fully rule out that misclassification might have impacted our results. Another limitation is that there may be other factors probably influencing our analysis on myopia for which we could not adjust (e.g. leisure time activities in early childhood and adolescence including daily time of outdoor activities and nearwork). In addition, one major restriction is the lack of data for gestational age at birth and postnatal occurrence of ROP. Therefore, we cannot separate the effects of low birth weight, preterm birth, and ROP and its impacts on the relationship between myopia and ocular geometric factors. For all three parameters, it is well known that they may affect refractive error and morphologic eye development.25 Because low birth weight infants are more likely to be born with low gestational age and have postnatal ROP occurrence, we assume that low birth weight may also reflect the influence of preterm birth to some extent. A further restriction is that we cannot provide any information about the strength of correlation between birth weight and gestational age in our population-based study design. Refractive error was not measured in cycloplegic state. This could be a further limitation of the study, especially in younger subjects. In addition, we do neither have the shape and position of the human lens nor the refractive power and, thus, cannot state on any differences across birth weight groups. In previous reports, more extreme low birth weight subjects were investigated, which may lead to a larger impact of extreme low birth weight subjects on the results. This is in contrast to our study, which represents a more general and population-based approach. Furthermore, there is the possibility that our study is over-powered.
Summary
This study reports new results on the relation between refractive error and ocular geometry considering effect modification by birth weight. Our results indicate that axial length variation explains the majority of variance in refractive error, while steeper corneal shape has no effects on refractive error. Low birth weight is not linked to slightly larger effects of steeper corneal shape on myopic refractive error, while the effect of axial length on myopia is fractionally enlarged in those subjects.
Ethics approval and consent to participate
The study protocol and study documents were approved by the local ethics committee of the Medical Chamber of Rhineland-Palatinate, Germany (reference no. 837.020.07; original vote: 22.3.2007, latest update: 20.10.2015). According to the tenets of the Declaration of Helsinki, written informed consent was obtained from all participants prior to entering the study.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Funding/support/financial disclosure
All authors: The Gutenberg Health Study is funded through the government of Rhineland-Palatinate (“Stiftung Rheinland-Pfalz für Innovation“, contract AZ 961-386261/733), the research programs “Wissen schafft Zukunft” and “Center for Translational Vascular Biology (CTVB)” of the Johannes Gutenberg-University of Mainz, and its contract with Boehringer Ingelheim and PHILIPS Medical Systems, including an unrestricted grant for the Gutenberg Health Study. Wild PS is funded by the Federal Ministry of Education and Research (BMBF 01EO1503) and he is PI of the German Center for Cardiovascular Research (DZHK).
Schuster AK holds the professorship for ophthalmic healthcare research donated by „Stiftung Auge “and financed by „Deutsche Ophthalmologische Gesellschaft “and „Berufsverband der Augenärzte Deutschland e.V.“ He received research funding from Bayer Vital, Novartis, Heidelberg Engineering, Allergan and Plusoptix.
Pfeiffer N: receives financial support and grants by Novartis, Ivantis, Santen, Thea, Boehringer Ingelheim Deutschland GmbH & Co. KG, Alcon, Sanoculis; Nickels S: received reimbursement of travel expenses from Heidelberg Engineering GmbH; Beutel ME received speakers honorary from Pfizer Deutschland GmbH, Shire Deutschland GmbH and currently research grants from the governments of Rhineland-Palatinate and Nordrhein-Westfalen, the German Association of Psychoanalysis and Psychotherapy (DGPT), the German Research Foundation, the German Ministry of Research, the German Cancer Aid and the European Union; Fieß A, Schulz A, Münzel T, Urschitz M, Lackner KJ: none
Authors' contributions
Conceived and designed the study: MEB, NP, AF, AKS, SN; analyzed the data: AF, AKS, AS, SN; wrote the paper: AF, revised it critically: SN, AS, TM, PSW, MEB, MU, KJL, NP, AKS; all authors read and approved the final manuscript.
Access to data, responsibility and analysis
AS and PSW had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Statistical analyses were performed by AS.
The analysis presents clinical data of a large-scale population-based cohort with ongoing follow-up examinations. This project constitutes a major scientific effort with high methodological standards and detailed guidelines for analysis and publication to ensure scientific analyses on highest level. Therefore, data are not made available for the scientific community outside the established and controlled workflows and algorithms. To meet the general idea of verification and reproducibility of scientific findings, we offer access to data at the local database in accordance with the ethics vote upon request at any time. The GHS steering committee, which comprises a member of each involved department and the coordinating PI of the Gutenberg Health Study (PSW), convenes once a month. The steering committee decides on internal and external access of researchers and use of the data and biomaterials based on a research proposal to be supplied by the researcher. Interested researchers make their requests to the coordinating PI of the Gutenberg Health Study (Philipp S. Wild; philipp.wild@unimedizin-mainz.de. More detailed contact information is available at the homepages of the GHS (www.gutenberghealthstudy.org).
Acknowledgments
We thank all study participants for their willingness to provide data for this research project, and we are indebted to all coworkers for their enthusiastic commitment.
References
- 1.Fledelius H.C. Pre-term delivery and subsequent ocular development. A 7-10 year follow-up of children screened 1982-84 for ROP. 3) refraction. Myopia of prematurity. Acta Ophthalmologica Scandinavica. 1996;74:297–300. doi: 10.1111/j.1600-0420.1996.tb00096.x. [DOI] [PubMed] [Google Scholar]
- 2.Nissenkorn I., Yassur Y., Mashkowski D., Sherf I., Ben-Sira I. Myopia in premature babies with and without retinopathy of prematurity. Br J Ophthalmol. 1983;67:170–173. doi: 10.1136/bjo.67.3.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Quinn G.E., Dobson V., Kivlin J. Prevalence of myopia between 3 months and 5 1/2 years in preterm infants with and without retinopathy of prematurity. Cryotherapy for retinopathy of prematurity cooperative group. Ophthalmology. 1998;105:1292–1300. doi: 10.1016/s0161-6420(98)97036-1. [DOI] [PubMed] [Google Scholar]
- 4.Quinn G.E., Dobson V., Repka M.X. Development of myopia in infants with birth weights less than 1251 grams. The cryotherapy for retinopathy of prematurity cooperative group. Ophthalmology. 1992;99:329–340. doi: 10.1016/s0161-6420(92)31968-2. [DOI] [PubMed] [Google Scholar]
- 5.Robinson R., O’Keefe M. Follow-up study on premature infants with and without retinopathy of prematurity. Br J Ophthalmol. 1993;77:91–94. doi: 10.1136/bjo.77.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holmstrom M., el Azazi M., Kugelberg U. Ophthalmological long-term follow up of preterm infants: a population based, prospective study of the refraction and its development. Br J Ophthalmol. 1998;82:1265–1271. doi: 10.1136/bjo.82.11.1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Larsson E.K., Rydberg A.C., Holmstrom G.E. A population-based study of the refractive outcome in 10-year-old preterm and full-term children. Arch Ophthalmol. 2003;121:1430–1436. doi: 10.1001/archopht.121.10.1430. [DOI] [PubMed] [Google Scholar]
- 8.Fledelius H. Changes in refraction and eye size during adolescence. With special reference to the influence of low birth weight. Doc Ophthalmol Proc Series. 1981;29:217–223. [Google Scholar]
- 9.Fledelius H.C. Pre-term delivery and the growth of the eye. An oculometric study of eye size around term-time. Acta Ophthalmol (Copenh) 1992:10–15. doi: 10.1111/j.1755-3768.1992.tb04915.x. [DOI] [PubMed] [Google Scholar]
- 10.Fielder A.R., Levene M.I., Russell-Eggitt I.M., Weale R.A. Temperature--a factor in ocular development? Dev Med Child Neurol. 1986;28:279–284. doi: 10.1111/j.1469-8749.1986.tb03873.x. [DOI] [PubMed] [Google Scholar]
- 11.Hodos W., Revzin A.M., Kuenzel W.J. Thermal gradients in the chick eye: a contributing factor in experimental myopia. Invest Ophthalmol Vis Sci. 1987;28:1859–1866. [PubMed] [Google Scholar]
- 12.Garcia-Valenzuela E., Kaufman L.M. High myopia associated with retinopathy of prematurity is primarily lenticular. J AAPOS. 2005;9:121–128. doi: 10.1016/j.jaapos.2004.12.018. [DOI] [PubMed] [Google Scholar]
- 13.Connolly B.P., Ng E.Y., McNamara J.A., Regillo C.D., Vander J.F., Tasman W. A comparison of laser photocoagulation with cryotherapy for threshold retinopathy of prematurity at 10 years: part 2. Refractive outcome. Ophthalmology. 2002;109:936–941. doi: 10.1016/s0161-6420(01)01015-6. [DOI] [PubMed] [Google Scholar]
- 14.Kardaras D., Papageorgiou E., Gaitana K. The association between retinopathy of prematurity and ocular growth. Invest Ophthalmol Vis Sci. 2019;60:98–106. doi: 10.1167/iovs.18-24776. [DOI] [PubMed] [Google Scholar]
- 15.Kent D., Pennie F., Laws D., White S., Clark D. The influence of retinopathy of prematurity on ocular growth. Eye. 2000;14:23–29. doi: 10.1038/eye.2000.6. [DOI] [PubMed] [Google Scholar]
- 16.Fledelius H.C. Ophthalmic changes from age of 10 to 18 years. A longitudinal study of sequels to low birth weight. I. Refraction. Acta Ophthalmol (Copenh). 1980;58:889–898. doi: 10.1111/j.1755-3768.1980.tb08314.x. [DOI] [PubMed] [Google Scholar]
- 17.Fieß A., Schuster A.K., Nickels S. Association of low birth weight with myopic refractive error and lower visual acuity in adulthood: results from the population-based gutenberg health study (GHS) Br J Ophthalmol. 2018;103:99–105. doi: 10.1136/bjophthalmol-2017-311774. [DOI] [PubMed] [Google Scholar]
- 18.Fieß A., Schuster A.K., Nickels S. Association of Low birth weight with altered corneal geometry and axial length in adulthood in the German gutenberg health study. JAMA Ophthalmology. 2019;137:507–514. doi: 10.1001/jamaophthalmol.2018.7121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wild P.S., Zeller T., Beutel M. [The gutenberg health study] Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz. 2012;55:824–829. doi: 10.1007/s00103-012-1502-7. [DOI] [PubMed] [Google Scholar]
- 20.Fieß A., Elbaz H., Korb C.A. Low birth weight Is linked to age-related macular degeneration: results from the population-based gutenberg health study (GHS) Invest Ophthalmol Vis Sci. 2019;60:4943–4950. doi: 10.1167/iovs.19-27964. [DOI] [PubMed] [Google Scholar]
- 21.Fieß A., Elflein H.M., Urschitz M.S. Prevalence of strabismus and its impact on vision-related quality of life: results from the German population-based gutenberg health study. Ophthalmology. 2020 doi: 10.1016/j.ophtha.2020.02.026. [DOI] [PubMed] [Google Scholar]
- 22.Hohn R., Kottler U., Peto T. The ophthalmic branch of the gutenberg health study: study design, cohort profile and self-reported diseases. PLoS ONE. 2015;10 doi: 10.1371/journal.pone.0120476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.German Federal Statistical Office. Bevölkerung und Erwerbstätigkeit, Bevölkerungsbewegung: German Federal Statistical Office. Fachserie 1, Reihe 2. 1972-1980.
- 24.Shah P.S. Paternal factors and low birthweight, preterm, and small for gestational age births: a systematic review. Am J Obstet Gynecol. 2010;202:103–123. doi: 10.1016/j.ajog.2009.08.026. [DOI] [PubMed] [Google Scholar]
- 25.Fieß A., Kolb-Keerl R., Knuf M. Axial length and anterior segment alterations in former preterm infants and full-term neonates analyzed with scheimpflug imaging. Cornea. 2017;36:821–827. doi: 10.1097/ICO.0000000000001186. [DOI] [PubMed] [Google Scholar]
- 26.Fielder A.R., Quinn G.E. Myopia of prematurity: nature, nurture, or disease? Br J Ophthalmol. 1997;81:2–3. doi: 10.1136/bjo.81.1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ojaimi E., Robaei D., Rochtchina E., Rose K.A., Morgan I.G., Mitchell P. Impact of birth parameters on eye size in a population-based study of 6-year-old Australian children. Am J Ophthalmol. 2005;140:535–537. doi: 10.1016/j.ajo.2005.02.048. [DOI] [PubMed] [Google Scholar]
- 28.Fieß A., Schuster A.K., Pfeiffer N., Nickels S. Association of birth weight with corneal power in early adolescence: results from the national health and nutrition examination survey (NHANES) 1999-2008. PLoS ONE. 2017;12 doi: 10.1371/journal.pone.0186723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sun C., Ponsonby A.L., Brown S.A. Associations of birth weight with ocular biometry, refraction, and glaucomatous endophenotypes: the Australian twins eye study. Am J Ophthalmol. 2010;150:909–916. doi: 10.1016/j.ajo.2010.06.028. [DOI] [PubMed] [Google Scholar]
- 30.Dirani M., Islam F.M., Baird P.N. The role of birth weight in myopia--the genes in myopia twin study. Ophthalmic Res. 2009;41:154–159. doi: 10.1159/000209669. [DOI] [PubMed] [Google Scholar]
- 31.Algawi K., Goggin M., O’Keefe M. Refractive outcome following diode laser versus cryotherapy for eyes with retinopathy of prematurity. Br J Ophthalmol. 1994;78:612–614. doi: 10.1136/bjo.78.8.612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.White J.E., Repka M.X. Randomized comparison of diode laser photocoagulation versus cryotherapy for threshold retinopathy of prematurity: 3-year outcome. J Pediatr Ophthalmol Strabismus. 1997;34:83–87. doi: 10.3928/0191-3913-19970301-06. quiz 121-122. [DOI] [PubMed] [Google Scholar]
- 33.Holmstrom G.E., Larsson E.K. Development of spherical equivalent refraction in prematurely born children during the first 10 years of life: a population-based study. Arch Ophthalmol. 2005;123:1404–1411. doi: 10.1001/archopht.123.10.1404. [DOI] [PubMed] [Google Scholar]
- 34.Barker D.J., Bull A.R., Osmond C., Simmonds S.J. Fetal and placental size and risk of hypertension in adult life. Bmj. 1990;301:259–262. doi: 10.1136/bmj.301.6746.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barker D.J. Maternal nutrition, fetal nutrition, and disease in later life. Nutrition (Burbank, Los Angeles County, Calif.). 1997;13:807–813. doi: 10.1016/s0899-9007(97)00193-7. [DOI] [PubMed] [Google Scholar]
- 36.Lampert T., Kroll L.E., Muters S., Stolzenberg H. [Measurement of the socioeconomic status within the German health update 2009 (GEDA)] Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz. 2013;56:131–143. doi: 10.1007/s00103-012-1583-3. [DOI] [PubMed] [Google Scholar]