Participation in regular physical activity improves quality of life and well-being in many, including older adults and adults.
Keywords: Quality of life, Health-related quality of life, Well-being, Physical activity, Systematic review
Abstract
Maintaining or improving quality of life (QoL) and well-being is a universal goal across the lifespan. Being physically active has been suggested as one way to enhance QoL and well-being. In this systematic review, conducted in part for the 2018 U.S. Health and Human Services Physical Activity Guidelines for Americans Scientific Advisory Committee Report, we examined the relationship between physical activity (PA) and QoL and well-being experienced by the general population across the lifespan and by persons with psychiatric and neurologic conditions. Systematic reviews, meta-analyses, and pooled analyses from 2006 to 2018 were used for the evidence base. Strong evidence (predominantly from randomized controlled trials [RCTs]) demonstrated that, for adults aged 18–65 years and older adults (primarily 65 years and older), PA improves QoL and well-being when compared with minimal or no-treatment controls. Moderate evidence indicated that PA improves QoL and well-being in individuals with schizophrenia and Parkinson’s disease, and limited evidence indicated that PA improves QoL and well-being for youth and for adults with major clinical depression or bipolar disorder. Insufficient evidence existed for individuals with dementia because of a small number of studies with mixed results. Future high-quality research designs should include RCTs involving longer interventions testing different modes and intensities of PA in diverse populations of healthy people and individuals with cognitive (e.g., dementia) and mental health conditions (e.g., schizophrenia) to precisely characterize the effects of different forms of PA on aspects of QoL and well-being.
Implications.
Practice: Researchers, educators, and providers should know that participation in regular physical activity (PA) is likely to improve quality of life (QoL) and well-being in many populations.
Policy: Enrolling samples of sufficient size and diversity to support intervention moderator analyses along with mediator analyses will provide useful information for adapting the interventions to optimize uptake among different subgroups.
Research: Incorporating diverse population subgroups, including diverse racial/ethnic groups and vulnerable and underrepresented population groups will expand the potential for having a broader public health impact in disseminating this research.
INTRODUCTION
The World Health Organization (WHO) definition of health encompasses both the absence of disease and the presence of mental and social well-being [1]. Separate theoretical traditions distinguish between evaluative well-being (e.g., life satisfaction and quality of life [QoL]) and experienced well-being (e.g., happiness and positive affect) [2]. These subjective reports frequently overlap, so an umbrella domain of QoL and well-being has emerged [3]. QoL is a global construct often used interchangeably with subjective well-being [4]. QoL is distinct from mental health symptoms and reflects the presence of positive aspects in one’s life.
QoL has a hierarchical structure, with domain-specific components under the umbrella of overall QoL. One domain typically represents health-related QoL (HRQoL) [5]; this domain is often split further into subdomains of physical HRQoL (e.g., evaluations of physical function) and mental HRQoL (e.g., emotional health). Three separate components of subjective well-being have been identified: positive affect, negative affect, and life satisfaction [6]. The first two components refer to the affective, emotional aspects of the construct; the latter to the cognitive-judgmental aspects [4,6]. Given the variable and expansive conceptualizations of QoL and well-being, the literature reviewed here is comprehensive in nature and focuses on both global QoL and HRQoL, as well as on well-being and its derivatives, such as subjective well-being, positive well-being, or psychological well-being.
Being physically active has been suggested as one way to enhance QoL and well-being. Potential mechanisms of the physical activity (PA) and QoL/well-being relationship include PA-induced changes in neurotransmitters of the brain and endogenous opioids that are known to be associated with depression, anxiety, and other mood constructs [7,8]. Others have found that a latent conceptualization of psychological distress (i.e., depression, anxiety, stress, and sleep disturbance) was associated with improvements in well-being/satisfaction with life [9]. Psychological constructs have also been reported to play a mechanistic role. Elavsky et al. [10] reported that increased self-efficacy and positive affect resulting from a PA intervention were significantly associated with greater well-being/satisfaction with life. Research has also shown that personality traits (e.g., neuroticism, extroversion, and agreeableness) may predict well-being/satisfaction with life [11,12]. That said, more work is needed to examine if these are truly causal mechanisms.
The charge of the 2018 Physical Activity Guidelines Advisory Committee (PAGAC) was to review the scientific literature of the relationships between PA and QoL. The PAGAC Brain Health Subcommittee was to focus on the general population and not those with chronic diseases being covered by other PAGAC subcommittees. The exception was that the PAGAC Brain Health Subcommittee was also charged with examining the topic (PA and QoL) in populations with conditions related specifically to the brain (e.g., schizophrenia and depression). Also, PA levels have been shown to decline across the lifespan and, thus, a lifespan approach allowed us to examine whether effects are more consistent at certain points in the lifespan. We describe the results of this review and expand it to incorporate research on the relationships between PA and well-being. By integrating the literature across ages and mental health conditions, we sought to develop a global assessment of three questions: (a) What is the relationship between PA and QoL and well-being? (b) Does a dose–response relationship exist and what is the shape of the relationship? (c) Does the relationship vary by age, sex, race/ethnicity, socioeconomic status, or weight status?
METHODS
This paper summarizes evidence from scientific reviews examining the effects of PA on QoL and well-being across the lifespan and the effects of PA on QoL and well-being in individuals with psychiatric conditions (but excludes mental health symptoms as outcomes). QoL among individuals who have a chronic physical condition, such as diabetes or osteoarthritis, was not examined here because it was covered by other subcommittees of the PAGAC (e.g., [13, 14]).
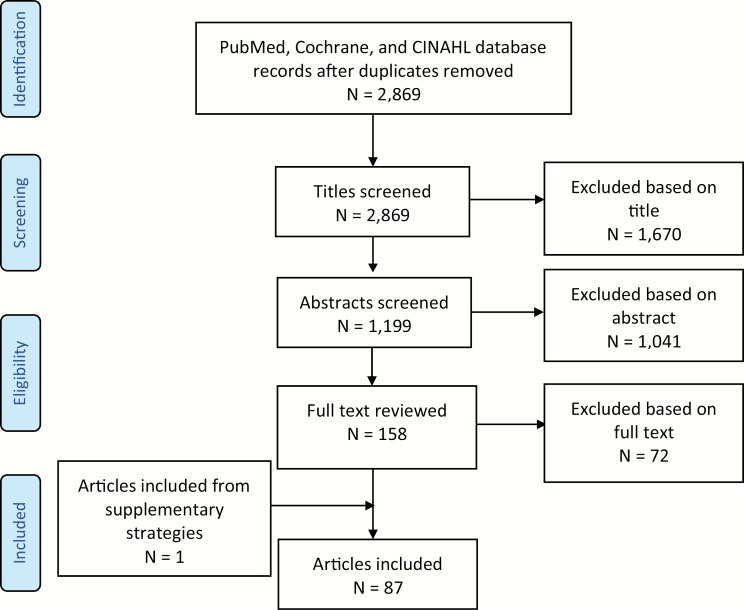
This review followed the methods used to conduct the reviews that informed the 2018 PAGAC Scientific Report [15]. The searches were conducted in electronic databases (PubMed, CINAHL, and Cochrane) and supplemented by additional articles identified by experts. The inclusion criteria were predefined, and studies were considered potentially eligible if they were systematic reviews (SRs), meta-analyses (MAs), or pooled analyses published in English from 2006 to February 2017. The year 2006 was chosen as the earliest year of publication of the reviews reviewed. Although QoL was not included in the 2008 PA Guidelines, we wanted to include studies that would not have been included in the 2008 Guidelines. Studies of PA and well-being or studies published in 2017 or 2018 (i.e., after data extraction for the PAGAC report) are also included as the search was updated for this manuscript. Details of the PAGAC search strategy is available at https://health.gov/paguidelines/second-edition/report/supplementary_material/pdf/Brain_Health_Q2_Quality_of_Life_Evidence_Portfolio.pdf.
Given that the terms QoL and well-being are often used interchangeably, and the 2018 PA Guidelines Scientific Advisory Committee was unable to include well-being in their search, we added it to this review for a more comprehensive paper. For the sake of this review, we used a relatively broad definition of PA to include play and recess activities in children to structured exercise programs for adults and experimental manipulations of acute bouts of exercise. All types and intensities of PA, including free-living activities and play, were included in the search as intervention/exposures as was sedentary behavior. Studies of hospitalized patients or animals were excluded.
Two abstractors independently conducted data abstraction tasks. Abstractors were assigned groups of articles to review in an online database. After both abstractors completed the groups, the pair reviewed their entries, discussed discrepancies, and reached an agreement. When needed, the abstractors included a third team member to discuss the disagreements or to gain clarification. In addition to abstracting key information from SRs, MAs, and pooled analyses, the pair of abstractors independently assessed each existing review’s quality using AMSTARExBP, a modified version of “A Measurement Tool to Assess Systematic Reviews” (AMSTAR). This was used to assess the methodological quality of SRs and MAs. AMSTARExBP is an adaptation of AMSTAR that focuses on MAs that examined the effects of exercise training on blood pressure. The training and quality control team made additional revisions to adapt AMSTARExBP for the Committee (SR, MA, and Pooled Analysis Quality Assessment Using Tailored AMSTARExBP Instrument). The protocol for this review was registered at PROSPERO #CRD42018096695. Figure 1 shows the search strategy and study selection process.
Fig 1.
Systematic review process.
RESULTS
A total of 87 articles (35 from the original PAGAC report; 52 from the updated search) comprised of 29 MAs and 58 SRs were identified, which examined the effects of randomized controlled trials (RCTs) and prospective longitudinal studies with QoL and well-being outcomes. Data were extracted and bias was assessed independently by two reviewers, with disagreement resolved by discussion or by a third person. The results of the bias assessment can be seen in the Supplementary Appendix. Reviews included results from youth (<18 years; n = 8), adults (n = 31), older adults (n = 25), and nonspecified age and conditions (n = 2), as well as populations with depression or bipolar disorder (n = 4), dementia (n = 5), Parkinson’s disease (n = 5), and schizophrenia (n = 7). We summarized the outcomes of our review with the following “grades”: (a) Not assignable, (b) Limited, (c) Moderate, and (d) Strong (see [15] for an in-depth description and the defining characteristics of these categories). Table 1 presents conclusions on the strength of the evidence in each of the following domains.
Table 1.
Assigned grades for the effects of physical activity (PA) on quality of life (QoL) and well-being for various ages and clinical outcomes
| Population or condition | Outcome | Grade |
|---|---|---|
| Older adults | Strong evidence demonstrates that, for older adults (older than 50 years; primarily 65 years and older), PA improves health-related QoL (HRQoL) and well-being when compared with minimal or no-treatment controls. | Strong |
| Adults | Strong evidence demonstrates that, for adults aged 18–65 years, PA improves HRQoL and well-being when compared with minimal or no-treatment controls. | Strong |
| Youth | Limited evidence suggests that, among youth aged 5–18 years, greater PA and lower levels of sedentary time are associated with higher perceptions of QoL and well-being. | Limited |
| Dementia | Insufficient evidence to determine the relationship between PA and QoL and well-being in individuals with dementia because of a small number of controlled studies with mixed results | Not assignable |
| Depression and bipolar disorder | Limited evidence suggests that PA improves QoL and well-being for adults with major clinical depression and bipolar disorder. | Limited |
| Schizophrenia | Moderate evidence indicates that PA improves QoL and well-being in individuals with schizophrenia. | Moderate |
| Parkinson’s disease | Moderate evidence indicates that PA improves QoL and well-being in individuals with Parkinson’s disease. | Moderate |
| Across variable conditions and populations | Insufficient evidence to determine the relationship between PA and QoL and well-being. | Not assignable |
OLDER ADULTS
The greatest wealth of evidence for an effect of PA on QoL and well-being was found for older adults. In a review of reviews, Zubala et al. found that despite their heterogeneity, interventions often resulted in sustained increases in PA over the study period, typically at 12 months, and led to improvements in general well-being [16]. In a pooled analysis, participants who were physically active for more than 150 min per week, but then dropped to below 150 min per week from baseline to 6 months, showed an average drop of −11.8 (p < .001) in SF-36 physical function scores. In contrast, those who were physically active for fewer than 150 min per week but then increased to more than 150 min per week from baseline to 6 months showed an average increase of +5.1 in SF-36 physical function scores [17].
Overall, meta-analytic results showed that PA consistently improved QoL in older adults. One MA reported that, collectively, exercise programs (1,317 participants) improved QoL (overall and health-related combined) of older adult participants relative to inactive control groups (Z = 2.23, p = .03), with a pooled standardized mean difference (SMD) of 0.86 (95% confidence interval [CI]: 0.11 to 1.62) [18]. Another MA found an overall positive effect of exercise interventions on mental well-being (standardized effect size = 0.27; CI = 0.14 to 0.40) and concluded that mental well-being in later life is modifiable through exercise and PA [19]. Kelly et al. found improvements for the physical function subscale of the physical function component summary score of the SF-36 (Hedges’ g = 0.41, 95% CI: 0.19 to 0.64, p < .001) [20].
These results appear to be consistent across modes of PA. Modes of PA that involve mental and physical components, such as Yoga, Pilates, Qigong, and Tai Chi, hold great potential for improving QoL in both healthy and chronically ill individuals [21]. An SR of 10 intervention studies on Pilates included four studies showing improvement in domains of HRQoL, including domains of sensorial abilities, activities, social participation, and intimacy. Furthermore, an MA pooling effects of alternative modes of PA on HRQoL, depression, and activities of daily living showed a large composite positive effect size (Hedges’ g = 0.93; 95% CI: 0.631 to 1.25, p < .001) [22]. Two recent MAs found a positive effect of specific modes of PA. One included intervention studies of Nordic Walking, a form of brisk walking utilizing a walking pole. Nordic Walking improved QoL compared with walking without poles (d = 0.53) or resistance training (d = 0.93) [23]. Another identified 12 RCTs of high methodological quality, totaling 752 participants, and found that Yoga improved HRQoL with a medium effect size (Hedges’ g = 0.51, 95% CI: 0.25 to 0.76) and improved mental well-being with a small effect (Hedges’ g = 0.38, 95% CI: 0.15 to 0.62) [24]. Another review suggested that mindful movement (e.g., Yoga, Tai Chi, and walking meditation) may outperform conventional physical exercise with regard to effects on QoL [25]. However, some modes of PA, such as interventions with virtual reality/gaming systems had low-quality ratings and limited the ability to draw conclusion on the effectiveness of such modes of PA [26].
The amount of change in overall and specific components of QoL and well-being varied across studies of older adults. Some reviews showed a wide range in QoL score improvement (17.1%–178%) and found that only some SF-36 subscales improved (i.e., physical functioning, role limitations due to physical health or emotional problems, pain, general health, and vitality [energy/fatigue]) [27]. Raymond [28] found improved HRQoL in four of these subscales among the six it examined (physical functioning, role limitations due to physical health or emotional problems, vitality, social functioning, and mental health [emotional well-being]; p range <.001 to .04). A meta-analytic review by Stevens [29] found significant improvements in vitality (odds ratio [OR] = 4.43, 95% CI: 0.31 to 8.54) and general health (OR = 5.46, 95% CI: 1.69 to 9.24). A meta-analytic review of Yoga studies reported improvements for the composite scores for both the physical health subdomain of the SF-36 (SMD = 0.65 [95% CI: 0.02 to 1.28]) and for the mental health subdomain (SMD = 0.66 [95% CI: 0.10 to 1.22]) in favor of the Yoga intervention [30]. A review of intervention, cross-sectional, and longitudinal studies found that PA was consistently associated with several QoL domains: functional capacity; general QoL; autonomy; past, present, and future activities; death and dying; intimacy; mental health; vitality; and psychological QoL [31].
The effects of PA on QoL and well-being on specific segments of older adults are less clear. One SR that intended to assess the effectiveness of interventions across the transition to retirement was inconclusive because of insufficient evidence [32]. Among frail older adults, one review found no significant difference in QoL in studies that used water exercises, flexibility exercises, Tai Chi, and resistance exercises compared to control groups [33] and others found too few studies to reach conclusions [34–36].
A related SR examined combined interventions that included PA but did not focus on PA. Not surprisingly, it was found that combined dietary and exercise components (compared to exercise alone) led to the greatest improvement in QoL [37]. Another review assessed the effectiveness of psychosocial interventions for the promotion of mental health and prevention of depression among older people, but the effects of exercise specifically on QoL was not reported [38]. Reviews of multimodal exercise programs in older adults (strengthening exercises, cardiovascular, flexibility, and balance training) found small improvements in QoL [39,40].
In sum, strong evidence demonstrates that, for older adults (older than 50 years; primarily 65 years and older), PA improves HRQoL and well-being when compared with minimal or no-treatment controls.
ADULTS AGED 18–65 YEARS
Fewer studies have examined young and midlife adults compared to older adults, but those that have indicated a positive association between PA and QoL and well-being. One MA reported a positive trend for PA on overall QoL (n = 7, SMD = 0.11 [95% CI: −0.03 to 0.24]) and positive effects on physical health QoL (n = 6, SMD = 0.22 [95% CI: 0.07 to 0.37]) and psychological well-being (n = 6, SMD = 0.21 [95% CI: 0.06 to 0.36]) as a result of PA interventions [41]. Another review (n = 15: 4 RCTs, 3 cohorts, and 5 cross-sectional studies) allowed the examination of PA exposure and QoL [42]. Three of the four RCTs reported significant improvements in reported QoL for the PA exposure versus control group. All of the cohort studies reported significantly higher QoL among those who were more physically active, and all of the cross-sectional studies reported a positive association between more PA and higher-assessed QoL. A large SR included 58 individual studies, 18 (3 cohort and 15 cross-sectional designs) of which assessed QoL with the SF-36 [43]. Of the three cohort studies, all reported positive associations for mental health and two of the three for physical health and vitality. Of the 15 cross-sectional studies, 13 reported positive associations between PA and the physical health domain and 9 reported positive associations for the mental health domain, with positive associations for subdomains related to vitality (9 studies) and pain (8 studies).
Recent MAs have examined the effects of Pilates, Yoga, or Tai Chi on QoL or well-being. However, some MAs did not examine the effects of PA on QoL or well-being as primary outcomes; thus, quantitative data on QoL or well-being was not presented. In an MA and review of Pilates, Pilates practice yielded positive effects on QoL up to 6 months in RCT results [44]. An MA of 17 RCTs reported a significant increase in psychological well-being in favor of Yoga over no active control groups but not compared to other modes of PA. However, for life satisfaction (emotional well-being), social relationships (social well-being), and mindfulness, no significant effects for Yoga were found across active or nonactive controls [45]. An SR on Sahaja Yoga found similar results such that Sahaja Yoga is also associated with increased subjective well-being and psychological well-being [46]. Another MA compared Yoga with no treatment, but results for QoL were not reported, partially, because the focus was on menopausal symptoms [47]. Walking groups also have an impact on QoL in adults. An MA showed increases in the SF-36 (physical functioning) score of 6.02 (0.51–11.53) [48]. However, the evidence was less clear for other outcomes, such as the SF-36 mental health component, and these studies did not have controls. A more recent MA of group walking found that five of seven trials showed improved scores for group walking versus inactive controls [49].
An MA of Tai Chi interventions found that Tai Chi had a significant effect on general health (SMD = −5.08; 95% CI: −7.60, –2.56; p < .0001) and vitality (SMD = −5.67; 95% CI: –8.54, –2.81; p = .0001) of the SF-36 but had no effect on physical function, emotional health, social function, and physical role of the SF-36 [50]. More MAs demonstrated that leisure-time PA (LTPA) is associated with life satisfaction (k = 7; n = 2,544; r = .12) [51] and that trials showed general improvements in QoL over 6–12 months within PA intervention groups, but there was no consistent benefit of the intervention compared with control conditions [52]. Also, meta-analytical methods have indicated that lower levels of sedentary behaviors were associated with higher physical HRQoL (estimate of average effect: r = −.140; 95% CI: −.191, −.088) [53].
These positive associations of PA with QoL and well-being from MAs were partly corroborated in reviews of SRs. A review of SRs of Tai Chi studies found fair evidence for increased well-being as a result of participation in Tai Chi but not excellent or good evidence as found for other health outcomes [54]. A review of reviews found that walking programs improved psychological well-being and subjective well-being, although findings varied in effectiveness and the volume of walking required [55].
Other SRs reported similar positive associations between PA and QoL across domains and modes of PA, including LTPA [56], walking [57], gardening [58], Zumba [59], Qigong and related alternative or complementary types of PA [60], and mixtures of aerobic, strength training and alternative or complementary types of PA [61,62]. A review of strength training on psychological outcome measures including QoL reported either comparable effects or no additional benefits to those interventions on QoL [63].
A number of SRs focused on segments of the population, as opposed to the mode of PA. Among office-based workers, PA interventions (exercise, Yoga, and walking) improved well-being across workplace settings compared to no intervention [64]. Inconsistent results with respect to subjective well-being at work were found in a review of the effects of strength training for women on their health in the workplace [65]. Positive effects of PA on well-being were also found for military personnel and veterans. In one review, exercise was found as one of the nondeployment-related factors positively impacting well-being of military personnel [66], and PA enhanced subjective well-being in combat veterans through active coping [67]. Reviews of perimenopausal or postmenopausal women and women with premenstrual syndrome (PMS) found reductions in symptoms; however, results specific to QoL were not reported [68,69].
Some SRs included PA as one of many health behaviors in interventions, and they appear to have benefits to well-being spanning healthy populations and those with physical or mental health problems [70]; however, the findings specific to the independent effect of PA was not clear. One review found that exercise was more effective than meditation for improving physical HRQoL. That said, the interventions (nonactive forms of meditation vs. exercise) were comparable when evaluating well-being outcomes [71]. In sum, strong evidence demonstrated that, for adults aged 18–65 years, PA improved HRQoL and well-being when compared with minimal or no-treatment controls.
YOUTH
At the time of writing of the PAGAC scientific report, only one review on sedentary behavior and QoL was published in youth. Of the 91 studies included in that review, 15 studies provided information about the relationship between sedentary behavior and QoL among youth aged approximately 9−17 years. Nine of the 12 cross-sectional studies and 2 of the 3 longitudinal studies reported a negative association between sedentary behavior time and QoL [72].
In the updated search of our group that included PA and well-being (vs. QoL only), reviews focused on sedentary behavior and QoL and well-being in youth were found. A review of screen-based sedentary behavior among adolescent girls reported negative associations between screen time and psychological well-being [73]. A more recent review of sedentary behavior and PA similarly found that higher levels of PA were associated with better HRQoL and increased time of sedentary behavior was linked to lower HRQoL among children and adolescents [74].
Other reviews have focused only on PA and QoL or well-being, with mixed results. In primary school-aged children, null results were found between the PA program Loose Parts Play (LPP) and control groups for psychosocial QoL [75]. Joronen et al. reviewed studies of exergames on child and adolescent well-being, and exergaming was found to have some positive effects on psychological and social well-being [76]. Poitras et al.’s review of apparently healthy children and youth (including those with overweight and obesity) with a mean age of 5–17 years found available studies to be of poor quality with no consistent findings but did find that total PA (steps per day) was positively correlated with QoL [77].
Two SRs focused on specific segments of the youth population, both with limitations. One focused on at-risk youth (e.g., high risk, troubled, and antisocial) and identified 15 studies that examined the effects of three types of PA (i.e., outdoor adventure, sport- and skill‐based, and physical fitness programs) on social and emotional well‐being. However, while many of the interventions reported significant positive effects, the risk of bias was high in all of the included studies [78]. Another review of overweight or obese children from the age of 6 to 11 years examined behavioral treatments, which included PA. Unfortunately, few trials reported HRQoL outcomes, and none of the analyses demonstrated a substantial difference in these outcomes between intervention and control groups [79]. In sum, limited evidence suggested that among youth aged 5−18 years, greater PA and lower levels of sedentary time are associated with higher perceptions of QoL and well-being.
DEMENTIA
Overall, few reviews addressed the association between PA and QoL for individuals with dementia; and most did not support an association between PA and QoL for individuals with dementia. MA of six studies showed no significant differences in five of the studies for QoL outcomes for individuals in PA intervention groups compared with controls. The average effect was small and nonsignificant (SMD = 0.33 [95% CI: −0.21 to 0.87]). Also, when one outlier was excluded, the effect was not significantly different from 0 (SMD = 0.06 [95% CI: −0.10 to 0.22]). Modes of PA included aerobic training, strength training, combined aerobic and resistance training, flexibility, balance, Yoga, and Tai Chi [80].
Recent reviews have concluded that strong evidence indicates that exercise did not improve QoL in this population [81,82]; one review of SRs found no evidence on the benefits of exercise on QoL [83]. Two reviews reported on specific domains of QoL. One review found positive effects on selected domains of QoL, including physical role functioning [84], while a review with six randomized and controlled studies had mixed results for both global QoL and specific domains [85].
Overall, the evidence for an association between PA and QoL based on controlled studies was inconsistent, in part, due to the small number of studies that systematically evaluated QoL and well-being and inconsistency in outcome measures with respect to reporting generalized QoL versus disease-specific QoL outcomes. In addition, the number of studies and sample sizes were insufficient to adequately analyze effects of different exercise training modalities, and no studies differentiated their effects based upon the categorical type of dementia (Alzheimer’s disease [AD] and related dementias) or the stage(s) of dementia in the participants. In sum, there was insufficient evidence to determine the association between PA and QoL and well-being in individuals with dementia.
DEPRESSION AND BIPOLAR DISORDER
A small but growing area of research focuses on the impact of PA on QoL and well-being in individuals with major clinical depression or bipolar disorder. Limited evidence from 11 controlled studies suggests that PA improves selected domains of QoL for adults with major clinical depression, while the evidence for bipolar disorder was insufficient [85–87].
MAs of four RCTs in adults with clinical depression comparing PA to either placebo or no PA found no differences for the mental (SMD = −0.24, 95% CI: −0.76 to 0.29), psychological (SMD = 0.28, 95% CI: −0.29 to 0.86), and social domains (SMD = 0.19, 95% CI: −0.35 to 0.74) [86]. However, two studies reported a moderate effect size for improved environment domain (SMD = 0.62, 95% CI: 0.06 to 1.18), and four out of four studies reported a moderate effect size for improved physical domain (SMD = 0.45, 95% CI: 0.06 to 0.83) in favor of the group assigned to structured PA. By contrast, controlled studies comparing PA to other therapeutic modalities for the treatment of depression, including cognitive therapy, as well as antidepressant medication, showed no between-group differences in the mental or physical domains of QoL [86]. A review of four RCTs in older adults with depression found that PA improved QoL in most reports [85]. One RCT comparing Yoga to a relaxation control group showed an improvement of 50% or greater on mental QoL domain in the Yoga group [87].
One review examined lifestyle interventions targeting dietary habits and exercise in individuals with bipolar disorder. Overall findings point toward a beneficial role of lifestyle interventions on PA and overall well-being; however, the magnitude is unknown [88]. In sum, limited evidence suggested that PA improves QoL and well-being for adults with major clinical depression and bipolar disorder.
SCHIZOPHRENIA
Moderate evidence supports the positive effects of PA on QoL for individuals with schizophrenia. These results come from consistent findings from SRs of studies involving inpatients and outpatients across the adult age span [89,90]. The positive effects of PA are shown by their effect size in MAs of 11 controlled or uncontrolled intervention studies that show significant improvements, with moderate standardized effect sizes for overall QoL (Hedges’ g = 0.55, p < .01) and for specific domains of physical (Hedges’ g = 0.50), social (Hedges’ g = 0.67), and environmental QoL (Hedges’ g = 0.62) [91]. Mental QoL did not change in this population (Hedges’ g = 0.38). Both aerobic exercise (Hedges’ g = 0.58) and Yoga interventions (Hedges’ g = 0.58) were found to be effective. Holley et al.’s SR found that PA has a beneficial effect on some attributes associated with psychological well-being in individuals with schizophrenia [92], but instruments used to measure psychological well-being varied across all studies, limiting the ability to compare results.
Several reviews focused on the impact of Yoga (varying forms) as PA on QoL and well-being in people with schizophrenia. An MA reported moderate evidence for short-term effects of Yoga on QoL compared to usual care (SMD = 2.28; 95% CI 0.42 to 4.14; p = .02,), but these effects were only present in studies with high risk of bias. When comparing Yoga to exercise, no evidence was found for short-term effects on QoL (SMD = 0.17; 95% CI −0.27 to 0.61; p = .45) [87]. A small review of three RCTs reported that physical, psychological, social, and environmental HRQoL as measured with the abbreviated version of the WHO Quality of Life questionnaire (WHOQOL-BREF) increased more significantly after Yoga than after exercise or waiting list control conditions [89].
A series of SRs from Broderick et al. examined Yoga versus standard care [93], versus nonstandard care [94], and as part of a package of care versus standard care [95]. Promising effects were found, including differences in QoL in favor of the yoga group versus standard care [93]; however, nearly all of the studies examined were rated as low-quality evidence, had a small sample size, and had mixed results. In sum, moderate evidence indicated that PA improves QoL and well-being in individuals with schizophrenia.
PARKINSON’S DISEASE
An emerging area of research examines the impact of PA on QoL and well-being among people with Parkinson’s disease (PD). This topic was not covered in the PAGAC Scientific Report, but the results of two recently published MAs are summarized here. Lee et al. reported on the effects of nonpharmacological interventions on HRQoL, including exercise programs with an effect size of −5.73 with 95% CI of −11.36 to −0.10 (Z = 2.00, p = .05) [96]. Thus, nonpharmacological interventions, and particularly exercise programs, were effective in improving HRQoL of PD patients [96]. Another MA suggested a potential benefit of Tai Chi Quan for improving QoL for individuals with PD [Effect Size = −0.393, p < .001] [97].
SRs, in addition to MAs, support the potential for PA to influence QoL and well-being among people with PD. Wu [98] found evidence to support the efficacy of PA to influence QoL for the PD population. Aerobic training exercise significantly improved the participants’ QoL scores, and a balance-training program, such as Tai Chi, also improved QoL [98]. A review of aquatic physiotherapy also suggested that it improved aspects of QoL [99]. A review of Tai Chi studies found that participants enrolled in Tai Chi had improved well-being (one or more aspect) by the end of the program [100]. In sum, moderate evidence indicated that PA improves QoL and well-being in individuals with PD.
CHRONICALLY ILL POPULATIONS
Two recent SRs examined the evidence related to PA and QoL or well-being more broadly [101,102]. Zou et al. examined studies with Baduanjin Qigong as the mode of PA, and participants across studies included 559 adults with healthy status and 976 with different types of diseases (e.g., Type 2 diabetes mellitus, cancer, PD, hypertension, knee osteoarthritis, and chronic fatigue syndrome-like illness). The aggregated results showed significant benefits in favor of Baduanjin Qigong on QoL (SMD = −0.75; 95% CI −1.26 to −0.24; p = .004; [101]). Another review examined modern postural Yoga as a mental health promoting tool with conflicting results across samples of youth, middle-aged women, and older adults [102]. Given the small number of reviews and variable nature of the individual studies and sample makeup, a grade is not assignable.
DISCUSSION
Due to a lack of experimental studies, few MAs and SRs have focused on the impact of PA on well-being or QoL in older adults [103], let alone across a broad array of QoL and well-being. Thus, rigorous SRs of these reviews are even rarer. There has also been inconsistency in search strategies across prior reviews; thus, the exhaustive search strategy we employed tried to be as inclusive as possible. The rigor of the current review, the large number of reviews included, and conclusions for various aspects of the population contribute to our knowledge on the topic of the relationship between PA and QoL and well-being.
The first aim of this umbrella review was to determine the relationship between PA and QoL and well-being. The strongest evidence existed for older adults and was based on the largest body of evidence. Adults also demonstrated a positive relationship between PA and QoL and well-being. The vast majority of studies included in the reviews were RCTs, though not all of them; thus, it is possible that unobserved third variables (e.g., functional ability) could create the appearance of an effect.
For several other populations, an insufficient number of studies and mixed- or low-quality studies included in the reviews provided weaker evidence. In some populations (e.g., neurologic and psychiatric conditions), it is much more difficult to conduct a well-controlled PA intervention of moderate intensity for any long period of time.
With the exception of evidence on the variation of results by age and sex (i.e., strong evidence of effects for adults and older adults, but limited evidence among youth), the other aims of the umbrella review (dose response and variation by race/ethnicity, socioeconomic status, or weight status) could not be evaluated because of absence of information on these topics in the SRs and MAs. Existing SRs were not written with similar goals as the current paper, so the reviews were not set up to examine whether associations varied by these factors. Also, we did not perform a quantitative MA of the existing reviews, so we are not able to discuss the moderating role of the variables. Unfortunately, SRs are not the best method for estimating dose–response relations or effect modifiers, and many research studies in the field do not systematically evaluate these relations.
One issue across populations included in this review was the lack of agreement across measures of QoL and well-being, which hinders research conclusions of the impact of PA on the outcomes. The most commonly used measures of QoL and well-being are shown in Table 2. Consistent measurement across studies would allow for more direct comparisons across studies and potentially across populations. With the different conceptualizations and measurement, it is possible and, perhaps, likely that slightly different constructs are actually being assessed in spite of the same labels/names of the constructs. As Marsh [104] described, we must be aware of the “jingle” fallacy (that scales with the same name measure the same construct) or its converse, the “jangle” fallacy (that scales with different names measure different constructs). That said, the fact that the conclusions are reasonably consistent across variable measures demonstrates the strength and robustness of the findings.
Table 2.
Commonly used measures of QoL and well-being
| Measures of QoL |
|---|
| Short Form Survey (SF-36 and SF-12) |
| Satisfaction with Life Scale |
| MacNew global score |
| World Health Organization’s (WHO) Quality of Life Questionnaire (WHOQoL) |
| WHO Quality of Life Assessment—Module for Older Adults (WHOQoL-Old) |
| EuroQol Group 5—Dimension Self-Report Questionnaire |
| Life Satisfaction Index—A |
| Disease- or population-specific measures |
| • Diabetes QoL instrument |
| • Alzheimer’s Disease Related Quality of Life |
| • Pediatric Quality of Life Inventory |
| Measures of well-being |
| WHO—Five Well-Being Index (WHO-5) |
| Subjective Vitality Scale |
| Positive and Negative Affect Schedule |
| Lawton’s PGC Morale Scale |
| Psychological Well-Being Scale |
| Warwick–Edinburgh Mental Well-Being Scale |
Improvements in research design will accelerate the explication of the relationship between PA and QoL and well-being across populations. Rigorously designed and long-term experimental studies are needed. Although many current studies are promising, the use of more rigorous designs (e.g., RCTs) and longer intervention periods (e.g., more than 1 year) will bring needed clarity to the question of the impact of PA on QoL and well-being. Enrolling samples of sufficient size and diversity to support intervention moderator analyses (i.e., exploration of subgroup effects in relation to intervention success) along with mediator analyses (i.e., exploration of putative mechanisms through which the interventions operate) will provide useful information for adapting the interventions to optimize uptake among different subgroups, as well as to identify key elements of interventions that are essential to improving QoL. Incorporating diverse population subgroups, including diverse racial/ethnic groups and vulnerable and underrepresented population groups (e.g., lower-income residents and frail older adults), will expand the potential for having a broader public health impact in disseminating this research.
Furthermore, studies should be designed to examine factors that moderate intervention effects, including factors such as characteristics of the activities, person, or disease status. To date, research has focused on the average effects of PA across all individuals and activities. Identifying features of the person (i.e., individual differences) or of specific PA prescriptions that modulate these effect sizes will lead to more targeted and precise behavioral interventions to promote QoL.
Future research within specific populations is also needed. Research is needed to develop a more precise estimate of the effect of PA on QoL in people with dementia, to establish subgroups of optimal responders and nonresponders, and to identify the optimal activity prescription (particularly varying the intensity of physical activities). Subgroups of people with dementia who have been understudied include individuals at different stages of AD progression, individuals with other types of dementia, including, but not limited to, vascular, mixed, frontotemporal, and Lewy body dementia.
Research is also needed to understand how PA interacts with common treatments used by individuals with schizophrenia and effects on disease-specific factors related to QoL. Schizophrenia spectrum disorders include symptoms categorized as positive and negative. Antipsychotic medications are considered to be effective for many positive symptoms but not for negative symptoms and cognitive effects. Existing research suggests that these latter symptom categories may be improved with PA in this population. This research can elucidate how clinical and mental health factors, as well as the modality and setting (institutionalized vs. community or home) of PA, influence QoL outcomes.
Lastly, research is needed to establish the effects of PA on disease- and patient-specific factors related to QoL for individuals with depression and other depressive and bipolar disorders across the spectrum of aging. Most research has focused on the effects of PA on adults with major clinical depression. Knowledge gaps exist regarding the relationships between PA and QoL for individuals classified as having bipolar and related disorders and depressive disorders, including more recently defined conditions such as disruptive mood dysregulation and premenstrual dysphoric disorder [105]. These studies will help to clarify the roles moderators (e.g., patient-, activity-, and disease-status-specific factors) may play in influencing results by type of disorder and how they may interact with medical treatment(s) for these conditions. Future research should also examine the interaction of PA and psychiatric conditions across the lifespan.
In summary, the majority of evidence of the impact of PA on QoL and well-being is positive. That said, there are varying levels of impact on different populations and conditions and not enough evidence to make any conclusive statements of the relationship for some populations and conditions. Although there is a lot of research on the topic of QoL and well-being, more is needed to learn of the intricacies of the constructs and their relationship with PA. Future research is likely to expand upon the work of the PAGAC and could arrive at different conclusions for other populations of the impact of PA on QoL and well-being.
Supplementary Material
Acknowledgments:
The authors did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors for the work contained in this manuscript. The authors reviewed all articles for relevant content, assessed the strength of the evidence, determined conclusions, and wrote the manuscript. The PAGAC committee’s work during the process of conducting the review for the Physical Activity Guidelines was heavily supported by members of the Department of Health and Human Services (DHHS) who provided organizational and infrastructure support for the committee. DHHS also provided funding for a contract that provided staff who conducted the initial search and provided ongoing and infrastructural support related to summarizing the methods for the articles selected for the review. DHHS and contract staff were also involved in editing the manuscript. All authors have seen and approved this version and have no conflicts of interest to report. The conclusions in this article are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation.
Compliance with Ethical Standards
Conflicts of Interest: The authors declare that they have no conflicts of interest.
Authors’ Contributions: D.X.M., S.A., P.M.V., D.E.C., B.B.S. collected data; D.X.M., S.A., P.M.V., D.E.C., K.I.E., C.H., C.M.S., R.M.B., B.B.S., S.J.P., A.C.K., K.E.P. analyzed the data, wrote and edited the manuscript.
Ethical Approval: For this type of study, formal consent is not required. This article does not contain any studies with animals performed by any of the authors.
Informed Consent: This study does not involve human participants and informed consent was, therefore, not required.
References
- 1. International Health Conference. Constitution of the World Health Organization. 1946. Bull World Health Organ. 2002;80(12):983–984. [PMC free article] [PubMed] [Google Scholar]
- 2. Kahneman D. Objective happiness. In: Kahneman D, Diener E, Schwarz N, eds Well-being: The Foundations of Hedonic Psychology. New York, NY: Russell Sage Foundation; 1999:3–25. [Google Scholar]
- 3. Skevington SM, Böhnke JR. How is subjective well-being related to quality of life? Do we need two concepts and both measures? Soc Sci Med. 2018;206:22–30. [DOI] [PubMed] [Google Scholar]
- 4. Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. J Pers Assess. 1985;49(1):71–75. [DOI] [PubMed] [Google Scholar]
- 5. Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 6. Andrews FM, Withey SB. Social Indicators of Well-Being : Americans’ Perceptions of Life Quality. New York, NY: Plenum Press; 1976. [Google Scholar]
- 7. Antunes HK, Stella SG, Santos RF, Bueno OF, de Mello MT. Depression, anxiety and quality of life scores in seniors after an endurance exercise program. Braz J Psychiatry. 2005;27(4):266–271. [DOI] [PubMed] [Google Scholar]
- 8. Morgan WP, O’Connor PJ, Ellickson KA, Bradley PW. Personality structure, mood states, and performance in elite male distance runners. Int J Sport Psychol. 1988;19(4):247–263. [Google Scholar]
- 9. Awick EA, Ehlers DK, Aguiñaga S, Daugherty AM, Kramer AF, McAuley E. Effects of a randomized exercise trial on physical activity, psychological distress and quality of life in older adults. Gen Hosp Psychiatry. 2017;49:44–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Elavsky S, McAuley E, Motl RW, et al. Physical activity enhances long-term quality of life in older adults: Efficacy, esteem, and affective influences. Ann Behav Med. 2005;30(2):138–145. [DOI] [PubMed] [Google Scholar]
- 11. Artese A, Ehley D, Sutin AR, Terracciano A. Personality and actigraphy-measured physical activity in older adults. Psychol Aging. 2017;32(2):131–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. DeNeve KM, Cooper H. The happy personality: A meta-analysis of 137 personality traits and subjective well-being. Psychol Bull. 1998;124(2):197–229. [DOI] [PubMed] [Google Scholar]
- 13. Pescatello LS, Buchner DM, Jakicic JM, et al. ; 2018 Physical Activity Guidelines Advisory Committee Physical activity to prevent and treat hypertension. Med Sci Sports Exerc. 2019;51(6):1314–1323. [DOI] [PubMed] [Google Scholar]
- 14. Kraus VB, Sprow K, Powell KE, et al. ; 2018 Physical Activity Guidelines Advisory Committee Effects of physical activity in knee and hip osteoarthritis: A systematic umbrella review. Med Sci Sports Exerc. 2019;51(6):1324–1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Torres A, Tennant B, Ribeiro-Lucas I, Vaux-Bjerke A, Piercy K, Bloodgood B. Umbrella and systematic review methodology to support the 2018 physical activity guidelines advisory committee. J Phys Act Health. 2018;15(11):805–810. [DOI] [PubMed] [Google Scholar]
- 16. Zubala A, MacGillivray S, Frost H, et al. Promotion of physical activity interventions for community dwelling older adults: A systematic review of reviews. PLoS One. 2017;12(7):e0180902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Morey MC, Sloane R, Pieper CF, et al. Effect of physical activity guidelines on physical function in older adults. J Am Geriatr Soc. 2008;56(10):1873–1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Park SH, Han KS, Kang CB. Effects of exercise programs on depressive symptoms, quality of life, and self-esteem in older people: A systematic review of randomized controlled trials. Appl Nurs Res. 2014;27(4):219–226. [DOI] [PubMed] [Google Scholar]
- 19. Windle G, Hughes D, Linck P, Russell I, Woods B. Is exercise effective in promoting mental well-being in older age? A systematic review. Aging Ment Health. 2010;14(6):652–669. [DOI] [PubMed] [Google Scholar]
- 20. Kelley GA, Kelley KS, Hootman JM, Jones DL. Exercise and health-related quality of life in older community-dwelling adults. J Appl Gerontol. 2009;28(3):369–394. [Google Scholar]
- 21. Jahnke R, Larkey L, Rogers C, Etnier J, Lin F. A comprehensive review of health benefits of Qigong and Tai Chi. Am J Health Promot. 2010;24(6):e1–e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bullo V, Bergamin M, Gobbo S, et al. The effects of Pilates exercise training on physical fitness and wellbeing in the elderly: A systematic review for future exercise prescription. Prev Med. 2015;75:1–11. [DOI] [PubMed] [Google Scholar]
- 23. Bullo V, Gobbo S, Vendramin B, et al. Nordic walking can be incorporated in the exercise prescription to increase aerobic capacity, strength, and quality of life for elderly: A systematic review and meta-analysis. Rejuvenation Res. 2018;21(2):141–161. [DOI] [PubMed] [Google Scholar]
- 24. Tulloch A, Bombell H, Dean C, Tiedemann A. Yoga-based exercise improves health-related quality of life and mental well-being in older people: A systematic review of randomised controlled trials. Age Ageing. 2018;47(4):537–544. [DOI] [PubMed] [Google Scholar]
- 25. Laird KT, Paholpak P, Roman M, Rahi B, Lavretsky H. Mind-body therapies for late-life mental and cognitive health. Curr Psychiatry Rep. 2018;20(1):2. [DOI] [PubMed] [Google Scholar]
- 26. Miller KJ, Adair BS, Pearce AJ, Said CM, Ozanne E, Morris MM. Effectiveness and feasibility of virtual reality and gaming system use at home by older adults for enabling physical activity to improve health-related domains: A systematic review. Age Ageing. 2014;43(2):188–195. [DOI] [PubMed] [Google Scholar]
- 27. Bouaziz W, Vogel T, Schmitt E, Kaltenbach G, Geny B, Lang PO. Health benefits of aerobic training programs in adults aged 70 and over: A systematic review. Arch Gerontol Geriatr. 2017;69:110–127. [DOI] [PubMed] [Google Scholar]
- 28. Raymond MJ, Bramley-Tzerefos RE, Jeffs KJ, Winter A, Holland AE. Systematic review of high-intensity progressive resistance strength training of the lower limb compared with other intensities of strength training in older adults. Arch Phys Med Rehabil. 2013;94(8):1458–1472. [DOI] [PubMed] [Google Scholar]
- 29. Stevens Z, Barlow C, Kendrick D, et al. Effectiveness of general practice-based physical activity promotion for older adults: Systematic review. Prim Health Care Res Dev. 2014;15(2):190–201. [DOI] [PubMed] [Google Scholar]
- 30. Patel NK, Newstead AH, Ferrer RL. The effects of yoga on physical functioning and health related quality of life in older adults: A systematic review and meta-analysis. J Altern Complement Med. 2012;18(10):902–917. [DOI] [PubMed] [Google Scholar]
- 31. Vagetti GC, Barbosa Filho VC, Moreira NB, de Oliveira V, Mazzardo O, de Campos W. Association between physical activity and quality of life in the elderly: A systematic review, 2000–2012. Rev Bras Psiquiatr.. 2014;36(1):76–88. [DOI] [PubMed] [Google Scholar]
- 32. Baxter S, Blank L, Johnson M, et al. Interventions to Promote or Maintain Physical Activity During and After the Transition to Retirement: An Evidence Synthesis. Southampton, UK: NIHR Journals Library; 2016. [PubMed] [Google Scholar]
- 33. Chou CH, Hwang CL, Wu YT. Effect of exercise on physical function, daily living activities, and quality of life in the frail older adults: A meta-analysis. Arch Phys Med Rehabil. 2012;93(2):237–244. [DOI] [PubMed] [Google Scholar]
- 34. Chao YY, Scherer YK, Montgomery CA. Effects of using Nintendo Wii exergames in older adults: A review of the literature. J Aging Health. 2015;27(3):379–402. [DOI] [PubMed] [Google Scholar]
- 35. Clegg AP, Barber SE, Young JB, Forster A, Iliffe SJ. Do home-based exercise interventions improve outcomes for frail older people? Findings from a systematic review. Rev Clin Gerontol. 2012;22(1):68–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Weening-Dijksterhuis E, de Greef MH, Scherder EJ, Slaets JP, van der Schans CP. Frail institutionalized older persons: A comprehensive review on physical exercise, physical fitness, activities of daily living, and quality-of-life. Am J Phys Med Rehabil. 2011;90(2):156–168. [DOI] [PubMed] [Google Scholar]
- 37. Batsis JA, Gill LE, Masutani RK, et al. Weight loss interventions in older adults with obesity: A systematic review of randomized controlled trials since 2005. J Am Geriatr Soc. 2017;65(2):257–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Forsman AK, Nordmyr J, Wahlbeck K. Psychosocial interventions for the promotion of mental health and the prevention of depression among older adults. Health Promot Int.. 2011;26(suppl 1):i85–i107. [DOI] [PubMed] [Google Scholar]
- 39. Baker MK, Atlantis E, Fiatarone Singh MA. Multi-modal exercise programs for older adults. Age Ageing. 2007;36(4):375–381. [DOI] [PubMed] [Google Scholar]
- 40. Bouaziz W, Lang PO, Schmitt E, Kaltenbach G, Geny B, Vogel T. Health benefits of multicomponent training programmes in seniors: A systematic review. Int J Clin Pract. 2016;70(7):520–536. [DOI] [PubMed] [Google Scholar]
- 41. Gillison FB, Skevington SM, Sato A, Standage M, Evangelidou S. The effects of exercise interventions on quality of life in clinical and healthy populations: A meta-analysis. Soc Sci Med. 2009;68(9):1700–1710. [DOI] [PubMed] [Google Scholar]
- 42. Bize R, Johnson JA, Plotnikoff RC. Physical activity level and health-related quality of life in the general adult population: A systematic review. Prev Med. 2007;45(6):401–415. [DOI] [PubMed] [Google Scholar]
- 43. Pucci GC, Rech CR, Fermino RC, Reis RS. Association between physical activity and quality of life in adults. Rev Saude Publica. 2012;46(1):166–179. [DOI] [PubMed] [Google Scholar]
- 44. Campos RR, Dias JM, Pereira LM, et al. Effect of the Pilates method on physical conditioning of healthy subjects: A systematic review and meta-analysis. J Sports Med Phys Fitness. 2016;56(7–8):864–873. [PubMed] [Google Scholar]
- 45. Hendriks T, de Jong J, Cramer H. The effects of yoga on positive mental health among healthy adults: A systematic review and meta-analysis. J Altern Complement Med. 2017;23(7):505–517. [DOI] [PubMed] [Google Scholar]
- 46. Hendriks T. The effects of Sahaja Yoga meditation on mental health: A systematic review. J Complement Integr Med. 2018;15(3). [DOI] [PubMed] [Google Scholar]
- 47. Cramer H, Peng W, Lauche R. Yoga for menopausal symptoms—A systematic review and meta-analysis. Maturitas. 2018;109:13–25. [DOI] [PubMed] [Google Scholar]
- 48. Hanson S, Jones A. Is there evidence that walking groups have health benefits? A systematic review and meta-analysis. Br J Sports Med. 2015;49(11):710–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Meads C, Exley J. A systematic review of group walking in physically healthy people to promote physical activity. Int J Technol Assess Health Care. 2018;34(1):27–37. [DOI] [PubMed] [Google Scholar]
- 50. Wang Y, Shan W, Li Q, Yang N, Shan W. Tai Chi exercise for the quality of life in a perimenopausal women organization: A systematic review. Worldviews Evid Based Nurs. 2017;14(4):294–305. [DOI] [PubMed] [Google Scholar]
- 51. Wiese CW, Kuykendall L, Tay L. Get active? A meta-analysis of leisure-time physical activity and subjective well-being. J Posit Psychol. 2018;13(1):57–66. [Google Scholar]
- 52. Patnode CD, Evans CV, Senger CA, Redmond N, Lin JS. Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults without known cardiovascular disease risk factors: Updated evidence report and systematic review for the US preventive services task force. JAMA. 2017;318(2):175–193. [DOI] [PubMed] [Google Scholar]
- 53. Boberska M, Szczuka Z, Kruk M, et al. Sedentary behaviours and health-related quality of life. A systematic review and meta-analysis. Health Psychol Rev. 2018;12(2):195–210. [DOI] [PubMed] [Google Scholar]
- 54. Huston P, McFarlane B. Health benefits of Tai Chi: What is the evidence? Can Fam Physician. 2016; 62(11):881–890. [PMC free article] [PubMed] [Google Scholar]
- 55. Kelly P, Williamson C, Niven AG, Hunter R, Mutrie N, Richards J. Walking on sunshine: scoping review of the evidence for walking and mental health. Br J Sports Med. 2018;52(12):800–806. [DOI] [PubMed] [Google Scholar]
- 56. Brown HE, Gilson ND, Burton NW, Brown WJ. Does physical activity impact on presenteeism and other indicators of workplace well-being? Sports Med. 2011;41(3):249–262. [DOI] [PubMed] [Google Scholar]
- 57. Orgeta V, Miranda-Castillo C. Does physical activity reduce burden in carers of people with dementia? A literature review. Int J Geriatr Psychiatry. 2014;29(8):771–783. [DOI] [PubMed] [Google Scholar]
- 58. Soga M, Gaston KJ, Yamaura Y. Gardening is beneficial for health: A meta-analysis. Prev Med Rep. 2017;5:92–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Vendramin B, Bergamin M, Gobbo S, et al. Health benefits of Zumba fitness training: A systematic review. PM R. 2016;8(12):1181–1200. [DOI] [PubMed] [Google Scholar]
- 60. Wang F, Man JK, Lee EK, et al. The effects of Qigong on anxiety, depression, and psychological well-being: A systematic review and meta-analysis. Evid Based Complement Alternat Med. 2013;2013:152738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Elkington TJ, Cassar S, Nelson AR, Levinger I. Psychological responses to acute aerobic, resistance, or combined exercise in healthy and overweight individuals: A systematic review. Clin Med Insights Cardiol. 2017;11: doi: 10.1177/1179546817701725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Lambert SD, Duncan LR, Kapellas S, et al. A descriptive systematic review of physical activity interventions for caregivers: Effects on caregivers’ and care recipients’ psychosocial outcomes, physical activity levels, and physical health. Ann Behav Med. 2016;50(6):907–919. [DOI] [PubMed] [Google Scholar]
- 63. Ten Hoor GA, Kok G, Peters GY, Frissen T, Schols AMWJ, Plasqui G. The psychological effects of strength exercises in people who are overweight or obese: A systematic review. Sports Med. 2017;47(10):2069–2081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Abdin S, Welch RK, Byron-Daniel J, Meyrick J. The effectiveness of physical activity interventions in improving well-being across office-based workplace settings: A systematic review. Public Health. 2018;160:70–76. [DOI] [PubMed] [Google Scholar]
- 65. Nestler K, Witzki A, Rohde U, Rüther T, Tofaute KA, Leyk D. Strength training for women as a vehicle for health promotion at work. Dtsch Arztebl Int. 2017;114(26):439–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Brooks SK, Greenberg N. Non-deployment factors affecting psychological wellbeing in military personnel: Literature review. J Ment Health. 2018;27(1):80–90. [DOI] [PubMed] [Google Scholar]
- 67. Caddick N, Smith B. The impact of sport and physical activity on the well-being of combat veterans: A systematic review. Psychol Sport Exerc. 2014;15(1):9–18. [Google Scholar]
- 68. Daley A. Exercise and premenstrual symptomatology: A comprehensive review. J Womens Health (Larchmt). 2009;18(6):895–899. [DOI] [PubMed] [Google Scholar]
- 69. Shepherd-Banigan M, Goldstein KM, Coeytaux RR, et al. Improving vasomotor symptoms; psychological symptoms; and health-related quality of life in peri- or post-menopausal women through yoga: An umbrella systematic review and meta-analysis. Complement Ther Med. 2017;34:156–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Dale H, Brassington L, King K. The impact of healthy lifestyle interventions on mental health and wellbeing: A systematic review. Mental Health Rev J. 2014;19(1):1–26. [Google Scholar]
- 71. Edwards MK, Loprinzi PD. Comparative effects of meditation and exercise on physical and psychosocial health outcomes: A review of randomized controlled trials. Postgrad Med. 2018;130(2):222–228. [DOI] [PubMed] [Google Scholar]
- 72. Suchert V, Hanewinkel R, Isensee B. Sedentary behavior and indicators of mental health in school-aged children and adolescents: A systematic review. Prev Med. 2015;76:48–57. [DOI] [PubMed] [Google Scholar]
- 73. Costigan SA, Barnett L, Plotnikoff RC, Lubans DR. The health indicators associated with screen-based sedentary behavior among adolescent girls: A systematic review. J Adolesc Health. 2013;52(4):382–392. [DOI] [PubMed] [Google Scholar]
- 74. Wu XY, Han LH, Zhang JH, Luo S, Hu JW, Sun K. The influence of physical activity, sedentary behavior on health-related quality of life among the general population of children and adolescents: A systematic review. PLoS One. 2017;12(11):e0187668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Gibson JL, Cornell M, Gill T. A systematic review of research into the impact of loose parts play on children’s cognitive, social and emotional development. School Ment Health. 2017;9(4):295–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Joronen K, Aikasalo A, Suvitie A. Nonphysical effects of exergames on child and adolescent well-being: A comprehensive systematic review. Scand J Caring Sci. 2017;31(3):449–461. [DOI] [PubMed] [Google Scholar]
- 77. Poitras VJ, Gray CE, Borghese MM, et al. Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41(6 (suppl 3)), S197–S239. [DOI] [PubMed] [Google Scholar]
- 78. Lubans DR, Plotnikoff RC, Lubans NJ. Review: A systematic review of the impact of physical activity programmes on social and emotional well-being in at-risk youth. Child Adolesc Ment Health. 2012;17(1):2–13. [DOI] [PubMed] [Google Scholar]
- 79. Mead E, Brown T, Rees K, et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese children from the age of 6 to 11 years. Cochrane Database Syst Rev. 2017;22(6):CD012651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Ojagbemi A, Akin-Ojagbemi N. Exercise and quality of life in dementia: A systematic review and meta-analysis of randomized controlled trials. J Appl Gerontol. 2019;38(1):27–48. [DOI] [PubMed] [Google Scholar]
- 81. Lam FM, Huang MZ, Liao LR, Chung RC, Kwok TC, Pang MY. Physical exercise improves strength, balance, mobility, and endurance in people with cognitive impairment and dementia: A systematic review. J Physiother. 2018;64(1):4–15. [DOI] [PubMed] [Google Scholar]
- 82. Gonçalves AC, Cruz J, Marques A, Demain S, Samuel D. Evaluating physical activity in dementia: A systematic review of outcomes to inform the development of a core outcome set. Age Ageing. 2018;47(1):34–41. [DOI] [PubMed] [Google Scholar]
- 83. McDermott O, Charlesworth G, Hogervorst E, et al. Psychosocial interventions for people with dementia: A synthesis of systematic reviews. Aging Ment Health. 2019;23(4):393–403. [DOI] [PubMed] [Google Scholar]
- 84. Potter R, Ellard D, Rees K, Thorogood M. A systematic review of the effects of physical activity on physical functioning, quality of life and depression in older people with dementia. Int J Geriatr Psychiatry. 2011;26(10):1000–1011. [DOI] [PubMed] [Google Scholar]
- 85. Tavares BB, Moraes H, Deslandes AC, Laks J. Impact of physical exercise on quality of life of older adults with depression or Alzheimer’s disease: a systematic review. Trends Psychiatry Psychother. 2014;36(3):134–139. [DOI] [PubMed] [Google Scholar]
- 86. Cooney GM, Dwan K, Greig CA, et al. Exercise for depression. Cochrane Database Syst Rev. 2013;12(9):CD004366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Cramer H, Lauche R, Klose P, Langhorst J, Dobos G. Yoga for schizophrenia: A systematic review and meta-analysis. BMC Psychiatry. 2013;13:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Bauer IE, Gálvez JF, Hamilton JE, et al. Lifestyle interventions targeting dietary habits and exercise in bipolar disorder: A systematic review. J Psychiatr Res. 2016;74:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Vancampfort D, Vansteelandt K, Scheewe T, et al. Yoga in schizophrenia: A systematic review of randomised controlled trials. Acta Psychiatr Scand. 2012;126(1):12–20. [DOI] [PubMed] [Google Scholar]
- 90. Vera-Garcia E, Mayoral-Cleries F, Vancampfort D, Stubbs B, Cuesta-Vargas AI. A systematic review of the benefits of physical therapy within a multidisciplinary care approach for people with schizophrenia: an update. Psychiatry Res. 2015;229(3):828–839. [DOI] [PubMed] [Google Scholar]
- 91. Dauwan M, Begemann MJ, Heringa SM, Sommer IE. Exercise improves clinical symptoms, quality of life, global functioning, and depression in schizophrenia: A systematic review and meta-analysis. Schizophr Bull. 2016;42(3):588–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Holley J, Crone D, Tyson P, Lovell G. The effects of physical activity on psychological well-being for those with schizophrenia: A systematic review. Br J Clin Psychol. 2011;50(1):84–105. [DOI] [PubMed] [Google Scholar]
- 93. Broderick J, Knowles A, Chadwick J, Vancampfort D. Yoga versus standard care for schizophrenia. Cochrane Database Syst Rev.. 2015;21(10):CD010554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Broderick J, Crumlish N, Waugh A, Vancampfort D. Yoga versus non-standard care for schizophrenia. Cochrane Database Syst Rev. 2017;28(9):CD012052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Broderick J, Vancampfort D. Yoga as part of a package of care versus standard care for schizophrenia. Cochrane Database Syst Rev. 2017;29(9):CD012145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Lee J, Choi M, Yoo Y. A meta-analysis of nonpharmacological interventions for people with Parkinson’s disease. Clin Nurs Res. 2017;26(5):608–631. [DOI] [PubMed] [Google Scholar]
- 97. Song R, Grabowska W, Park M, et al. The impact of Tai Chi and Qigong mind-body exercises on motor and non-motor function and quality of life in Parkinson’s disease: A systematic review and meta-analysis. Parkinsonism Relat Disord. 2017;41:3–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Wu PL, Lee M, Huang TT. Effectiveness of physical activity on patients with depression and Parkinson’s disease: A systematic review. PLoS One. 2017;12(7):e0181515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Terrens AF, Soh SE, Morgan PE. The efficacy and feasibility of aquatic physiotherapy for people with Parkinson’s disease: A systematic review. Disabil Rehabil. 2018;40(24):2847–2856. [DOI] [PubMed] [Google Scholar]
- 100. Ćwiękała-Lewis KJ, Gallek M, Taylor-Piliae RE. The effects of Tai Chi on physical function and well-being among persons with Parkinson’s disease: A systematic review. J Bodyw Mov Ther. 2017;21(2):414–421. [DOI] [PubMed] [Google Scholar]
- 101. Zou L, SasaKi JE, Wang H, Xiao Z, Fang Q, Zhang M. A systematic review and meta-analysis Baduanjin Qigong for health benefits: Randomized controlled trials. Evid Based Complement Alternat Med. 2017;2017:4548706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Domingues RB. Modern postural yoga as a mental health promoting tool: A systematic review. Complement Ther Clin Pract. 2018;31:248–255. [DOI] [PubMed] [Google Scholar]
- 103. Ehlers DK, Salerno EA, Aguiñaga S, McAuley E. Physical activity interventions: effects on well-being outcomes in older adults. In: Diener E, Oishi S, Tay L, eds Handbook of Well-being. Salt Lake City, UT: DEF Publishers; 2018. [Google Scholar]
- 104. Marsh HW. Sport motivation orientations: Beware of jingle-jangle fallacies. J Sport Exerc Psychol. 1994;16(4):365–380. [Google Scholar]
- 105. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.