The spreading of SARS‐CoV‐2 disease by infected, asymptomatic subjects is one of the greatest concerns in controlling the pandemic (Gandhi et al., 2020), especially in the dental setting, where the aerosol generated by dental handpieces (Harrel & Molinari, 2004) that contaminates virtually any dental operatory surface (Ionescu et al., 2020) may substantially increase the risk of SARS‐CoV‐2 airborne transmission (Ge et al., 2020).
In the struggle to reduce the risk of such infection by dental aerosols and spatter, two non‐mutually exclusive strategies have been proposed: enhancing protection through personal protective equipment (PPE) (Herron et al., 2020) and mitigating aerosol spreading, for instance using high‐volume evacuator (HVE) (Ravenel et al., 2020) and adding antiviral agents to the cooling spray of dental handpieces. We designed a study to evaluate in vitro the protective efficacy of different types of PPEs, and the efficiency of a hydrogen peroxide‐based spray in reducing a coronavirus viral load, similar to that of asymptomatic patients, dispersed during a conventional dental procedure.
Into a class III cabinet‐like, pressure‐tight, custom‐built chamber, dental practice was reproduced using phantom heads for both patient and operator, and a routine procedure using aerosol‐generating air turbine was performed (Figure 1). An artificial saliva solution containing 6.03 ± 0.04 log10 gene copies/ml of coronavirus 229E (the amount of viral load of an asymptomatic person) (Han et al., 2020) was inserted into a patient‐simulating phantom dummy, before operating the air turbine with the air spray for 10 s. The operator phantom was equipped with different types of PPE on several consecutive runs, including surgical masks, N95/FFP2 and FFP3 respirators, and face shields, while a vacuum pump simulated the operator's breathing. The influence of HVE and the addition of 0.5 vol% H2O2 to the handpiece's water intake in mitigating viral loads were also tested. After performing the dental procedure, the viral presence on the operator was assessed on its forehead, on masks’ and respirators' outer surface, and inside the mouth of the phantom (Table 1).
FIGURE 1.
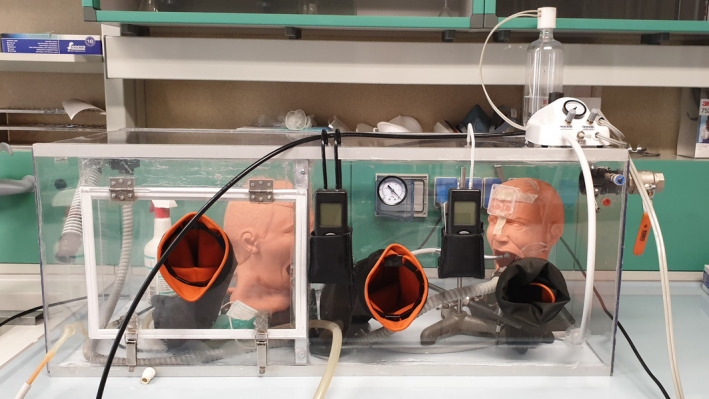
Setup of the custom‐built Class III‐like air‐tight glove box with chamber pressure control. Three accesses for gloves are shown on the front panel, one created at the center of the door. Between glove apertures, two digital manometers and a backup analog manometer measured the negative pressure inside the chamber, and the differential pressure inside the mouth of the operator dummy when a mask or respirator covered its mouth and nose. On the upper right corner of the chamber, the two air leak valves for pressure control are visible .The control apparatus operating the air turbine is located on the right part of the upper panel, having attached the pressurized water tank to generate the air‐water cooling spray for the turbine handpiece. Inside the chamber, on the right was situated the patient phantom, having the air‐turbine and HVE tip fixed in the same position throughout all experimental runs, as if operated by a dentist and dental assistant. On the left, the operator phantom to be equipped with the tested PPE. The chamber is still to be connected to an oil‐free air compressor, HVE line, and two low‐vacuum pumps, here not shown.
TABLE 1.
Results (mean ± SD) of the log‐transformed viral copies per square centimeter for each experimental run and target
| Exp. run | Target | PPE configuration | Suction | Log10 viral copies/cm2 |
|---|---|---|---|---|
| 1 | Mouth | With surgical mask | NO HVE | 0.317 ± 0 * c |
| 2 | Mouth | With surgical mask | HVE | 0.317 ± 0 * c |
| 3 | Mouth | With FFP2 mask | HVE | 0.317 ± 0 * c |
| 4 | Mouth | With FFP3 mask | HVE | 0.317 ± 0 * c |
| 5 | Mouth | With surgical mask and face shield | HVE | 0.317 ± 0 * c |
| 6 | Mouth | With FFP2 mask and face shield | HVE | 0.317 ± 0 * c |
| 7 | Mouth | With surgical mask + H2O2 30 s | NO HVE | 0.317 ± 0 * c |
| 8 | Mouth | With surgical mask + H2O2 60 s | NO HVE | 0.317 ± 0 * c |
| 1 | Mask | With surgical mask | NO HVE | 1.249 ± 0.372 a |
| 2 | Mask | With surgical mask | HVE | 1.214 ± 0.538 a |
| 3 | Mask | With FFP2 mask | HVE | 1.365 ± 0.519 a |
| 4 | Mask | With FFP3 mask | HVE | 1.391 ± 0.630 a |
| 5 | Mask | With surgical mask and face shield | HVE | 0.317 ± 0 * c |
| 6 | Mask | With FFP2 mask and face shield | HVE | 0.317 ± 0 * c |
| 7 | Mask | With surgical mask + H2O2 30 s | NO HVE | 0.317 ± 0 * c |
| 8 | Mask | With surgical mask + H2O2 60 s | NO HVE | 0.317 ± 0 * c |
| 1 | Forehead | With surgical mask | NO HVE | 0.783 ± 0.212 b |
| 2 | Forehead | With surgical mask | HVE | 0.711 ± 0.164 b |
| 3 | Forehead | With FFP2 mask | HVE | 0.698 ± 0.160 b |
| 4 | Forehead | With FFP3 mask | HVE | 0.776 ± 0.205 b |
| 5 | Forehead | With surgical mask and face shield | HVE | 0.633 ± 0.076 b |
| 6 | Forehead | With FFP2 mask and face shield | HVE | 0.669 ± 0.177 b |
| 7 | Forehead | With surgical mask + H2O2 30 s | NO HVE | 0.317 ± 0* c |
| 8 | Forehead | With surgical mask + H2O2 60 s | NO HVE | 0.317 ± 0* c |
Different letters indicate significant differences between groups (Tukey's test, p < .05).
Under the detection limit, determined to be equal to 4 viral copies/sample.
We detected very low viral loads on the external targets compared to the inoculum, suggesting that the aerosol generated by dental handpieces may have low viral content.
Unsurprisingly, we found the highest viral loads over the external surfaces of mask and respirators when a face shield was not worn, confirming that great attention has to be paid when disposing of used masks and respirators. Conversely, when the shield was on, viral loads on masks/respirators surfaces were under the detection limit, demonstrating shield efficacy.
Importantly, inside the operator's mouth, the viral load was under the detection limit using any PPE, with no differences between surgical masks and respirators, all of which showing protection against the virus. These data agree with the findings of Loeb et al., who did not found differences in the efficacy of surgical masks compared to N95 respirators against influenza virus (Loeb et al., 2009).
Notably, when the 0.5 vol% H2O2‐containing cooling spray was used, the viral load was under the detection limit on any tested surface or target, confirming previous findings on the virucidal activity of hydrogen peroxide, probably due to an excess generation of reactive oxygen species with a denaturing effect on viral proteins and nucleic acids (Saini et al., 2020). In fact, vaporizing hydrogen peroxide may have enhanced its activity (Saini et al., 2020). Finally, and surprisingly, HVE showed no impact in mitigating the viral load reaching the operator.
In conclusion, the concomitant use of face shield and surgical mask or N95/FFP2 respirator, and a 0.5 vol% H2O2‐containing cooling spray, seems to confer a very high level of protection, drastically reducing the possibility of coronavirus transmission during the execution of dental procedures.
CONFLICT OF INTEREST
The authors have nothing to disclose.
AUTHOR CONTRIBUTION
Andrei Cristian Ionescu: Conceptualization; Methodology; Writing‐original draft. Eugenio Brambilla: Conceptualization; Validation; Writing‐original draft. Lamberto Manzoli: Formal analysis; Resources; Writing‐review & editing. Giovanna Orsini: Writing‐review & editing. Valentina Gentili: Data curation; Methodology. Roberta Rizzo: Data curation; Writing‐review & editing.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/odi.13736.
ACKNOWLEDGEMENTS
The authors wish to acknowledge SISOPD (Società Italiana Stomatologia Odontoiatria Protesi Dentaria—Italian Society of Dentistry, Stomatology, and Prosthodontics) Foundation, and ANDI (Associazione Nazionale Dentisti Italiani—Italian Dental Association) Progetti S.r.l. for supporting this study. The sponsors had no role on the design, analysis, and interpretation of the study.
Ionescu AC, Brambilla E, Manzoli L, Orsini G, Gentili V, Rizzo R. Efficacy of personal protective equipment and H2O2‐based spray against coronavirus in dental setting. Oral Dis.2022;28(Suppl. 1):1010–1012. 10.1111/odi.13736
REFERENCES
- Gandhi, M. , Yokoe, D. S. , & Havlir, D. V. (2020). Asymptomatic transmission, the Achilles’ heel of current strategies to control COVID‐19. New England Journal of Medicine, 382, 2158–2160. 10.1056/NEJMe2009758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ge, Z. Y. , Yang, L. M. , Xia, J. J. , Fu, X. H. , & Zhang, Y. Z. (2020). Possible aerosol transmission of COVID‐19 and special precautions in dentistry. Journal of Zhejiang University Science B, 16, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han, M. S. , Seong, M. W. , Kim, N. , Shin, S. , Cho, S. I. , Park, H. , Kim, T. S. , Park, S. S. , & Choi, E. H. (2020). Viral RNA load in mildly symptomatic and asymptomatic children with COVID‐19, Seoul, South Korea. Emerging Infectious Diseases, 26(10), 2497–2499. 10.3201/eid2610.202449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrel, S. K. , & Molinari, J. J. (2004). Aerosols and splatter in dentistry: A brief review of the literature and infection control implications. Journal of the American Dental Association, 135(4), 429–437. 10.14219/jada.archive.2004.0207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herron, J. B. , Hay‐David, A. G. , Gilliam, A. D. , & Brennan, P. A. (2020). Personal protective equipment and Covid 19‐a risk to healthcare staff? British Journal of Oral and Maxillofacial Surgery, 58(5), 500–502. 10.1016/j.bjoms.2020.04.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ionescu, A. C. , Cagetti, M. G. , Ferracane, J. L. , Garcia‐Godoy, F. , & Brambilla, E. (2020). Topographic aspects of airborne contamination caused by the use of dental handpieces in the operative environment. Journal of the American Dental Association, 151(9), 660–667. 10.1016/j.adaj.2020.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeb, M. , Dafoe, N. , Mahony, J. , John, M. , Sarabia, A. , Glavin, V. , Webby, R. , Smieja, M. , Earn, D. J. , Chong, S. , & Webb, A. (2009). Surgical mask vs N95 respirator for preventing influenza among health care workers: A randomized trial. Journal of the American Medical Association, 302(17), 1865–1871. 10.1001/jama.2009.1466 [DOI] [PubMed] [Google Scholar]
- Rautemaa, R. , Nordberg, A. , Wuolijoki‐Saaristo, K. , & Meurman, J. H. (2006). Bacterial aerosols in dental practice–a potential hospital infection problem? J Hospital Infect, 64(1), 76–81. 10.1016/j.jhin.2006.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravenel, T. D. , Kessler, R. , Comisi, J. C. , Kelly, A. , Renne, W. G. , & Teich, S. T. (2020). Evaluation of the spatter‐reduction effectiveness and aerosol containment of eight dry‐field isolation techniques. Quintessence International, 51(8), 660–670. [DOI] [PubMed] [Google Scholar]
- Saini, V. , Sikri, K. , Batra, S. D. , Kalra, P. , & Gautam, K. (2020). Development of a highly effective low‐cost vaporized hydrogen peroxide‐based method for disinfection of personal protective equipment for their selective reuse during pandemics. Gut Pathogens, 12(1), 1. 10.1186/s13099-020-00367-4 [DOI] [PMC free article] [PubMed] [Google Scholar]


