Abstract
Purpose
To describe our experience concerning lung ultrasound (LUS) in the pediatric emergency clinic, and to investigate the diagnostic value of LUS in coronavirus disease‐2019 (COVID‐19).
Methods
Patients aged under 18 admitted to the pediatric emergency clinic with suspicion of COVID‐19, who underwent point‐of‐care LUS and from whom COVID‐19 reverse transcription polymerase chain reaction (RT‐PCR) samples were collected, were included in the study.
Results
Point‐of‐care LUS was performed on 74 patients in the emergency room. LUS findings were more sensitive than chest X‐ray in the early stages of the disease and in mild cases. Involvement was observed at LUS despite RT‐PCR being negative in some symptomatic patients with a COVID‐19 contact history.
Conclusions
We think that LUS can be beneficial in terms of identifying patients with lung involvement and staging their severity in this new disease in pediatric emergency clinics. The procedure is noninvasive, rapid, reproducible, and low cost, involving simple sterilization. Based on the current literature and our own practical experience, we think that increased use of point‐of‐care LUS can protect patients from unnecessary radiation and treatment delays during the COVID‐19 pandemic.
Keywords: COVID‐19, pandemic, pediatric, pneumonia, point‐of‐care lung ultrasound
1. INTRODUCTION
Patients with pneumonia caused by a new type of coronavirus infection appeared in Wuhan city in the Chinese province of Hubei in early December 2019, after which the disease spread rapidly and worldwide. 1 The World Health Organization named the disease caused by the new infection “coronavirus disease‐2019” (COVID‐19). 2 The clinical symptoms of COVID‐19 can range from a mild, self‐limiting flu‐like syndrome, to acute respiratory distress syndrome (ARDS), and life‐threatening multiorgan failure, and interstitial pneumonia. 3
Numerous previous studies have shown that lung ultrasound (LUS) is capable of detecting interstitial lung disease and subpleural consolidations. 4 , 5 , 6 In addition, evidence from recent studies has confirmed the usefulness of LUS in the diagnosis, management, and follow‐up of patients with COVID‐19 pneumonia. 7 , 8 , 9
Although several studies have investigated LUS in adult patients with COVID‐19, the literature for the pediatric age group is limited. The purpose of this study is to report our experiences concerning LUS in the pediatric emergency clinic, to investigate the diagnostic value of LUS in COVID‐19, and to gather evidence and contribute urgently needed information by retrospectively examining the point‐of‐care LUS findings of patients with fever or cough admitted to our pediatric emergency clinic with suspected COVID‐19.
2. MATERIALS AND METHODS
Patients aged under 18 admitted to the pediatric emergency clinic with suspected COVID‐19 between March 15, 2020 and May 10, 2020, who underwent point‐of‐care LUS, and from whom COVID‐19 reverse transcription polymerase chain reaction (RT‐PCR) samples were collected, were included in the study. Patient data were retrieved from patient files and the hospital automation system. Age, sex, COVID‐19 contact history, LUS findings, COVID‐19 RT‐PCR results, and chest X‐ray (CXR) findings were recorded. Patients not undergoing RT‐PCR or LUS, or with symptoms other than fever or cough were excluded from the study.
Sonographic lung evaluations were performed by a single operator (pediatric emergency specialist) with 4 years' experience of point‐of‐care LUS using a LOGIQ P9 (GE Healthcare, Wauwatosa, Wisconsin) ultrasound (US) device. LUS was performed using personal protective equipment and with all requisite precautions being taken against infection transmission. The US device was disinfected after each patient. A low‐frequency convex probe was used to evaluate lung parenchymal structures, and a high‐frequency linear probe was used to evaluate the pleural line. LUS was performed with patients in the sitting or supine positions, depending on their age. If the patient was in the sitting position, 14 segments of both hemithoraces, including anterior (superior/inferior), lateral (superior/inferior), and posterior (superior/medial/inferior) segments were examined. If the patient was in the supine position, eight segments including anterior (superior/inferior) and lateral (superior/inferior) segments were examined. LUS findings such as pleural thickening, pleural irregularity, subpleural consolidation, B lines, and white lung were recorded.
Statistical analysis was performed on Statistical Package for the Social Sciences for Windows Version 20.0 software. Categorical variables were expressed as n (%), while mean ± SD was used for continuous variables with normal distribution, and median (lower‐upper limit) values for continuous variables without normal distribution. Descriptive analyses were used to analyze the distribution and frequency of data, and the Chi‐square test was used to compare two independent groups. The independent t test was used to compare mean values in two independent groups. Significance was set at <.05 for all statistical analyses.
3. RESULTS
A total of 74 patients were included in the study. Fifty‐seven (77%) patients had histories of contact with a COVID‐19‐positive family member. RT‐PCR results were positive in 24 (32.4%) cases and negative in 50 (67.6%). Patients' epidemiological and clinical characteristics, and CXR and LUS findings are shown in Table 1.
TABLE 1.
Epidemiologic and clinical characteristics, and X‐ray and LUS findings of the COVID‐19 RT‐PCR‐positive and ‐negative patients
| COVID‐19 RT‐PCR positive (n = 24) | COVID‐19 RT‐PCR negative (n = 50) | Total (N = 74) | P | |
|---|---|---|---|---|
| Epidemiological features | ||||
| Female n (%) | 8 (33.3%) | 21 (42%) | 29 (39.2%) | >.05 |
| Male n (%) | 16 (66.7%) | 29 (58%) | 45 (60.8%) | >.05 |
| Age (mo) | 134 ± 51.93 | 101.36 ± 45.45 | 112.15 ± 39.31 | .023 |
| Patients with COVID‐19 contact in the family | 19 (79.2%) | 38 (76%) | 57 (77%) | >.05 |
| Symptoms | ||||
| Fever | 4 (16.7%) | 5 (10%) | 9 (12.2%) | >.05 |
| Cough | 7 (29.2%) | 27 (54%) | 34 (45.9%) | >.05 |
| Fever + cough | 13 (54.2) | 18 (36%) | 31 (41.9%) | >.05 |
| CXR findings | ||||
| Normal | 10 (41.7%) | 37 (74%) | 47 (63.5%) | .01 |
| Consolidation | 8 (33.3%) | 8 (16%) | 16 (21.6%) | >.05 |
| Peribronchial thickening | 4 (16.7%) | 5 (10%) | 9 (12.2%) | >.05 |
| Interstitial infiltration | 2 (8.3%) | 0 | 2 (2.7%) | >.05 |
| LUS findings | ||||
| Normal | 6 (25%) | 37 (74%) | 43 (58.1%) | <.001 |
| Patients with LUS findings | 18 (75%) | 13 (26%) | 31 (41.9%) | <.001 |
| Pleural irregularity | 18 (75%) | 13 (26%) | 31 (41.9%) | <.001 |
| Pleural thickening | 18 (75%) | 13 (26%) | 31 (41.9%) | <.001 |
| B line (focal) | 3 (12.5%) | 5 (10%) | 8 (10.8%) | >.05 |
| B line (focal and confluent) | 13 (54.2%) | 8 (16%) | 21 (28.4%) | <.001 |
| White lung | 13 (54.2%) | 8 (16%) | 21 (28.4%) | <.001 |
| Subpleural consolidation | 16 (66.7%) | 12 (24%) | 28 (37.8%) | <.001 |
Abbreviations: COVID‐19, coronavirus disease‐2019; CXR, chest X‐ray; LUS, lung ultrasound; RT‐PCR, reverse transcription polymerase chain reaction.
Comparison of the LUS findings of the groups with positive and negative RT‐PCR results revealed significantly greater LUS findings in 18 (75%) of the 24 positive patients (P = .001). Examination of the CXRs of the 31 patients with LUS findings revealed statistically significant findings in 27 (87.1%) (P = .001). Four (12.9%) patients had LUS findings, but normal CXRs.
LUS findings were determined in 31 (41.9%) patients, all of whom exhibited pleural thickening and irregularity. US images from patients with pleural thickening and irregularity are shown in Figure 1C, Figure 2A,C,D, and Figure 3D. B lines were observed in 29 (93.5%) of the 31 patients with LUS findings, these being focal in 8 (27.6%) cases and confluent in 21 (72.4%). US images from patients with focal B lines are shown in Figures 1B‐D and 2A,B,D, and images from patients with confluent B lines are shown in Figures 2C and 3C. White lung findings were observed in 21 (72.4%) patients with LUS findings, and subpleural consolidation areas of various sizes in 28 (90.3%). US images from patients with a white lung appearance are shown in Figures 2B,C and 3A‐C, and from patients with subpleural consolidation areas in Figures 2A‐C and 3A,B,D. Bilateral involvement was determined in 17 (54.8%) of the 31 patients with LUS findings, right lung involvement in 11 (35.5%), and left lung involvement in three (9.7%).
FIGURE 1.
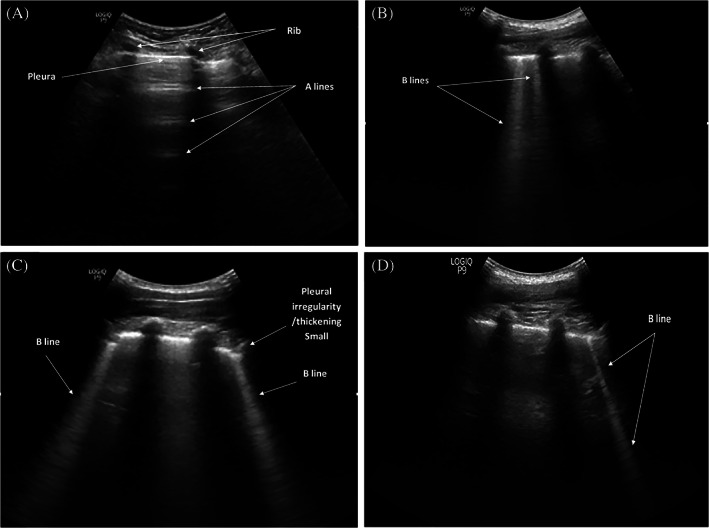
A, Normal lung sonogram. B, Focal B lines. C, Focal B lines, pleural thickening/irregularity, and small subpleural consolidation. D, Focal B lines
FIGURE 2.
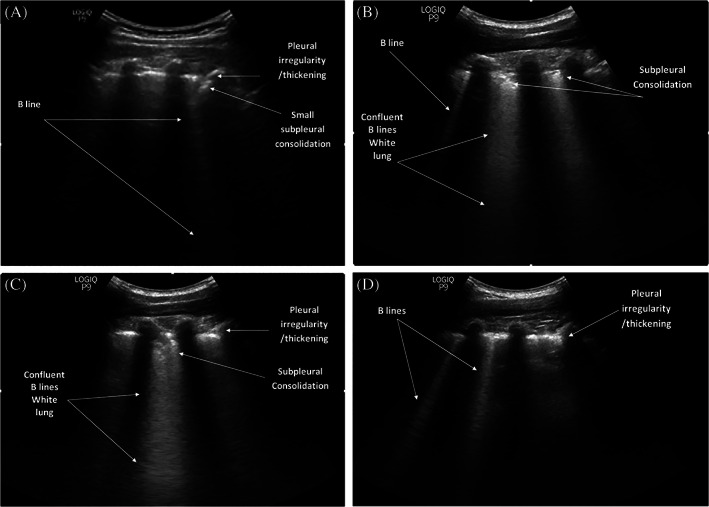
A, Focal B lines, pleural thickening/irregularity, and small subpleural consolidation. B, Focal and confluent B lines, subpleural consolidation, and white lung appearance. C, Pleural thickening/irregularity, subpleural consolidation, and white lung appearance. D, Pleural thickening/irregularity and focal B lines
FIGURE 3.
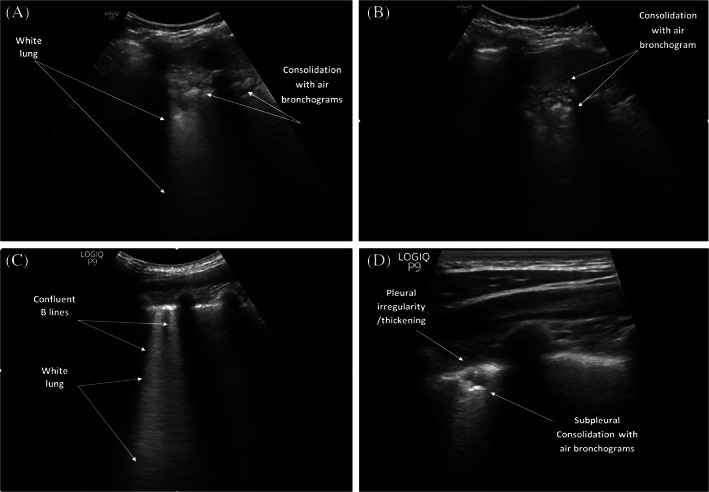
A, Lung ultrasound (LUS) shows white lung appearance and consolidations with air bronchograms. B, LUS shows consolidations with air bronchograms. C, Confluent B lines and white lung appearance. D, LUS image of pleural thickening/irregularity and consolidations with air bronchograms obtained using a linear transducer
Influenza RT‐PCR results in the emergency department were negative in all patients. No patients underwent thoracic computed tomography (CT). Treatment was started in all patients with LUS findings. No patients required intubation or intensive care unit hospitalization.
4. DISCUSSION
This study examines the point‐of‐care LUS findings of patients admitted to our pediatric emergency department with a suspicion of COVID‐19 and with fever or cough. LUS findings were found to be more sensitive than CXR in the early stages of the disease and in mild cases. In addition, involvement was observed at LUS despite RT‐PCR being negative in some symptomatic patients with a COVID‐19 contact history.
Studies in recent years have shown that LUS can detect interstitial lung disease, subpleural consolidations, and ARDS. 4 , 10 The fact that LUS can be performed quickly at the bedside, can reduce the use of tomography and CXR and can eliminate patient exposure to radiation, and its inexpensive, rapid, noninvasive, and reproducible nature have further encouraged its use in lung evaluations during the COVID‐19 pandemic. 11 , 12 Since the most important area of involvement of COVID‐19 is the pulmonary system, LUS performed by a trained physician can be useful in triage, the classification of disease severity, and treatment planning in the emergency department and intensive care unit.
LUS findings in patients with COVID‐19 are similar to those commonly described in other types of pneumonia. 13 Subpleural consolidations with indirect symptoms such as pleural thickening and irregularities, loss of A‐lines and an increase in B‐lines due to pulmonary diseases all occur. B‐lines in COVID‐19 pneumonia can appear in both separate and confluent forms, and B‐line clusters can give the appearance of a glowing white lung and radiate in the form of rays that maintain their brightness without fading to the edge of the screen. These artifacts represent typical signs of the disease, but can also be observed in other interstitial diseases of various etiologies. 14 Musolino et al 15 described vertical B artifacts, white lung areas, subpleural consolidations, and pleural irregularities as the main findings in pediatric COVID‐19 pneumonia in their LUS evaluation of 10 children. In another study involving a limited number of pediatric patient, Denina et al 16 detected small subpleural consolidations and B‐lines were detected. In agreement with the previous literature, we also detected pleural thickening and irregularity, B lines (focal and confluent), a white lung appearance, and subpleural consolidation in COVID‐19 pneumonia.
Although CXR has traditionally been used for the diagnosis of lung diseases, it may not be able to detect early‐stage COVID‐19 pneumonia. 17 Weinstock et al 18 examined CXRs obtained from symptomatic patients with confirmed COVID‐19 and found that CXRs were normal in 58.3% of patients, and normal or only mild findings at CXR in 89%. They concluded that there was no guarantee that CXR results would be normal. Denina et al 16 compared CXR and LUS findings in children and described them as compatible. Although CXR was normal in the present study, four (12.9%) patients had LUS findings. This suggests that point‐of‐care LUS will be useful in detecting early stage pneumonia in addition to mild COVID‐19 pneumonia and in terms of initiating early treatment, especially in childhood.
RT‐PCR has become the standard evaluation method for the diagnosis of COVID‐19 infection according to current diagnostic criteria. 19 However, the rates of false‐positive or false‐negative results are still unclear. 20 Thoracic CT is often recommended as a screening tool for adult patients with suspected COVID‐19 pneumonia. 21 Fang et al 22 reported higher sensitivity for thoracic CT than RT‐PCR in patients with COVID‐19 pneumonia (98% vs 71%, respectively, P < .001). Those authors also concluded that thoracic CT should be used in COVID‐19 screening for patients with clinical and epidemiological features compatible with COVID‐19. Ai et al 23 investigated the correlation between thoracic CT and RT‐PCR and similarly found that more than 70% of patients with negative RT‐PCR tests exhibited typical CT findings. In our clinic, we evaluated patients using CXR and LUS instead of thoracic CT in order to minimize radiation exposure in pediatric patients. Studies show that LUS findings are quite consistent with thoracic CT findings of COVID‐19 pneumonia and that LUS constitutes an alternative imaging method for identifying characteristic lesions. 24 , 25 Consistent with the existing literature, positive LUS findings were detected in 13 (26%) of 50 patients with negative RT‐PCR in the present study. Due the false‐negative results produced by RT‐PCR, rapid and accurate diagnostic methods are urgently needed to identify, isolate, and treat COVID‐19 as rapidly as possible. The use of thoracic CT is limited, particularly in childhood and among pregnant women, due to the effect of radiation. This suggests that LUS can represent a useful method for detecting lung abnormalities in children with COVID‐19 in the early stages, and that it can be used for screening, as an ancillary diagnostic method, and for patient follow‐up.
There are a number of limitations to the present study. First, the research presents observational data from a single center. The fact that LUS was performed by a single sonographer also resulted in a limited sample size. In addition, our patients admitted to the pediatric emergency clinic with suspected symptomatic COVID‐19 underwent LUS at the time of admission. This meant that the number of patients who were positive for RT‐PCR was relatively low. Larger multicenter studies are therefore now needed to establish protocols for the use of point‐of‐care LUS in pediatric emergency clinics. Despite these limitations, our study is one of the largest to examine the use of point‐of‐care LUS in the COVID‐19 pandemic in children.
We conclude that as a noninvasive, rapid, and reproducible procedure, also involving ease of sterilization and low costs, LUS can be useful in identifying patients with lung involvement and in staging their severity in this new disease in pediatric emergency clinics. Based on the current evidence concerning COVID‐19 and our own practical experience, we think increased use of point‐of‐care LUS during the COVID‐19 pandemic can protect patients from unnecessary exposure to radiation and treatment delays.
Türe E, Korkmaz MF, Aksoy FD, et al. Point‐of‐care lung ultrasound findings in the pediatric emergency clinic during the COVID‐19 pandemic. J Clin Ultrasound. 2021;49:85–90. 10.1002/jcu.22947
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- 1. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus‐infected pneumonia. N Engl J Med. 2020;382:1199‐1207. 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Singhal T. A review of coronavirus disease‐2019 (COVID‐19). Indian J Pediatr. 2020;87:281‐286. 10.1007/s12098-020-03263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708‐1720. 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mojoli F, Bouhemad B, Mongodi S, Lichtenstein D. Lung ultrasound for critically ill patients. Am J Respir Crit Care Med. 2019;199:701‐714. 10.1164/rccm.201802-0236CI. [DOI] [PubMed] [Google Scholar]
- 5. Mayo PH, Copetti R, Feller‐Kopman D, et al. Thoracic ultrasonography: a narrative review. Intensive Care Med. 2019;45:1200‐1211. 10.1007/s00134-019-05725-8. [DOI] [PubMed] [Google Scholar]
- 6. Soldati G, Smargiassi A, Inchingolo R, et al. Lung ultrasonography and vertical artifacts: the shape of air. Respiration. 2015;90:86. 10.1159/000430483. [DOI] [PubMed] [Google Scholar]
- 7. Peng QY, Wang XT, Zhang LN. Chinese critical care ultrasound study group (CCUSG). Findings of lung ultrasonography of novel corona virus pneumonia during the 2019‐2020 epidemic. Intensive Care Med. 2020;46:849‐850. 10.1007/s00134-020-05996-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Soldati G, Smargiassi A, Inchingolo R, et al. Is there a role for lung ultrasound during the COVID‐19 pandemic? J Ultrasound Med. 2020;39:1459‐1462. 10.1002/jum.15284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Secco G, Delorenzo M, Zattera C, et al. Lung ultrasound in Covid‐19: a useful diagnostic tool. Emerg Care J. 2020;16:35‐38. [Google Scholar]
- 10. Soldati G, Demi M, Smargiassi A, Inchingolo R, Demi L. The role of ultrasound lung artifacts in the diagnosis of respiratory diseases. Expert Rev Respir Med. 2019;13:163‐172. 10.1080/17476348.2019.1565997. [DOI] [PubMed] [Google Scholar]
- 11. Moore S, Gardiner E. Point of care and intensive care lung ultrasound: A reference guide for practitioners during COVID‐19. Radiography. 2020;26(4):e297‐e302. 10.1016/j.radi.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Volpicelli G, Lamorte A, Villén T. What's new in lung ultrasound during the COVID‐19 pandemic. Intensive Care Med. 2020;46:1445‐1448. 10.1007/s00134-020-06048-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Volpicelli G, Elbarbary M, Blaivas M, et al. International evidence‐based recommendations for point‐of‐care lung ultrasound. Intensive Care Med. 2012;38:577‐591. 10.1007/s00134-012-2513-4. [DOI] [PubMed] [Google Scholar]
- 14. Volpicelli G, Gargani L. Sonographic signs and patterns of COVID‐19 pneumonia. Ultrasound J. 2020;12:22. 10.1186/s13089-020-00171-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Musolino AM, Supino MC, Buonsenso D, et al. Lung ultrasound in children with COVID‐19: preliminary findings. Ultrasound Med Biol. 2020;46:2094‐2098. 10.1016/j.ultrasmedbio.2020.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Denina M, Scolfaro C, Silvestro E, et al. Lung ultrasound in children with COVID‐19. Pediatrics. 2020;146(1):e20201157. 10.1542/peds.2020-1157. [DOI] [PubMed] [Google Scholar]
- 17. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507‐513. 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Weinstock MB, Echenique A, DABR JWR, et al. Chest X‐ray findings in 636 ambulatory patients with COVID‐19 presenting to an urgent care center: a Normal chest X‐ray is no guarantee. J Urgent Care Med. 2020;14:13‐18. [Google Scholar]
- 19. Corman VM, Landt O, Kaiser M, et al. Detection of 2019 novel coronavirus (2019‐nCoV) by real‐time RT‐PCR. Euro Surveill. 2020;25(3):2000045. 10.2807/1560-7917.ES.2020.25.3.200004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Long C, Xu H, Shen Q, et al. Diagnosis of the coronavirus disease (COVID‐19): rRT‐PCR or CT? Eur J Radiol. 2020;126:108961. 10.1016/j.ejrad.2020.108961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Caruso D, Zerunian M, Polici M, et al. Chest CT features of COVID‐19 in Rome, Italy. Radiology. 2020;296(2):E79‐E85. 10.1148/radiol.2020201237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Fang Y, Zhang H, Xie J, et al. Sensitivity of chest CT for COVID‐19: comparison to RT‐PCR. Radiology. 2020;296(2):E115‐E117. 10.1148/radiol.2020200432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ai T, Yang Z, Hou H, et al. Correlation of chest CT and RT‐PCR testing for coronavirus disease 2019 (COVID‐19) in China: a report of 1014 cases. Radiology. 2020;296(2):E32‐E40. 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Huang Y, Wang S, Liu Y, et al. A preliminary study on the ultrasonic manifestations of peripulmonary lesions of non‐critical novel coronavirus pneumonia (COVID‐19). https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3544750. Accessed February 26, 2020.
- 25. Poggiali E, Dacrema A, Bastoni D, et al. Can lung US help critical care clinicians in the early diagnosis of novel coronavirus (COVID‐19) pneumonia? Radiology. 2020;295(3):E6. 10.1148/radiol.2020200847. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


