Abstract
Background/Objective: To assess the differential efficacy between mindfulness-based interventions and cognitive-behavioral Therapy (CBT) on chronic pain across medical conditions involving pain. Method: ProQuest, Science Direct, Google Scholar, Pubmed, and Embase databases were searched to identify randomized clinical trials. Measurements of mindfulness, pain, mood, and further miscellaneous measurements were included. Results: 18 studies met the inclusion criteria (fibromyalgia, n = 5; low back pain, n = 5; headache/migraine, n = 4; non-specific chronic pain, n = 4). In fibromyalgia, mindfulness based stress reduction (MBSR) was superior to the usual care and Fibroqol, in impact and symptoms. In low back pain, MBSR was superior to the usual care, but not to CBT, in physical functionality and pain intensity. There were no studies on differential efficacy between mindfulness and CBT for headache and non-specific chronic pain, but Mindfulness interventions were superior to the usual care in these syndromes. Conclusions: Mindfulness interventions are superior to usual cares in all diagnoses, but it is not possible to conclude their superiority over CBT. Comparisons between mindfulness interventions are scarce, with MBSR being the most studied. In central sensitization syndromes, variables associated with pain tend to improve with treatment. More research is needed to differentiate diagnosis and intervention.
Keywords: Mindfulness, Chronic pain, Cognitive behavioral therapy, Systematic review
Abstract
Introducción/Objetivo: Estudiar la eficacia diferencial entre terapias basadas en mindfulness y terapia cognitivo-conductual (TCC) en síndromes asociados a dolor crónico. Método: ProQuest, Science Direct, Google Scholar, Pubmed y Embase fueron las bases utilizadas para identificar los ensayos clínicos aleatorizados. Los resultados fueron medidas de mindfulness, dolor, estado de ánimo y otras. Resultados: 18 estudios cumplieron criterios de inclusión (fibromialgia, n = 5; lumbalgia, n = 5; cefalea/migraña, n = 4; dolor crónico no especificado, n = 4). En fibromialgia, la terapia basada en mindfulness para la reducción del estrés (MBSR, por sus siglas en inglés) fue superior a tratamiento habitual y Fibroqol en impacto y sintomatología. En lumbalgia, MBSR fue superior a tratamiento habitual, pero no frente a TCC, en funcionalidad física e intensidad del dolor. No se encontraron estudios de eficacia diferencial entre mindfulness y TCC en cefalea y dolor crónico no especificado, pero las intervenciones mindfulness fueron superiores a tratamiento habitual en estos síndromes. Conclusiones: Las intervenciones mindfulness son superiores al tratamiento habitual en todos los diagnósticos, pero no es posible concluir su superioridad sobre TCC. Son escasas las comparaciones entre intervenciones mindfulness, siendo MBSR la más estudiada. En síndromes de sensibilización central tienden a mejorar variables asociadas al dolor. Es necesaria más investigación diferenciando diagnóstico e intervención.
Palabras clave: Mindfulness, Dolor crónico, Terapia cognitivo-conductual, Revisión sistemática
Non-oncological chronic pain is defined as pain that persists for more than six months after the causing lesion in absence of an oncological process, and it could be perpetuated beyond the lesion and even in its absence (Moix & Casado, 2011). Within this field, a set of illnesses are delimited whose course includes the hypersensitization of the somatosensory system, called Central Sensitization Syndrome (CSS; Yunus, 2008). The illnesses whose etiology is CSS, such as fibromyalgia, chronic low back pain or headaches/migraines, show an amplification of the nociceptive signals due to the presence of a constant harmful peripheral stimulus. In developed countries, it is estimated that between 10 and 29% of the adults have chronic pain (Sá et al., 2019), in Europe around 19% (Reid et al., 2011), and in Spain around 15% (Dueñas et al., 2015). The high comorbidity with anxiety-depressive symptoms, sleep disorders, substance use disorder and suicidal ideation (Xu et al., 2020), entails a greater amount of medication, its bad usage and risk of death due to overdose (Owen-Smith et al., 2020). Likewise, the economic cost derived from the rates of unemployment and temporary disability (Leadley et al., 2012) signifies between 2-2.8% of the GDP (Álvarez-Caramés & Navarro-Ribero, 2016).
Within this context, cognitive-behavioral therapy (CBT) has been established as one of the non-pharmacological therapies of choice (Ehde et al., 2014, Morley et al., 2008), including psychoeducation about pain, cognitive restructuring, problem resolution, relaxation and behavioral activation. In the last few years, the perspective of mindfulness has been incorporated, creating diverse approaches such as mindfulness-based cognitive therapy (MBCT; Segal et al., 2012), MBCT for chronic pain (Day, 2017), therapy based on mindfulness for the reduction of stress (MBSR; Kabat-Zinn, 1990, Kabat-Zinn, 2013), and the mindfulness-oriented recovery enhancement (MORE; Garland, 2013). These interventions are focused in the present, trying to increase awareness and acceptance, of the emotional suffering as well as the physical one. Significant improvements have been found in the pain interference, self-efficacy in pain control, acceptance, reduction of catastrophizing and decrease in the daily peaks of pain (Day, 2017), with size effects that are similar to those found in other psychological interventions such as the CBT (Williams et al., 2012).
As for the evidence of the mindfulness interventions, many meta-analyses have revealed the absence of efficacy (McClintock et al., 2018) or insufficient evidence (Bawa et al., 2015), up to the decrease in depression (Ball et al., 2017), and pain, and improved quality of life (Hilton et al., 2016). As for the differential efficacy between mindfulness and CBT, Goldberg et al. (2018) and Khoo et al. (2019) have provided similar information on pain intensity, physical functionality and depression, even after six months, although Goldberg points to the superiority of mindfulness to decrease pain. Although it should be highlighted that Khoo specifically studied MBSR, while Goldber studied various minfulness interventions. However, these meta-analyses are scarce and do not include the variety of formats of mindfulness interventions or medical diagnosis that involve chronic pain. For these reasons, the objective of the present systematic review is the description of the evidence about the efficacy of different interventions based on mindfulness in diverse medical diagnoses that involve chronic pain, and in second place, their comparisons with cognitive-behavioral therapy.
Method
The systematic review was registered with PROSPERO (registration number: 176041) and the PRISMA (http://www.prisma-statement.org/ statement.htm) were followed for its creation, as well as the recommendations by Perestelo-Pérez (2013).
Study selection criteria
Following the criteria of the PICOS format (participants-interventions/comparisons-results-design of studies), the studies selected were published in English and Spanish, aside from complying with the following criteria:
Population: participants older than 18 years of age with non-oncological chronic pain of at least three months.
Interventions/comparisons: studies which researched the efficacy of MBCT, MBSR, mindfulness intervention (MI), mindfulness-based intervention (MBI), MBCT for chronic pain and MORE, as compared to other mindfulness interventions or CBT, and with a control group comparison. The mindfulness programs had to have a group format of at least one hour per session for eight weeks.
Description of the results: following the IMMPACT recommendations, standardized measurement results of pain, physical functionality, emotional functionality (presence of emotional distress) and scores of the participants in overall improvement.
Types of studies: randomized controlled studies.
Sources of information and search strategies
A structured review of the following databases was conducted: ProQuest (PILOTS, PsycArticles, PsicoDoc, PsycInfo), Science Direct, Google Scholar, Pubmed and Embase. The search terms were: Mindfulness Based Cognitive Therapy, Mindfulness Based Stress Reduction, Mindfulness Interventions, Mindfulness Based Cognitive Therapy for Chronic Pain, Cognitive-Behavioural Therapy, Mindfulness-Oriented Recovery Enhancement, Mindfulness Brief Interventions and Chronic Pain, with different combinations and always including the term chronic pain. The search was conducted between September 1st, 2019 and January 31st, 2020. Gray literature was not included.
Study selection process
The inclusion criteria were: (1) subjects older than 18, (2) studies that test the effects of MBCT, MBSR, MI, MBCT for chronic pain, MORE and MBI, alone, in comparison between mindfulness interventions or contrasted with CBT or control group, (3) provide results on pain perception, physical functionality, emotional functionality and/or overall improvement, (4) randomized clinical trials, and (5) in-person interventions. The following were excluded (1) articles published in languages other than English or Spanish, (2) not published, (3) that did not include mindfulness interventions, (4) patients with oncological pain, and (6) remote interventions. Restrictions were not placed on year of publication.
The selection of the studies was performed by two researchers who worked in duplicate independently, following the criteria mentioned. The first filtering was performed through the search of keywords in the title and the abstract. Each researcher extracted the size of the sample, therapies compared, dependent variables, measurement instrument and main results. If there was disagreement between the researchers, the article was revised again until agreement was reached.
Assessment of risk of bias
The tool Cochrane Collaboration tool (Higgins et al., 2019) was utilized to monitor the risk (high, low, or unclear) of bias in the selection of the sample (the selection as well as the allocation), blindness, incomplete data of the results and selective reporting of the data; and any other bias that could be perceived. If the researchers did not reach a consensus, the process was repeated until an agreement was reached.
Analysis and summary of data
The results were analyzed according to therapy and patient diagnosis. Most of the studies had continuous quantitative measurements and the results were presented as standardized differences in means and indicators of the effect size.
Results
Studies selected
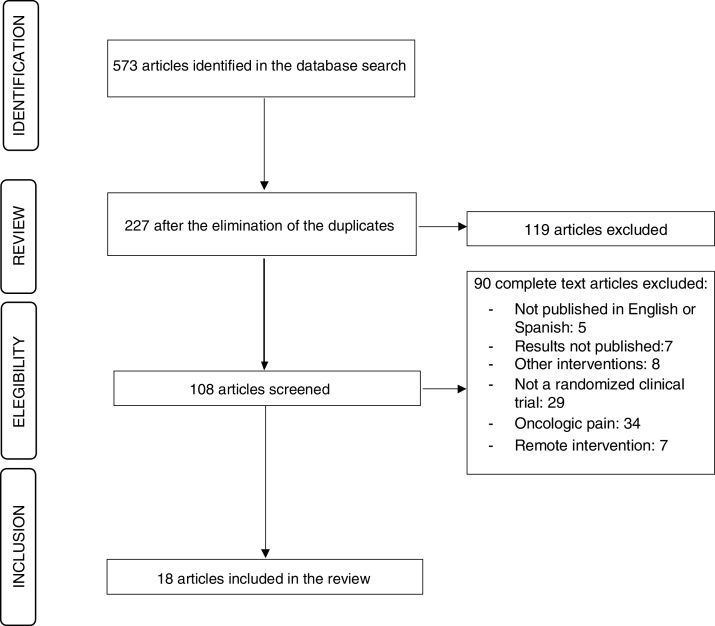
Of the 573 studies initially found, 227 remained after eliminating the duplicates, and 18 complied with all the inclusion criteria. The studies were published between 2008 and 2019 (Figure 1 and Table 1).
Figure 1.
Flow diagram of the selection process.
Table 1.
Description of the studies analyzed (N = 18).
| Authors (year) |
N |
Type of pain | Age | % Women | Conditions | Monitoring (months) |
Measurements |
|||
|---|---|---|---|---|---|---|---|---|---|---|
| Mindfulness | Pain | Mood | Others | |||||||
| Andrés-Rodríguez et al. (2019) | 70 |
Fibromyalgia | 53.36 | 100% | MBSR and medication / Medication |
12 | FFMQ | FIQR | HADS PSS-10 MISCI PCS PIPS |
|
| Bakhshani et al. (2015) | 40 | TH and migraine | 31.05 | 67.50% | MBSR/UC | VAS Number of hours pain/day Frequency of pain per month |
SF36 | |||
| Cash et al. (2015) | 91 |
Fibromyalgia | MBSR/WL | 2 | Frequency of mediation at home. | VAS FIQR |
BDI CTQ-SF PSS |
SSQ FSI |
||
| Chavooshi et al. (2017) | 63 | NSCP | 33 | 30% | ISTDP/ MBSR/ UC |
3 | MAAS | NPRS | DASS-21, ERQ | |
| Cherkin et al. (2016) | 342 |
CLBP | 49.30 | 65.70% | MBSR/CT/ UC |
6.50 and 13 | RDQ VAS PGIC |
PHQ-8 GAD-2 |
SF-12 | |
| Day et al. (2014) | 36 |
86%migraine 11.10% TH 2.80% without classification |
41.60 | 88.85% | MBCT/WL | MAAS CPAQ MBCT-AAQS |
Frequency, duration VAS intensity Distress Medication BPI |
PCS HMSE |
Checking adherence WAI-S | |
| Day et al. (2019) | 69 |
CLBP | 51 | 52% | MM/CT/ MBCT |
3 and 6 | FFMQ CPAQ |
NRS | PROMIS | PHS PGIC |
| De Jong et al. (2018) | 40 |
NSCP | 50.70 | 75% | MBCT/UC | BPI-SF VAS PGIC |
QIDS-C16 HRSD-17 BAI |
SF36 | ||
| La Cour and Petersen (2015) | 109 |
NSCP | 45.68 | 85% | MBSR/WL | 6 | CPAQ | PI SF36 |
HAD SF36 CSQ |
SF36 |
|
Morone et al. (2016) |
141 |
CLBP | 75.50 | 33.70% | MBSR/ Education |
6 | MAAS | RMDQ NRS CPSES |
GDS | SF36 PHS |
| Omidi and Zargar (2015) | 66 |
TH | 33.25 | 79.80% | MBSR/UC | 3 | PSS BSI |
|||
| Parra-Delgado and Latorre-Postigo (2013) | 33 |
Fibromyalgia | 52.90 | MBCT/UC | 3 | MINI FIQ VAS |
BDI | |||
| Pérez-Aranda et al. (2019) | 225 |
Fibromyalgia | 53.27 | 98.93% | MBSR and UC/ FibroQoL and UC/UC |
12 | FFMQ SCS-12 |
FIQR FSDC PGIC PSIC CEQ |
HADS PCS PSS-10 MISCI PIPS |
|
| Reiner et al. (2019) | 67 |
CLBP | 58 | 72% | MI/WL | 3 | BPI-SF TSA-II WST HPT STP |
|||
|
Schmidt et al. (2011) |
177 |
Fibromyalgia | 52.50 | 100% | MBSR/ Active control/WL |
FMI | FIQ VAS PPS |
CES-D STAI | QoL PSQI GCQ |
|
| Turner et al. (2016) | 341 |
CLBP | 49 | 87% | MBSR/CT/ UC |
13 | FFMQ-SF CPAC |
PCS | PSEQ | |
| Wells et al. (2014) | 10 |
Migraine | 45 | 90% | MBSR/UC | 28 days | FFMQ | Frequency HIT-6 MIDAS |
PHQ-9 STAI PSS-10 HMSE |
MSQoL |
| Yeung et al. (2011) | 99 |
NSCP: 85.8% back 83% Joint |
47.9 | MBSR/MPI | 3 and 6 | NRS | POMS STAI CES-D |
SF-12 | ||
Notes: Mindfulness. CPAQ: Chronic Pain Acceptance Questionnaire, MAAS: Mindful Attention and Awareness Scale, MBCT-AAQS: Mindfulness- Based Cognitive Therapy Adherence, Appropriateness, and Quality Scale, FFMQ: Five Facet Mindfulness Questionnaire, FFMQ-SF: Five Facet Mindfulness Questionnaire short form, FMI: Freiburg Mindfulness Inventory, SCS-12: Self-Compassion Scale—short form.
Pain. BPI: Brief Pain Inventory; BPI-SF: Brief Pain Inventory Short Form, BSI: Brief Symptom Inventory, CEP: Coping efficacy for pain CPSES: Chronic Pain Self-Efficacy Scale, FIQ: Fibromyalgia Impact Questionnaire, FIQR: Revised Fibromyalgia Impact Questionnaire, FSI: Fatigue Symptom Inventory, FSDC:Fibromyalgia Survey Diagnostic Criteria, GCQ: Giessen Complaint Questionnaire, HIT-6: Headache Impact Test-6, HPT: Heat Pain Threshold, MIDAS: Migraine Disability Assessment, NPRS: Numerical Pain Rating Scale, NRS: numerical rating scale, PGIC: Patient Global Impression of Change, PIS: Pain Interference Scale, PPS: Pain perception Scale, PSEQ: Pain Self-Efficacy Questionnaire, PSIC: Pain- Specific Impression of Change, RDQ: Roland Disability Questionnaire; RMDQ: Roland and Morris Disability Questionnaire, STP: Supra Threshold Pain, TSA-II: Thermal Sensory Analyzer, VAS: Visual Analogue Scale, WST: Warm Sensation Threshold.
Type of pain. TH: tension headache, NSCP: non-specific chronic pain, CLBP: Chronic low back pain.
Mood. BAI: Beck Anxiety Inventory, BDI: Beck Depression Inventory, CES-D: Centre for Epidemiological Studies-Depression Scale, CEQ: Credibility/Expectancy Questionnaire, CSQ: Coping Strategies Questionnaire, CTQ-SF: Childhood Trauma Questionnaire, Short Form, DASS-21: Depression Anxiety Stress Scale 21, ERQ: Emotion Regulation Questionnaire, GAD-2: Generalized Anxiety Disorder-2, GDS: Geriatric Depression Scale, HADS: Hospital Anxiety and Depression Scale, HMSE: Headache Management Self-Efficacy Scale, HRSD-17: 17-item Hamilton Depression Rating Scale, MINI: Mini International Neuropsychiatric Interview, MISCI: Multidimensional Inventory of Subjective Cognitive Impairment, PCS: Pain catastrophizing Scale, PIPS: The Psychological Inflexibility in Pain Scale, POMS: Profile of Mood States; PCS: The Pain Catastrophizing Scale,PSS-10:Perceived Stress Scale, STAI: State-Trait Anxiety Inventory, QIDS-C16: Quick Inventory Depressive Symptoms, SCID-I: structured clinical interview for DSM-IV axis I.
Others. MSQoL: Migraine Specific Quality of Life Questionnaire, PHC: Physical Health Composite, PHQ-8: Patient Health Questionnaire-8, PHQ-9: Patient Health Questionnaire-9, PROMIS: Patient-Reported Outcomes Measurement Information System, PLC: Quality of Life Profile for the Chronically Ill, PSQI: Pittsburgh Sleep Quality Index, QoL: Quality of Life Profile for the Chronically Ill, SF12: 12-Item Short Form Health Survey, SF36: Health Status Inventory SF36, SSQ: Stanford Sleep Questionnaire, WAI-S: Working Alliance Inventory-short.
Interventions. CT: Cognitive Therapy, FibroQol: psychoeducational multicomponent treatment, ISTDP: intensive short-term dynamic psychotherapy, MBCT: Mindfulness-Based Cognitive Therapy, MI: Mindfulness Intervention, MBSR: Mindfulness-Based Stress Reduction, MM: Mindfulness Meditation, MPI: multidisciplinary pain intervention, UC: usual care, WL: Waiting list.
Description of the characteristics of the study
Designs. Of all the trials, 68.40% used two groups, and the rest (n = 6) were random clinical trials with three groups, which differentiated a second experimental group in which other active treatments were implemented (CBT, brief psychodynamic therapy, FibroQol).
Samples. The samples oscillated between 10 and 342 participants (total = 2.567, M = 100), with an average age of 43.31. Also, 42.10% of the studies had a female representation between 50-90%, and a few had a presence higher than 90% (n = 2) and lower than 50% (n = 3), two trials were only conducted with women, and three did not specify the sex. Eighteen studies grouped the most prevalent pain syndromes: fibromyalgia (n = 5), chronic low back pain (n = 5), headache/migraines (n = 5), and non-specific chronic pain (n = 4).
Mindfulness interventions. Thirteen studies utilized MBSR, four MBCT, and one create its own intervention based on MBSR and MBCT (Reiner et al., 2019). Studies with MORE or MBI were not found.
Control group conditions. The control groups were: usual treatment (medication and clinical control) (n = 9), waiting list (n = 5), medication (n = 1), education (n = 1) and multidisciplinary intervention of pain (explanations of the illness from diverse health professionals) (n = 1).
Results. All the clinical trials collected their results after the end of the intervention, and 73.68% monitored the patients, from 28 days up to 13 months. A great heterogeneity was observed in the types of evaluation instruments, with 23 for mood, 25 for pain, 17 for quality of life, and 7 for mindfulness.
Risk of bias
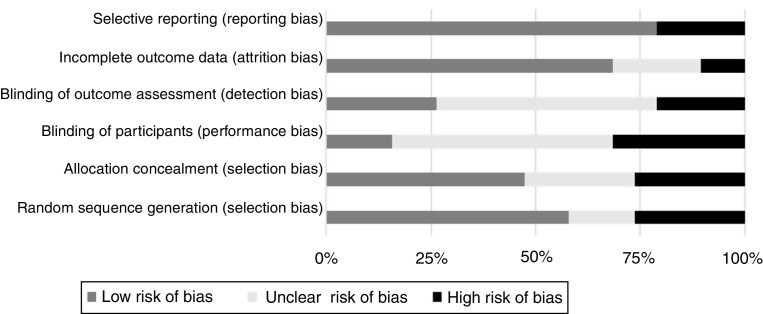
The risk of bias was relatively low for selection (55%), reporting (79%), attrition (70%), and allocation concealment selection (48%). On the contrary, the performance bias was unclear in 47% and the detection bias was unclear in 49%, as shown in Figure 2.
Figure 2.
Analysis of risk of bias in the studies (N = 18) with the Cochrane Collaboration Tool.
Main effects of the interventions
In the content analysis, the articles were grouped according to the main diagnosis of the subjects. The risk of bias was low for fibromyalgia and non-specific chronic pain, high in headache and migraine, and variable in chronic low back pain. Due to the heterogeneity of the scales, special attention was paid to the results obtained with the same instruments to obtain more solid conclusions. The results obtained are presented below.
Fibromyalgia
Only the impact and symptoms of pain had comparable measurements (FIQR, in four out of five studies), with the superiority of MBSR observed as compared to the usual treatment, and in two trials as compared to a multicomponent psychoeducational treatment (FibroQol/active control), with large size effects (impact: d between 0.80 and 1.11; symptomology: d between 0.46 and 1.04), and maintained all year. In the rest of the variables, the superiority of the MBSR was also evidenced as compared to the usual care and multicomponent treatments, although in these measurements there was a greater heterogeneity of instruments. However, in mindfulness skills, MBSR was shown to be superior to the usual care, but not as compared to multicomponent treatments. As for MBCT, a study informed about superiority as compared to the habitual depression treatment, but information on monitoring was not provided (Table 2).
Table 2.
Content analysis of clinical trials for fibromyalgia (N = 5).
| Authors (year) | Andrés-Rodríguez et al. (2019) |
Pérez-Aranda et al. (2019) |
Cash et al. (2015) |
Schmidt et al. (2011) |
Parra-Delgado and Latorre-Postigo (2013) | |||
|---|---|---|---|---|---|---|---|---|
| Treatment | MBSR/TH | MBSR/ FibroQol | MBSR/UC | FibroQol/UC | MBSR/WL | MBSR and AC/ WL | MBSR/AC | MBCT/UC |
| HH Mindfulness | ↑ (d = 2.01)*** | Observing: ↑ (d = 0.66)** 12M: w/sd Awareness: w/sd Nonjudging: ↑ (d = 0.57)** 12M: w/sd Describing: w/sd 12M: ↑ (d = 0.50)*** Non-reactivity: w/sd Self-compassion: ↑ (d = 0.47)* 12M: w/sd |
Observing: ↑ (d = 0.79)*** 12M: ↑ (d = 0.84)*** Awareness: ↑ (d = 0.66)** 12M: ↑ (d = 0.53)* Nonjudging: ↑ (d = 0.89)*** 12M: ↑ (d = 0.66)** Describing: w/sd 12M: ↑ (d = 0.66)** Non-reactivity: w/sd 12M: w/sd Self-compassion: ↑ (d = 0.66)** 12M: w/sd |
Observing: w/sd 12M: ↑ (d = 0.63)** Awareness: ↑ (d = 0.46)* 12M: ↑ (d = 0.62)* Nonjudging: w/sd 12M: ↑ (d = 0.47)* Describing: w/sd 12M: w/sd Non-reactivity: w/sd 12M: w/sd Self-compassion: w/sd 12M: w/sd |
w/sd | ↑ * | ||
| Pain and impact | Impact fibromyalgia: ↓ (d = 0.99)** | Impact fibromyalgia: ↓(d = 0.86)*** 12M: w/sd Symptoms fibromyalgia: w/sd 12M: ↓(d = 0.82)*** |
Impact fibromyalgia: ↓ (d = 1.11)*** 12M: ↓ (d = 0.80)*** Symptoms fibromyalgia: ↓ (d = 0.97)*** 12M: ↓(d = 1.04)*** |
Impact fibromyalgia: w/sd 12M: w/sd Symptoms fibromyalgia: ↓ (d = .54)* 12M: w/sd |
Symptoms fibromyalgia: ↓ (IOT: d = 0.46**, BP: d = 0.58**) Physical functioning: w/sd (IOT and BP) Intensity: w/sd (IOT and BP) |
w/sd | w/sd | Impact: w/sd Pain: w/sd |
| Cognitive Functioning | Cognitive skills: ↑ (d = 0.97)* Catastrophizing: ↓ (d = 0.74)* Inflexibility: w/sd |
Cognitive skills: ↑ (d = 0.95)*** 12M: w/sd Catastrophizing: ↓ (d = 0.65)* 12M: ↓ (d = 0.58)* Inflexibility: ↓ (d = 0.49)* 12M: ↓ (d = 0.47)* |
Cognitive skills: ↑ (d = 0.86)*** 12M: ↑ (d = 0.99)*** Catastrophizing: ↓ (d = .84)*** 12M: ↓ (d = 0.73)** Psychological inflexibility: ↓ (d = 0.67)*** 12M:↓ (d = 0.88)*** |
Cognitive skills: w/sd 12M: ↑ (d = 0.65)* Catastrophizing: w/sd 12M: w/sd Psychological inflexibility: w/sd 12M: w/sd |
||||
| Anxiety | w/sd |
↓ (d = 0.49)* 12M: w/sd |
↓ (d = 0.84)*** 12M: ↓ (d = 0.67)* |
w/sd 12M: ↓ (d = 0.57)* |
↓* | w/sd | ||
| Depression | ↓ (d = 1.04)** | w/sd | w/sd | ↓ * | ||||
| Stress | ↓ (d = 1.01)** | ↓ (d = 0.77)*** 12M: w/sd |
↓ (d = 1.07)*** 12M: ↓ (d = 0.58)* |
w/sd 12M: w/sd |
↓ (IOT: d = 0.48***, BP: d = 0.69***) | |||
| Quality of life | Sleep disorders: ↓ (IOT: d = 0.25*, BP: w/sd) Fatigue: ↓(IOT: d = 0.47**, BP: d = 0.73*) |
w/sd | w/sd | |||||
Note: Treatments = AC: active control, FibroQol: psychoeducational multicomponent treatment, MBCT: Mindfulness-Based Cognitive Therapy, MBSR: Mindfulness-Based Stress Reduction, UC: Usual care, WL: Waiting list. Level of significance = *.05 **.01 ***.001, w/sd: without significant differences. Monitoring = 12M: 12 months. Type of analysis = IoT: intention of treatment (analysis of the results including abandonments), BP: by protocol (analysis of results only with subjects who finish the protocol). Statistics = p η2: partial η2, d: Cohen’s d.
Chronic low back pain
It is observed that there is no coincidence between the measurement instruments in any of the variables between the studies, making difficult the extraction of consistent conclusions. In spite of this, three studies provided information on the superiority of the MBSR as compared to the usual care with maintenance performed after a year due to discomforts, and intensity of pain, disability and catastrophizing, while the psychological well-being and self-efficacy showed post-treatment differences which were attenuated with time. Differences were not observed between both treatments in mindfulness skills.
Three trials compared MBSR with active control (CBT, n = 2; Health Education Program, HEP, n = 1), measuring the same variables, but with different instruments and the results found being divergent as for their meaning and maintenance. It is underlined that one studied provided information on the start of pain equally improved between MBSR and CBT as compared to the usual care in the long term (1 year), but not in the post-treatment measurement. On the other hand, another trial informed on the superiority of the CBT as compared to MBSR for the improvement of depression in the short term.
A study on MBCT and another on MBI were found but both had a high risk of bias in their results and none of them provided information about monitoring (Table 3).
Table 3.
Content analysis of clinical trials for chronic low back pain (N = 5).
| Authors (year) |
Cherkin et al. (2016) |
Morone et al. (2016) |
Turner et al. (2016) |
Day et al. (2019) |
Reiner et al. (2019) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Treatment | MBSR/ UC |
MBSR/ CBT | CBT / UC |
MBSR/PES | MBSR/ UC | MBSR/ CBT | CBT / UC | MBCT/ CT |
MM/CT | MBCT/MM | MBI/WL |
| HH Mindfulness | w/sd | Observing: w/sd Awareness: w/sd Nonjudging: ↑* 6M: w/sd 12M: w/sd Non-reactivity: ↑* 6M: w/sd 12M: w/sd Acceptance(total): w/sd Activity engagement: w/sd Pain willingness: w/sd 6M: w/sd 12M: ↑* |
Observing: w/sd Awareness: w/sd Nonjudging: ↑* 6M: w/sd 12M: w/sd Non-reactivity: w/sd Acceptance(total): w/sd Activity engagement: w/sd Pain willingness : w/sd |
Observing: w/sd Awareness: w/sd Nonjudging: w/sd Non-reactivity: ↑* 6M: w/sd 12M: w/sd Acceptance(total): w/sd Activity engagement: w/sd Pain willingness w/sd 6M: w/sd 12M: ↑* |
|||||||
| Pain | Discomfort due to pain: ↓* 6M: ↓* 12M: ↓* Intensity: ↓* 6M: ↓* 12M: ↓* |
Discomfort due to pain: w/sd Intensity: w/sd |
Discomfort due to pain: ↓* 6M: ↓* 12M: ↓* Intensity:↓* 6M: ↓* |
Mean pain: w/sd Current pain: ↓ (d = -0,21)* 6M: ↓ (d = -0.33)* Severe pain: ↓ (d = -0,08)* 6M: ↓ (d = -0.19)* |
Interference: w/sd Intensity: w/sd |
Interference: w/sd Intensity: w/sd |
Interference ↓** Intensity: w/sd |
Severity: ↓(np2 = 0.12)* Interference: ↓ (np2 = 0.11)* Supraliminar pain: ↓ (np2 = 0.12)* |
|||
| Disability | ↓ * 6M: ↓* 12M: ↓* |
w/sd | ↓ * 6M: ↓* 12M: ↓* |
↓ (d = -0.23)* 6M: ↓ (d = -0.08)** |
|||||||
| Anxiety | w/sd | w/sd 6M: ↓* 12M: w/sd |
↓* 6M: ↓* 12M: w/sd |
||||||||
| Depression | ↓ * 6M: w/sd 12M: w/sd |
↓* (TCC > MBSR) 6M: w/sd 12M: w/sd |
↓ * 6M: ↓* 12M: w/sd |
w/sd | w/sd | Depression: ↑** |
|||||
| Self-efficacy | Coping: ↑ (d = 0.32)** 6M: ↑ (d = 0.15)** Functional self-efficacy: ↑ (d = 0.17)* 6M: ↑ (d = 0.03)* Pain self-efficacy: ↑ (d = 0.51)** 6M: ↑ (d = 0.017)** |
↑* 6M: w/sd 12M: w/sd |
w/sd | ↑* 6M: w/sd 12M: w/sd |
|||||||
| Quality of life | Physical health: w/sd Mental health: ↑* 6M: w/sd 12M: w/sd |
Physical health: w/sd Mental health: w/sd |
Physical health: w/sd Mental health: ↑* 6M: ↑* 12M: w/sd |
Global health: ↑ (d = 0.18)* 6M: ↑ (d = 0.02)* Physical health: ↑ (d = 0.18)* 6M: ↓ (d = -0.01)* |
w/sd | Physical functioning↑** | Physical functioning↑** | ||||
| Catastrophizing | - | - | - | ↓ (d = -0.19)* 6M: ↑ (d = 0.05)* |
↓* 6M: w/sd 12M: ↓* |
TCC: ↓* 6M: w/sd 12M: w/sd |
w/sd 6M: w/sd 12M: ↓* |
||||
Note: Treatments = CBT: Cognitive-Behavioral Therapy, CT: Cognitive Therapy, MBCT: Mindfulness-Based Cognitive Therapy, MBSR: Mindfulness-Based Stress Reduction, MM: Mindfulness Meditation, HEP: Health Education Program, UC: Usual care, WL: Waiting list. Level of significance = *.05 **.01 ***.001, w/sd: without significant differences. Monitoring = 6M: 6 months, 12M: 12 months. Statistics = p η2: partial η2 l, d: Cohen’s d.
Headache and migraine
The intensity (VAS) and self-efficacy in the control of pain (HMSE) were only variables where the instruments in both studies coincided, and each of them implemented a different type of mindfulness intervention (MBSR and MBCT). Thus, self-efficacy in the control of pain improved pain in the short term in both interventions as compared to the usual care. As for pain intensity, MBSR was shown to be superior to MBCT as compared to the usual care, but both studies were high risk, and these differences should be taken with caution. As for the rest of the variables, the three MBSR studies showed a trend of its superiority, as compared to the usual care, although the results were not very comparable between them and came from studies with diverse methodological quality (Table 4).
Table 4.
Content analysis of clinical trials for headache/migraine (N = 4).
| Authors (year) | Omidi and Zargar (2015) | Bakhshani et al. (2015) | Wells et al. (2014) | Day et al. (2014) |
|---|---|---|---|---|
| Treatment | MBSR/UC | MBSR/UC | MBSR/UC | MBCT/TD |
| HH Mindfulness | - | - | Mindfulness Attitude: ↑ * 28 days* |
Mindfulness Attitude:w/sd Acceptance: ↑ (IOT, d = 0.82*; BP, d = 1.22*) |
| Pain and impact | Symptoms:↓*** 3M: w/sd |
Intensity:↓ (η2 = 0,68) *** Dolor corporal: ↓ (pη2 = 0.34) ** |
Duration↓* Impact↓* 28 days* Self-efficacy↓ * 28 days: w/sd |
Control of headache: ↑ (IOT, d = 0.82*; BP, d = 1.65*). Interference of pain: ↓ (BP: d = -1.29)** Frequency: w/sd Duration: w/sd Intensity of peak and the mean: w/sd Distress: w/sd Self-efficacy: ↑ (IOT, d = 0.82*; BP, d = 1.65*) |
| Cognitive Functioning | - | - | - | Catastrophizing ↓: (IOT: w/sd, BP: d = -0.94**) |
| Anxiety | - | - | w/sd | - |
| Depression | - | - | w/sd | - |
| Stress | Stress perceived↓ *** 3M: w/sd |
w/sd | - | |
| Quality of life | - | Physical health: ↑ (pη2 = 0.18)* Mental health:↑ (pη2 = 0.33)** Global health: ↑ (pη2 = 0.28)** Energy and vitality: ↑ (pη2 = 0.34)** Emotional health: ↑ (pη2 = 0.60)*** |
Disability↓* 28 days: w/sd Quality of life: w/sd |
- |
| Others | - | w/sd in Physical functioning, limitations of role due to emotional and social functioning problems. | - | Good viability of the MBCT (79%), significantly less tolerance ** |
Note: Treatments = TD: treatment delayed, MBCT: Mindfulness-Based Cognitive Therapy, MBSR: Mindfulness-Based Stress Reduction, UC: Usual care. Level of significance = *.05 **.01 ***.001, w/sd: without significant differences. Monitoring = 3 M: 3 months, 6 M: 6 months, 12M: 12 months. Statistics = p η2: partial η2, d: Cohen’s d.
Non-specific chronic pain
The quality of life was measured in two trials with SF-36, and one trial used SF-12. On the MBSR intervention, just as in one of the trials with MBCT, an increase in vitality and mental health was reported in the short term as compared to the usual care. A divergent study with MBCT as compared to a multidisciplinary intervention for pain (MPI) was not taken into consideration due to its high risk (Yeung et al., 2011).
As for pain, this was measured with analog scales (NRS and NPRS) for a study with MBSR and another with MBCT, and both were assessed as high risk. For this, although the results were contradictory, it was not considered that they demonstrated a differential efficacy between therapies.
Lastly, an intensive short-term dynamic psychotherapy (ISTDP) trial was applied (Chavooshi et al., 2017), for the evaluation of a group intervention (MBSR) as compared to an individual one, so that the results are not comparable (Table 5).
Table 5.
Analysis of the results from clinical trials on non-specific chronic pain (N = 4).
| Authors (year) |
Chavooshi et al. (2017) |
La Cour and Petersen (2015) | Yeung et al. (2011) | De Jong et al. (2018) | ||
|---|---|---|---|---|---|---|
| Treatment | MBSR/ISTDP | MBSR/TH | ISTDP/TH | MBSR/LE | MBCT/MPI | MBCT/TH |
| HH mindfulness | Not reported | Mindfulness Attitude↑*** | Mindfulness Attitude ↑*** | Acceptance: ↑ (d = 0.60)** 6M: ↑** Engagement: ↑ (d = 0.71)*** 6M: ↑** Pain willingness : w/sd 6M: ↑** |
||
| Pain and impact | Intensity in ISTDP:↓ (d = -1.85) ** 3M: (d = -1.40) ** |
Intensity: ↓ (d = -0.80)*** 3M: (d = -0.67) *** |
Intensity: ↓ (d = -1.95) *** 3M: (d = 1.70) *** |
Intensity: w/sd (BPI and SF-36): w/sd 6M: ↓** (SF-36) Control: ↑ (d = 0.55)*** 6M: ↑** Minimization: w/sd |
Intensity: w/sd | Intensity: w/sd |
| Anxiety | Not reported | ↓ *** | ↓ *** | ↓ (d = 0.50)* 6M: w/sd | w/sd | w/sd |
| Depression | Not reported | ↓ *** | ↓ *** | ↓ (d = 0.37)* 6M: ↓** | w/sd | ↓ (IOT: d = w/sd, BP: d = 1.6) *** |
| Stress | Not reported | ↓ *** | ↓ *** | Distress: MPI ↓ (WS = 3.98) ** | ||
| Quality of life | Vitality: ↑ (d = 0.39) * 6M: ** Quality of life: ↑ (d = 0.21)* 6M: ↑** Psychological well-being: ↑ (d = 0.43)* 6M: w/sd Mental health: ↑ (d = 0.48)* 6M: w/sd Physical health: w/sd 6M: ↑** Physical functioning: w/sd 6M: ↑** |
Mental health: w/sd Physical health: w/sd Vigorous activity: ↑ (WS = 4.05)* 3 and 6 M: w/sd |
Vitality: ↑ (IOT: d = 0.50**; BP: d = 0.68**) Quality of life: w/sd (IOT and BP) Psychological well-being: w/sd (IOT and BP) Mental health: ↑ (IOT: d = 0.57**; BP: d = 0.83**) Physical health: w/sd (IOT and BP) Physical functioning: w/sd (IOT and BP) Subjective improvement: ↑ (IOT and BP) ** |
|||
| Others | Emotional regulation ↑*** | Emotional regulation ↑*** | Catastrophizing: w/sd | |||
Note: Treatments = ISTDP: Intensive short-term dynamic psychotherapy, MBCT: Mindfulness-Based Cognitive Therapy, MBSR: Mindfulness-Based Stress Reduction, MPI: multidisciplinary pain intervention, UC: Usual care, WL: Waiting list. Level of significance = *.05 **.01 ***.001, w/sd: without significant differences. Monitoring = 3 M: 3 months, 6 M: 6 months. Statistics = p η2: partial η2, d: Cohen’s d, WS: Wald statistic.
Discussion
In fibromyalgia, more support has been found for MBSR, which has improved a greater number of variables as compared to Fibroqol and usual care, in agreement with previous reviews (Crowe et al., 2015). More specifically, in this review we found more solid evidence for MBSR in the reduction of the impact and symptomatology of fibromyalgia, with maintenance after a year. These results contradict those found by Lauche et al. (2013), although these researchers included studies that were not randomized clinical trials in their study, and in the present review, we have included three studies after 2013 with provide new evidence.
In chronic low back pain, the results of this review are compromised by the heterogeneity of the scales. In agreement with Chou et al. (2017) and Anheyer et al. (2017), we found that MBSR has superior effects in diverse variables as compared to the usual care, but its effects are mainly in the short term, and its differential efficacy required more research. Particularly, our review coincides with that from Anheyer et al. (2017), in pointing out the improvement of physical functionality and the intensity of pain with MBSR as compared to the usual care.
On the other hand, when considering chronic low back pain and migraine, the results are limited, with studies with a high risk and lack of comparison with CBT. Fang et al. (2018) reported on improvements in different variable, for MBSR as well as MBCT, but in our review, we could not make these assertions due to heterogeneity indicated, except for self-efficacy in the control of pain, for which both mindfulness interventions had the same efficacy in the short term.
As for non-specific chronic pain, a comparison with CBT was not found, and when compared with the usual care, the superiority of MBSR and MBCT was observed for improving vitality and mental health. As for the decrease in pain, it could not be concluded that there was a differential efficacy between both mindfulness interventions, due to the methodological deficiencies of the studies that evaluate this variable. It is difficult to extract clear trends from the previous reviews which could be used to compare the results (Ball et al., 2017, Bawa et al., 2015, Goldberg et al., 2018, Hilton et al., 2016, Khoo et al., 2019, McClintock et al., 2018, Perestelo-Perez et al., 2017), due to the heteregeneity of the diagnoses that have an influence. This problem has been tried to be solved in the present review by differentiating between syndromes. Thus, this is reason why studies that coincided with our results on non-specific chronic pain were not found.
In response to the objectives set in this review, it can be concluded that the mindfulness interventions produce improvements in a greater number of variables as compared to the usual care in all the group diagnoses, with variable maintenance, and paradoxically, the improvement is not always found in the mindfulness variables. Likewise, a greater evidence was observed for the MBSR intervention format, while MBCT was less studied, with trials with a smaller number of variables and habitually of high risk. The trials on the differential efficacy between mindfulness interventions are practically non-existent, thus it is a promising field of study.
As for the differential efficacy of mindfulness as compared to CBT, trials were only found for chronic low back pain, but were not comparable between themselves, and did not provide a clear conclusion about the superiority of any treatment. For fibromyalgia, although comparisons were not found with CBT, a superiority was found as compared to active control. On their part, for headaches and chronic pain, comparisons with CBT were not found either. Therefore, further research is needed to clarify the differential efficacy between Mindfulness and CBT interventions for any of the diagnoses.
We believe that the most interesting finding from this review is that the diagnosis that form part of CSS (fibromyalgia, chronic low back pain and headache) shared an improvement in the symptomatology related to pain (impact and symptoms of fibromyalgia, intensity of pain and physical functioning in chronic low back pain, and self-efficacy in the management of headaches), while the studies on non-specific chronic pain reported a reduction in less specific symptoms such as vitality and mental health. We set for the possibility that the mindfulness interventions are more efficient in the diagnoses that involve a CSS etiology. It is also possible that the category of non-specific chronic pain encompasses heterogeneous diagnoses that make difficult the finding of more clear trends.
Lastly, it should be considered that these conclusions are subject to limitations due to the heterogeneity of the evaluation instruments, sample and therapies, as well as the reduced number of trials per diagnosis. However, the present review has itemized what is normally treated as a set, and ultimately points out the need to differentiate according to syndromes to arrive at more precise conclusions.
References
- Álvarez-Caramés Á.M., Navarro-Ribero M. Costes del tratamiento del dolor versus su no tratamiento. Aproximación a la realidad de Portugal y España. Dor. 2016;24:1–9. [Google Scholar]
- *Andrés-Rodríguez L., Borràs X., Feliu-Soler A., Pérez-Aranda A., Rozadilla-Sacanell A., Montero-Marin J., Maes M., Luciano J.V. Immune-inflammatory pathways and clinical changes in fibromyalgia patients treated with Mindfulness-Based Stress Reduction (MBSR): A randomized, controlled clinical trial. Brain, Behavior, and Immunity. 2019;80:109–119. doi: 10.1016/j.bbi.2019.02.030. [DOI] [PubMed] [Google Scholar]
- Anheyer D., Haller H., Barth J., Lauche R., Dobos G., Cramer H. Mindfulness-based stress reduction for treating low back pain: A systematic review and meta-analysis. Annals of Internal Medicine. 2017;166:799–807. doi: 10.7326/M16-1997. [DOI] [PubMed] [Google Scholar]
- *Bakhshani N.M., Amirani A., Amirifard H., Shahrakipoor M. The effectiveness of mindfulness-based stress reduction on perceived pain intensity and quality of life in patients with chronic headache. Global Journal of Health Science. 2015;8:142–151. doi: 10.5539/gjhs.v8n4p142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball E.F., Nur Shafina Sharizan Muhammad E., Franklin G., Rogozińska E. Does mindfulness meditation improve chronic pain? A systematic review. Current Opinion in Obstetrics and Gynecology. 2017;29:359–366. doi: 10.1097/GCO.0000000000000417. [DOI] [PubMed] [Google Scholar]
- Bawa F.L.M., Mercer S.W., Atherton R.J., Clague F., Keen A., Scott N.W., Bond C.M. Does mindfulness improve outcomes in patients with chronic pain? Systematic review and meta-analysis. British Journal of General Practice. 2015;65:387–400. doi: 10.3399/bjgp15X685297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Cash E., Salmon P., Weissbecker I., Rebholz N., Bayley-Veloso R., Zimmaro L., Floyd A., Dedert E., Sephton S. U. S. Department of Veterans Affairs Women: Results of a Randomized Clinical Trial. Annals of Behavioral Medicine. 2015;49:319–330. doi: 10.1007/s12160-014-9665-0.Mindfulness. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Chavooshi B., Saberi M., Tavallaie S.A., Sahraei H. Psychotherapy for medically unexplained pain: a randomized clinical trial comparing intensive short-term dynamic psychotherapy and cognitive-behavior therapy. Psychosomatic. 2017;85:123–125. doi: 10.1016/j.psym.2017.01.003. [DOI] [PubMed] [Google Scholar]
- *Cherkin D.C., Sherman K.J., Balderson B.H., Cook A.J., Anderson M.L., Hawkes R.J., Hansen K.E., Turner J.A. Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: A randomized clinical trial. JAMA - Journal of the American Medical Association. 2016;315:1240–1249. doi: 10.1001/jama.2016.2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou R., Deyo R., Friedly J., Skelly A., Hashimoto R., Weimer M., Fu R., Dana T., Kraegel P., Griffin J., Grusing S., Brodt E.D. Nonpharmacologic therapies for low back pain: a systematic review for an american college of physicians clinical practice guideline. Annals of Internal Medicine. 2017;166:493. doi: 10.7326/m16-2459. [DOI] [PubMed] [Google Scholar]
- Crowe M., Jordan J., Burrell B., Jones V., Gillon D., Harris S. Mindfulness-based stress reduction for long-term physical conditions: A systematic review. Australian and New Zealand Journal of Psychiatry. 2015;50:21–32. doi: 10.1177/0004867415607984. [DOI] [PubMed] [Google Scholar]
- Day M. John Wiley and Sons; 2017. Mindfulness-Based Cognitive Therapy for Chronic Pain. [Google Scholar]
- *Day M.A., Thorn B.E., Rubin N.J. Mindfulness-based cognitive therapy for the treatment of headache pain: A mixed-methods analysis comparing treatment responders and treatment non-responders. Complementary Therapies in Medicine. 2014;22:278–285. doi: 10.1016/j.ctim.2013.12.018. [DOI] [PubMed] [Google Scholar]
- *Day M.A., Ward L.C., Ehde D.M., Thorn B.E., Burns J., Barnier A., Mattingley J.B., Jensen M.P. A pilot randomized controlled trial comparing mindfulness meditation, cognitive therapy, and mindfulness-based cognitive therapy for chronic low back pain. Pain Medicine (Malden, Mass.) 2019;20:2134–2148. doi: 10.1093/pm/pny273. [DOI] [PubMed] [Google Scholar]
- *De Jong M., Peeters F., Gard T., Ashih H., Doorley J., Walker R., Rhoades L., Kulich R.J., Kueppenbender K.D., Alpert J.D., Hoge E.A., Britton W.B., Lazar S.W., Fava M., Mischoulon D. A randomized controlled pilot study on mindfulness-based cognitive therapy for unipolar depression in patients with chronic pain. Journal of Clinical Psychiatry. 2018;79:26–34. doi: 10.4088/JCP.15m10160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dueñas M., Salazar A., Ojeda B., Fernández-Palacín F., Micó J.A., Torres L.M., Failde I. A nationwide study of chronic pain prevalence in the general spanish population: identifying clinical subgroups through cluster analysis. Pain Medicine (United States) 2015;16:811–822. doi: 10.1111/pme.12640. [DOI] [PubMed] [Google Scholar]
- Ehde D.M., Dillworth T.M., Turner J.A. Cognitive-behavioral therapy for individuals with chronic pain: Efficacy, innovations, and directions for research. American Psychologist. 2014;69:153–166. doi: 10.1037/a0035747. [DOI] [PubMed] [Google Scholar]
- Fang X.-M., Gu Q., Hou J.-C. Mindfulness Meditation for Primary Headache Pain: A Meta-Analysis. Chinese Medical Journal. 2018;131:829. doi: 10.4103/0366-6999.228242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland E.L. NASW Press; 2013. Mindfulness-Oriented Recovery Enhancement for addiction, stress, and pain. [Google Scholar]
- Goldberg S.B., Tucker R.P., Greene P.A., Davidson R.J., Wampold B.E., Kearney D.J., Simpson T.L. Mindfulness-based interventions for psychiatric disorders: A systematic review and meta-analysis. Clinical Psychology Review. 2018;59:52–60. doi: 10.1016/j.cpr.2017.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins J.P., Savović J., Page M.J., Elbers R.G., Sterne J.A. Assessing risk of bias in a randomized trial. In: Higgins J.P.T., Thomas J., Chandler J., Cumpston M., Li T., Page M.J., Welch V.A., editors. Cochrane Handbook for Systematic Reviews of Interventions. John Wiley & Sons; 2019. pp. 205–228. [Google Scholar]
- Hilton L., Hempel S., Ewing B.A., Apaydin E., Xenakis L., Newberry S., Colaiaco B., Maher A.R., Shanman R.M., Sorbero M.E., Maglione M.A. Mindfulness meditation for chronic pain: systematic review and meta-analysis. Annals of Behavioral Medicine. 2016;51:199–213. doi: 10.1007/s12160-016-9844-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J. Delacourt; 1990. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain and illness. [Google Scholar]
- Kabat-Zinn J. Hachette; 2013. Full Catastrophe Living. [Google Scholar]
- Khoo E.L., Small R., Cheng W., Hatchard T., Glynn B., Rice D.B., Skidmore B., Kenny S., Hutton B., Poulin P.A. Comparative evaluation of group-based mindfulness-based stress reduction and cognitive behavioural therapy for the treatment and management of chronic pain: A systematic review and network meta-analysis. Evidence-Based Mental Health. 2019;22:26–35. doi: 10.1136/ebmental-2018-300062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *La Cour P., Petersen M. Effects of mindfulness meditation on chronic pain: a randomized controlled trial. Pain Medicine (United States) 2015;16:641–652. doi: 10.1111/pme.12605. [DOI] [PubMed] [Google Scholar]
- Lauche R., Cramer H., Dobos G., Langhorst J., Schmidt S. A systematic review and meta-analysis of mindfulness-based stress reduction for the fibromyalgia syndrome. Journal of Psychosomatic Research. 2013;75:500–510. doi: 10.1016/j.jpsychores.2013.10.010. [DOI] [PubMed] [Google Scholar]
- Leadley R.M., Armstrong N., Lee Y.C., Allen A., Kleijnen J. Chronic diseases in the European Union: The prevalence and health cost implications of chronic pain. Journal of Pain and Palliative Care Pharmacotherapy. 2012;26:310–325. doi: 10.3109/15360288.2012.736933. [DOI] [PubMed] [Google Scholar]
- McClintock A.S., McCarrick S.M., Garland E.L., Zeidan F, Zgierska A.E. Brief mindfulness-based interventions for acute and chronic pain: A systematic review. The Journal of Alternative and Complementary Medicine. 2018;25:265–278. doi: 10.1089/acm.2018.0351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moix J., Casado M.I. Terapias Psicológicas para el Tratamiento del Dolor Crónico. Clínica y Salud. 2011;22:41–50. doi: 10.5093/cl2011v22n1a3. [DOI] [Google Scholar]
- Morley S., Williams A., Hussain S. Estimating the clinical effectiveness of cognitive behavioural therapy in the clinic: Evaluation of a CBT informed pain management programme. PAIN Reports. 2008;137:670–680. doi: 10.1016/j.pain.2008.02.025. [DOI] [PubMed] [Google Scholar]
- *Morone N.E., Greco C.M., Moore C.G., Rollman B.L., Lane B., Morrow L.A., Glynn N.W., Weiner D.K. A mind-body program for older adults with chronic low back pain a randomized clinical trial. JAMA Internal Medicine. 2016;176:329–337. doi: 10.1001/jamainternmed.2015.8033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Omidi A., Zargar F. Effects of mindfulness-based stress reduction on perceived stress and psychological health in patients with tension headache. Journal of Research in Medical Sciences. 2015;20:1058–1063. doi: 10.4103/1735-1995.172816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owen-Smith A., Stewart C., Sesay M.M., Strasser S.M., Yarborough B.J., Ahmedani B., Miller-Matero L.R., Waring S.C., Haller I.H., Waitzfelder B.E., Sterling S.A., Campbell C.I., Hechter R.C., Zeber J.E., Copeland L.A., Scherrer J.F., Rosson J., Simon G. Chronic pain diagnoses and opioid dispensings among insured individuals with serious mental illness. BMC Psychiatry. 2020;20:1–11. doi: 10.1186/s12888-020-2456-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Parra-Delgado M., Latorre-Postigo J.M. Effectiveness of mindfulness-based cognitive therapy in the treatment of fibromyalgia: A randomised trial. Cognitive Therapy and Research. 2013;37:1015–1026. doi: 10.1007/s10608-013-9538-z. [DOI] [Google Scholar]
- Perestelo-Pérez L. Standards on how to develop and report systematic reviews in Psychology and Health. International Journal of Clinical and Health Psychology. 2013;13:49–57. [Google Scholar]
- Perestelo-Perez L., Barraca J., Rivero-Santana A., Alvarez-Perez Y. Mindfulness-based interventions for the treatment of depressive rumination: Systematic review and meta-analysis. International Journal of Clinical and Health Psychology. 2017;17:282–295. doi: 10.1016/j.ijchp.2017.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Pérez-Aranda A., Feliu-Soler A., Montero-Marín J., García-Campayo J., Andrés-Rodríguez L., Borràs X., Rozadilla-Sacanell A., Peñarrubia-Maria M.T., Angarita-Osorio N., McCracken L.M., Luciano J.V. A randomized controlled efficacy trial of mindfulness-based stress reduction compared with an active control group and usual care for fibromyalgia: The EUDAIMON study. Pain. 2019;160:2508–2523. doi: 10.1097/j.pain.0000000000001655. [DOI] [PubMed] [Google Scholar]
- Reid K.J., Harker J., Bala M.M., Truyers C., Kellen E., Bekkering G.E., Kleijnen J. Epidemiology of chronic non-cancer pain in Europe: Narrative review of prevalence, pain treatments and pain impact. Current Medical Research and Opinion. 2011;27:449–462. doi: 10.1185/03007995.2010.545813. [DOI] [PubMed] [Google Scholar]
- *Reiner K., Shvartzman P., Cohen Z.Z., Lipsitz J.D. Assessing the effectiveness of mindfulness in the treatment of chronic back pain: Use of quantitative sensory pain assessment. Mindfulness. 2019;10:943–952. doi: 10.1007/s12671-018-1053-6. [DOI] [Google Scholar]
- Sá K.N., Moreira L., Baptista A.F., Yeng L.T., Teixeira M.J., Galhardoni R., de Andrade D.C. Prevalence of chronic pain in developing countries. PAIN Reports. 2019;4:e779. doi: 10.1097/pr9.0000000000000779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Schmidt S., Grossman P., Schwarzer B., Jena S., Naumann J., Walach H. Treating fibromyalgia with mindfulness-based stress reduction: Results from a 3-armed randomized controlled trial. Pain. 2011;152:361–369. doi: 10.1016/j.pain.2010.10.043. [DOI] [PubMed] [Google Scholar]
- Segal Z.V., Williams J.M., Teasdale J.D. Guildford Press; 2012. Mindfulness-Based Cognitive Therapy for Depression. [Google Scholar]
- *Turner J.A., Anderson M.L., Balderson B.H., Cook A.J., Sherman K.J., Cherkin D.C. Mindfulness-based stress reduction and cognitive behavioral therapy for chronic low back pain: Similar effects on mindfulness, catastrophizing, self-efficacy, and acceptance in a randomized controlled trial. Pain. 2016;157:2434–2444. doi: 10.1097/j.pain.0000000000000635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Wells R.E., Burch R., Paulsen R.H., Wayne P.M., Houle T.T., Loder E. Meditation for migraines: A pilot randomized controlled trial. Headache. 2014;54:1484–1495. doi: 10.1111/head.12420. [DOI] [PubMed] [Google Scholar]
- Williams A.C., Eccleston C., Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database of Systematic Reviews. 2012;11:1–83. doi: 10.1002/14651858.CD007407.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Y., Wang Y., Chen J., He Y., Zeng Q., Huang Y., Xu X., Lu J., Wang Z., Sun X., Chen J., Yan F., Li T., Guo W., Xu G., Tian H., Xu X., Ma Y., Wang L., Zhang M., Yan Y., Wang B., Xiao S., Zhou L., Li L., Zhang Y., Chen H., Zhang T., Yan J., Ding H., Yu Y., Kou C., Jia F., Liu J., Chen Z., Zhang N., Du X., Du X., Wu Y., Li G. The comorbidity of mental and physical disorders with self-reported chronic back or neck pain: Results from the China Mental Health Survey. Journal of Affective Disorders. 2020;260:334–341. doi: 10.1016/j.jad.2019.08.089. [DOI] [PubMed] [Google Scholar]
- *Yeung S., Wong S., Chan F.W.-K., Wong R.L.-P., Chu M.-C., Lam Y.-Y.K., Mercer S.W., Ma S.H. Comparing the effectiveness of mindfulness-based stress reduction and multidisciplinary intervention programs for chronic pain a randomized comparative trial. Clinical Journal of Pain. 2011;27:724–734. doi: 10.1097/AJP.0b013e3182183c6e. [DOI] [PubMed] [Google Scholar]
- Yunus M.B. Central sensitivity syndromes: a new paradigm and group nosology for fibromyalgia and overlapping conditions, and the related issue of disease versus illness. Seminars in Arthritis and Rheumatism. 2008;37:339–349. doi: 10.1016/j.semarthrit.2007.09.003. [DOI] [PubMed] [Google Scholar]