Abstract
Background
Containment of the coronavirus disease 2019 (COVID‐19) pandemic requires the public to change behavior under social distancing mandates. Social media are important information dissemination platforms that can augment traditional channels communicating public health recommendations. The objective of the study was to assess the effectiveness of COVID‐19 public health messaging on Twitter when delivered by emergency physicians and containing personal narratives.
Methods
On April 30, 2020, we randomly assigned 2,007 U.S. adults to an online survey using a 2 × 2 factorial design. Participants rated one of four simulated Twitter posts varied by messenger type (emergency physician vs. federal official) and content (personal narrative vs. impersonal guidance). The main outcomes were perceived message effectiveness (35‐point scale), perceived attitude effectiveness (PAE; 15‐point scale), likelihood of sharing Tweets (7‐point scale), and writing a letter to their governor to continue COVID‐19 restrictions (write letter or none).
Results
The physician/personal (PP) message had the strongest effect and significantly improved all main messaging outcomes except for letter writing. Unadjusted mean differences between PP and federal/impersonal (FI) were as follows: perceived messaging effectiveness (3.2 [95% CI = 2.4 to 4.0]), PAE (1.3 [95% CI = 0.8 to 1.7]), and likelihood of sharing (0.4 [95% CI = 0.15 to 0.7]). For letter writing, PP made no significant impact compared to FI (odds ratio = 1.14 [95% CI = 0.89 to 1.46]).
Conclusions
Emergency physicians sharing personal narratives on Twitter are perceived to be more effective at communicating COVID‐19 health recommendations compared to federal officials sharing impersonal guidance.
The coronavirus disease 2019 (COVID‐19) crisis has exposed the critical need for clearly and consistently communicating public health guidelines anchored in the best available evidence, Yet many voices are competing with public health officials, particularly given that social media outlets frequently supplant traditional news sources. 1 Amid this backdrop, the United States has had higher COVID‐19–associated deaths and excess all‐cause mortality compared to most peer countries. 2 Despite the alarming rate of viral transmission, the public has not had full compliance with pandemic guidelines. 3 , 4 Policymakers and public health officials therefore must be strategic in communicating pandemic‐related messages to the public.
Emergency physicians can play a key role in disseminating and amplifying public health recommendations especially during a crisis. 5 , 6 Emergency departments (EDs) experienced the severity of the initial COVID‐19 viral surge and were challenged by a rapid response to the influx of ED patients. 7 , 8 , 9 Serving at the front lines of the epidemic, emergency physicians have played a prominent role as a trusted source in communicating COVID‐19 updates and urging the public to stay home. 6 , 10 , 11 The effectiveness of public messaging can be influenced by the credibility of the messenger 12 , 13 and the content of the message. 14 However, there are little experimental data measuring the effectiveness of public health communication through personal narrative or by physicians, which has been commonly seen in social media posts during the COVID‐19 pandemic.
The goal of this study was to evaluate the effectiveness of a physician versus federal official and personal versus impersonal content in delivering COVID‐19 public health recommendations on Twitter, a popular social media platform. We tested the following hypotheses: 1) Emergency physicians deliver a more effective message than federal officials, 2) personal appeals are more effective than impersonal ones, and 3) the interaction of a physician messenger with a personal message is synergistic.
METHODS
Study Design and Setting
We conducted a preregistered randomized experiment using simulated Twitter accounts and posts that randomly manipulated messenger type and message content in a 2 × 2 between‐subject factorial design. We launched the experiment on April 30, 2020, the day the White House–issued public restriction guidelines were set to expire, transferring decision‐making responsibility on restrictions to state governments.
This trial was approved by the institutional review board at the University of Michigan. Written informed consent was obtained from participants before participation. This trial followed the Consolidated Standards of Reporting Trials (CONSORT) 15 guideline with suggested amendments for reporting nonpharmacologic treatments and factorial trials. 16
Participants
We recruited U.S.‐based adult participants from Lucid Theorem, a nationally representative crowdsourced online subject pool that is quota‐sampled to match census demographics on age, gender, race/ethnicity, and region. 17 Participants were eligible if ≥ 18 years old. We included responses for analysis if ≥ 80% of study questions were complete. We assessed the impact of weighting the sample based on demographic characteristics of U.S. adults with Internet access as reported by the 2017 U.S. Census 18 (Data Supplement S1, Tables S1 and S2, available as supporting information in the online version of this paper, which is available at http://onlinelibrary.wiley.com/doi/10.1111/acem.14188/full). Participants in Lucid were compensated at a rate comparable to $1 per study. Median time to complete the study was 11 minutes.
Study Procedures
Participants accessed the online survey (Qualtrics, Provo UT) through their personal electronic devices and gave consent blinded to the study objectives. They first underwent a pretreatment attention assessment with the correct answer embedded in the instruction stem. 19 We randomized participants to one of four treatment arms with simulated Twitter posts and they answered a series of questions to measure primary outcomes. This was followed by a second attention check to recall the messenger’s occupation, which was a means of assessing that participants read the post and had received the intervention. Finally, participants were invited to take a stay‐at‐home pledge, to write a letter to their governor, and to answer additional covariate questions.
Twitter Stimuli and Randomization
We created images of a Twitter account and message for experimental exposures. We used the same male actor for the emergency physician (dressed in scrubs and a surgical cap) and the nonphysician federal official (business clothes). The background photo was a building selected to plausibly appear as either a federal building or a hospital. We took other Twitter metrics (date joined, number of accounts followed, and followers) from an exemplar emergency physician Twitter account that were the same across conditions.
For message content, we compared the effect of a personal versus impersonal message. The personal message was based on “the identifiable victim effect,” that having more identifiable information about a victim increases caring. 20 In contrast, the language for the impersonal message was used directly from a mass federal communication mailed on postcards to 130 million U.S. households 21 as part of the “President’s Coronavirus Guidelines for America” and from the White House “Opening Up America Again” guidelines. 22 , 23
The two messages had approximately the same number of words (personal = 61, impersonal = 55) and delivered a similar three‐part message: 1) young people are at risk, 2) public activity restrictions should continue, and 3) continuing restrictions would reduce the risk of viral resurgence (Figure 1).
Figure 1.

Simulated Twitter messages for COVID‐19 public health messaging. Simulated Twitter posts showing a sample of the physician/personal arm on the left, and the federal official/impersonal treatment arm on the right. The text was copied in larger font on the online survey. Two additional posts were created with the texts reversed.
Simple random assignment was accomplished via the randomizer tool in Qualtrics. Each participant was assigned to one of four possible treatment arms with equal probability: 498 to physician/personal (PP), 505 to physician/impersonal (PI), 505 to federal/personal (FP), and 499 to federal/impersonal (FI).
Primary Outcome Measures
To evaluate the effect of messages, we measured 1) perceived message effectiveness (PME); 2) perceived attitude effectiveness (PAE); and 3) behavioral outcomes: likelihood of sharing or writing a letter to a governor. The PME scale was intended to measure the message’s emotional impact and was adapted from a scale used in the context of smoking cessation research. 24 Participants evaluated the messages as memorable, grabbed my attention, powerful, meaningful, and convincing on a 7‐point Likert scale “strongly disagree” to “strongly agree” (coded 1–7), summed to a 35‐point rating (Data Supplement S1, section 5). We modified the original scale by removing subscale “informative,” due to COVID‐19 information saturation. The modified scale demonstrates high reliability (α = 0.93) and an eigenvalue of 3.96 accounting for 79.2% of the variance, similar to the original scale reliability (α = 0.94) and eigenvalue of 4.22 accounting for 70% of the variance.
The PAE scale was intended to measure the message’s effect on attitudes and was adapted from a scale used in smoking cessation research. 25 Participants evaluated whether the message 1) “Made me concerned about the health effects of lifting restrictions on public activity”; 2) “Made lifting restrictions less appealing”; or 3) “Discourages me from supporting opening America up right now” on a 5‐point Likert scale, “not effective at all” to “extremely effective” (coded 1–5), summed to a 15‐point rating. The modified scale demonstrates high reliability (α = 0.88) and one‐factor dimension that accounted for 81.3% of the variance, similar to the original scale reliability (α = 0.93) and a general factor that accounted for 82.6% of the variance.
We measured likelihood to share the Tweet as an estimator of the messages’ behavioral impact. This was measured on a 7‐point Likert scale “extremely unlikely” to “extremely likely” (coded 1–7). Self‐reported willingness to share social media posts has previously been correlated with increased sharing in reality. 26
Finally, we asked participants whether they were interested in writing a letter to their state governor (yes/no). Participants who agreed were provided a free‐text response box to write to the governor (not a form letter) and were truthfully informed that we would send this letter anonymously, which we did via state government online communication forms. Because of the cognitive effort involved, the letter‐writing task is less susceptible to desirability bias. 27
Secondary Outcome Measures
As an exploratory outcome, we asked participants to take a pledge (yes/no) to stay inside to fight COVID‐19. Pledging has been a popular way in the COVID‐19 pandemic for concerned groups to encourage social distancing. 28 Prior research indicates that pledging to engage in prosocial behavior (e.g., voting, environmental protection) has a small but significant effect on increasing the desired outcome. 29
Covariate Measures
We incorporated additional variables in a covariate‐adjusted model and to explore heterogeneous treatment effects using demographic information provided by Lucid (age, education, race/ethnicity, sex, household income, political party, state), which we supplemented with survey questions on overall health, marital status, population density, number in household, employment status, and political ideology. We also collected variables related to health behaviors, policy positions, and messaging receptiveness: anxiety about coronavirus, trust in federal officials and physicians, 30 economy versus public health trade‐off, 31 political engagement, 32 consumption of media bias via AllSides rankings, 33 empathy (using the empathic concern subscale of the Brief Interpersonal Reactivity Index 34 ), and news exposure frequency. Finally, we incorporated data on the extent of COVID‐19 cases and restrictions based on the participant’s state of residence (Data Supplement S1, section 3).
Data Analysis
Sample size was determined from a pilot survey with 601 Lucid participants conducted 2 weeks prior and not included in the final study. We estimated with 438 participants per treatment arm (n = 1,752), the minimum detectable effect at 80% power using a two‐sided hypothesis test (α = 0.05) is approximately 0.10 standardized units for a bivariate outcome difference of letter writing.
The statistical analysis plan was preregistered prior to data collection through the Open Science Framework (Data Supplement S1, section 9). We compared demographic characteristics and outcomes across groups by analysis of variance and t‐test for continuous variables and chi‐square test and Z‐test of proportions for categorical variables. As recommended for the accurate reporting of factorial studies, 16 we present three major comparisons: 1) four‐level treatment effects, 2) each factor pooled (messenger and message content), and 3) interaction between factors. Assumptions for each statistical test were evaluated using standard diagnostic tests and no major violations were found.
We estimated treatment effects using ordinary least‐squares linear regression and logistic regression on the four‐level treatment factor, with federal impersonal as the omitted reference category. Regression models were covariate‐adjusted to maximize the precision of estimated treatment effects. Covariates were selected by items expected to be associated with social distancing and then manually backward selected for inclusion based on the strength of the association with the outcome and Akaike information criterion of the model fit: race/ethnicity, marital status, political party, gender, COVID‐19 anxiety, news frequency, and economy versus public health trade‐off. All models were assessed for violations of basic assumptions and no major violations were found. Participants with missing value for a variable were included with a missing data indicator for that variable.
We also examined whether subgroups of participants were affected differently by treatments using generalized random forest, a machine learning algorithm that estimates treatment effect heterogeneity as a function of each participant’s covariate profile by nonparametric statistical estimation based on random forests. 35 Understanding how demographics may contribute to different responses to messaging can help in creating tailored content for specific groups at higher risk for COVID‐19. 4 Identifying these groups would create opportunities for audience segmentation—varying messaging strategies to address different groups—as demonstrated in climate science communication literature. 36 We assessed the effect heterogeneity specifically for PME because as an emotion‐based rapid cognition, we hypothesized that it would be more likely to be influenced by demographic profiles. 37 R version 3.5.2 (R Foundation for Statistical Computing) was used for statistical analyses, and the grf package was used for Causal Forests. 38
RESULTS
Of 2,090 participants who entered the survey, 2,007 consented, were randomized, and completed the survey with ≥ 80% data (Data Supplement S1, Figure S1). All participants that were randomized were included in the analysis. Participants’ mean (±SD) age was 45 (±16.7 years), 51% (n = 1,034) were female, 10.6% (n = 214) were Black, and 11.6% (n = 234) were Hispanic. Baseline characteristics and covariates were well balanced across the four treatment arms (Table 1; Data Supplement S1, Table S3).
Table 1.
Participant Demographics and Baseline Characteristics
| No.(%) of Participants by Treatment Arm | |||||
|---|---|---|---|---|---|
| Federal Impersonal | Federal Personal | Physician Impersonal | Physician Personal | Overall | |
| (n = 499) | (n = 505) | (n = 505) | (n = 498) | (n = 2,007) | |
| Demographics | |||||
| Female | 246 (49.3) | 247 (48.9) | 271 (53.7) | 267 (53.6) | 1,034 (51.4) |
| Age group (years) | |||||
| 18–24 | 59 (12.4) | 70 (14.3) | 67 (13.8) | 61 (12.7) | 257 (13.3) |
| 25–44 | 187 (39.3) | 163 (33.4) | 189 (38.9) | 178 (36.9) | 720 (37.2) |
| 45–64 | 148 (31.1) | 178 (36.5) | 152 (31.3) | 157 (32.6) | 635 (32.8) |
| 65+ | 82 (17.2) | 77 (15.8) | 78 (16.0) | 86 (17.8) | 323 (16.7) |
| Region (%) | |||||
| Midwest | 90 (18.0) | 107 (21.2) | 94 (18.6) | 96 (19.3) | 388 (19.3) |
| Northeast | 100 (20.0) | 115 (22.8) | 96 (19.0) | 103 (20.7) | 414 (20.6) |
| South | 189 (37.9) | 184 (36.4) | 209 (41.4) | 189 (38.0) | 772 (38.4) |
| West | 120 (24.0) | 99 (19.6) | 106 (21.0) | 110 (22.1) | 436 (21.7) |
| Race/ethnicity | |||||
| American Indian or Alaskan Native | 5 (1.0) | 4 (0.8) | 4 (0.8) | 3 (0.6) | 16 (0.8) |
| Asian | 25 (5.0) | 27 (5.3) | 30 (5.9) | 27 (5.4) | 110 (5.5) |
| Black | 53 (10.6) | 51 (10.1) | 59 (11.7) | 51 (10.2) | 214 (10.6) |
| Hispanic | 57 (11.4) | 60 (11.9) | 62 (12.3) | 55 (11.0) | 234 (11.6) |
| Other | 15 (3.0) | 16 (3.2) | 18 (3.6) | 12 (2.4) | 61 (3.0) |
| White | 344 (68.9) | 347 (68.7) | 332 (65.7) | 350 (70.3) | 1,375 (68.4) |
| Education | |||||
| College graduate | 291 (58.6) | 261 (51.9) | 270 (53.6) | 299 (60.0) | 1,122 (56.0) |
| High school graduate | 107 (21.5) | 123 (24.5) | 115 (22.8) | 84 (16.9) | 430 (21.4) |
| No diploma | 12 (2.4) | 12 (2.4) | 13 (2.6) | 10 (2.0) | 47 (2.3) |
| Some college | 87 (17.5) | 107 (21.3) | 106 (21.0) | 105 (21.1) | 406 (20.2) |
| Income | |||||
| Missing | 14 (2.8) | 15 (3.0) | 21 (4.2) | 13 (2.6) | 63 (3.1) |
| <$25,000 | 134 (26.9) | 117 (23.2) | 140 (27.7) | 106 (21.3) | 498 (24.8) |
| >$99,000 | 108 (21.6) | 97 (19.2) | 82 (16.2) | 114 (22.9) | 401 (20.0) |
| $25,000–$49,000 | 110 (22.0) | 118 (23.4) | 130 (25.7) | 102 (20.5) | 461 (22.9) |
| $50,000–$74,000 | 69 (13.8) | 95 (18.8) | 83 (16.4) | 95 (19.1) | 343 (17.1) |
| $75,000‐$993,000 | 64 (12.8) | 63 (12.5) | 49 (9.7) | 68 (13.7) | 244 (12.1) |
| Marital status | |||||
| Married | 227 (45.5) | 233 (46.1) | 233 (46.1) | 245 (49.2) | 938 (46.7) |
| Other | 130 (26.1) | 127 (25.1) | 134 (26.5) | 121 (24.3) | 512 (25.5) |
| Single | 142 (28.5) | 145 (28.7) | 138 (27.3) | 132 (26.5) | 557 (27.8) |
| Health status | |||||
| Missing | 6 (1.2) | 6 (1.2) | 7 (1.4) | 6 (1.2) | 28 (1.4) |
| Excellent | 67 (13.4) | 64 (12.7) | 62 (12.3) | 75 (15.1) | 268 (13.3) |
| Fair | 78 (15.6) | 66 (13.1) | 76 (15.0) | 69 (13.9) | 289 (14.4) |
| Good | 189 (37.9) | 202 (40.0) | 182 (36.0) | 191 (38.4) | 764 (38.0) |
| Poor | 16 (3.2) | 9 (1.8) | 15 (3.0) | 13 (2.6) | 53 (2.6) |
| Very good | 143 (28.7) | 158 (31.3) | 163 (32.3) | 144 (28.9) | 608 (30.2) |
| Baseline Characteristics | |||||
| News frequency | |||||
| Frequently | 140 (28.1) | 156 (30.9) | 154 (30.5) | 145 (29.1) | 595 (29.6) |
| Other | 97 (19.4) | 93 (18.4) | 92 (18.2) | 80 (16.1) | 362 (18.0) |
| Very frequently | 262 (52.5) | 256 (50.7) | 259 (51.3) | 273 (54.8) | 1,050 (52.3) |
| Prioritize public health over economy | 394 (79.1) | 396 (78.9) | 414 (82.8) | 407 (82.1) | 1,611 (80.7) |
| Political party | |||||
| Democrat | 237 (47.5) | 229 (45.3) | 229 (45.3) | 209 (42.0) | 905 (45.0) |
| Independent | 60 (12.0) | 62 (12.3) | 76 (15.0) | 69 (13.9) | 268 (13.3) |
| Republican | 202 (40.5) | 214 (42.4) | 200 (39.6) | 220 (44.2) | 837 (41.6) |
| Political ideology | |||||
| Missing | 6 (1.2) | 9 (1.8) | 9 (1.8) | 6 (1.2) | 33 (1.6) |
| Conservative | 101 (20.2) | 99 (19.6) | 110 (21.8) | 101 (20.3) | 411 (20.4) |
| Liberal | 93 (18.6) | 91 (18.0) | 81 (16.0) | 79 (15.9) | 344 (17.1) |
| Moderate | 191 (38.3) | 193 (38.2) | 196 (38.8) | 197 (39.6) | 777 (38.7) |
| Very conservative | 75 (15.0) | 72 (14.3) | 79 (15.6) | 73 (14.7) | 299 (14.9) |
| Very liberal | 33 (6.6) | 41 (8.1) | 30 (5.9) | 42 (8.4) | 146 (7.3) |
| Anxiety level | |||||
| Missing | 6 (1.2) | 6 (1.2) | 6 (1.2) | 1 (0.2) | 22 (1.1) |
| Not at all | 110 (22.0) | 94 (18.6) | 116 (23.0) | 109 (21.9) | 429 (21.3) |
| More than half the days | 91 (18.2) | 103 (20.4) | 97 (19.2) | 98 (19.7) | 389 (19.4) |
| Several days | 162 (32.5) | 185 (36.6) | 166 (32.9) | 172 (34.5) | 685 (34.1) |
| Nearly every day | 130 (26.1) | 117 (23.2) | 120 (23.8) | 118 (23.7) | 485 (24.1) |
Main Outcomes
For the four‐level treatment results, participants rated PME, PAE, and likelihood of sharing significantly higher in the PP condition compared with the FI condition, with largest effect on PME (Figure 2). Unadjusted estimated effects of PP versus FI are presented here with outcome means (Data Supplement S1, Table S4); the remaining comparisons are shown in Data Supplement S1, Table S5. For the PME 35‐point scale outcome, the means (±SDs) were PP 28.52 (±6.81) versus FI 25.32 (±6.95; difference = 3.2 [95% CI = 2.37 to 4.02], p < 0.001). For the PAE 15‐point scale, the means (±SDs) were PP 11.02 (±3.66) versus FI 9.77 (±3.54; difference = 1.26 [95% CI = 0.81 to 1.7], p < 0.001). For the likelihood to share 7‐point scale, the means (±SDs) were PP 4.99 (±2.09) versus FI 4.59 (±2.13; difference = 0.4 [95% CI = 0.15 to 0.66], p = 0.003). There was no significant difference across treatment arms of letter writing to the governor to continue public activity restrictions (odds ratio for PP compared to FI was 1.14 [95% CI = 0.89 to 1.46]). The proportion letter writing was 50.6% for PP versus 47.3% for FI (difference = 3.3% [95% CI = −3.1% to 9.7%], p = 0.33). There was similarly no significant effect on the pledge to stay home secondary outcome: mean PP 90.6% versus FI 90.0% (p = 0.99). As expected, adjusted means had similar effect estimates with more precise confidence intervals (Data Supplement S1, Table S6).
Figure 2.
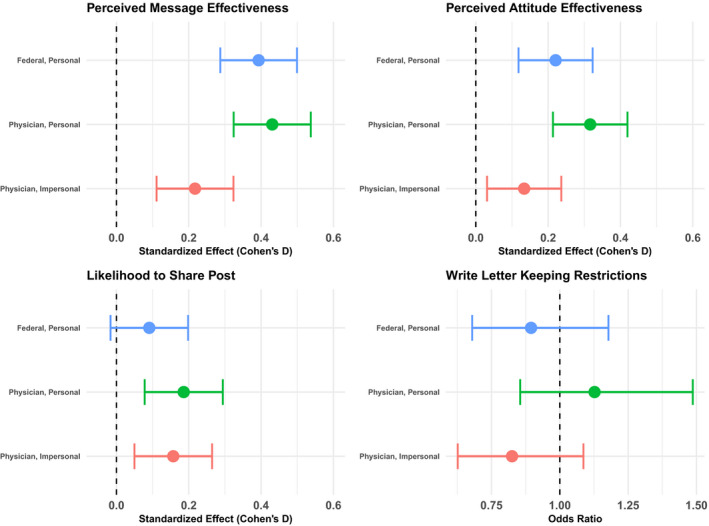
Estimated treatment effects on primary outcomes by treatment arm compared to the federal, impersonal condition. Covariate‐adjusted treatment effects from ordinary least squares regression with reference being the control group, federal impersonal message. Estimates are standardized using Cohen’s D, which scales outcomes by the pooled standard deviation. A Cohen’s D of 0.2 is considered a small effect and 0.5 a medium effect. 39 (Table S6 for tabular form). Points are bounded by 95% CIs. Regression adjusted by covariates: race/ ethnicity, marital (married, single, other), party, gender, anxiety about COVID‐19, news frequency (very frequent, frequent, other), and economy versus public health trade‐off.
The average effects of the messenger and message are presented in Data Supplement S1, Table S7. The pooled treatment effect of both personal content and physician messenger had a statistically significant impact on both PME and PAE. Cohen’s D, a standardized measure of effect size, is presented here to facilitate comparing across different scales—0.2 is considered a small effect and 0.5 a medium effect. 39 The average personal content had a stronger effect compared to physician messenger for PME (0.40 [95% CI = 0.28 to 0.52], p < 0.001; versus 0.25 [95% CI = 0.13 to 0.37], p < 0.001) and PAE (0.22 [95% CI = 0.10 to 0.35], p < 0.001; versus 0.16 [95% CI = 0.04 to 0.29], p = 0.009), respectively. Conversely, personal content did not significantly increase likelihood of sharing, while the physician messenger retained a positive effect (0.17 [95% CI = 0.05 to 0.30], p = 0.006). We found a negative interaction for PME such that physicians had an incrementally increased score compared to federal officials when presenting for the impersonal context, but less so for the personal narrative (–1.18 [95% CI = –2.35 to –0.02], p = 0.045). No significant interactions were found for the other primary outcomes.
Sensitivity Analysis Attention Check Question
We presented participants with two attention checks. Most participants passed the postoutcome measured manipulation check, correctly selecting the occupation in the Twitter profile (81.1%, n = 1,628). Far fewer passed the preexposure check in which the correct answer was hidden within the instruction paragraph (52.1%, n = 1,046). The groups were similar in treatment effects but had slightly stronger effects in the groups with higher levels of attention checks. (Data Supplement S1, Table S8, Figure S2).
Treatment Effect Heterogeneity
We did not find significant heterogeneity in causal forest‐estimated treatment effects of the personal message on PME. Causal forest was trained on many key variables, and test set predictions and CIs were assessed (Figure 3). While some patterns visually emerged among the variables specifically selected for graphical illustration based on hypothesized effect heterogeneity—political ideology, health status, age, and race/ethnicity—all individual CIs overlapped, coinciding with a failure to reject the null hypothesis of no treatment effect heterogeneity with a global test. 40
Figure 3.
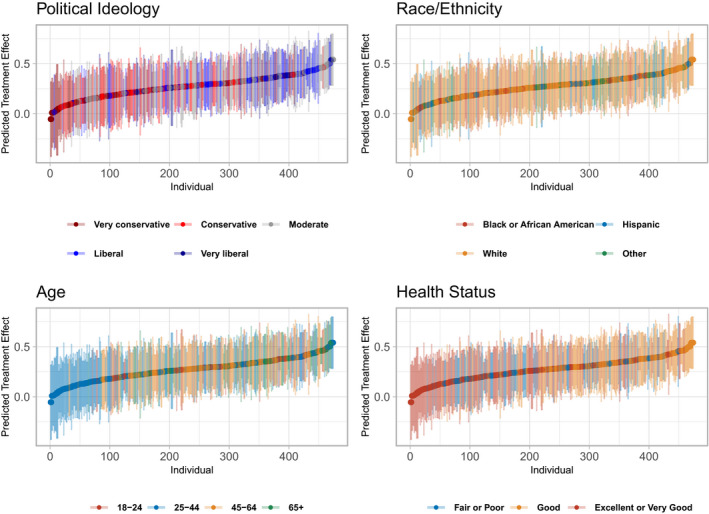
Causal forest assessment of treatment effect heterogeneity on perceived message effectiveness by participant characteristics. Treatment effect heterogeneity shown for perceived messaging effect outcome, ordered by predicted treatment effect size in Cohen’s D standardized units. A Cohen’s D of 0.2 is considered a small effect and 0.5 a medium effect. 39 Omnibus test for heterogeneity 40 found no significant heterogeneity in the effect (p‐value 0.26). Political ideology and age selected due to highest relative variable importance, though not statistically significant. Race/ethnicity and health status selected due to hypothesized importance, though visually and statistically no heterogeneity demonstrated.
DISCUSSION
To our knowledge, this is the first large‐scale, nationally representative, preregistered, randomized experiment to directly estimate the effect of a physician versus federal official messenger and message content of simulated social media posts on individual perceptions, attitudes, and behavior. We found that public health messages delivered by physicians and personal messages elicited stronger emotions, greater changes in attitudes, and an increased willingness to disseminate the message than when federal officials delivered impersonal messages. We did not observe differences in a stay‐at‐home pledge (which was near ceiling) nor in willingness to write a letter to the governor to continue restrictions. These findings suggest that emergency physicians sharing personal stories on social media may be more effective in increasing general adherence to public health guidelines than federal officials sharing impersonal messages. Complementary communication campaigns are still needed to augment these recommendations to change pandemic‐related individual behavior.
Our study adds important findings of source effects and messaging content on a nontraditional communication platform during this public health crisis. We demonstrate that trusted messengers can alter opinions on contentious public policy issues consistent with prior experiments finding that a medical scientist and physician increased support for antimicrobial resistance policy 12 and comparative effectiveness research, 13 respectively. The framing of health messages also matters. Similar to identifiable victim effect findings, we found enhanced emotional and attitudinal impact when the message was to help a single, identifiable person (i.e., the COVID‐19 victim who was a friend) compared to the concept of helping the many, unidentifiable others. 20 , 41 Moreover, findings of increased public health messaging effectiveness from personal narratives is also supported by organ donation literature, which has shown that when viewers are more emotionally involved in a television narrative they were more likely to become organ donors if the show encouraged donation. 42
We also assessed heterogeneous treatment effects to determine if there were distinct subpopulations which were impacted by the intervention differently, a finding that would be helpful for tailoring messaging for different groups. Despite a rigorous investigation harnessing machine learning tools, we found no significant impact of any participant characteristic, on the extent or direction of the message’s impact, specifically examining political ideology, health status, age, and race/ethnicity. Although we did not observe a differential impact of the emergency physician or federal official on lower income or minority participants, underserved populations may have lower trust in physicians than those included in our study 43 and may interact with messages differently from our participants. Future research should examine how to most effectively communicate with underserved minority populations hardest hit by the pandemic.
Our results add to a growing body of research investigating the impact of social media platforms for public health communication. The majority of Twitter users cite it as a news source, 1 presenting an opportunity for health professionals to capitalize on this channel as an adjunct for reaching a broader segment of the public. Physicians, scientists, and health providers have played an increasing role on Twitter, using it to share personal communications 44 and engage with the public on health issues. 45 Relevant to a pandemic, Twitter has been identified as a tool for efficient information dissemination during emergency events 5 and in public health crises to communicate recommendations. 46 Our findings support the increased use of Twitter by health care professionals as a platform to communicate directly to the public.
While government‐mandated public activity restrictions and social distancing recommendations play a key role in preventing the spread of COVID‐19, these interventions will be ineffective if the public is not willing to adhere to them. Social media–based public messaging may help to improve the public’s perception of these measures and thus adherence to health guidelines. However, during the pandemic, several U.S. health care institutions urged physicians not to make public appeals. 47 , 48 , 49 , 50 Our findings bolster policies that protect social media use by scientists and health providers to share public health communications directly to the public.
LIMITATIONS
This study has several limitations. First, the experimental design used a simulated Twitter message in the context of an online survey. Federal officials may be restricted on what they can communicate on social media using their official titles, but pilot data for this experiment showed most participants found the Twitter stimuli believable. It is possible that participants would react differently if they encountered these messages on the actual social media platform. However, participant likelihood to share a post has been shown to correlate highly with action in real life. 26 Furthermore, while the effects of user comments on social media were beyond the scope of this study, prior research has shown that user comments may have an additive effect on messaging impact. 51 , 52 Whether it will change reader behavior is unknown. Although we observed an increased willingness to share certain messages, we did not find differences in pledging to stay home nor writing a letter to the governor to maintain restrictions. It remains unclear if the impact of the messages would translate into real‐life changes in compliance with social distancing measures. Second, though the participant pool matches U.S. demographics in most regards, our participants had higher educational attainment and lower proportion of Hispanic origin (approximately 15.4% of U.S. population with access to Internet versus 11% in our study). 18 We weighted our sample to account for educational differences and still did not observe an appreciable impact on treatment effects (Data Supplement S1, Table S3). Further supporting generalizability, Lucid participants have exhibited behavioral experimental results similar to U.S. national probability samples. 17 Third, the high levels of reported anxiety created a likely ceiling effect for our outcomes. For PME, almost half of participants rated the message at 6 or above on a 7‐point scale. Ceiling effects may have reduced sensitivity to determining differences by treatment, biasing results toward null. Finally, we selected white males for the physician and federal official in the study, the most common demographic for both groups. It is possible that other races and genders of the Twitter messenger could have influenced subpopulations of this study differently than White males; however, prior patient satisfaction simulation studies did not find differences by physician race or gender. 53
CONCLUSION
Using a rigorous randomized experiment of a simulated Twitter message, we found that an emergency physician’s Twitter message of a personal story and recommendation related to COVID‐19 increased the attitudinal, emotional, and willingness to share measures of impact compared to a federal official sharing impersonal guidance. These results underscore the advocacy role for physicians on social media in promoting public health recommendations. We did not find an impact on letter writing to their governor to support COVID‐19 restrictions nor pledging to stay home. Future directions should explore the real‐world impact of emergency physician public health Tweets on measures of behavior change.
Supporting information
Data Supplement S1. Supplemental material.
Academic Emergency Medicine 2021;28:172–183.
Received September 24, 2020; revision received November 26, 2020; accepted November 30, 2020.
The University of Michigan National Clinical Scholars Program supported this work. Dr. Solnick was supported by the Institute for Healthcare Policy and Innovation at U‐M National Clinician Scholars Program. Dr. Chao was supported by the VA Office of Academic Affiliations through the VA/National Clinician Scholars Program and the University of Michigan Medicine at UM. The contents do not represent the views of the U.S. Department of Veterans Affairs or the United States Government.
The University of Michigan National Clinical Scholars Program provided funding for the study but had no role in the conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; the decision to submit the manuscript for publication; or the decision as to which journal the manuscript was submitted. No other funding sources had a role in the study.
Author contributions: RES had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design—RES, GC, GTKT, RR, KEK; acquisition, analysis, or interpretation of data—RES, GC, GTKT, RR, KEK; drafting of the manuscript—RES, GC, GTKT, RR, KEK; critical revision of the manuscript for important intellectual content—RES, GC, GTKT, RR, KEK; statistical analysis—RES, GTKT, RR; obtained funding—RES; administrative, technical, or material support—RES, KEK; and supervision—KEK.
Trial registration: https://osf.io/kabvr.
References
- 1. The Evolving Role of News on Twitter and Facebook . Pew Research Center’s Journalism Project. 2015. Available at: https://www.journalism.org/2015/07/14/the‐evolving‐role‐of‐news‐on‐twitter‐and‐facebook/. Accessed May 4, 2020.
- 2. Bilinski A, Emanuel EJ. COVID‐19 and excess all‐cause mortality in the US and 18 comparison countries. JAMA 2020;324:2100–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Park CL, Russell BS, Fendrich M, Finkelstein‐Fox L, Hutchison M, Becker J. Americans’ COVID‐19 stress, coping, and adherence to CDC guidelines. J Gen Intern Med 2020;35:2296–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Block R Jr, Berg A, Lennon RP, Miller EL, Nunez‐Smith M. African American adherence to COVID‐19 public health recommendations. Health Lit Res Pract 2020;4:e166–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hughes AL, Palen L. Twitter adoption and use in mass convergence and emergency events. IJEM 2009;6:248–60. [Google Scholar]
- 6. Gaeta C, Brennessel R, COVID‐19: emergency medicine physician empowered to shape perspectives on this public health crisis. Cureus 2020;12:e7504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rothfeld M, Sengupta S, Goldstein J, Rosenthal BM. 13 deaths in a day: an “apocalyptic” coronavirus surge at an N.Y.C. hospital. The New York Times. 2020. Available at: https://www.nytimes.com/2020/03/25/nyregion/nyc‐coronavirus‐hospitals.html Accessed Sep 24, 2020.
- 8. Feldman N, Lane R, Iavicoli L, et al. A snapshot of emergency department volumes in the “epicenter of the epicenter” of the COVID‐19 pandemic. Am J Emerg Med 2020. 10.1016/j.ajem.2020.08.057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Whiteside T, Kane E, Aljohani B, Alsamman M, Pourmand A. Redesigning emergency department operations amidst a viral pandemic. Am J Emerg Med 2020;38:1448–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chokshi DA, Katz MH. Emerging lessons from COVID‐19 response in New York City. JAMA 2020;323:1996–7. [DOI] [PubMed] [Google Scholar]
- 11. Elemental Editors .50 Experts to Trust in a Pandemic. Medium Elemental. 2020. Available at: https://elemental.medium.com/50‐experts‐to‐trust‐in‐a‐pandemic‐fe58932950e7. Accessed Sep 24, 2020.
- 12. Martin A, Gravelle TB, Baekkeskov E, Lewis J, Kashima Y. Enlisting the support of trusted sources to tackle policy problems: the case of antimicrobial resistance. PLoS One 2019;14:e0212993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gerber AS, Patashnik EM, Doherty D, Dowling CM. Doctor knows best: physician endorsements, public opinion, and the politics of comparative effectiveness research. J Health Polit Policy Law 2014;39:171–208. [DOI] [PubMed] [Google Scholar]
- 14. Davis KC, Duke J, Shafer P, Patel D, Rodes R, Beistle D. Perceived effectiveness of antismoking ads and association with quit attempts among smokers: evidence from the tips from former smokers campaign. Health Commun 2017;32:931–8. [DOI] [PubMed] [Google Scholar]
- 15. Boutron I, Moher D, Altman DG, Schulz KF, Ravaud P; CONSORT Group . Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Ann Intern Med 2008;148:295–309. [DOI] [PubMed] [Google Scholar]
- 16. McAlister FA, Straus SE, Sackett DL, Altman DG. Analysis and reporting of factorial trials: a systematic review. JAMA 2003;289:2545–53. [DOI] [PubMed] [Google Scholar]
- 17. Coppock A, McClellan OA. Validating the demographic, political, psychological, and experimental results obtained from a new source of online survey respondents. Res Politics 2019;6:2053168018822174. [Google Scholar]
- 18. Broadband Adoption and Computer Use by Year, State, Demographic Characteristics . Data.gov. Available at: https://catalog.data.gov/dataset/broadband‐adoption‐and‐computer‐use‐by‐year‐state‐demographic‐characteristics. Accessed Nov 19, 2020.
- 19. Berinsky AJ, Margolis MF, Sances MW, Warshaw C. Using screeners to measure respondent attention on self‐administered surveys: Which items and how many? Political Science Research and Methods. 2019. Available at: https://www.cambridge.org/core/services/aop‐cambridge‐core/content/view/979A15EB14DBBF596D56032D0CBB4424/S2049847019000530a.pdf/div‐class‐title‐using‐screeners‐to‐measure‐respondent‐attention‐on‐self‐administered‐surveys‐which‐items‐and‐how‐many‐div.pdf. Accessed Apr 29, 2020.
- 20. Small DA, Loewenstein G. Helping a victim or helping the victim: altruism and identifiability. J Risk Uncertain 2003;26:5–16. [Google Scholar]
- 21. Stankiewicz K. US households are being mailed ‘President Trump’s Coronavirus Guidelines for America’. CNBC 2020. Available at: https://www.cnbc.com/2020/03/27/us‐households‐are‐being‐mailed‐trumps‐coronavirus‐guidelines.html. Accessed May 1, 2020. [Google Scholar]
- 22. Opening Up America Again | The White House . The White House. 2020. Available at: https://www.whitehouse.gov/openingamerica/. Accessed May 1, 2020.
- 23. 30 Days to Slow the Spread . WhiteHouse.gov. 2020. Available at: https://www.whitehouse.gov/wp‐content/uploads/2020/03/03.16.20_coronavirus‐guidance_8.5x11_315PM.pdf. Accessed Apr 29, 2020.
- 24. Davis KC, Nonnemaker J, Duke J, Farrelly MC. Perceived effectiveness of cessation advertisements: the importance of audience reactions and practical implications for media campaign planning. Health Commun 2013;28:461–72. [DOI] [PubMed] [Google Scholar]
- 25. Baig SA, Noar SM, Gottfredson NC, Boynton MH, Ribisl KM, Brewer NT. UNC perceived message effectiveness: validation of a brief scale. Ann Behav Med 2019;53:732–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mosleh M, Pennycook G, Rand DG. Self‐reported willingness to share political news articles in online surveys correlates with actual sharing on Twitter. PLoS One 2020;15:e0228882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Crowne DP, Marlowe D. A new scale of social desirability independent of psychopathology. J Consult Psychol 1960;24:349–54. [DOI] [PubMed] [Google Scholar]
- 28. An Open Letter to All New Yorkers from the Emergency Department Frontline . Change.org. 2020. Available at: https://www.change.org/p/new‐yorkers‐plea‐from‐ed‐doctors‐to‐listen‐to‐covid‐19‐public‐health‐advise?recruiter=20768044&utm_source=share_petition&utm_medium=twitter&utm_campaign=psf_combo_share_abi&utm_term=psf_combo_share_initial&recruited_by_id=aeb355d0‐f085‐012f‐725f‐4040acce234c. Accessed May 18, 2020.
- 29. Costa M, Schaffner BF, Prevost A. Walking the walk? Experiments on the effect of pledging to vote on youth turnout. PLoS One 2018;13:e0197066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Reinhart RJ. Nurses Continue to Rate Highest in Honesty, Ethics. Gallup.com. 2020. Available at: https://news.gallup.com/poll/274673/nurses‐continue‐rate‐highest‐honesty‐ethics.aspx. Accessed May 1, 2020.
- 31. Ballew M, Bergquist P, Goldberg M, et al. American Public Responses to COVID‐19. Yale University and George Mason University. 2020. Available at: https://climatecommunication.yale.edu/publications/american‐public‐responses‐to‐covid‐19‐april‐2020/. Accessed Apr 29, 2020.
- 32. Measures and Scales . Pew Research Center ‐ U.S. Politics & Policy. 2018. Available at: https://www.people‐press.org/2018/04/26/appendix‐a‐measures‐and‐scales‐2/. Accessed Apr 29, 2020.
- 33. AllSides Media Bias Ratings . AllSides. 2020. Available at: https://www.allsides.com/media‐bias/media‐bias‐ratings. Accessed Apr 29, 2020.
- 34. Ingoglia S, Lo Coco A, Albiero P. Development of a Brief Form of the Interpersonal Reactivity Index (B‐IRI). J Pers Assess 2016;98:461–71. [DOI] [PubMed] [Google Scholar]
- 35. Athey S, Tibshirani J, Wager S. Generalized random forests. Ann Stat 2019;47:1148–78. [Google Scholar]
- 36. Maibach EW, Leiserowitz A, Roser‐Renouf C, Mertz CK. Identifying like‐minded audiences for global warming public engagement campaigns: an audience segmentation analysis and tool development. PLoS One 2011;6:e17571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Slovic P, Finucane ML, Peters E, MacGregor DG. The affect heuristic. Eur J Oper Res 2007;177:1333–52. [Google Scholar]
- 38. Tibshirani J, Athey S, Friedberg R. Package “Grf.” 2020. Available at: https://cran.r‐project.org/web/packages/grf/grf.pdf. Accessed Jun 12, 2020.
- 39. Cohen J. Statistical Power Analysis for the Behavioral Sciences. Routledge. 2013. Available at: https://play.google.com/store/books/details?id=cIJH0lR33bgC. Accessed Jun 12, 2020. [Google Scholar]
- 40. Chernozhukov V, Demirer M, Duflo E, Fernández‐Val I. Generic machine learning inference on heterogenous treatment effects in randomized experiments. 2018. Available at: https://open.bu.edu/handle/2144/31469. Accessed Jun 8, 2020.
- 41. Jenni K, Loewenstein G. Explaining the identifiable victim effect. J Risk Uncertain 1997;14:235–57. [Google Scholar]
- 42. Morgan SE, Movius L, Cody MJ. The power of narratives: the effect of entertainment television organ donation storylines on the attitudes, knowledge, and behaviors of donors and nondonors. J Commun 2009;59:135–51. [Google Scholar]
- 43. Duke C, Stanik C. Overcoming Lower‐Income Patients’ Concerns About Trust And Respect From Providers. Health Affairs Blog. 2016. Available at: https://www.healthaffairs.org/do/10.1377/hblog20160811.056138/full/. Accessed Nov 18, 2020.
- 44. Lee JL, DeCamp M, Dredze M, Chisolm MS, Berger ZD. What are health‐related users tweeting? A qualitative content analysis of health‐related users and their messages on Twitter. J Med Internet Res 2014;16:e237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Choo EK, Ranney ML, Chan TM, et al. Twitter as a tool for communication and knowledge exchange in academic medicine: a guide for skeptics and novices. Med Teach 2015;37:411–6. [DOI] [PubMed] [Google Scholar]
- 46. Jahng MR, Lee N. When scientists tweet for social changes: dialogic communication and collective mobilization strategies by Flint Water Study scientists on Twitter. Sci Commun 2018;40:89–108. [Google Scholar]
- 47. Gallegos A. Hospitals Muzzle Doctors and Nurses on PPE, COVID‐19 Cases. Medscape. 2020. Available at: https://www.medscape.com/viewarticle/927541. Accessed May 28, 2020.
- 48. Carville O, Court E, Brown KV. Hospitals Tell Doctors They’ll Be Fired If They Speak Out About Lack of Gear. Bloomberg News. 2020. Available at: https://www.bloomberg.com/news/articles/2020‐03‐31/hospitals‐tell‐doctors‐they‐ll‐be‐fired‐if‐they‐talk‐to‐press. Accessed Nov 18, 2020.
- 49. Friedersdorf C. Hospitals Must Let Doctors and Nurses Speak Out. The Atlantic. 2020. Available at: https://www.theatlantic.com/ideas/archive/2020/04/why‐are‐hospitals‐censoring‐doctors‐and‐nurses/609766/. Accessed Nov 18, 2020.
- 50. Stone W. ‘It’s Like Walking Into Chernobyl,’ One Doctor Says Of Her Emergency Room. NPR. 2020. Available at: https://www.npr.org/2020/04/09/830143490/it‐s‐like‐walking‐into‐chernobyl‐one‐doctor‐says‐of‐her‐emergency‐room. Accessed Nov 18, 2020.
- 51. Clementson DE. How web comments affect perceptions of political interviews and journalistic control: effects of web news attributions. Polit Psychol 2019;40:815–36. [Google Scholar]
- 52. Brewer PR, Habegger M, Harrington R, Hoffman LH, Jones PE, Lambe JL. Interactivity between candidates and citizens on a social networking site: effects on perceptions and vote intentions. J Exp Political Sci 2016;3:84–96. [Google Scholar]
- 53. Solnick RE, Peyton K, Kraft‐Todd G, Safdar B. Effect of physician gender and race on simulated patients’ ratings and confidence in their physicians: a randomized trial. JAMA Netw Open 2020;3:e1920511. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Supplement S1. Supplemental material.


