Abstract
Objective
To investigate the perceived educational and health risks associated with the COVID‐19 pandemic amongst dental students and educators.
Methods
A 17‐item electronic survey was sent to 496 undergraduate dental students and 53 clinical faculty members who attended clinical sessions during the outbreak period. The survey explored various aspects related to primary sources and prevention of disease exposure, dental management of suspected cases, impact of COVID‐19 on students’ clinical performance and effects of suspension of educational activities on academic performance and clinical competence.
Results
The response rate of the students’ was 60.7% (n = 301). The majority of students reported that performing clinical work during the outbreak posed significant health concerns, resulted in a significant stress and negatively affected their clinical performance. The majority of students believed that aerosols generated during dental procedures are the major source for disease exposure and universal protective equipment is not effective for prevention. The decision to suspend teaching activities was supported by 89% of the students. Opinions were divided regarding the impact of the suspension on the academic performance and clinical competence. Educational videos were the most preferred form of distance education. The response rate of faculty members was 60.4% (n = 32). Responses of faculty members were similar to students, though fewer concerns were reported regarding the risk of disease transmission. All respondents agreed that extra‐precautionary measures are required to ensure optimum protection against disease exposure.
Conclusions
The recent COVID‐19 outbreak has adversely affected various elements of dental education. High levels of major health risk perception were noted amongst students and educators. The interruption to academic and clinical activities may lead to an inevitable skill deficit within the new generation of dental graduates. Educators are under significant pressure to accommodate abrupt changes in teaching methods, find solutions to mitigate skill deficit and ensure safe clinical practice once clinical activities are resumed.
Keywords: COVID‐19, dental education, infection control, teaching clinics
1. INTRODUCTION
The emergent coronavirus disease‐2019 (COVID‐19) pandemic has led to a significant global crisis owing to the rapid spread and high morbidity and mortality rates. 1 Respiratory droplets containing the novel virus, the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), are the primary contagion of the disease. 2 The spread of the causative agent is primarily mediated by inhalation of respiratory droplets or direct contact with contaminated surfaces. 3 Faecal‐oral and air‐borne routes of transmission have also been reported. 4 , 5 , 6 The role of asymptomatic and pre‐symptomatic infected subjects in COVID‐19 transmission to close contacts and healthcare providers is still controversial. 7 Family clusters have been related to cases positive for SARS‐CoV‐2 RNA 7 , 8 , 9 whilst other reports demonstrated a lack of evidence to support such findings. 7 , 10 , 11 Prevalence of asymptomatic cases is dependent on disease activity, the number of confirmed cases and the number of random tests. 7 Studies from areas with varied disease activity and at different stages of the pandemic revealed that the prevalence of asymptomatic COVID‐19‐infected cases can be in the range of 0.003%‐1.4%. 7 , 12 , 13 , 14
The COVID‐19 pandemic has increased the burden on already strained health services worldwide. 15 The lack of a tested vaccine for the SARS‐CoV‐2 or evidence‐based treatment protocols with long‐term positive outcomes have added to the distress of the current situation. 16 Several countries have undertaken extreme and radical measures in an attempt to achieve containment of the disease and to flatten the COVID‐19 curve. Nationwide lockdowns have been imposed, home quarantines have been instated, travel restrictions and borders shutdown have been witnessed across the globe.
In several countries, suspension of educational activities has been implemented in all academic institutions aiming to reduce disease transmission amongst large cohorts of staff and students. Clinical activities within dental schools were amongst the earliest to be suspended. This was attributed to the risk of disease exposure and transmission in dental settings. 17 Dentists and allied dental personnel were ranked amongst the high‐risk category according to the risk of disease exposure per profession. 18 , 19 , 20 Such risk can be attributed to the close physical proximity to patients during treatment, high possibility of contacting respiratory droplets and contaminated body fluids, a moral obligation to treat patients in pain and inability to make a decision for self‐isolation. Almost all dental procedures generate significant contaminated splatter and aerosols that can be suspended in air for extended periods. 3 , 4 Instruments and surfaces contaminated with various body fluids of an infected individual are another source of virus transmission. 3 , 17 Inhalation of such aerosols or direct contact with mucosal membranes may lead to transmission of the disease to dental personnel and other patients. Injuries with contaminated sharp objects can also lead to disease transmission. 3 , 17
The pace and extent of disease transmission can be alarming particularly in dental teaching facilities. The increased risk can be related to (a) the large number of patients and their companions who are present in a confined space, (b) the large amount of aerosolised body fluids generated during the use of multiple hand‐pieces and ultrasonic scalers simultaneously, 3 (c) the architectural design of teaching clinics where aerosols can affect several individuals through the interconnected dental units, (d) inadequate adherence to infection control protocols by less experienced undergraduate students and (e) administrative staff members who have access to dental clinics without personal protective equipment (PPE) who can possibly spread the infection through their workplaces. That being said, strong adherence to cross infection control policies seems to limit disease transmission in dental settings. In Wuhan city where the pandemic started, nine staff members of Wuhan School and Hospital of Stomatology have been diagnosed with COVID‐19. 20 Epidemiologic investigation of the nine cases suggested that the infection was not acquired as a result of clinical activities within the dental school. Further, the number of cases did not increase despite the large number of patients who attended the dental school during the peak of the pandemic. 20 Moreover, a recent study has demonstrated a low risk of COVID‐19 transmission in dental offices as a result of the already instated infection control policies and precautionary measures. 7
The suspension of educational activities poses few challenges in theoretical disciplines. Advances in internet based‐communication, videoconferencing applications and educational blogs have facilitated efficient delivery of the theoretical educational content. In fact, it has been reported that teaching didactic dental subjects by videoconferencing was as effective as traditional face‐to‐face seminars. 21 , 22 However, clinical courses are designed primarily to ensure students’ competence in routine dental procedures. Such clinical skills and expertise cannot be optimally gained without a supervised patient treatment experience.
The entire educational sector has been disturbed by the current global crisis. Dental students and educators are amongst the most affected being at risk of exposure to an unprecedented and potentially fatal disease. 3 , 20 Furthermore, significant interruption to the educational process may adversely affect the development of students’ competencies. The aim of this study was to investigate, using an electronic survey, the health and educational risks of COVID‐19 as perceived by dental students and educators.
2. METHODS
A focus group comprised of four faculty members who were actively involved in dental education developed an initial version of the survey. A pilot questionnaire was distributed to five faculty members and twenty‐five students. Feedback was collected regarding the clarity and order of questions, and whether questions covered the objectives of the study. The final version of the electronic survey was set on the Google forms platform. A link was sent to the undergraduate dental students in the clinical years at the Jordan University of Science & Technology via their e‐learning accounts (n = 496). Another link to a modified survey was sent to faculty members who supervised clinical sessions during the early period of the COVID‐19 outbreak (n = 53). A follow‐up reminder was sent after two and five days. The survey was closed after one week. Ethical approval was obtained from the Institutional Research Board at the Jordan University of Science & Technology (Reference no. 54/132/2020).
The survey contained seventeen questions that investigated the impact of the COVID‐19 pandemic on the educational process from both dental students’ and educators’ perspectives. Responding to all multiple‐choice questions was a prerequisite for submission and recording of responses. Respondents were given the option to provide further explanation/justification/comments in a free‐text field to most of the questions. The survey explored several aspects related to the following:
perception of health risks and concerns whilst working in dental teaching clinics during the early stages of COVID‐19 outbreak,
effects of the COVID‐19 pandemic on stress levels,
effectiveness of PPE and the preventive measures implemented to reduce the risk of disease exposure,
effects of the COVID‐19 pandemic on student's performance and flow of patients,
attitudes towards the government decision to suspend educational activities and implement distance education, and
impact on academic performance and clinical competence.
Data are presented as percentage (number) of respondents per question. Pearson's correlation coefficient was calculated to evaluate the factors that may have affected respondents’ perception of some educational and health risks. All analyses were performed using Statistical Package for Social Sciences software (Version 23, IBM® SPSS® Statistics).
3. RESULTS
The response rate was 60.7% (n = 301) for dental students and 60.4% (n = 32) for faculty members. Table 1 summarises the demographics of the respondents.
Table 1.
Survey respondent demographics
| Respondents | Students | Faculty members | |
|---|---|---|---|
| Number of respondents | 301 | 32 | |
| Age | Median (IQR) | 23.0 (1.0) | 39.5 (12.5) |
| Gender | Male | 38.1% | 53.1% |
| Female | 61.9% | 46.9% | |
| Level | 4th year | 40.1% | ‐ |
| 5th year | 59.9% | ||
| Specialty | Oral medicine and surgery | ‐ | 21.9% |
| Restorative dentistry | 50.0% | ||
| Orthodontics | 6.2% | ||
| Periodontics | 12.5% | ||
| Paediatric dentistry | 9.4% | ||
3.1. Risk of exposure to COVID‐19
The majority of students (n = 279, 92.7%) considered themselves being at an increased health risk whilst practicing in the dental teaching clinics during the early period of the COVID‐19 pandemic. A lower percentage was reported amongst respondent faculty members (n = 25, 78.1%). Spreading the disease to family members was the primary concern of the majority of students and faculty members (n = 285, 86% and n = 24, 75%, respectively). Only 18.8% (n = 6) of faculty members did not have concerns regarding students being a source of disease transmission to their families and local communities. Concerns about acquiring COVID‐19 were distressing and had adverse effects on the clinical performance of 56.1% (n = 169) of students. Only 40.6% (n = 13) of faculty members observed that the COVID‐19 outbreak was distressing for students and adversely affected their clinical performance. Further, less than one‐third (28.1%, n = 9) of the faculty members reported that the COVID‐19 pandemic had the same negative impact on them. The majority of students (n = 205, 68.1%) were significantly concerned to an extent that they would make a unilateral decision not to attend clinical sessions amid the risk of exposure to COVID‐19 should the university keep clinical activities running as usual. The majority of respondents considered aerosols generated during dental treatments, crowding in clinics and waiting areas and unintentional violation of cross infection protocols as potential primary sources for disease transmission (Figure 1).
Figure 1.
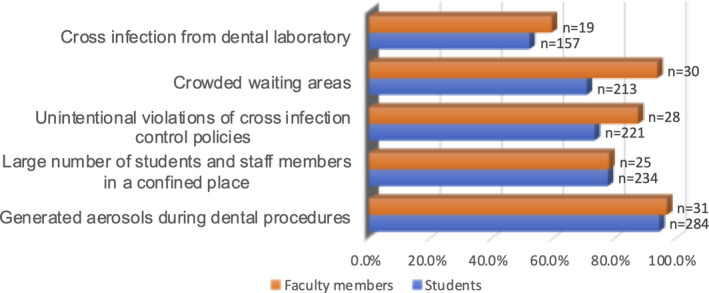
Primary transmission sources of COVID‐19 according to respondents
3.2. Prevention of exposure to COVID‐19
Universal precautions and standard PPE were considered ineffective by 59.1% (n = 178) of the respondent students and 40.6% (n = 13) of the respondent faculty members. The majority of faculty members (81.3%, n = 26) reported that they would instruct students not to treat any patient with obvious symptoms of a respiratory tract infection. Further, only one‐third (n = 10) of faculty members would allow students to treat a patient who had recently travelled to a country with a high incidence of COVID‐19. Less than two‐thirds of students stated that they would refuse to treat any patient with an obvious respiratory tract infection (64.5%, n = 194) or recent travel history to COVID‐19 hotspots (65.1%, n = 196). Patient flow and commitment to dental appointments were adversely affected during the COVID‐19 outbreak according to 59.8% (n = 180) of students and half (n = 16) of faculty members. The respondents reported the use of, or the need for, several additional precautionary measure(s) to prevent the exposure to COVID‐19 such as advanced PPE, restriction of dental treatment to emergency cases only and measuring patients’ and staff members’ body temperature as a precautionary measure (Figure 2).
Figure 2.
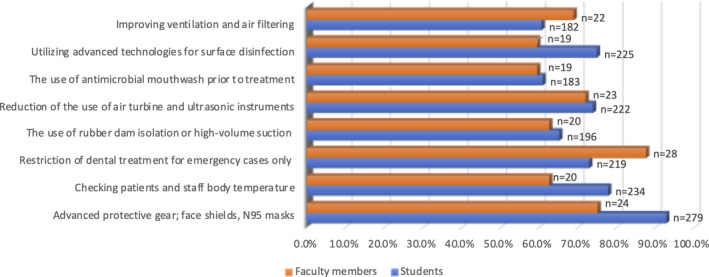
Additional precautionary measures to reduce risk of exposure to COVID‐19
There was an agreement between respondent students and faculty members regarding the reliable sources of information for keeping up to date regarding the current COVID‐19 pandemic. Reference health institutions or authorities such as Ministry of Health, World Health Organization and Centres for Disease Control and Prevention were the primary resources for information for 93.8% (n = 30) of faculty members and 76.7% (n = 231) of students. Institution updates and social media platforms were utilised by 57.3% (n = 173) and 54.8% (n = 165) of the students, respectively. Less than 50% of the students referred to news reports and scientific papers. Scientific papers (n = 24, 75%,) were the second most utilised resource, whilst social media platforms (n = 11, 34.4%) were the least visited for this purpose by the respondent faculty members.
3.3. Suspension of educational activities and distance education
The majority of respondent students (n = 268, 89%) agreed that the temporary suspension of clinical activities would help in the containment of the COVID‐19 pandemic. All respondent faculty members (n = 32) supported the rationale of suspending clinical activities. Half of them (n = 16) initiated a process of, or demanded, suspending clinical activities since the diagnosis of the first COVID‐19 case in Jordan. Amid the suspension, 52.5% (n = 158) students believed that it would adversely affect their clinical competence due to reduced clinical exposure. With respect to faculty members, 56.3% (n = 18) believed that the suspension would adversely affect the clinical competence of students. Respondents were divided regarding the potential impact of suspending teaching activities on students’ academic performance as follows:
no significant impact: students (n = 123, 41.9%), faculty members (n = 8, 25%),
negative impact: students (n = 112, 37.2%), faculty members (n = 18, 56.2%), and
positive impact: students (n = 66, 21.9%), faculty members (n = 6, 18.8%).
Educational videos were the preferred distance educational method for students (n = 224, 74.4%) and faculty members (n = 29, 90.6%). Self‐learning was the least favoured by students, whilst using clinical simulation laboratories to replace clinical sessions during the suspension period was the least preferred by the faculty members (Figure 3).
Figure 3.
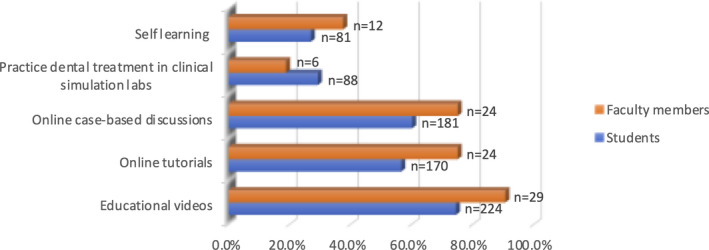
Distance educational methods to be utilised during suspension period according to the respondents
Faculty members suggested the following measures in order to address the interruption of educational activities:
extension of the academic year to compensate for the suspension period (n = 23, 71.9%),
addressing the resultant clinical skill deficit during vocational training (VT) as far as final‐year students are concerned (n = 15, 46.9%),
reduction of the number of clinical requirements (n = 10, 31.3%),
reduction of the difficulty index of exam questions (n = 4, 12.5%),
grading on a curve to boost students' grades (n = 4, 12.5%) and
no additional measures should be in place as the suspension will have no impact on the educational outcomes (n = 8, 25%).
3.4. Association between independent variables
Pairwise Pearson correlation analysis was used to identify the variables that had significant association with:
the perceived increased health risk,
the increased stress levels during clinical activities,
refusing treating patients who travelled to epidemic areas or showing symptoms of respiratory tract infection and
perceived negative impact on academic performance or clinical competence.
Variables that exhibited significant correlation with the above‐perceived educational and health risks amongst respondent students and staff members are listed in Table 2.
Table 2.
Independent variable (perceived risks or factors) that exhibited significant correlation
| Independent variables | P‐value | Correlation coefficient | 95% CI | ||
|---|---|---|---|---|---|
| Students | Perceived effectiveness of PPE | Increased health risk | 0.036 | −0.206 | −0.139:0.087 |
| Disease transmission to family and community | 0.004 | −0.164 | −0.272:−0.052 | ||
| Unilateral decision not to attend clinical sessions | 0.022 | −0.069 | −0.181:0.021 | ||
| Refuse to treat patients recently travelled to epidemic areas | 0.047 | 0.505 | 0.416:0.585 | ||
| Stress during clinical activities | Increased health risk | 0.001 | 0.166 | 0.054:0.274 | |
| Disease transmission to family and community | 0.004 | 0.189 | 0.078:0.296 | ||
| Perceived effectiveness of PPE | 0.004 | −0.082 | −0.193:0.032 | ||
| Refuse to treat patients recently travelled to epidemic areas | 0.001 | 0.196 | 0.085:0.302 | ||
| Refuse to treat patients exhibiting symptoms of respiratory tract infection | 0.001 | 0.197 | 0.086:0.303 | ||
| Unilateral decision not to attend clinical sessions | <0.001 | 0.228 | 0.118:0.333 | ||
| Academic and clinical deficits | 5th year student | 0.008 | 0.190 | 0.079:0.297 | |
| Staff | Faculty members with administrative roles | Negative impact on students’ academic performance and clinical competence | 0.010 | 0.442 | 0.116:0.682 |
| Initiate or support decision to suspend educational activities | 0.018 | 0.412 | 0.075:0.665 | ||
| Significant concerns that students will transmit infection to family and community members | 0.048 | 0.333 | −0.011:0.607 | ||
| Increased health risk | Concerns regarding disease transmission to own family and community members | 0.022 | 0.398 | 0.064:0.652 | |
| Concerns that students may contribute to disease transmission to family and community members | 0.002 | 0.524 | 0.221:0.735 | ||
| Students under stress during clinical activities | 0.015 | 0.418 | 0.088:0.666 | ||
| Initiate or support decision to suspend educational activities | 0.019 | 0.412 | 0.074:0.665 | ||
| Staff under stress | Encourage students not to treat patients recently travelled to epidemic areas | 0.020 | 0.404 | 0.072:0.657 | |
4. DISCUSSION
The situation of COVID‐19 pandemic is rapidly unfolding owing to the novelty and rapid spread of the disease. The initial response of some countries has changed from taking minimal actions to deal with “just a flu” to announcing a nationwide state of emergency and lockdown in a very short period. 23 No country, to date, has been immune to the repercussions of this crisis. The number of fatalities and infected cases continues to rise even in economically and politically advantaged countries. 24 , 25 World‐leading healthcare systems are under unsurpassed pressure with a large‐scale collapse possibly iminent. 26
Despite the preparedness and high capacity of health services (ventilator to individual ratio of 1:4400 compared to 1:14,000 in other countries) 27 , 28 and the relatively small population size, severe mitigation measures were taken early on in Jordan. The first COVID‐19‐infected case in Jordan was reported on 2 March 2020 for a subject who acquired the infection in Italy. On March 15th, the government announced the suspension of all teaching activities nationwide when twelve new COVID‐19 cases were confirmed. 20 In the period in‐between, clinical activities were running as usual in the dental teaching clinics at the Jordan University of Science & Technology. A total lockdown was shortly instated afterwards, and provision of dental care was restricted to designated, hospital‐based practices within Ministry of Health facilities. In early June 2020, 979 cases were registered with only nine fatalities, 29 lockdown was eased, and all dental practices resumed work under strict precautions except for university‐based dental teaching clinics, as the risk of disease transmission was deemed to be high.
This study aimed to investigate dental students’ and educators’ perceived health risks associated with practicing clinical dentistry during the COVID‐19 pandemic. We also explored the consequences of suspending clinical activities and strategies to reduce any adverse impact on students’ academic performance and clinical competence. We used an electronic survey for this purpose that contained seventeen questions in addition to twelve open ended fields for comments or explanations in some of the questions. One of the limitations of this study was the relatively lengthy survey. This might have negatively affected the response rate as answering all questions was mandatory. Despite that this study was very timely to address an area of immediate concern in dental education, the influence of the timing of the survey could be twofold; (a) respondents were experiencing significant uncertainty as the pandemic was in its early stages which may have meant that respondents were overly concerned, and (b) the announced lockdown period was fourteen days only at the time of survey distribution, which might have led to underestimation of the sequela of the pandemic on dental education.
The overwhelming majority of respondent students considered working in dental teaching clinics during the outbreak as a major risk for exposure to COVID‐19. The most frequently cited causes for such concerns were the novel nature of the virus, lack of vaccines or effective treatments, emerging reports indicating that the disease can be decapacitating to all age groups, 30 close proximity to untested patients, high risk to inhale or contact respiratory droplets and saliva in the confined space of the dental unit, and the lack of patients’ awareness regarding the disease and precautionary measures. Similar findings were reported in a study where third‐ and fourth‐year students submitted a written reflection as part of a mandatory assignment for the dental geriatric modules. 31 The vast majority of students in the latter study expressed concerns regarding the risk of disease exposure and transmission. 31 Such findings suggest the urgent need for efficient counselling and psychological support in order alleviate students’ stress and concerns. 7 , 20
The minority of respondent students (n = 35, 7.3%) who marginalised the health risk of COVID‐19 trusted their infection control practices and believed that the severity of COVID‐19 was exaggerated by social media. A higher percentage of respondent faculty members (n = 7, 21.9%) disregarded the major health risks of COVID‐19 whilst supervising clinical sessions. This can be possibly related to the higher experience of the latter and reduced contact time with patients compared to students in the teaching clinics. It is noteworthy that this study was conducted during the early stages of the pandemic when little was known about the transmissibility of COVID‐19. The perception of risk might have been lower should the survey been conducted months later given the emerging evidence suggesting a very low risk of acquiring COVID‐19 as a result of clinical activities in dental offices. A recent study reported a very low annualised probability (0.008%) for a dental healthcare personnel to acquire COVID‐19 infection in a dental setting. 7 The authors attributed their findings to the following factors: “the effectiveness of PPEs including N95 masks and face shields, low prevalence of asymptomatic patients in the community, low transmissibility of both symptomatic and asymptomatic patients in healthcare settings, less severe outcomes of COVID‐19 in individuals with no underlying conditions, the relatively low viral load of SARS‐CoV‐2 in human saliva even in severely ill patients, extremely low probability for dental aerosols to contain viable viruses, readily available viricidal oral rinses that could rapidly inactivate viable viruses and the relatively brief period of contact with dental patients in an outpatient dental setting”. 7
One disconcerting finding was that less than half of the respondent faculty members observed that over half of the students were overly stressed during the outbreak. Many students reported being very distracted in the clinics as they were focusing on infection control and keeping distance from the patient rather than the treatment itself. This, of course, had an impact on competence development and increased the incidence of errors in clinical sessions. Students also reported, which was also observed by faculty members, performing fewer procedures and reduced acceptance of new cases. The vast majority of respondents were concerned that they might spread the disease to their families. All concerned respondents emphasised that they were particularly anxious regarding spreading the disease to vulnerable subjects such as senior family members with complex medical histories or children.
There was an agreement amongst all respondents that aerosolised respiratory droplets, saliva and blood were the major sources of infection. As anticipated, faculty members reported that violation of infection control protocols was an important source for disease transmission as they are always in a position to monitor students’ adherence to such protocols. It was however interesting that a high percentage of students reported this as a concerning primary source of exposure as they usually very focused on the procedure during the clinical session and rarely pay attention to such violations.
Surgical masks and goggles were considered ineffective to prevent disease exposure by 59.1% of students and 40.1% of faculty members. The vast majority of respondents reiterated the need for advanced PPE such as N95 respirators, face shields and disposable waterproof gowns. In vitro studies demonstrated the effectiveness of filtering viable H1N1 viruses carried in artificial saliva at a continuous flow rate. 32 Given that the filtration efficiency of a N95 respirator is primarily dependent on the size and not the type or origin of the particles, N95 respirators can effectively prevent inhalation SARS‐CoV‐2 virus as it exhibits a larger diameter when compared to H1N1 counterpart. 7 , 32 , 33 Furthermore, using N95 respirators significantly reduced COVID‐19 infections amongst healthcare professionals (0.06%) compared to the early stages of the pandemic when health workers did not use N95 respirators (2.83%). 7 Further protection can be obtained by face shields as they prevent contact between mucus membranes and mediums containing pathogens. 7 , 34 Face shields reduced viral exposure by 96% to particulates produced by a cough from 18 inches distance. 34 Face shields also have the advantage that they can be disinfected and re‐used. Moreover, face shields tend to reduce autoinoculation as they break the habit of face touching whilst in place. Consequently, they have been highly recommended as part of the standard PPE in dental practices. 35
Regarding management of dental patients during the pandemic, there was a consensus amongst the majority of published guidelines/protocols regarding the virtue of patient triage and reduction of microbial load prior to commencing dental treatment. 3 , 20 It was reassuring that the majority of respondents in this study were aware of such guidelines as they reported the importance of triage, history taking and body temperature measurement. Moreover, reduction of generated aerosols, the use of antimicrobial mouthwash prior treatment 15 and rubber dam isolation, which is also known to reduce nosocomial infections, 20 , 36 were all cited by the majority of respondents. Furthermore, most of the respondents commented about the importance of installing air filters and utilisation of the current methods of surface disinfection and coatings that can reduce microbial colonisation.
The currently available guidelines recommend postponing the treatment of any patient who had contact with infected subjects or those who have travelled to highly epidemic areas. 3 , 20 In excess of two‐thirds of all respondents agreed that patients with symptoms of respiratory tract infection or with recent travel history to areas of epidemics should not be treated in students’ clinics. Respondents reiterated that emergency cases can be referred to hospital‐based dental settings and non‐urgent treatments can be deferred with appropriate referral for medical care. Faculty staff members who were willing to treat the earlier cases justified their choice on the basis of effectiveness of the implemented infection control protocols. On the other hand, students’ decisions to treat patients were primarily driven by the pressure of clinical requirements.
The decision to suspend clinical activities was accepted by all but a small fraction of students who were concerned about the completion of clinical requirements or assumed that existing infection control procedures were adequate for the prevention of exposure. One interesting finding was that about two‐thirds of the respondent students reported that they would make a unilateral decision to refrain attending clinical sessions should the number of COVID‐19‐infected cases significantly increase. They indicated their concerns regarding exposure to the disease exceeded the concerns about any subsequent disciplinary proceedings.
Respondents were divided regarding the effect of the suspension on the academic performance of the students. Respondents who did not foresee a negative impact had this point of view as the suspension period was announced first for 14 days, a rather short period that can be compensated via additional clinical sessions. As the suspension was extended for more than 4 months, a completely different response from the majority of participants would possibly have been expected. The expected negative impact can be related to the fact that face‐to‐face education is the primary teaching/learning modality in the Jordan University of Science & Technology and perhaps the entire region. Thus, the implementation of distance education may be challenging to the faculty members with limited experience in this field and students who may be reluctant to accept such fundamental change in learning methods. The negative impact on dental education was reported by other studies. 37 , 38 The inability to deliver adequate teaching of clinical skills through distance education was believed to be the most important cause for such negative impact. 37 , 38 A minority of students and faculty members indicated that this suspension may have a positive impact. In their opinion, the suspension would allow students to revise and prepare for the final examinations, which they usually do not have sufficient time for due to the busy daily schedule where students are engaged for eight hours of clinical sessions and seminars per day. Off note, the suspension of educational activities has elicited an unprecedented positive response from various institutes and individuals involved in dental education around the world. We observed substantial interaction and cooperation between various academic institutes and regulatory bodies, 38 , 39 , 40 major online publishers provided free access to their educational and scientific materials, 41 online conferences, webinars and courses attended by thousands of students most of whom would not be able to afford due to financial and time restrictions prior the pandemic. We expect that the aforementioned may have a notable positive impact on the academic performance of students who made the most of such opportunities.
With regard to the effect of suspension on clinical competence, respondents were divided regarding this aspect as just over half of both students and faculty members foresaw a negative impact on students’ clinical competence. Again, this can be related to the assumption that the suspension would last for a short period and the fact that only six weeks remained for the second semester of the academic year. Students who indicated a negative impact were in either in the final year or were running behind with clinical requirements. Faculty members were also concerned primarily about these particular groups. Similar responses were reported in another study were the majority of the respondents expressed deep concerns regarding graduating without practicing certain clinical procedures under supervision in the university. 31
Adopting online distance education was essential during the suspension period in order to achieve the educational objectives. 20 Educational videos were the preferred distance education method amongst all respondents. Videos and animations demonstrating clinical techniques are amongst the most attractive and effective educational materials. 42 , 43 They can replace, or at least, be a very effective adjunct to a static series of slides. This in turn, may maximise the educational benefits of the interaction with the teaching material by providing an enhanced and diverse learning environment. 44 Furthermore, our experience indicates that students already utilise educational videos as a succinct, accessible and readily available resource in order to help them prepare for clinical work. They were also utilised by students to get access to contemporary materials and techniques that dental schools may not be able to provide/demonstrate for students in the undergraduate programs. Such videos may satisfy students’ scientific curiosity and motivate them to further explore various disciplines of dentistry.
The majority of respondent faculty members, one‐third of whom had administrative roles, supported the extension of the academic calendar to compensate for the suspension period. This proposal sounded reasonable in the short term. However, it may have some implications as it may lead to delay the graduation of final‐year students and subsequently their enrolment in the VT programs and workforce. A large proportion of graduates apply for postgraduate programs immediately after the completion of VT. In the case of such delays, graduates will miss application deadlines unless they are amended, or the VT duration period reduced. Reduction in the length of VT would further compromise the plan to compensate for any clinical skill deficit caused by the suspension period.
The authors of this study conducted a relatively similar study at the University of Otago‐Faculty of Dentistry, New Zealand. 45 The used survey was modified in order to adapt to situation there as students were still working at the time when the survey was distributed. There was an agreement between the findings regarding the key aspects explored in both studies. Though the New Zealand study reported a more pronounced negative impact on academic performance and clinical competence by students and staff members. 45
The world is currently observing an increased incidence of emerging, contagious diseases. As dental professionals and students may be at a high risk of infection and transmission, dental practice and education may have to undergo a significant transformation in order to prepare for such events. This and similar studies are pivotal to improving risk assessment and quality control processes during such pandemics. The findings of this study may potentially improve the utilisation of distance education as a method to reduce the negative impact of any suspension period on students' academic performance and clinical competence. Leading regulatory bodies should proactively work on strategies to mitigate the deficits created by such pandemics. Immediate strategies and guidance are urgently required to address the reduced clinical exposure of the current final year students and to coordinate their enrolment in VT and speciality training programs. Dental educators and institutes should seize the opportunity to re‐visit the current strategies in order to strengthen dental educational systems. Long‐term guidance and strategies are required to regulate various aspects that may contribute to the risk of disease transmission within dental teaching clinics such as the number of admitted students, infection control policies and armamentarium, and exploiting advanced technologies and artificial intelligence to optimise distance education and simulated clinical training. A comprehensive analysis of the currently available experimental and clinical evidence is required to ensure safe return of students, educators and patients to dental schools. Biosafety committees comprised of students, administrative and academic staff can play an important role in addressing the concerns of all parties regarding teaching and clinical activities. Further studies are warranted to evaluate and develop the current students’ assessment methods and to explore how the reduced clinical exposure and the pandemic will potentially impact graduates’ future career plans.
5. CONCLUSIONS
In the opinion of the respondents to this study, the COVID‐19 outbreak had adversely affected various elements of the dental education. Concerns regarding acquiring and transmitting the disease amongst students and faculty members were raised during the early stages of the pandemic. The significant interruption to the academic and clinical activities of this student cohort may lead to an inevitable skill deficit within the new generation of dental graduates. Educators are under significant pressure to accommodate the abrupt changes in the teaching methods, find solutions to mitigate skill deficit and ensure safe clinical practice once clinical activities are resumed. Fundamental changes and improvements are urgently needed to reform our educational systems and strategies to accommodate the impact of the current pandemic and similar events that could take place in the future.
CONFLICT OF INTEREST
None of the authors of this manuscript have any conflict of interest to declare.
ACKNOWLEDGMENTS
The authors would like to acknowledge with gratitude Dr Nosayba Alazzam for her help with statistical analysis. We also deeply thank all students and faculty members who responded to this survey in the Faculty of Dentistry at JUST.
Jum’ah AA, Elsalem L, Loch C, Schwass D, Brunton PA. Perception of health and educational risks amongst dental students and educators in the era of COVID‐19. Eur J Dent Educ.2021;25:506–515. 10.1111/eje.12626
Contributor Information
Ahmad A. Jum’ah, Email: aajuma@just.edu.jo.
Donald Schwass, Email: donald.schwass@otago.ac.nz.
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no data sets were generated or analysed during the current study.
REFERENCES
- 1. World Health Organization . WHO announces COVID‐19 outbreak a pandemic 2020. http://www.euro.who.int/en/health‐topics/health‐emergencies/coronavirus‐covid‐19/news/news/2020/3/who‐announces‐covid‐19‐outbreak‐a‐pandemic accessed April 6, 2020
- 2. World Health Organization . Guidance on routine immunization services during COVID‐19 pandemic in the WHO European Region 2020 http://www.euro.who.int/en/health‐topics/health‐emergencies/coronavirus‐covid‐19/novel‐coronavirus‐2019‐ncov‐technical‐guidance/coronavirus‐disease‐covid‐19‐outbreak‐technical‐guidance‐europe/guidance‐on‐routine‐immunization‐services‐during‐covid‐19‐pandemic‐in‐the‐who‐european‐region‐2020 accessed April 6, 2020
- 3. Peng X, XuX LIY, Cheng L, Zhou X, Ren B. Transmission routes of 2019‐nCoV and controls in dental practice. Int J Oral Sci. 2020;12(1):1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chen J. Pathogenicity and transmissibility of 2019‐nCoV—A quick overview and comparison with other emerging viruses. Microbes Infect. 2020;22(2):69‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gu J, Han B, Wang J. COVID‐19: Gastrointestinal Manifestations and Potential Fecal‐Oral Transmission. Gastroenterology. 2020;158(6):1518‐1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. World Health Organization . Transmission of SARS‐CoV‐2: implications for infection prevention precautions 2020. https://www.who.int/news‐room/commentaries/detail/transmission‐of‐sars‐cov‐2‐implications‐for‐infection‐prevention‐precautions accessed August 16 2020
- 7. Ren Y, Feng C, Rasubala L, Malmstrom H, Eliav E. Risk for dental healthcare professionals during the COVID‐19 global pandemic: an evidence‐based assessment. J Den. 2020;101:103434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zhang J, Tian S, Lou J, Chen Y. Familial cluster of COVID‐19 infection from an asymptomatic. Crit Care. 2020;24(1):119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gandhi M, Yokoe DS, Havlir DV. Asymptomatic transmission, the achilles’ heel of current strategies to control Covid‐19. N Engl J Med. 2020;382:2158‐2160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Burke RM. Active monitoring of persons exposed to patients with confirmed COVID‐19—United States, January–February 2020. Morb Mortal Wkly Rep. 2020;69(9):245‐246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kimball A, Hatfield KM, Arons M, et al. Asymptomatic and Presymptomatic SARS‐CoV‐2 Infections in Residents of a Long‐Term Care Skilled Nursing Facility ‐ King County, Washington, March 2020. Morb Mortal Wkly Rep. 2020;69(13):377‐381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gudbjartsson DF, Helgason A, Jonsson H, et al. Spread of SARS‐CoV‐2 in the Icelandic Population. N Engl J Med. 2020;382(24):2302‐2315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Oran DP, Topol EJ. Prevalence of Asymptomatic SARS‐CoV‐2 Infection: A Narrative Review. Ann Intern Med. 2020;173:362‐367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lavezzo E, Franchin E, Ciavarella C, et al. Suppression of a SARS‐CoV‐2 outbreak in the Italian municipality of Vo'. Nature. 2020;584(7821):425‐429. [DOI] [PubMed] [Google Scholar]
- 15. Ji Y, Ma Z, Peppelenbosch MP, Pan Q. Potential association between COVID‐19 mortality and health‐care resource availability. Lancet Glob Health. 2020;8(4):e480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. U.S. Food and Drug Administration , Coronavirus Disease 2019 (COVID‐19) 2020 https://www.fda.gov/emergency‐preparedness‐and‐response/counterterrorism‐and‐emerging‐threats/coronavirus‐disease‐2019‐covid‐19 accessed April 6, 2020.
- 17. Centers for Disease Control and Prevention , Interim Infection Prevention and Control Guidance for Dental Settings During the COVID‐19 Response 2020 https://www.cdc.gov/coronavirus/2019‐ncov/hcp/dental‐settings.html, accessed April 6, 2020
- 18. Ather A, Patel B, Ruparel NB, Diogenes A, Hargreaves KM. Coronavirus Disease 19 (COVID‐19): Implications for Clinical Dental Care. J Endod. 2020;46(5):584‐595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. O*NET Resource Center , O*NET® 24.2 Database 2020 https://www.onetonline.org/find/descriptor/result/4.C.2.c.1.b accessed April 6, 2020
- 20. Meng L, Hua F, Bian Z. Coronavirus Disease 2019 (COVID‐19): Emerging and Future Challenges for Dental and Oral Medicine. J Dent Res. 2020;99(5):481‐487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Miller KT, Hannum WM, Morley T, Proffit WR. Use of recorded interactive seminars in orthodontic distance education. Am J Orthod Dentofacial Orthop. 2007;132(3):408‐414. [DOI] [PubMed] [Google Scholar]
- 22. Reynolds PA, Eaton KA, Mason R. Seeing is believing: dental education benefits from developments in videoconferencing. Br Dent J. 2008;204(2):87‐92. [DOI] [PubMed] [Google Scholar]
- 23. Sean F.Europe surpasses 100,000 confirmed coronavirus deaths – how did we get here? 2020; https://www.weforum.org/agenda/2020/04/coronavirus‐deaths‐europe/ accessed August 21 2020
- 24. European Centers for Disease Prevention and Control . COVID‐19 situation update for the EU/EEA and the UK, as of 21 August 2020, 2020; https://www.ecdc.europa.eu/en/cases‐2019‐ncov‐eueea accessed August 21 2020
- 25. Johns Hopkins University of Medicine , Coronavirus Resource Center. Cumulative Cases By Days Since 50th Confirmed Case, https://coronavirus.jhu.edu/data/cumulative‐cases accessed August 21 2020
- 26. Stein R.Pandemic Is Overwhelming U.S. Public Health Capacity in Many States. What Now? The Coronavirus Crisis, 2020, https://www.npr.org/sections/health‐shots/2020/07/28/894858475/pandemic‐is‐overwhelming‐u‐s‐public‐health‐capacity‐in‐many‐states‐what‐now accessed August 21 2020.
- 27. Banga B.COVID‐19 is causing supply issues for ventilators in France, https://www.bioworld.com/articles/433964‐covid‐19‐is‐causing‐supply‐issues‐for‐ventilators‐in‐france, accessed April 6 2020
- 28. National Center of Security and Crises Management . 2020. COVID‐19 Preparedness 2020 http://www.ncscm.gov.jo/index.php accessed April 6
- 29. Jordan News Agency , Jordan COVID‐19 Daily Wrap‐up 2020 https://petra.gov.jo/Include/Main.jsp?lang=en, 2020 accessed April 6, 2020.
- 30. Centers for Disease Control and Prevention , Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID‐19)‐United States, February 12‐March 16, 2020. https://www.cdc.gov/mmwr/volumes/69/wr/mm6912e2.htm?s_cid=mm6912e2_w, accessed April 6, 2020.
- 31. Brondani M, Donnelly L. COVID‐19 pandemic: Students' perspectives on dental geriatric care and education. J Dent Educ. 2020;84(11):1237–1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Harnish DA, Heimbuch BK, Husband M, et al. Challenge of N95 filtering facepiece respirators with viable H1N1 influenza aerosols. Infect Control Hosp Epidemiol. 2013;34(5):494‐499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Tiwari M, Mishra D. Investigating the genomic landscape of novel coronavirus (2019‐nCoV) to identify non‐synonymous mutations for use in diagnosis and drug design. J Clin Virol. 2020;128:104441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lindsley WG, Noti JD, Blachere FM, Szalajda JV, Beezhold DH. Efficacy of face shields against cough aerosol droplets from a cough simulator. J Occup Environ Hyg. 2014;11(8):509‐518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Perencevich EN, Diekema DJ, Edmond MB. Moving Personal Protective Equipment Into the Community: Face Shields and Containment of COVID‐19. JAMA. 2020;323(22):2252‐2253. [DOI] [PubMed] [Google Scholar]
- 36. Samaranayake LP, Reid J, Evans D. The efficacy of rubber dam isolation in reducing atmospheric bacterial contamination. ASDC J Dent Child. 1989;56(6):442‐444. [PubMed] [Google Scholar]
- 37. Iyer P, Aziz K, Ojcius DM. Impact of COVID‐19 on dental education in the United States. J Dent Educ. 2020;84(6):718‐722. [DOI] [PubMed] [Google Scholar]
- 38. Peres KG, Reher P, Castro RDD, Vieira AR. COVID‐19‐Related Challenges in Dental Education: Experiences From Brazil, the USA, and Australia. Pesqui Bras Odontopediatria Clin Integr. 2020;20:130. [Google Scholar]
- 39. Coulthard P. Dentistry and coronavirus (COVID‐19) ‐ moral decision‐making. Br Dent J. 2020;228(7):503‐505. [DOI] [PubMed] [Google Scholar]
- 40. Alzahrani SB, Alrusayes AA, Aldossary MS. Impact of COVID‐19 Pandemic on Dental Education, Research, and Students. IJHSR. 2020;10(6):207‐212. [Google Scholar]
- 41. Frisch L. Here’s how you can access textbooks for free during the coronavirus lockdown. The Source, https://www.springernature.com/gp/researchers/the‐source/blog/blogposts‐life‐in‐research/access‐textbooks‐for‐free‐during‐the‐coronavirus‐lockdown/17897628 accessed August 21, 2020
- 42. Chen MS, Horrocks EN, Evans RD. Video versus lecture: effective alternatives for orthodontic auxiliary training. Br J Orthod. 1998;25(3):191‐195. [DOI] [PubMed] [Google Scholar]
- 43. Knosel M, Jung K, Bleckmann A. YouTube, dentistry, and dental education. J Dent Educ. 2011;75(12):1558‐1568. [PubMed] [Google Scholar]
- 44. McAndrew M, Johnston AE. The role of social media in dental education. J Dent Educ. 2012;76(11):1474‐1481. [PubMed] [Google Scholar]
- 45. Loch C, Kuan IBJ, Elsalem L, Schwass D, Brunton PA, Jum'ah A. COVID‐19 and dental clinical practice: Students and clinical staff perceptions of health risks and educational impact. J Dent Educ. 2020;10:1‐9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable to this article as no data sets were generated or analysed during the current study.


