Abbreviations
- Alk P
alkaline phosphatase
- ALT
alanine aminotransferase
- AST
aspartate aminotransferase
- KISC
ketamine‐induced sclerosing cholangitis
Drug‐induced (secondary) sclerosing cholangitis has recently been observed with a number of agents.( 1 ) Ketamine is a remarkably safe anesthetic, providing sedation and analgesia as an adjunct to, or substitute for, more traditional sedative medications. Although previous reports of recreational ketamine abuse have been associated with findings of secondary sclerosing cholangitis,( 2 , 3 ) we report here a presentation of the syndrome in association with prolonged ketamine use in the intensive care unit.
Case Summary
A 54‐year‐old female with type 2 diabetes, hypothyroidism, hypertension, and hyperlipidemia developed a severe COVID‐19 infection requiring mechanical ventilation for hypoxemic respiratory failure. She was difficult to sedate, requiring hydromorphone, midazolam, and high doses of propofol. Because of insufficient sedation, ketamine was added. After 15 days of ketamine infusions, she received oral ketamine for an additional 5 days. Nine days after extubation, she developed a cavitary Staphylococcal pneumonia, requiring reintubation, and another intravenous ketamine bolus at that time.
Her liver chemistries were normal upon admission. After she became critically ill, she was noted to have a slow but persistent rise in her alkaline phosphatase (Alk P), which peaked at 2,239 U/L (Fig. 1), with gamma‐glutamyl transferase (GGT) of 773 U/L 5 days after ketamine was initially discontinued. Aspartate aminotransferase (AST) and alanine aminotransferase (ALT) at the time were 1,260 and 1,729 U/L, respectively. Bilirubin remained normal at 0.4 mg/dL. Abdominal ultrasound showed heterogeneous liver parenchyma without bile duct abnormalities. Although her enzyme levels improved initially (Alk P 990, AST 40, and ALT 123 U/L), when she again became critically ill, she was given intravenous ketamine and her Alk P again rose abruptly to a peak of 1,720 U/L/GGT 538 U/L (Fig. 1), with AST 266 and ALT 407 U/L. Bilirubin remained normal at 0.3 mg/dL. Her international normalized ratio remained within normal limits throughout. Serological workup, including antinuclear, antimitochondrial, antismooth muscle, and antineutrophil cytoplasmic antibodies, was unrevealing. Viral infections, including HAV, HBV, HCV, HIV, Epstein‐Barr virus, and Herpes simplex virus, were also ruled out. A low titer of cytomegalovirus DNA in serum was detected.
FIG. 1.
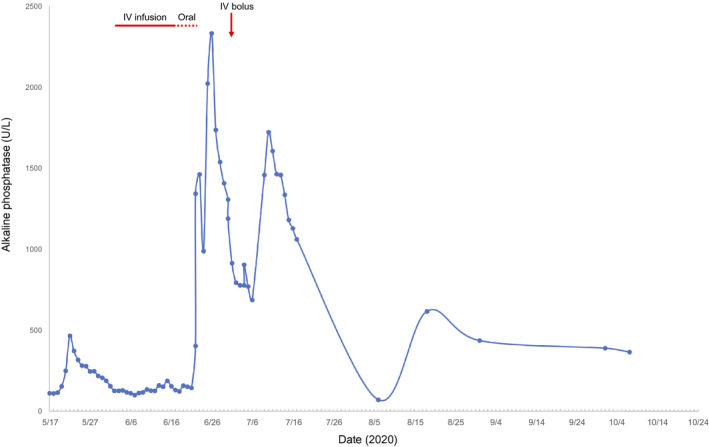
Graphic illustration of the rise and fall in Alk P in relation to ketamine administration. Solid red line indicates intravenous (IV) ketamine infusion, dashed red line indicates oral ketamine administration, and red arrow indicates the date of a ketamine IV bolus.
MR cholangiopancreatography at the height of her Alk P elevations showed intrahepatic dilatation with a beaded appearance as well as a dilated common bile duct with distal narrowing (Fig. 2A). Liver biopsy showed biliary ductular reaction with lobular inflammation and one small non‐necrotizing lobular granuloma without viral inclusions (Fig. 2B,C). Taken together, imaging and pathological findings are consistent with a unique form of drug‐induced liver injury: ketamine‐induced sclerosing cholangitis (KISC).
FIG. 2.
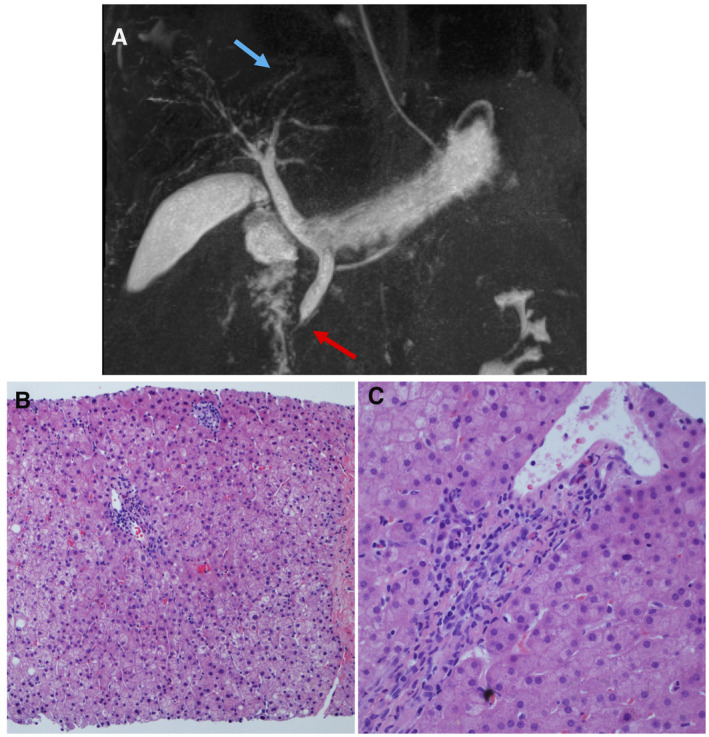
MR cholangiopancreatography and liver biopsy findings demonstrating sclerosing cholangitis. (A) MR cholangiopancreatography findings of KISC as noted by blue arrow highlighting intrahepatic biliary dilatation with a beaded appearance and red arrow pointing to a dilated common bile duct with distal narrowing. (B) Liver biopsy showing one small portal tract with mild bile duct injury/reactive changes, ductular proliferation, and one adjacent small lobular non‐necrotizing granuloma (HE, ×100). (C) Liver biopsy showing a portal tract with bile duct injury and minimal infiltration of neutrophils in the portal tract and lobule without marked cholestasis (HE, 40×).
By hospital day 71, her laboratory values improved, and she was discharged. Three months later, repeat liver enzyme tests in the clinic showed continued improvement: Alk P 365, AST 43, and ALT 55 U/L. We await repeat MR cholangiopancreatography, which is now scheduled for 6 months following onset.
Discussion
Previous case reports have documented KISC in patients after recreational ketamine use.( 2 , 3 ) This is a report of therapeutic use of ketamine causing a similar sclerosing cholangitis picture. Critically ill patients may develop sclerosing cholangitis following ischemic injury to the biliary tree( 4 ); however, our patient’s case is most consistent with ketamine toxicity, ischemic injury being unlikely in the absence of significant hypotension or histological findings consistent with ischemia. Given that her liver chemistries have continued to improve, we expect that KISC will be transient, but currently are awaiting repeat MR cholangiopancreatography.
Our patient highlights an under‐recognized side effect of prolonged use of ketamine as an analgesic/sedative in critically ill patients: KISC. The COVID‐19 pandemic has resulted in many patients with prolonged critical illness requiring intensive sedation, with ketamine being an alternative when conventional sedation is incomplete. Intensivists and hepatologists need to recognize that KISC can be a side effect of prolonged ketamine exposure.
Author Contributions:
S.A.I.K.: Conceptualization, investigation, data curation, writing ‐ original draft, and writing ‐ review and editing. A.A.: Conceptualization, investigation, writing ‐ review and editing. W.M.L.: Conceptualization, investigation, writing ‐ review and editing.
Acknowledgment
We are grateful for the diligent efforts of the pulmonary critical care staff at Parkland Memorial Hospital in caring for the innumerable COVID‐19 patients, and their consultation regarding this patient. We thank Dr. Zhikai Chi for the representative liver biopsy images.
Potential conflict of interest: Dr. Lee consults for Genentech, Pfizer, Karuna, Cortexyme, Affibody, and SeaGen. He received grants from Merck, Gilead, Conatus, Intercept, Bristol‐Myers Squibb, Novo Nordisk, Exalenz, and Instrumentation Labs.
References
- 1. Ahmad J, Rossi S, Rodgers SK, Ghabril M, Fontana RJ, Stolz A, et al. Sclerosing cholangitis‐like changes on magnetic resonance cholangiopancreatography in patients with drug‐induced liver injury. Clin Gastroenterol Hepatol 2019;17:789‐790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Turkish A, Luo JJ, Lefkowitch JH. Ketamine abuse, biliary tract disease, and secondary sclerosing cholangitis. Hepatology 2013;58:825‐827. [DOI] [PubMed] [Google Scholar]
- 3. Lo RSC, Krishnamoorthy R, Freeman JG, Austin AS. Cholestasis and biliary dilatation associated with chronic ketamine abuse: a case series. Singapore Med J 2011;52:52‐55. [PubMed] [Google Scholar]
- 4. Ruemmele P, Hofstaedter F, Gelbmann CM. Secondary sclerosing cholangitis. Nat Rev Gastroenterol Hepatol 2009;6:287‐295. [DOI] [PubMed] [Google Scholar]


