Abstract
There is evidence of increased incidence, rapid progression, and poor prognosis of COVID‐19 in patients with underlying comorbidities such as diabetes and epilepsy. Developing effective treatment regimens for COVID‐19 patients with multiple comorbidities is crucial, as patients' past medical history is an essential contributor to possible organ injuries in COVID‐19 patients. Herein, we report a confirmed case of COVID‐19 patient with a history of multiple underlying diseases, including diabetes, epilepsy, and gout. The patient developed multiple organ failure and died a week after intensive care unit (ICU) admission. Multiple organ failure is the most common cause of death in COVID‐19 patients.
Keywords: comorbidities, coronavirus, COVID‐19, diabetes, epilepsy
Developing effective treatment regimens for COVID‐19 patients with multiple comorbidities—especially diabetes and epilepsy—is crucial, as patients' past medical history is an essential contributor to possible organ injuries in COVID‐19 patients.
1. INTRODUCTION
In December 2019, an outbreak of unknown acute respiratory tract infection originated in Wuhan, China. 1 Shortly after first lower respiratory tract infection cases, the World Health Organization (WHO) named this newly emerged coronavirus as severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) and its resultant disease as coronavirus disease 2019 (COVID‐19). 2 , 3 Coronaviruses are a large class of viruses that often cause mild‐to‐moderate upper respiratory tract infection. However, three of them have arisen from animal sources in the past two decades, resulted in severe acute respiratory syndrome (SARS) and Middle East Respiratory Syndrome (MERS) epidemics as well as the novel COVID‐19 pandemic. 4 , 5 , 6
There is evidence of increased incidence, rapid progression, and poor prognosis of COVID‐19 in patients with underlying comorbidities. 7 , 8 Diabetes is a significant risk factor for hospitalization and adverse outcome in these patients, 9 , 10 , 11 as similar evidence was reported for two previous CoV infections, SARS and MERS. 4 , 5 , 12 Furthermore, diabetes is linked with an increased risk of thromboembolism among COVID patients, and D‐dimer levels have been confirmed to be directly proportionate to the severity of the disease. 13 Moreover, several studies have suggested epilepsy as a potential risk factor to morbidity and mortality in COVID‐19 patients; nevertheless, the association as of yet is unclear. 14 , 15 , 16
Herein, we report a confirmed case of COVID‐19 patient with a history of multiple underlying diseases, including diabetes, epilepsy, and gout. The patient died a week after intensive care unit (ICU) admission. We desire to highlight recesses in the knowledge that require further studies related to COVID‐19 in patients with underlying comorbidities.
2. CASE PRESENTATION
On 18 February 2020, a 47‐year‐old with acute respiratory syndrome, high fever (39.6 C), and severe shortness of breath was admitted to ICU at Ghaem Hospital in Karaj, Iran. Regarding strong suspicion of the COVID‐19 infection, complete laboratory tests and spiral chest‐computed tomography (CT) scan without contrast were performed for the patient. CT scan findings were consisted of bilateral ground‐glass opacities predominantly in lower zones, multiple atelectasis bilaterally in same regions, and elevation of right hemidiaphragm. No evidence of pericardial effusion, pleural fluid collection/thickening was reported. Imaging findings were characteristics of pneumonia attributed to SARS‐CoV‐2 (Figure 1). 17 , 18 , 19
FIGURE 1.
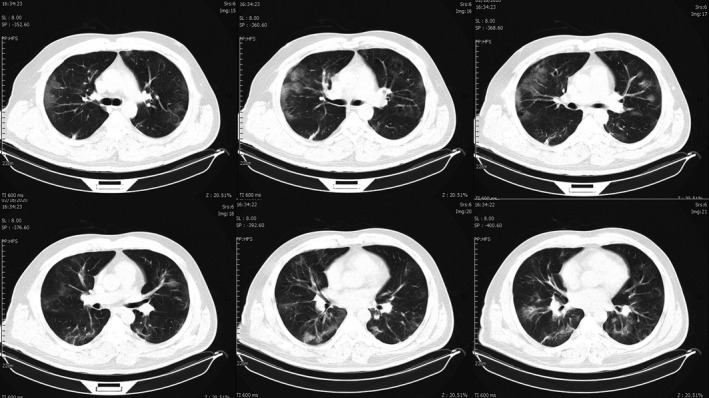
Chest CT images of the patient. Ground‐glass opacities are seen in both lungs, predominantly in lower zones. Multiple atelectasis is also seen in both lower zones
The patient had a history of epilepsy, gout (uric acid 9.0 mg/dL) and diabetes. Initial laboratory findings were described as follows: low white blood cells (WBC, 3400/microliter), high blood sugar (BS, 179 mg/dL), impaired liver function tests (SGOT/AST, 65 U/L and SGPT/ALT, 41 U/L), and low potassium (K, 3.2 mEq/L) (Table 1). On the first day of admission, the patient received 200 mg of hydroxychloroquine tablets twice daily (bd), 200 mg of lopinavir/ritonavir tablets twice daily (bd), and oseltamivir tablets 75 mg daily. On the second day, patient body temperature was reported 38.8 C and the Wright test was found negative. Moreover, liver enzymes SGOT/AST and SGPT/ALT were elevated to 85 and 56 U/L, respectively. Due to patient's history and an episode of seizure during hospitalization, levetiracetam 500 mg intravenous (IV) daily and levofloxacin tablets 750 mg daily were added to his treatment. On 3rd postadmission day, he had a 38°C fever. Sputum culture was performed, which came back negative 48 hours later. Naproxen tablet 500 mg daily was added to his medication. On the 7th postadmission day, the patient expired due to reduced oxygen pressure and asystole myocardial infarction.
TABLE 1.
Laboratory findings
| Date | 02/18 | 02/19 | 02/21 | 02/22 | 02/23 |
|---|---|---|---|---|---|
| WBC | 3400 | 4400 | 4800 | 7800 | |
| PaCo2 | 47 (40‐52) | 42 | 30.9 | ||
| PaO2 | 77.3 (80‐100) | 43 | 64 | ||
| Blood sugar | 179 | ||||
| SGOT (AST) | 65 | 85 | 138 | 144 | 90 |
| SGPT (ALT) | 41 | 56 | 90 | 101 | 93 |
| Total bilirubin |
1.5 mg/dL (0.1‐1.2) |
2.1 | 4.6 | ||
| CPK |
340 U/L (24‐195) |
||||
| Troponin I | 7.8 ng/L (negative) | ||||
| Prothrombin time (PT) |
14.7 s (12‐14) |
||||
| HBs Ag | Negative | ||||
| HCV Ab | Negative | ||||
| HIV Ab | Negative | ||||
| Urine protein | 3+ | ||||
| Urine bacteria | Moderate |
3. DISCUSSION
Underlying comorbidities are major risk factors for progression to critical illness and death in COVID‐19 patients. 7 , 8 Among them, our patient had history of diabetes and epilepsy, which are associated with altered immune system response and potential poor prognosis in COVID‐19 patients. 9 , 10 , 11 , 14 , 15 , 16 Weakened immune response might be related to mechanism in which these comorbidities modulate host‐viral or host‐immune system interactions. 20 , 21 Specifically, it has been demonstrated that diabetes is a major risk factor for in‐hospital mortality. Diabetes is also associated with an increased risk of thromboembolism in COVID‐19 patients, increasing disease severity and mortality. 13 Moreover, patient's urinary tract infection was assumed to be due to underlying comorbidities, especially diabetes and gout. 22 , 23 Development of acute kidney injury (AKI) in hospitalized COVID‐19 patients is a negative prognostic factor and ranges between 3% and 29%. Patient's proteinuria might be due to developed AKI during hospitalization which is highly associated with in‐hospital mortality. 24
The presented case developed multiple organ failure induced by COVID‐19. It is confirmed that COVID‐19 can cause cytokine storm, in which high pro‐inflammatory cytokines, as in the presented case, can lead to heart failure (CPK 340 U/L), liver failure (elevated SGOT, SGPT, and bilirubin), AKI, and respiratory failure (low PO2). Multiple organ failure is the most common cause of death in these patients. 25 , 26
It is crucial to develop effective treatment regimens for COVID‐19 patients with multiple comorbidities, as patients' past medical history is an essential contributor to possible organ injuries in these patients. Further observations will be required to comprehensively understand the full spectrum of COVID‐19 clinical features in patients with multiple comorbidities.
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTION
ARS, KM, FK, PF, and NR: Contributed to following criteria as described by the International Committee of Medical Journal Editors (ICMJE).
ETHICAL APPROVAL
Ethical approval is not necessary for retrospective studies and case presentations in our institutional policies.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient's next of kin for publication of this case report and any accompanying images.
ACKNOWLEDGMENT
We thank Mr Saeed Samaeinasab for assistance with writing the introduction section.
Safdarian AR, Momenzadeh K, Kahe F, Farhangnia P, Rezaei N. Death due to COVID‐19 in a patient with diabetes, epilepsy, and gout comorbidities. Clin Case Rep.2021;9:461–464. 10.1002/ccr3.3557
Amir Reza Safdarian and Kaveh Momenzadeh should be considered joint first author.
DATA AVAILABILITY STATEMENT
All data underlying the results are available as part of the article, and no additional source data are required.
REFERENCES
- 1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497‐506. 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565‐574. 10.1016/S0140-6736(20)30251-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hanaei S, Rezaei N. COVID‐19: developing from an outbreak to a pandemic. Arch Med Res. 2020;51(6):582‐584. 10.1016/j.arcmed.2020.04.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chan‐Yeung M, Xu RH. SARS: epidemiology. Respirology. 2003;8(Suppl):S9‐S14. 10.1046/j.1440-1843.2003.00518.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Morra ME, Van Thanh L, Kamel MG, et al. Clinical outcomes of current medical approaches for Middle East respiratory syndrome: a systematic review and meta‐analysis. Rev Med Virol. 2018;28(3):e1977 10.1002/rmv.1977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jabbari P, Jabbari F, Ebrahimi S, Rezaei N. COVID‐19: a chimera of two pandemics. Disaster Med Public Health Prep. 2020;14:1‐3. 10.1017/dmp.2020.223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zheng Z, Peng F, Xu B, et al. Risk factors of critical & mortal COVID‐19 cases: a systematic literature review and meta‐analysis. J Infect. 2020. 10.1016/j.jinf.2020.04.021 81(2):e16–e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID‐19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054‐1062. 10.1016/S0140-6736(20)30566-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Guo W, Li M, Dong Y, et al. Diabetes is a risk factor for the progression and prognosis of COVID‐19. Diabetes Metab Res Rev. 2020:e3319 10.1002/dmrr.3319. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hussain A, Bhowmik B, do Vale Moreira NC. COVID‐19 and diabetes: knowledge in progress. Diabetes Res Clin Pract. 2020;162:108142 10.1016/j.diabres.2020.108142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Singh AK, Gupta R, Ghosh A, Misra A. Diabetes in COVID‐19: prevalence, pathophysiology, prognosis and practical considerations. Diabetes Metab Syndr. 2020;14(4):303‐310. 10.1016/j.dsx.2020.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Huang YT, Lee YC, Hsiao CJ. Hospitalization for ambulatory‐care‐sensitive conditions in Taiwan following the SARS outbreak: a population‐based interrupted time series study. J Formos Med Assoc. 2009;108(5):386‐394. 10.1016/S0929-6646(09)60082-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Singhania N, Bansal S, Nimmatoori DP, Ejaz AA, McCullough PA, Singhania G. Current overview on hypercoagulability in COVID‐19. Am J Cardiovasc Drugs. 2020;20(5):393‐403. 10.1007/s40256-020-00431-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cabezudo‐Garcia P, Ciano‐Petersen NL, Mena‐Vazquez N, Pons‐Pons G, Castro‐Sanchez MV, Serrano‐Castro PJ. Incidence and case fatality rate of COVID‐19 in patients with active epilepsy. Neurology. 2020;95(10):e1417‐e1425. 10.1212/WNL.0000000000010033 [DOI] [PubMed] [Google Scholar]
- 15. Kuroda N. Epilepsy and COVID‐19: associations and important considerations. Epilepsy Behav. 2020;108:107122 10.1016/j.yebeh.2020.107122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yasri S, Wiwanikit V. COVID‐19 and Epilepsy. Ann Indian Acad Neurol. 2020;23(Suppl 1):S43 10.4103/aian.AIAN_254_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Brogna B, Bignardi E, Brogna C, et al. Typical CT findings of COVID‐19 pneumonia in patients presenting with repetitive negative RT‐PCR. Radiography (Lond). 2020; 10.1016/j.radi.2020.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708‐1720. 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Singhania N, Bansal S, Singhania G. An atypical presentation of novel coronavirus disease 2019 (COVID‐19). Am J Med. 2020;133(7):e365‐e366. 10.1016/j.amjmed.2020.03.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yazdanpanah F, Hamblin MR, Rezaei N. The immune system and COVID‐19: friend or foe? Life Sci. 2020;256:117900 10.1016/j.lfs.2020.117900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lotfi M, Rezaei N. SARS‐CoV‐2: a comprehensive review from pathogenicity of the virus to clinical consequences. J Med Virol. 2020;92(10):1864‐1874. 10.1002/jmv.26123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Singh JA, Cleveland JD. Serious infections in people with gout in the united states: a National study of incidence, time‐trends and outcomes. Arthritis Care Res (Hoboken). 2020. 10.1002/acr.24201 [DOI] [PubMed] [Google Scholar]
- 23. Bono MJ, Reygaert WC. Urinary Tract Infection. [Updated 2020 Jul 2]. 2020. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; Available from: https://www.ncbi.nlm.nih.gov/books/NBK470195/ [Google Scholar]
- 24. Cheng Y, Luo R, Wang K, et al. Kidney disease is associated with in‐hospital death of patients with COVID‐19. Kidney Int. 2020;97(5):829‐838. 10.1016/j.kint.2020.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rudrapal Mithun, Khairnar Shubham J., Borse Laxmikant B., Jadhav Anil G.. Coronavirus Disease‐2019 (COVID‐19): An Updated Review. Drug Research. 2020;70 (9): 389–400. 10.1055/a-1217-2397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sun YJ, Feng YJ, Chen J, Li B, Luo ZC, Wang PX. Clinical features of fatalities in patients with COVID‐19. Disaster Med Public Health Prep. 2020:1‐3. 10.1017/dmp.2020.235 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data underlying the results are available as part of the article, and no additional source data are required.


