Dear Editor,
Recent articles have highlighted the impact of infectious diseases, and coronavirus disease (COVID‐19) 1 , 2 , 3 in a developing country Pakistan, 4 , 5 , 6 and their drastic outcomes are still going on. The outbreak of COVID‐19 was stated a pandemic by the World Health Organization (WHO) on March 11, 2020, by the novel severe acute respiratory syndrome coronavirus (SARS‐CoV‐2) primarily reported in Wuhan, China. 7 By November 12, more than one million deaths in this pandemic occurred in 219 different countries, with more than 50 million confirmed cases worldwide. 8 , 9 Alarmingly, in Pakistan, the number of COVID cases increasing rapidly (328,602 cases), with the death toll exceeding 1 million, as shown in Figure 1A,B. 8 Simultaneously, as the peak season of H1N1 influenza approaches, the ongoing catastrophic effect of COVID‐19 is becoming more devastating and severe. Due to numerous facilities, services, and financial restrictions, these coepidemics create havoc and bends double the existing delipidated healthcare system. 10
Figure 1.
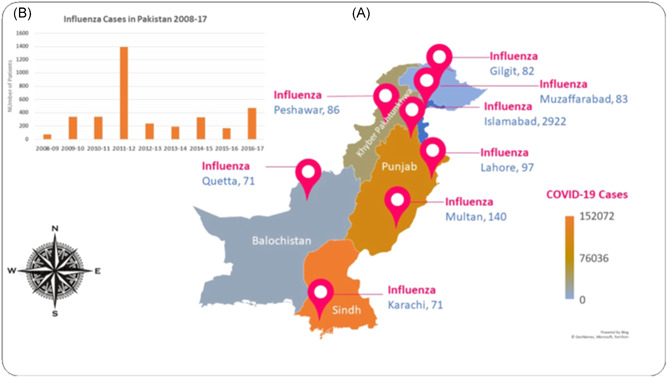
(A) Highlighting the COVID‐19 and influenza prevalence in the different geographical areas of Pakistan. (B) The number of influenza cases observed from the year 2008–2017 in Pakistan. Data is accessed by Nisar et al. 20
Similar transmitting features of the influenza H1N1 have been established with COVID‐19, comprising direct communication (human‐to‐human) and aerosols or airborne droplet. 11 , 12 However, both viral diseases' clinical manifestations are more similar including, headache, fever, mild cough, diarrhea, sore throat, dyspnea, and generalize muscle ache, as shown in Figure 2A,B. 13 Conversely, there are few clinical and epidemiological differences: influenza cases can be asymptomatic owing to herd immunity, and clinically mild to moderate symptoms may develop in the majority of patients, whereas most COVID‐19 patients display signs within 5–7 days of infection and severe symptoms may be reported. 12 , 14
Figure 2.
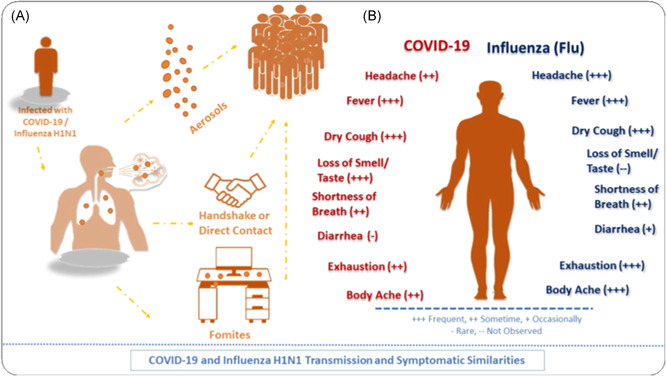
(A) Transmission similarities of both SARS‐CoV‐2 and the Influenza H1N1. (B) Common symptoms exhibit by both respiratory viruses COVID‐19 and Influenza (Data collected by Centers for Disease Control and Prevention)
Pakistan is the fifth‐largest country in the world, with more than 216 million people 15 and geographically located in South‐East Asia bearing tropical to moderate climate conditions. 16 In the tropics and subtropical regions, a swift increase in influenza cases has been recorded. 17 According to the WHO Recommendations, influenza should be vaccinated annually to high‐risk individuals, such as health workers, infants, pregnant and immunocompromised patients. Dreadfully, to date, Pakistan does not have an official policy on influenza vaccines. 16 , 18 In Pakistan, nearly 20,000 children are admitted to hospitals annually due to flu‐based symptoms and children at 5–14 years of age were more likely to be sick than elders. 18
In coinfected patients, Pakistan tends to have additional problems, particularly in the upcoming winter season, due to more widespread respiratory viruses, including influenza H1N1. It becomes crucial if patients have COVID‐19 indications, but their tests for SARS‐CoV‐2 are negative; in contrast, positive for other viruses. 13 , 19 In conclusion, the misdiagnosis of COVID‐19 by false‐negative or influenza virus infection may severely impact Pakistan's current overwhelmed health system. For effective etiological detection and clinical management, more robust viral testing is therefore required. Additionally, vaccination programs for flu should be launched on a massive scale in Pakistan to overcome the second wave of COVID‐19, which is predicted in the forthcoming peak influenza season.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Ding Q, Lu P, Fan Y, Xia Y, Liu M. The clinical characteristics of pneumonia patients coinfected with 2019 novel coronavirus and influenza virus in Wuhan, China. J Med Virol. 2020;92:1549‐1555. 10.1002/jmv.25781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gayam V, Konala VM, Naramala S, et al. Presenting characteristics, comorbidities, and outcomes of patients coinfected with COVID‐19 and Mycoplasma pneumoniae in the USA. J Med Virol. 2020;92:2181‐2187. 10.1002/jmv.26026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ribeiro VST, Telles JP, Tuon FF. Arboviral diseases and COVID‐19 in Brazil: concerns regarding climatic, sanitation and endemic scenario. J Med Virol. 2020;92:2390‐2391. 10.1002/jmv.26079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Haqqi A, Awan UA, Ali M, Saqib MAN, Ahmed H, Afzal MS. COVID‐19 and dengue virus co‐epidemics in Pakistan: a dangerous combination for overburdened healthcare system. J Med Virol. 2020. 10.1002/jmv.26144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Haqqi A, Khurram M, Din MSU, et al. COVID‐19 and Salmonella Typhi co‐epidemics in Pakistan: a real problem. J Med Virol. 2020. 10.1002/jmv.26293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Awan UA, Zahoor S, Ayub A, Ahmed H, Aftab N, Afzal MS. COVID‐19 and arboviral diseases: another challenge for Pakistan's delipidated healthcare system. J Med Virol. 2020. 10.1002/jmv.26668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Erkhembayar R, Dickinson E, Badarch D, et al. Early policy actions and emergency response to the COVID‐19 pandemic in Mongolia: experiences and challenges. Lancet Global Health. 2020;8:e1234‐e1241. 10.1016/s2214-109x(20)30295-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.COVID‐19 Weekly Epidemiological Update. 2020. https://www.who.int/publications/m/item/weekly-epidemiological-update-27-october-2020. Accessed October 27, 2020.
- 9.COVID‐19 Coronavirus Pandemic. 2020. https://www.worldometers.info/coronavirus/. Accessed November 12, 2020.
- 10. Shaikh BT, Ali N. COVID‐19 and fiscal space for health system in Pakistan: it is time for a policy decision. Int J Health Plan Manag. 2020;35:813‐817. 10.1002/hpm.2986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zhang N, Wang L, Deng X, et al. Recent advances in the detection of respiratory virus infection in humans. J Med Virol. 2020;92(4):408‐417. 10.1002/jmv.25674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jiang C, Yao X, Zhao Y, et al. Comparative review of respiratory diseases caused by coronaviruses and influenza A viruses during epidemic season. Microb Infect. 2020;22:236‐244. 10.1016/j.micinf.2020.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ozaras R, Cirpin R, Duran A, et al. Influenza and COVID‐19 co‐infection: report of 6 cases and review of the Literature. J Med Virol. 2020;92:2657‐2665. 10.1002/jmv.26125 [DOI] [PubMed] [Google Scholar]
- 14. Konala VM, Adapa S, Gayam V, et al. Co‐infection with Influenza A and COVID‐19. Eur J Case Rep Internal Med. 2020;7(5):1. 10.12890/2020_001656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fatima Z. Dengue infection in Pakistan: not an isolated problem. Lancet Infect Dis. 2019;19(12):1287‐1288. 10.1016/s1473-3099(19)30621-8 [DOI] [PubMed] [Google Scholar]
- 16. Nisar N, Badar N, Aamir UB, et al. Seasonality of influenza and its association with meteorological parameters in two cities of Pakistan: a time series analysis. PLOS One. 2019;14(7):e0219376. 10.1371/journal.pone.0219376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lowen AC, Steel J. Roles of humidity and temperature in shaping influenza seasonality. J Virol. 2014;88(14):7692‐7695. 10.1128/jvi.03544-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Farrukh MJ, Ming LC, Zaidi ST, Khan TM. Barriers and strategies to improve influenza vaccination in Pakistan. J Infect Public Health. 2017;10(6):881‐883. 10.1016/j.jiph.2016.11.021 [DOI] [PubMed] [Google Scholar]
- 19. Hashemi SA, Safamanesh S, Ghasemzadeh‐Moghaddam H, Ghafouri M, Azimian A. High prevalence of SARS‐CoV‐2 and influenza A virus (H1N1) coinfection in dead patients in Northeastern Iran. J Med Virol. 2020. 10.1002/jmv.26364 [DOI] [PubMed] [Google Scholar]
- 20. Nisar N, Aamir UB, Badar N, et al. Epidemiology of Influenza among patients with influenza‐like illness and severe acute respiratory illness in Pakistan: a 10‐year surveillance study 2008‐17. J Med Virol. 2020;92:3028‐3037. 10.1002/jmv.25913 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


