Abstract
Severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), also known as COVID‐19, is a new strain of coronavirus that has not been previously identified in humans. SARS‐CoV‐2 is recognized as a highly contagious respiratory virus with severe morbidity and mortality, especially in vulnerable populations. Being a novel disease, everyone is susceptible, there are no vaccine and no treatment. To contain the spread of the disease, health authorities throughout the world have restricted the social interactions of individuals in various degrees. Allergists, like other physicians, are faced with the challenge of providing care for their patients, while protecting themselves and patients from getting infected, with strategies that are in continuous evolution as states work through the different stages of social distance. Allergist provides care for patients with the most common non‐communicable disease in the world: asthma, allergic rhinitis, food allergy, venom allergy, drug allergy atopic dermatitis, and urticarial syndromes. Some of these diseases are not only considered risk factors for severe reactions but also have symptoms such as cough and sneezing that are in differential diagnosis with COVID‐19. As we move forward, allergy symptoms may prevent patients from working, go to school, or access medical services that increasingly are allowing only asymptomatic individuals. In this review, we will outline how to take care safety of different allergic patients during the pandemic.
Keywords: asthma, atopic dermatitis, atopy, COVID‐19, food allergy, immunotherapy, SARS‐CoV‐2
Key Message.
Severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), also known as COVID‐19, poses a new threat for the communities. Allergists serve patients, who are affected by chronic disease and need continuity of care during the pandemic. The level of community spread of the virus will likely fluctuate during the coming years until either a universal vaccine or herd immunity is achieved. Allergists need to be ready to operate safely with appropriate modifications of their practice tailored on community circulation.
1. INTRODUCTION
Severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), also known as COVID‐19, is a new strain of coronavirus that has not been previously identified in humans and is thought to have originated in chrysanthemum bats in Wuhan City, Hubei Province. 1 Since December 2019, when Chinese public health authorities noticed several cases of acute respiratory syndrome in Wuhan City, SARS‐CoV‐2 outbreaks and clusters of the disease have since been observed in Asia, Europe, Australia, Africa, and the Americas and WHO declared a pandemic on March 11, 2020.
SARS‐CoV‐2 is now recognized as a highly contagious respiratory virus. SARS‐CoV‐2 has multiple clinical presentations from asymptomatic to severe lung injury and multiorgan disease, especially in older individuals and those with chronic comorbidities. This polyhedric presentation makes it difficult to predict which health consequence the virus will have on the single individual and make it challenging to contain the spread. 2
Being a novel disease, everyone is susceptible, there are no vaccine and no treatment. To contain the spread of the disease, while developing drugs, vaccines, and hospital/healthcare preparedness, health authorities throughout the world have restricted social interactions of individuals in various degrees. Typically, the most restrictive measures are taken in the “red zone” or “phase 1” when full quarantine measures are recommended for all citizens. In such a phase, only life‐sustaining businesses are open, schools are closed, and there are government‐imposed social distancing rules. These extreme mitigation strategies are followed by a progressive reopening approach with different phases such as “orange zone,” “yellow zone,” “green zone,” or phase 2 and phase 3 that ease the restrictions as the virus becomes less prevalent in the community and healthcare systems are more prepared to treat the infected individuals (Figure 1). 3
Figure 1.
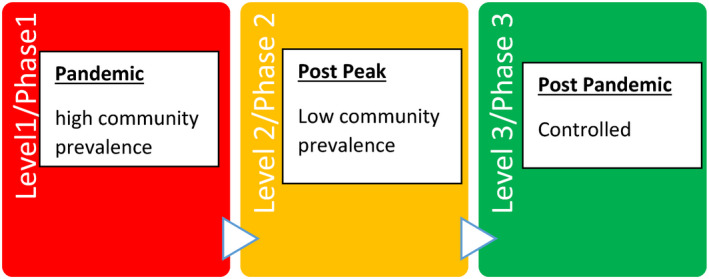
Viral community prevalence and safety recommendations
Allergists, like other physicians, face the challenge of providing care for their patients while protecting themselves and patients from getting infected. To achieve this goal, they use tactics that are in continuous evolution, adjusting work practices to state‐mandated restrictions, without clear guidelines but largely guided by fragmented recommendations given by local, national, and international organizations. 4
Allergists provide care for patients with the most common non‐communicable disease in the world: asthma, allergic rhinitis, food allergy, venom allergy, drug allergy atopic dermatitis, and urticarial syndromes. Some of these diseases are not only considered risk factors for severe reactions but also have symptoms, such as cough and sneezing, which are in differential diagnosis with COVID‐19. Taking care of the atopic patients is therefore essential not only to reduce severe outcomes of COVID‐19 infections, but also to prevent symptoms that may preclude allergy patients from working, go to school, or access medical services if they are suspected of carrying the novel virus. To take care of those patients, allergists use procedures that require close contact with patients and can aerosolize the virus, and many therapeutic approaches that modulate the immune system. Risk and benefit for the single patients and the staff need to be carefully evaluated before doing them. 4 , 5
2. HOW TO AVOID INFECTION IN THE OFFICE: PREVENTION AND CONTROL
We know that SARS‐CoV‐2 spreads mainly from person to person, for interaction below 6 feet (1.8 m) via large droplets, produced when an infected person coughs, sneezes, or talks. Those droplets can land in the mouth, nose, or eyes of people nearby and can be inhaled. Symptomatic and asymptomatic individuals can spread the disease very easily and sustainably between people. The virus can also spread in other ways, from touching surfaces or objects, feces, animals to people, and people to animals, but these are not thought to be the main ways the virus spreads. 3
Information from the ongoing COVID‐19 pandemic suggests that this virus is spreading more efficiently than influenza (R0= 1‐2), but not as efficiently as measles (R0= 12‐18), which is highly contagious. 1 We know that the way to reduce person‐to‐person spreads are to maintain good social distance (about 6 feet); cover your face with a mask; wash your hands often with soap and water or use a hand sanitizer with at least 60% alcohol; and routinely clean and disinfect frequently touched surfaces. 3 While organizing the office space, it is very important that when possible, staff will maintain 6‐feet distance from each other, and also healthcare providers will maintain when possible such distance from patients. This can be achieved by redistributing desks, staggering patient influx in waiting rooms, limiting the number of people coming with the patient (an adult should come alone when possible, children should be accompanied by 1 adult, and no siblings should not be allowed), and avoiding communal lunch or food sharing. Masking is increasingly recognized as an essential tool to slow the spread of the virus, and universal masking of patients and staff has also shown to reduce transmission in healthcare setting. 5 Furthermore, while the vaccine is not available, the CDC and ECDC have recommended the healthcare providers to use personal protective equipment (PPE) typical for standard, contact, and airborne precautions and use eye protection (Table 2). Therefore, to take care of COVID‐infected or potentially infected patients, gowns, gloves, and either an N95 respirator (in the USA) or FFP3/FFP2 (in Europe) plus face shield and goggles or a powered air‐purifying respirator (PAPR) should be used. However, there is a worldwide shortage of N95 and PARP; therefore, allergists may need to use a face mask instead of an N95 respirator if one is not available. In most hospital setting, N95 is used if aerosol procedures are done, whereas surgical masks are used for regular visits.
Table 2.
Summary of prevention control measure in the office
| Prevention measures | Implementation |
|---|---|
| 6 feet (1.8 m ) apart | Sign to remind to keep distance |
| Reduce number of staff and patients present at any given time | |
| Reduce or eliminate communal meals among staff, patients cannot eat in office | |
| PPE | Universal masking for staff and patients |
| Standard, contact, and droplet precaution | |
| Wash hand | Wash hands for 20 second |
| Use alcohol at least 60% if washing is not possible | |
| Clean frequently high surface areas | Clean using manufacturing recs, look time of contact for disinfectant to clean areas |
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
To reduce the risk of exposure, the allergist can decide to visit only asymptomatic patients, by strict screening phone call prior to the visit. Patients should be asked whether they have been exposed to COVID‐19 infected individuals, whether they have traveled to areas of high transmission, and whether they have any of the typical symptoms (Figure 2). Telehealth can be used instead of an in‐person visit. Furthermore, procedures such as spirometry and nebulizers should be avoided. 3
Figure 2.
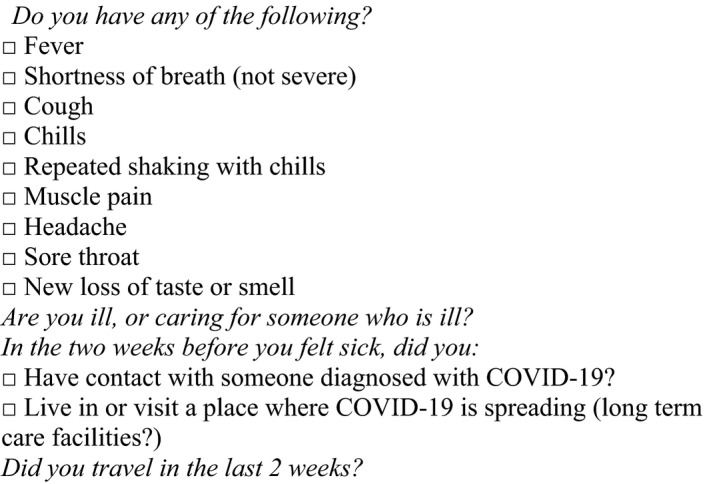
Questions to screen patients
To reduce the spread of the virus, policies in the office should be present in the office to self‐quarantine asymptomatic healthcare providers that have been directly exposed to sick patients or in the community (Figure 2 and Table 2).
For certain periods, allergist may be asked to reduce the visit to only essential ones, in order to reduce the physical contact among people and to preserve PPE and resources.
It is important to note that many allergy/immunology services are elective and can be managed without face‐to‐face interaction or deferred outright for short periods. Prioritizing certain services may be required when countries go in the red zone to prevent disease spread or based on the availability of adequate PPE for healthcare providers (Table 1 and Table 2). 4 , 5
Table 1.
Patient management during “red zone” shelter in place
| Steroid therapy per guidelines | Biologic | IVIG/SQ | IT initiation | IT escalation | IT maintenance | Challenge | Skin tests | Spirometry/nebulizer | |
|---|---|---|---|---|---|---|---|---|---|
| Asthma | Yes | Continue | NA | No | No | Continue | NA | No | No |
| Food allergy | NA | NA | NA | No | No | Continue | Selected | No | No |
| Eczema | Continue | Continue | NA | NA | NA | NA | NA | No | No |
| AR | Yes | NA | NA | No | No | Yes | NA | No | No |
| Venom allergy | NA | NA | NA | Yes | Yes | Continue | No | Yes | No |
| Drug allergy | NA | NA | Na | No | No | No | No | No | No |
| PID | NA | Continue | Yes | NA | NA | NA | NA | NA | No |
Abbreviations: AR, allergic rhinitis; IT, immunotherapy; IVIG, intravenous immunoglobulin or subcutaneous IG; NA, not available; PID, primary immunodeficiency;
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
We will here review how to treat specific conditions in the allergy office.
3. PROCEDURE IN THE ALLERGY OFFICE: HOW AND WHEN TO PERFORM THEM
3.1. Skin testing
Skin testing may require prolonged contact with the patients, and there is a risk of fluid body contamination, especially in children that may cry or cough while doing the procedure.
In the red zone, such a procedure can be delayed as often information is not essential for the immediate treatment of the patient.
Skin tests can be resumed in yellow/orange zone (phase 2/3) if appropriate PPE is available for healthcare providers such as a mask, eye protection, gowns, and gloves. 4 , 5
3.2. Food challenges
Food challenges represent the gold standard for the diagnosis of food allergy, as in vitro and in vivo testing has not enough specificity and sensitivity to predict tolerance of food in patients with IgE‐mediated and not‐IgE–mediated food allergies. For not‐IgE–mediated food allergies such as food protein‐induced enterocolitis (FPIES), no other tests exist besides food challenge.
Introduction of peanuts in patients sensitized to peanuts may prevent the development of food allergies (LEAP), food challenges or office maybe be required to introduce peanuts in patients at high risk of developing peanut allergies who have a positive IgE for peanuts.
Diagnostic food challenges may be food challenges that can largely be delayed except for peanut challenge in an infant for peanut introduction due to LEAP protocol or for introducing a food critical for appropriate nutrition to avoid intervention such as G tube or NG tube placement. 4 , 5
In the yellow/orange phase, food challenge may be resumed starting for those patients who are avoiding foods such as milk, egg, and wheat, or who have multiple food restrictions to avoid malnutrition and expand diet to essential foods. As during food challenges, prolonged contacted potential life resuscitation may be required PPE should be worn, and some hospital may require a negative swab from patients within 72 hours similar to those patients requiring procedures.
4. IMMUNOTHERAPY
Allergen injectable immunotherapy helps to reduce symptoms of allergic rhinitis. For those patients on maintenance, immunotherapy is considered essential, but the administration can be spaced to up to 6 weeks to reduce healthcare facility visits during the pandemic; dose adjustment may be needed until a regular schedule can be resumed. For patients on build‐up dosing for inhalant allergens, consider allowing for a longer period between injections (up to 14 days). Consideration of leveling off dosing in patients who are coming less often for immunotherapy may need to be individualized based on patient‐specific characteristics and tolerance of immunotherapy. The risk of reactions to ITS is highest during the escalation phase, and the risk and benefits of such risk need to be considered. Consequently, during the red zone, the initiation of immunotherapy should be avoided. As restriction ease and PPE, emergency services become more available more can be offered to patients in terms of immunotherapy as a strategy to maintain allergic rhinitis under control. 6
For venom allergy immunotherapy is considered a life‐saving treatment, there should be no change in service for initiation or build‐up venom immunotherapy (VIT) of patients with a history of a systemic reaction to the venom; this is an essential service provided by allergists. Patients on maintenance VIT can be spaced to every 2‐3 months if they have been on maintenance for at least a year. 6
Sublingual and oral immunotherapy environmental allergies should not be initiated in red zone restrictions but can be continued at home.
Food allergy immunotherapy visits for initiation and escalation could also be delayed, with patients maintaining current home dosing for those who have already been initiated. 4 , 5 The decision on when and how to restart the immunotherapy for food should be taken based on the availability of PPE, community transmission levels, and stage of immunotherapy. If patients due to pandemic have been maintained on a high dose and are 1‐2 doses from maintenance, those patients are likely low risk and can be restarted first, when conditions ease. Patients at low risk of reaction (higher doses of oral immunotherapy, never reacted before) should be restarted first followed by those patients at increased risk of reactions as conditions improve.
5. SPIROMETRY
Spirometry has the possibility of causing aerosolization, so special consideration needs to be made (McGowan, A et al Recommendation from ERS Group 9.1 (Respiratory function technologists/Scientists‐Lung function testing during COVID‐19 pandemic and beyond)).
The European Respiratory Society (ERS) does not recommend any patients with symptoms of COVID‐19 or flu‐like symptoms are tested with spirometry or lung function tests (LFTs) under any circumstances at this time. They recommend postponing all routine testing during the pandemic phase. COVID‐19 patients must not be tested for a minimum of 30 days post‐infection.
Full operation of lung function services may only resume when viral prevalence is low and reliable testing based on a combination of symptom screening, and testing is readily available.
In the interim period, ERS is recommended only for critical need and if these mitigation strategies can be implemented.
A test should always be carried out with a high specification disposable in‐line bacterial and viral filter in place with minimum proven efficiency for the high expiratory flow of 600 to 700 L/min.
The use of disposable combined mouthpieces/sensors is not recommended at this time: Maximize the use of single‐use consumables and dispose of the items with care, for example, nose clips and rubber mouthpieces.
For highest risk patients requiring essential testing, lung function should be carried out in a negative pressure room and using equipment only for high risk or infected patients.
This may only be available at specialist centers.
We recommend the use of either FFP3 masks or FFP2, where the former is not available. The duration of the use of protective masks should comply with local policy. Eye protection must always be worn, for example, goggles or face shields.
Disposable gloves should be used at all times when testing. These should be discarded afterward.
Exercise testing, nebulization, bronchial challenge tests, and other aerosol‐generating procedures should be postponed during the pandemic until the green phase is reached.
6. ASTHMA
Asthma is one of the most common lung diseases globally, and its incidence is still increasing in developing country. It is listed as a risk factor for severe disease by the CDC in the case of COVID‐19 infection. 3 This recommendation is largely based on the fact that SARS‐CoV‐2 is a coronavirus and can cause asthma exacerbation. However, other previous severe pandemic coronaviruses (SARS‐CoV and MERS‐CoV) have not been associated with asthma. Similarly, during this current pandemic, there are little data to demonstrate a specific increased risk of COVID‐19 from asthma. Data from China, Korea, and the United States note that asthma is not a strong risk factor for severe COVID‐19 disease, and actually, severe patients appear to be less likely to have asthma or COPD than the general population. 1 , 2 However, these data are based on hospitalized patients and may have significant limitations due to selection and reporting bias. It is also possible that asthma may use more caution and increased social distancing to avoid infections. Nonetheless, there is no evidence that anti‐inflammatory medication taken regularly to prevent inflammatory diseases is putting patients at increased risk of severe COVID‐19–related disease. 7 On the other hand, we know that patients with asthma during the pandemic continue to have a risk of exacerbation not only related to SARS‐CoV‐2 but also related to other infectious and allergy triggers with well‐known morbidity and mortality. Asthma exacerbation requiring medical emergency treatment may increase the risk of exposure to COVID‐19 due to visits to healthcare facilities. 4 , 5 Unless new evidence emerges that show otherwise, the current recommendations are to continue to follow guidelines to treat asthma, including the use of biologic agents—IL‐5, IL‐4/IL‐13, and IgE. 4 , 5 Biologics are considered among the essential services that allergists need to continue to provide during a red zone social distancing rule. However, given the unknown consequences of immunomodulation with biologics, during COVID‐19 infection, biologics should be paused until recovery in SARS‐CoV‐2–positive patients. 10
Special consideration to treat asthma is to reduce or avoid all together the use of nebulizer and spirometry for their risk to cause aerosolization of the virus in case of patients are carries as per before discussion. 4 , 5
7. ALLERGIC RHINITIS
Similar to patients with asthma, the medical treatment of patients with allergic rhinitis should be continued. 4 , 5 No evidence put this category of patients at risk of severe complication; during a COVID‐19 infection, not controlled allergic rhinitis in an individual with uncontrolled allergic rhinitis may increase the spread of diasease. 4 , 5 As restrictive measures get eased, allergic rhinitis patients if symptomatic may be prevented from accessing healthcare facilities, school, camp, and work as COVID‐19 symptoms may overlap with allergic rhinitis and pre‐screening of symptomatic patients will be widely implemented. 4 , 5 Under red zone circumstances, allergic rhinitis should be evaluated via telemedicine or telephone instead of in‐person. Evaluation of allergy can be postponed during red zone/phase 1 restrictions. Performing skin testing or in vitro serum‐specific IgE testing to inhalants may be appropriate as countries go to yellow, orange zones if the risk of acquiring COVID‐19 in healthcare facilities is low and adequate PPE protections are available to healthcare providers for the close contacts required to perform skin test. 4 , 5
Allergen immunotherapy can be considered the following recommendation outlined before l. 6
8. FOOD ALLERGY, EOSINOPHILIC ESOPHAGITIS (EoE), DRUG ALLERGY, AND ANAPHYLAXIS
Food allergy is a group of various diseases that pose different risk factors for patients. Acute IgE–mediated food allergy and food protein enterocolitis (FPIES) can be associated with the risk of acute life‐threatening or otherwise severe reaction, and eosinophilic esophagitis is linked with the risk of irreversible fibrosis. Many patients with food allergies are generally controlled if they avoid the known food that causes an issue. Delayed or deferred treatment in short term to intermediate term (a few weeks to even a few months) may not change the outcome of these diseases 4 , 5 .
Followup can be delayed or done via telehealth. Food challenges can largely be delayed except for peanut challenge in infants for peanut introduction due to LEAP protocol or for introducing a food critical for appropriate nutrition to avoid intervention such as G tube or NG tube placement.
During pandemic, treatment for anaphylaxis and FPIEs has also been slightly modified to avoid exposures to COVID‐19 in the healthcare setting as those risk and reduced with control of the infection normal. Patients are advised during anaphylaxis episode to self‐administer epinephrine and to call 911 only if symptoms do not resolve or worsen after first epinephrine dose; otherwise, they are advised to stay home. 8
Similarly, patients are advised to treat FPIEs acute episode at home unless severe dehydration ensues. 11
One challenge during pandemic is to find food allergen‐free or of a particular brand that patients are accustomed to; therefore, referral to nutrition to address the nutritional needs of patients may be warranted. 9
8.1. Allergic skin disorders, drug allergy, and venom allergy
For allergic skin disorder, specific recommendations on service reduction are as follows:
In patients with urticaria, angioedema, and atopic dermatitis, the majority of visits can be considered under the non‐urgent category where face‐to‐face care can be postponed or conducted via phone with digital photographs triage or telehealth. 3 , 10
Patients who are doing biologics for any of the above diseases can continue to receive those during the pandemic. For patients with known hereditary angioedema who develop an acute episode, visiting local urgent or emergency healthcare facilities is appropriate. Also, every effort should be made to obtain on‐demand therapy for home administration. 4 , 5
All visits can be postponed desensitization in the hospital setting for essential antibiotics can be done. 6
For venom allergy, being VIT of patients with a history of a systemic reaction to the venom, as this is a life‐threatening condition, is considered an essential service, as discussed before.
9. IMMUNODEFICIENCY
Patients with immunodeficiency are at high risk of complication for COVID‐19, so balance for prompt face‐in‐face service and risk that those services pose need to be carefully evaluated. Those patients can be continued on IVIG per regular therapy, although the IVIG products are unlikely to cover for the current virus, given the still low prevalence in the general population. Consideration to switch to subcutaneous vs IV formulation should be considered as well as at home vs. in hospital/office administration. Telehealth can be continued for those encounters that do not require in‐person visit. 4 , 5
10. CONCLUSIONS
A pandemic response is likely and once in a lifetime event, making challenging to reorganize clinical practice and continue to adapt those changes based on viral infection level in the community.
Any suggestions may, therefore, change rapidly based on the evolving situation on the territory. Limiting in‐person visit may have significant financial consequences, and also at a certain point, delay of procedure may represent a more significant risk for patient than the potential risk of being exposed to COVID‐19 and should be taken under consideration.
Author Contribution
Antonella Cianferoni: Conceptualization (equal); Methodology (equal); Project administration (equal); Writing‐original draft (equal); Writing‐review & editing (equal). Martina Votto: Methodology (equal); Data curation (equal); Writing‐original draft (equal).
Cianferoni A, Votto M. COVID‐19 and allergy: How to take care of allergic patients during a pandemic?. Pediatr Allergy Immunol. 2020;31(Suppl.26):96–101. 10.1111/pai.13367
References
- 1. Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID‐19) Outbreak in China: Summary of a Report of 72314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239. [DOI] [PubMed] [Google Scholar]
- 2. Del Rio C, Malani PN. 2019 Novel Coronavirus‐Important Information for Clinicians. JAMA. 2020;323(11):1039. [DOI] [PubMed] [Google Scholar]
- 3. CDC https://www.cdc.gov/coronavirus/2019‐ncov/index.html. CfDCaPCDC‐SSAf.
- 4. Shaker MS, Oppenheimer J, Grayson M, et al. COVID‐19: Pandemic Contingency Planning for the Allergy and Immunology Clinic. J Allergy Clin Immunol Pract. 2020;8(5):1477–1488.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brough HA, Kalayci O, Sediva A, et al. Managing childhood allergies and immunodeficiencies during respiratory virus epidemics ‐ the 2020 COVID‐19 pandemic. Pediatr Allergy Immunol. 2020. 10.1111/pai.13262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Epstein T. Administration of subcutaneous allergen immunotherapy during the COVID‐19 outbreak: A Work Group Report of the AAAAI Immunotherapy, Allergen Standardization and Allergy Diagnostics (IASAD) Committee. 2020.
- 7. Haberman R, Axelrad J, Chen A, et al. Covid‐19 in Immune‐Mediated Inflammatory Diseases ‐ Case Series from New York. N Engl J Med. 2020;383(1):85–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Casale TB, Wang J, Nowak‐Wegrzyn A. Acute At Home Management of Anaphylaxis During the Covid‐19 Pandemic. J Allergy Clin Immunol Pract. 2020;8(6):1795–1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Groetch M, Durban R, Meyer R, Venter C, Nowak‐Wegrzyn A. Dietary Management of Food Protein‐Induced Enterocolitis Syndrome during COVID‐19 Pandemic. Ann Allergy Asthma Immunol. 2020. 10.1016/j.anai.2020.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Vultaggio A. Considerations on Biologicals for Patients with allergic disease in times of the COVID‐19 pandemic. Allergy. 2020. 10.1111/all.14407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Nowak‐Wegrzyn A, Cianferoni A, Bird JA, et al. Medical Advisory Board of the International FPIES Association. Managing food protein‐induced enterocolitis syndrome during the coronavirus disease 2019 pandemic: Expert recommendations. Ann Allergy Asthma Immunol. 2020;125(1):14–16. 10.1016/j.anai.2020.04.032 [DOI] [PMC free article] [PubMed] [Google Scholar]


