Abstract
Interleukin‐6 (IL‐6)–mediated hyperinflammation may contribute to the mortality of coronavirus disease 2019 (COVID‐19). The IL‐6 receptor–blocking monoclonal antibody tocilizumab has been repurposed for COVID‐19, but prospective trials and dose‐finding studies in COVID‐19 have not yet fully reported. We conducted a single‐arm phase II trial of low‐dose tocilizumab in nonintubated hospitalized adult patients with COVID‐19, radiographic pulmonary infiltrate, fever, and C‐reactive protein (CRP) ≥ 40 mg/L. We hypothesized that doses significantly lower than the emerging standards of 400 mg or 8 mg/kg would resolve clinical and laboratory indicators of hyperinflammation. A dose range from 40 to 200 mg was evaluated, with allowance for one repeat dose at 24 to 48 hours. The primary objective was to assess the relationship of dose to fever resolution and CRP response. Thirty‐two patients received low‐dose tocilizumab, with the majority experiencing fever resolution (75%) and CRP decline consistent with IL‐6 pathway abrogation (86%) in the 24–48 hours following drug administration. There was no evidence of a relationship between dose and fever resolution or CRP decline over the dose range of 40–200 mg. Within the 28‐day follow‐up, 5 (16%) patients died. For patients who recovered, median time to clinical recovery was 3 days (interquartile range, 2–5). Clinically presumed and/or cultured bacterial superinfections were reported in 5 (16%) patients. Low‐dose tocilizumab was associated with rapid improvement in clinical and laboratory measures of hyperinflammation in hospitalized patients with COVID‐19. Results of this trial provide rationale for a randomized, controlled trial of low‐dose tocilizumab in COVID‐19.
Study Highlights.
WHAT IS THE CURRENT KNOWLEDGE ON THE TOPIC?
☑ Many patients with novel coronavirus disease 2019 (COVID‐19) develop acute lung injury and hypoxic respiratory failure possibly due to a hyperinflammatory state. Interleukin‐6 (IL‐6) has been implicated in this process; therefore patients with COVID‐19 may benefit from the IL‐6 receptor–blocking monoclonal antibody tocilizumab.
WHAT QUESTION DID THIS STUDY ADDRESS?
☑ No dose‐finding studies have been performed for tocilizumab in the setting of COVID‐19. This prospective phase II clinical trial is, to our knowledge, the first to evaluate different doses of tocilizumab in patients with COVID‐19.
WHAT DOES THIS STUDY ADD TO OUR KNOW‐LEDGE?
☑ The Tocilizumab to Prevent Clinical Decompensation in Hospitalized, Non‐critically Ill Patients With COVID‐19 Pneumonitis (COVIDOSE) study, together with retrospective and real‐world evidence studies, suggests that tocilizumab is a potential treatment for hyperinflammation among patients with COVID‐19. Randomized, controlled trials of tocilizumab, including one of low‐dose tocilizumab, in this patient population are ongoing.
HOW MIGHT THIS CHANGE CLINICAL PHARMA‐COLOGY OR TRANSLATIONAL SCIENCE?
☑ Under normal circumstances, application of interventional pharmacoeconomics (IVPE) can help contain drug costs through a reduction in units used. The COVIDOSE study demonstrates how interventional pharmacoeconomic principles can be applied to drug shortages in the context of a global pandemic.
The global pandemic of coronavirus disease 2019 (COVID‐19), the disease caused by severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), threatens public health, with quoted mortality among hospitalized patients exceeding 15%. 1 , 2 Late‐stage COVID‐19, marked by hyperinflammation leading to shock and respiratory failure, is associated with high levels of C‐reactive protein (CRP) and cytokines, including interleukin‐1 (IL‐1) and interleukin‐6 (IL‐6). 3 , 4 In patients with severe and critical COVID‐19, IL‐6–mediated hyperinflammation resembling cytokine release syndrome (CRS) may drive disease mortality, 5 suggesting that repurposing of anti–IL‐6 axis monoclonal antibodies such as tocilizumab, sarilumab, and siltuximab, or anti–IL1 therapies such as anakinra, warrant investigation. 3 , 5 , 6
Rapid resolution of clinical and biochemical signs of hyperinflammation has been noted following a single 400 mg dose of tocilizumab in patients with severe to critical COVID‐19, 7 and multicenter, retrospective case‐control studies suggest a 30% to 40% reduction in risk of invasive ventilation or COVID‐19–related mortality following tocilizumab. 8 , 9 , 10 Tocilizumab’s role in moderate, severe, and critical COVID‐19, however, remains ambiguous, with prospective data arguing both for and against its use. 11 An investigator‐initiated prospective, multi‐institutional, randomized, controlled trial evaluating tocilizumab 8 mg/kg in patients with moderate or severe COVID‐19 disease (CORIMUNO‐TOCI‐1 (Cohort Multiple Randomized Controlled Trials Open‐label of Immune Modulatory Drugs and Other Treatments in COVID‐19 Patients ‐ Tocilizumab Trial)) is positive, 12 while the EMPACTA (A Study to Evaluate the Efficacy and Safety of Tocilizumab in Hospitalized Participants With COVID‐19 Pneumonia) and COVACTA (A Study to Evaluate the Safety and Efficacy of Tocilizumab in Patients With Severe COVID‐19 Pneumonia) studies demonstrated decreased likelihood of death or mechanical ventilation and hospital length of stay, respectively. 13 , 14 Other prospective trials, however, have failed to meet diverse prespecified end points such as progression to critical disease, intensive care unit admission, or death and improvement in ordinal clinical status by day 28. 14 , 15 , 16
However, a tocilizumab dose lower than the labeled CRS dose of 8 mg/kg may be sufficient to block IL‐6 signaling. 17 Prior studies suggest that serum tocilizumab concentrations as low as 1 μg/mL—less than 1% of the peak concentration achieved with the 8 mg/kg dose—can blunt greater than 95% of IL‐6 receptor signaling. 18 A tocilizumab dose lower than 400 mg or 8 mg/kg may also be advantageous in COVID‐19. 17 In patients with COVID‐19, high doses of tocilizumab may increase the risk of secondary bacterial infections (e.g., hospital‐acquired and ventilator‐associated pneumonias) approximately fourfold. 8 , 9 Additionally, IL‐6 stimulates B‐cell proliferation, plasma cell maturation, and antibody responses. 19 , 20 , 21 Blocking IL‐6 receptor with tocilizumab might impair the generation of antibody responses to SARS‐CoV‐2. Therefore, administration of tocilizumab too early in the disease has the potential to suppress the adaptive immune response to SARS‐CoV‐2, and utilization of high doses of tocilizumab would be expected to suppress the immune system of patients for an extended period of time. Finally, using lower doses of tocilizumab may extend available supplies. 22
To our knowledge, no dose‐finding studies have been conducted for tocilizumab in COVID‐19. Drawing on lessons from interventional pharmacoeconomics (IVPE), 23 , 24 we hypothesized that doses of tocilizumab lower than those used in the outpatient rheumatologic (4–8 mg/kg) or the COVID‐19 settings (400 mg or 8 mg/kg) would reduce COVID‐19–related inflammation. 17 We developed a titration regimen to administer low‐dose tocilizumab to hospitalized patients with COVID‐19. 17 We present the results of our phase II study, demonstrating pharmacodynamic and clinical evidence of low‐dose tocilizumab activity in hospitalized patients with COVID‐19–associated hyperinflammation not requiring mechanical ventilation.
METHODS
Trial design and oversight
Tocilizumab to Prevent Clinical Decompensation in Hospitalized, Non‐critically Ill Patients With COVID‐19 Pneumonitis (COVIDOSE) was an investigator‐initiated, nonrandomized, open‐label, single‐arm phase II trial performed at a single site within the University of Chicago Medicine (UCM) health system. Details of the low‐dose tocilizumab treatment strategy have been described previously. 17 The University of Chicago sponsored and funded the trial, without any industry involvement. The trial was registered with the National Clinical Trials Registry (NCT04331795).
Study participants
Eligible patients were those hospitalized at UCM, aged 18 years or older, and who had (i) positive polymerase chain reaction test for SARS‐CoV‐2 RNA, (ii) chest radiograph findings such as bilateral ground glass opacities or hazy bilateral infiltrates consistent with viral or atypical pneumonia (as determined by UCM radiologists providing usual clinical care independent of COVIDOSE), (iii) documented fever, defined as temperature ≥ 38.0°C in the 24 hours prior to the time of tocilizumab administration as measured by commonly accepted clinical methods (predominantly oral or axillary), and (iv) CRP ≥ 40 mg/L. Key exclusion criteria included use of invasive mechanical ventilation, scheduled antipyretic medications (as‐needed administration of antipyretic following documented fever was allowed), vasopressor medications, active therapy with biologic immunosuppressive or Janus kinase inhibitor medications, and previous receipt of an investigational antiviral agent or off‐protocol anti–IL‐6 receptor therapy. Full eligibility criteria are available in the trial protocol, available in the Supplementary Material . Patients or their legally authorized representatives provided written or electronic informed consent.
Trial procedures
Enrolled patients were subdivided into two groups (Group A and Group B) based on laboratory signs of hyperinflammation and the presence or absence of risk factors for COVID‐19–related mortality (based on extant univariate regressions at the time of study and as agreed to by a multidisciplinary panel of institutional experts). Risk factors, nearly all of which were subsequently validated, 25 included any previous intensive care unit admission; previous nonelective intubation; hospitalization for exacerbation of congestive heart failure or chronic obstructive pulmonary disease in the past 12 months; coronary artery disease requiring percutaneous coronary intervention or coronary artery bypass grafting; stroke with residual neurologic deficit; pulmonary hypertension; home supplemental oxygen use; interstitial lung disease; asthma requiring inhaled corticosteroid use; history of pneumonectomy, lobectomy, or radiation therapy to lung; HIV/AIDS; cancer diagnosis (any stage) receiving nonhormonal treatment; immunodeficiency; end‐stage renal disease requiring hemodialysis or peritoneal dialysis; body mass index ≥ 30 kg/m2; and inpatient supplemental oxygen requirement > 6 L/minute at the time of enrollment. Group A patients had CRP ≥ 75 mg/L and at least one risk factor for mortality. Group B patients had CRP of 40–74 mg/L or lacked risk factors for COVID‐19–related mortality. This strategy was utilized to justify testing of a lower dose of tocilizumab in patients deemed at lower risk of death from COVID‐19.
After group assignment, patients were treated according to the low‐dose tocilizumab algorithm, integrated into usual clinical care (Figure S1 ). 17 Group A patients received tocilizumab 200 mg or, later, 120 mg. Group B patients received 80 mg or, later, 40 mg. The study was an adaptive design, and all dosage levels were protocol‐based and determined on a cohort basis by the trial operating committee (comprised of the investigators). The study began with 200‐mg and 80‐mg dose levels. After observing clinical and biochemical responses to the 200‐mg and 80‐mg dose levels and no safety events, we transitioned to 120‐mg and 40‐mg dose levels. Vital signs and laboratory studies were monitored per usual clinical care. CRP was evaluated immediately prior to tocilizumab administration (baseline) and approximately 24 hours following tocilizumab administration.
Patients were eligible for re‐dosing with tocilizumab. In the originally developed re‐dosing schema, the decision was guided strictly by CRP response. In an amended version of the protocol, however, the re‐dosing decision was guided by biochemical and clinical parameters. Patients were re‐dosed with tocilizumab if signs of clinical worsening (as defined by increased supplemental oxygen requirement or worsening fever curve determined by maximum temperature) were accompanied by CRP decline of < 25% when compared with baseline at the 24‐hour assessment (Figure S1 ). In the COVIDOSE algorithm, treating physicians maintained the option of administering off‐protocol tocilizumab (generally 400 mg) as indicated per their clinical judgment. Please see the Supplementary Material for further information.
Patients were followed for the duration of their hospitalization and were contacted 28 days after tocilizumab administration. At the 28‐day timepoint, survival, clinical status (including admission to a medical or assisted living facility), new or persistent supplemental oxygen requirement, and any notable diagnoses or treatments for secondary infection were documented. The initial planned enrollment was fifty patients, with the goal of determining the lowest pharmacodynamically active dose of tocilizumab (in the context of analyzing the dose–response relationship) for the treatment of COVID‐19. After enrolling the thirty‐second patient, remdesivir received Emergency Use Authorization and quickly became institutional standard of care. 26 To avoid collecting heterogeneous data confounded by remdesivir use, the COVIDOSE trial operating committee elected to close the study to further enrollment; it was not closed due to safety concerns.
Outcomes
The primary clinical outcome was resolution of fever in the 24‐hour period following tocilizumab, defined as a maximum temperature < 38.0°C. Fever resolution was chosen for its rapid readout and as a proxy for discharge in high‐risk patients with COVID‐19 who did not require supplemental oxygen (i.e., in the absence of requirement for supplemental oxygen in a high‐risk patient, a fever might prevent discharge while its absence might allow discharge). Patients’ requirement for supplemental oxygen was also tracked, so as to inform re‐dosing decisions (Figure S1 ). Originally, the primary biochemical outcomes were rate of and time to CRP normalization, guided by earlier tocilizumab‐related work. 7 , 17 During the conduct of the study, it became apparent that CRP normalization would lag behind a patient’s clinical improvement and the patient could be safely discharged before CRP had normalized, making CRP normalization an impractical outcome measure. We therefore report the percentage of patients who achieved biochemical response, defined as a CRP reduction ≥ 25% from baseline in the 24–48 hours after tocilizumab administration, consistent with a decline determined by CRP half‐life. 7 , 27
Secondary outcomes included overall survival at 28 days, survival to hospital discharge, rate and duration of nonelective mechanical ventilation, time to mechanical ventilation, rate and duration of vasopressor/inotropic agent utilization, time to vasopressor/inotropic agent utilization, and number of days spent in intensive care unit. One month after enrollment began, duration of supplemental oxygen requirement greater than a patient’s baseline was added. Definitions of outcomes are provided in the protocol.
Post Hoc evaluation of clinical recovery
Randomized, controlled trials of COVID‐19 therapies had not been published at the time of COVIDOSE initiation but were published prior to COVIDOSE data maturity. 28 To add context to COVIDOSE results, time to clinical recovery was evaluated post hoc. Using a previously developed seven‐point ordinal scale, 29 disease severity was assessed daily, with the patient’s worst clinical status and consequent ordinal score recorded for a given day. 28 , 29 Recovery was defined as the first day on which a patient achieved a clinical status of either “hospitalization without need for supplemental oxygen or ongoing medical care” or “not hospitalized.” 28 , 29 Time to recovery was defined as the time in days from study enrollment to achievement of recovery. 28 Two independently operating authors (G.W.S. and P.D.R.) adjudicated ratings.
Statistical analysis
We generated descriptive statistics of the clinical and biochemical response rates of patients treated with low‐dose tocilizumab. We assessed differences in the clinical and biochemical response rates between different tocilizumab doses using a two‐sided Fisher exact test, unadjusted for cohort or other risk factors. A P value of < 0.05 was considered to indicate statistical significance. All analyses were performed using Stata (Stata Corp., College Station, TX). For post hoc analysis, descriptive data summaries are reported as median (interquartile range (IQR)) or percentages.
Ethics approval
The UCM institutional review board (IRB) approved the trial protocol. Given the rapidly evolving landscape of COVID‐19, the IRB authorized an internal trial operating committee comprised of investigators to facilitate dose modifications based on incoming data (full details of this operating structure are available in the COVIDOSE trial protocol and Supplementary Material at Clinical Pharmacology & Therapeutics’ website). An internal data monitoring committee oversaw the trial’s progress and adjudicated outcomes, safety signals, and potential protocol deviations in weekly meetings. All authors attest to the validity of the data and adherence to the trial protocol, with reporting of violations where indicated.
RESULTS
Trial population
From April 1 through May 13, 2020, 32 patients consented to participate in COVIDOSE. Twelve were assigned to Group A, 8 of whom received 200 mg and 4 of whom received 120 mg. Twenty were assigned to Group B, 15 of whom received 80 mg and 5 of whom received 40 mg (Figure 1 ). Median time from hospital admission to study enrollment was 1 day (IQR, 1–2 days). All patients were included in the statistical analysis of fever resolution, and 29 patients were included in the statistical analysis of CRP response. Characteristics of the COVIDOSE subpopulations are summarized in Table 1 . Re‐dosing of low‐dose tocilizumab is discussed in the Supplementary Materials .
Figure 1.
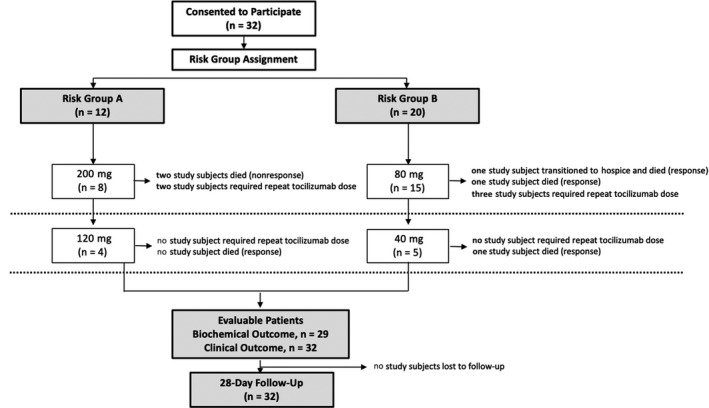
Flow of patients in the COVIDOSE trial. Thirty‐two eligible patients consented to participate in the COVIDOSE trial, of which 12 were assigned to Group A and 20 were assigned to Group B on the bases of magnitude of C‐reactive protein elevation and epidemiologic risk factors for COVID‐19 related mortality. Group A patients received either 200 or 120 mg of tocilizumab and were followed for 28 days following drug administration. Group B patients received either 80 or 40 mg of tocilizumab and were followed for 28 days following drug administration. All 32 patients were evaluable for the purposes of primary clinical outcome and 29 were evaluable for biochemical outcome. No patients were lost to follow‐up.
Table 1.
Demographic, clinical, and laboratory characteristics of patients enrolled on COVIDOSE
|
COVIDOSE Group A n = 12 |
COVIDOSE Group B n = 20 |
Overall COVIDOSE Population n = 32 |
|
|---|---|---|---|
| Age, median (IQR), years | 70 (51, 73) | 66 (41, 73) | 69 (41, 73) |
| Male sex, n, (%) | 7 (58.3%) | 9 (45.0%) | 16 (50.0%) |
| Race, n, (%) | |||
| White | 1 (8.3%) | 0 (0%) | 1 (3.1%) |
| Black | 9 (75.0%) | 16 (80.0%) | 25 (78.1%) |
| Hispanic/Latinx | 2 (16.7%) | 1 (5.0%) | 3 (9.4%) |
| Multiracial, other, prefer not to identify | 0 (0.0%) | 3 (15.0%) | 3 (9.4%) |
| Comorbidities per patient, n, (%) | |||
| None | 0 (0%) | 4 (20.0%) | 4 (12.5%) |
| 1 | 2 (16.7%) | 6 (30.0%) | 8 (25.0%) |
| 2 | 4 (33.3%) | 6 (30.0%) | 10 (31.3%) |
| 3 or greater | 6 (50.0%) | 4 (20.0%) | 10 (31.3%) |
| Epidemiologic risk factors from risk group stratification per patient, n, (%) | |||
| None | 1 (8.3%) | 12 (60.0%) | 13 (40.6%) |
| 1 | 5 (41.7%) | 5 (25.0%) | 10 (31.3%) |
| 2 | 5 (41.7%) | 3 (15.0%) | 8 (25.0%) |
| 3 or greater | 1 (8.3%) | 0 (0%) | 1 (3.1%) |
| Medications, at baseline, n, (%) | |||
| Hydroxychloroquine | 4 (33.3%) | 6 (30.0%) | 10 (31.3%) |
| Azithromycin | 5 (41.7%) | 8 (40.0%) | 13 (40.6%) |
| Lopinavir‐Ritonavir | 1 (8.3%) | 3 (15.0%) | 4 (12.5%) |
| Systemic corticosteroid (within 24h of enrollment) | 0 (0%) | 0 (0%) | 0 (0%) |
| Supplemental O2 Requirement at enrollment (eligibility), n, (%) | |||
| None | 2 (16.7%) | 6 (30.0%) | 8 (25.0%) |
| Low‐flow oxygen | 9 (75.0%) | 13 (65.0%) | 22 (68.8%) |
| Noninvasive ventilation or high‐flow oxygen | 1 (8.3%) | 1 (5.0%) | 2 (6.5%) |
| C‐Reactive Protein, baseline, mean (SEM), mg/L | 175 (24) | 138 (17 | 152 (14) |
| D‐dimer, baseline, mean (SEM), pg/mL | 1.98 (0.50) | 2.2 (0.96) | 2.12 (0.62) |
| Ferritin, baseline, mean (SEM), pg/mL | 2022 (458) | 1151 (308) | 1478 (264) |
| COVID‐GRAM risk prediction score, median (IQR) | 126.8 (113.5, 151.8) | (102.3, 158.9) |
IQR, interquartile range.
Clinical outcomes
The trend of the maximum daily temperature (mean ± standard error of the mean) in COVIDOSE patients is shown in Figure 2a . At 24 hours following tocilizumab administration, 24 COVIDOSE patients (75.0%) were afebrile (maximum temperature < 38·0°C), including 67% of patients in Group A and 80% of those in Group B (Figure 2b ). There was no evidence of a relationship between the tocilizumab dose and rate of fever resolution in the first 24 hours (Figure 2c ). Ten of the 24 patients (42%) with baseline supplemental oxygen requirement had a decrease in maximum oxygen requirement in the first 24 hours following tocilizumab administration.
Figure 2.
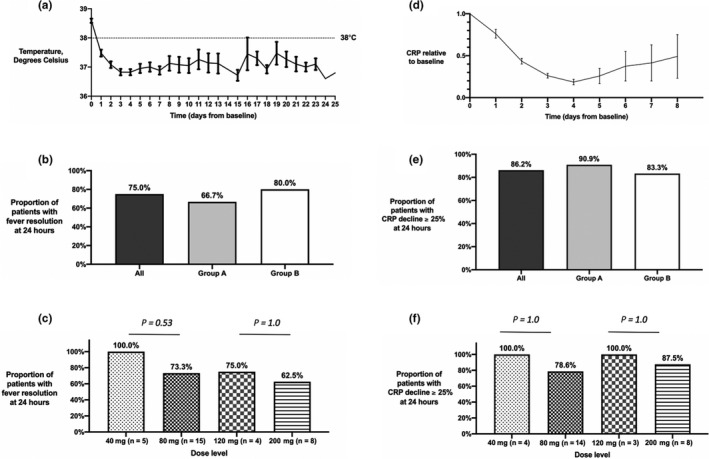
Temperature and CRP decrease rapidly following administration of low‐dose tocilizumab. (a) Temperature values for COVIDOSE patients following eligibility (mean ± standard error of mean). (b) Percentage of COVIDOSE (dark gray), COVIDOSE Group A (light gray), and COVIDOSE Group B (white) patients meeting the primary outcome of Tmax24 hours < 38.0°C. (c) Relationship between tocilizumab dose and probability of achieving fever resolution. Percentage of COVIDOSE patients at the noted tocilizumab dose levels achieving the outcome of Tmax24 hours < 38.0°C. Bars denote one‐sided Fisher exact test for difference in proportions. P values are as shown in the panel. (d) Representative CRP values for COVIDOSE patients following eligibility (mean ± standard error of mean). (e) Percentage of COVIDOSE (dark gray), COVIDOSE Group A (light gray), and COVIDOSE Group B (white) patients meeting the primary biochemical outcome of CRP decline of ≥ 25% at 24 hours. (f) Relationship between tocilizumab dose and probability of achieving CRP decline of ≥ 25%. Percentage of COVIDOSE patients at the noted tocilizumab dose levels achieving CRP decline of ≥ 25%. Bars denote one‐sided Fisher exact test for difference in proportions. P values are as shown in the panel figure. CRP, C‐reactive protein; Tmax24 hours, maximum temperature within 24 hours following drug administration.
Biochemical outcomes
The CRP trend (mean ± standard error of the mean) for the COVIDOSE population is shown in Figure 2d . The vast majority (29/32) of patients were evaluable for CRP response, of whom 25 (86%) achieved CRP decrease ≥ 25%. This included 91% of Group A patients and 83% of Group B patients (Figure 2e ). There was no evidence of a relationship between tocilizumab dose and likelihood of achieving CRP decrease ≥ 25% (Figure 2f ).
Post hoc evaluation of recovery time and safety
The 28‐day mortality rate was 16% (Table 2 ). The median time to recovery for the remaining patients was 3 days (IQR, 2–5), and appeared to be associated with the severity of disease at enrollment (Table 2 ). Culture‐proven or clinically suspected ventilator‐associated or hospital‐acquired pneumonias were identified in 5 (16%) patients.
Table 2.
Post hoc clinical outcomes in the overall COVIDOSE study population
| Overall | Ordinal Score at Baseline | Risk Group Stratification at Baseline | ||||
|---|---|---|---|---|---|---|
| 3 – NIV, HHFNC (n = 4) | 4 – Low‐flow oxygen (n = 17) | 5 – No supp. oxygen (n = 11) | Risk Group A (n = 12) | Risk Group B (n = 20) | ||
| Recovery | ||||||
| No. of recoveries | 27 | 2 | 15 | 10 | 10 | 17 |
| Median time to recovery (IQR), days | 3 (2–5) | 11.5 (10.75–12.25) | 4 (3–5) | 2 (2–3) | 4.5 (2.5–6.75) | 3 (2–4) |
| Mortality | ||||||
| No. of deaths by day 28 | 5 | 2 | 2 | 1 | 2 | 3 |
Post hoc clinical outcomes in the overall COVIDOSE study population, according to baseline ordinal clinical status and risk group assignment.
HHFNC, heated high‐flow nasal cannula; IQR, interquartile range; NIV, noninvasive ventilation; supp., supplemental.
DISCUSSION
Low‐dose tocilizumab was clinically and biochemically active in patients with COVID‐19 and related hyperinflammation who did not require invasive ventilation, with no apparent relationship between tocilizumab dose and clinical or biochemical improvement over the studied dose range of 40 to 200 mg. Although the minimum effective dose of tocilizumab was not identified in this clinical trial, the COVIDOSE study demonstrated that a tocilizumab dose of 40 mg may be sufficient to blunt the clinical and biochemical signs of COVID‐19–related hyperinflammation. Referencing clinical pharmacology arguments, 17 the absence of a dose–response relationship suggests that a dose much lower than those utilized in other COVID‐19 studies (400 mg) or approved by regulatory bodies for the treatment of chimeric antigen receptor T‐cell–related CRS (4–8 mg/kg) may be sufficient to blunt IL‐6–mediated hyperinflammation. The COVIDOSE trial provides proof of concept for a COVID‐19 therapeutic strategy centered on the administration of low‐dose tocilizumab, with re‐dosing guided by readily assessable clinical and biochemical responses.
To our knowledge, COVIDOSE is the first trial to provide prospectively collected evidence of low‐dose tocilizumab’s clinical benefit. Marked declines in maximum body temperature and CRP were noted in the 24–48 hours following administration of low‐dose tocilizumab—responses that mimic those observed in patients with severe and critical COVID‐19 who received tocilizumab 400 mg. 7 Though an increase in CRP after day 4 may be suggested by the data presented, it is not necessarily statistically or clinically significant and is likely attributable to COVIDOSE patients being more chronically ill than other hospitalized patients with COVID‐19 and at higher likelihood for secondary issues. The issue will be fully explored in an ongoing randomized, controlled trial. 30 In comparison with a retrospectively identified cohort of similar patients who did not receive tocilizumab, CRP and temperature declines occurred more rapidly in COVIDOSE‐enrolled patients. 31 Post hoc analysis of COVIDOSE patients’ clinical trajectories provides encouraging evidence of low‐dose tocilizumab’s benefit. Patients requiring supplemental oxygen at enrollment experienced median time to recovery of 4 days. This is an encouraging finding in the context of a median time to recovery of approximately 7 days in a similarly risked subpopulation receiving remdesivir. 28 Notably, the COVIDOSE population had higher likelihood of comorbidities associated with poor COVID‐19–related outcomes. 28 The COVIDOSE data add context to the emerging real‐world evidence for tocilizumab’s benefit and will add context to the interpretations of the COVACTA, CORIMUNO‐TOCI, and Randomised Evaluation of COVID‐19 Therapy (RECOVERY) tocilizumab trials once these studies are published. 8 , 9 , 32 , 33 Care needs to be taken in interpreting these studies given significant heterogeneity found in the control arms of COVID‐19 therapeutic trials—14‐day mortality of 13.4% in Adaptive COVID‐19 Treatment Trial (ACTT‐1) (16.5% in the subgroup of patients requiring invasive mechanical ventilation) and 22‐day mortality of 22.9% in the overall population of RECOVERY. 2 , 28
More relevant moving forward is where tocilizumab fits into a COVID‐19 treatment paradigm that consists of remdesivir with the possible addition of corticosteroids for patients who require mechanical ventilation and, depending on local institutional standards, supplemental oxygen. 34 , 35 The field lacks evidence‐based, highly efficacious treatment for patients with severe (but not critical) COVID‐19—the confidence interval of the hazard ratios for corticosteroids in this clinical scenario ranges from 0.73 to 1.00. 34 Strategies including drugs that are both accurate and precise—Janus kinase inhibitors or IL–6‐targeted drugs, for example—may be beneficial in patients who are not yet intubated, as suggested by early press releases describing the possible efficacy of baricitinib in COVID‐19. 36 Tocilizumab’s role in moderate, severe, and critical COVID‐19 remains ambiguous. 11 Benefit has been identified in the prospective EMPACTA and CORIMUNO‐TOCI‐1 randomized controlled trials, 12 , 13 with these studies meeting their primary end points of death or mechanical ventilation and survival without mechanical ventilation, respectively. The COVACTA study demonstrated a marked decrease in hospital length of stay, but failed to meet its primary end point of improvement in ordinal clinical status at day 28. 14 Recently published studies, though likely underpowered, failed to meet their primary end points of progression to death, intensive care unit admission, or critical disease, respectively. 15 , 16 Trials that have not yet reported include A Study to Evaluate the Efficacy and Safety of Remdesivir Plus Tocilizumab Compared With Remdesivir Plus Placebo in Hospitalized Participants With Severe COVID‐19 Pneumonia (REMDACTA) and our own Low‐Dose Tocilizumab Versus Standard of Care in Hospitalized Patients With COVID‐19 (COVIDOSE‐2) study. 30 , 37 The latter of these studies allows for concomitant remdesivir and/or corticosteroids and allows for enrollment on one of two substudies at the discretion of clinicians—one substudy evaluates against a tocilizumab‐free control arm while the other evaluates against a comparator of the standard 400 mg dose of tocilizumab. 30 As this body of evidence develops, the COVIDOSE data will become particularly compelling.
The data presented in COVIDOSE suggest that a threefold to 10‐fold tocilizumab supply expansion may be possible due to lower dosing regimens. In this trial, we administered a total of 4,120 mg of tocilizumab, corresponding to 37 doses for 32 patients. In comparison, 12,800 mg would have been administered had each patient received 400 mg. 7 , 33 The EMPACTA, CORIMUNO‐TOCI‐1, and COVACTA trials utilize a dose of 8 mg/kg. 12 , 13 , 14 Rapid, global scaling is necessary for tocilizumab to become a safe, effective, and equitable therapy for hospitalized patients with COVID‐19, and an IVPE‐based approach is one possible strategy for extending supplies. 17 , 22
Beyond sustainability, low‐dose tocilizumab may be clinically advantageous over higher dosages. Utilizing lower doses of tocilizumab may lessen the depth and duration of its immunosuppressive effect while retaining clinical benefit, as evidenced by declines in maximum temperature and CRP. Despite a rate of secondary bacterial infection fourfold of that observed in COVIDOSE, mechanically ventilated patients who received tocilizumab 8 mg/kg derived survival benefit. 8 , 9 How the prospectively collected rates of secondary infections compare between low‐dose tocilizumab‐ treated, tocilizumab 8mg/kg–treated, and dexamethasone‐treated patients, as well as the combination of dexamethasone and tocilizumab, remains to be seen, but lower doses of tocilizumab may be advantageous. 2 A priori rationale for the safety of combining corticosteroid and tocilizumab can be found in the treatment of giant cell arteritis. 38 Finally, in biological studies conducted in parallel with COVIDOSE, no statistically significant differences in anti–SARS‐CoV2 antibody production between patients treated with any dose of tocilizumab, remdesivir, or supportive care alone were identified. 39 Carefully conducted prospective trials with appropriate biological correlative studies are needed.
The COVIDOSE trial is not without limitations. It was a small, single‐center study conducted at a tertiary care center with active research efforts in COVID‐19–related supportive care. The absence of a randomized control arm limits formal conclusions about low‐dose tocilizumab’s safety and efficacy. The rapidly changing understanding of COVID‐19 and local practice prevented trending CRP to normalization, leading to the need for reporting of a different biochemical outcome than originally expected. The COVIDOSE study, however, provides proof of concept as well as valuable lessons that are being incorporated into a randomized, controlled trial evaluating the clinical efficacy of low‐dose tocilizumab in COVID‐19. 30
Funding
This trial was funded and sponsored by the University of Chicago. The institution had no role in the design, execution, or analysis of this trial. There was no industry involvement in COVIDOSE.
Conflict of Interest
G.W.S. is supported by the Richard and Debra Gonzalez Research Fellowship at the University of Chicago (established through philanthropy by Abbott Laboratories; Lake Bluff, Illinois, USA). B.L.H. is funded by the T32 GM007019 grant from the National Institute of General Medical Sciences. M.E.S. reports research grants from Boerhinger Ingelheim, Galapagos and Novartis and personal fees from Boerhinger Ingelheim and Genentech. M.J.R. reports other support including the following: personal fees from multiple generic companies, personal fees from Cyclacel, personal fees from Aptevo, personal fees from Shionogi, other from Dicerna, personal fees and other from Genentech, other from BeiGene, other from AbbVie, other from Corvus, other from Bristol‐Myers Squibb, other from Xencor, outside the submitted work. In addition, M.J.R. has a patent US6395481B1 with royalties paid to Mayo Medical, a patent EP1629111B1 with royalties paid to Mayo Medical, a patent US8877723B2 issued, a patent US9617583B2 issued, and a patent provisional patent pending and Director and Treasurer, Value in Cancer Care Consortium. G.W.S., B.L.H., P.D.R., and M.J.R. are coinventors of a filed provisional patent on the use of low‐dose tocilizumab in viral infections. All other authors declared no competing interests for this work.
Author Contributions
G.W.S., M.J.R., and P.D.R. wrote the manuscript. G.W.S., B.L.H., S.J.R., J.A.T., C.C.E., I.B.V., N.N.P., B.K.P., J.P., M.E.S., T.F.G., M.J.R., and P.D.R. designed the research. G.W.S., B.L.H., S.J.R., J.A.T., J.Y., A.J.K., R.C.W., A.K.K., K.D., E.F.H., J.C.B., A.C., and P.D.R. performed the research. G.W.S., A.J.K., T.G.K., T.F.G., M.J.R., and P.D.R. analyzed the data. E.F.H. and A.W. contributed new reagents/analytical tools.
Supporting information
Fig S1
Supplementary Material1
Supplementary Material2
Acknowledgments
The authors wish to thank Spring Maleckar for her assistance and contributions in creating the REDCap database and Bethany Martell for her expertise throughout aspects of the COVIDOSE trial’s proceedings. We also thank Athalia Pyzer, MD, Yuanyuan Zha, Blake Flood, Glee Li, Hongyuan Jiao, Apameh Pezeshk, Lara Kozloff, Randy Sweis, MD, and the Human Immunologic Monitoring core facility of the University of Chicago Comprehensive Cancer Center for contributions to the COVID‐19 biobanking project.
Trial Registration: ClinicalTrials.gov number NCT04331795.
References
- 1. Petrilli, C.M. et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ 369, m1966 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Horby, P. et al. Dexamethasone in hospitalized patients with Covid‐19 — preliminary report. N. Engl. J. Med. (2020). 10.1056/NEJMoa2021436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mehta, P. , McAuley, D.F. , Brown, M. , Sanchez, E. , Tattersall, R.S. & Manson, J.J. COVID‐19: consider cytokine storm syndromes and immunosuppression. Lancet 395, 1033–1034 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Siddiqi, H.K. & Mehra, M.R. COVID‐19 illness in native and immunosuppressed states: a clinical‐therapeutic staging proposal. J. Heart Lung Transplant. 39, 405–407 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Liu, T. et al. The potential role of IL‐6 in monitoring coronavirus disease 2019. In Preprints with The Lancet, SSRN First Look (Huazhong University of Science and Technology, The Lancet, 2020). 10.2139/ssrn.3548761 [DOI] [Google Scholar]
- 6. Cavalli, G. et al. Interleukin‐1 blockade with high‐dose anakinra in patients with COVID‐19, acute respiratory distress syndrome, and hyperinflammation: a retrospective cohort study. Lancet Rheumatol. 2, e325–e331 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Xu, X. et al. Effective treatment of severe COVID‐19 patients with tocilizumab. Proc. Natl. Acad. Sci. USA. 117, 10970–10975 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Guaraldi, G. et al. Tocilizumab in patients with severe COVID‐19: a retrospective cohort study. Lancet Rheumatol. 2, e474–e484 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Somers, E.C. et al. Tocilizumab for treatment of mechanically ventilated patients with COVID‐19. Clin. Infect. Dis. (2020). 10.1093/cid/ciaa954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gupta, S. et al. Association between early treatment with tocilizumab and mortality among critically Ill patients with COVID‐19. JAMA Intern. Med. (2020). 10.1001/jamainternmed.2020.6252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Parr, J.B. Time to reassess tocilizumab's role in COVID‐19 pneumonia. JAMA Intern. Med. (2020). 10.1001/jamainternmed.2020.6557 [DOI] [PubMed] [Google Scholar]
- 12. Hermine, O. et al. Effect of tocilizumab vs usual care in adults hospitalized with COVID‐19 and moderate or severe pneumonia: a randomized clinical trial. JAMA Intern. Med. (2020). 10.1001/jamainternmed.2020.6820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Genentech/Roche . Roche's phase III EMPACTA study showed Actemra/RoActemra reduced the likelihood of needing mechanical ventilation in hospitalised patients with COVID‐19 associated pneumonia <https://www.roche.com/investors/updates/inv‐update‐2020‐09‐18.htm> (2020). Accessed September 18, 2020.
- 14. Rosas, I. et al. Tocilizumab in hospitalized patients with COVID‐19. medRxiv (2020). 10.1101/2020.08.27.20183442 [DOI] [Google Scholar]
- 15. Salvarani, C. et al. Effect of tocilizumab vs standard care on clinical worsening in patients hospitalized with COVID‐19 pneumonia: a randomized clinical trial. JAMA Intern. Med. (2020). 10.1001/jamainternmed.2020.6615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stone, J.H. et al. Efficacy of tocilizumab in patients hospitalized with Covid‐19. N. Engl. J. Med. (2020). 10.1056/NEJMoa2028836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Strohbehn, G.W. , Reid, P.D. & Ratain, M.J. Applied clinical pharmacology in a crisis: Interleukin‐6 axis blockade and COVID‐19. Clin. Pharmacol. Ther. 108, 425–427 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. US Food and Drug Administration. Multi‐Discipline Review: Application Number BLA 125276 S‐114 (US Food and Drug Administration, Montgomery County, 2017). [Google Scholar]
- 19. Muraguchi, A. et al. The essential role of B cell stimulatory factor 2 (BSF‐2/IL‐6) for the terminal differentiation of B cells. J. Exp. Med. 167, 332–344 (1988). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kopf, M. , Herren, S. , Wiles, M.V. , Pepys, M.B. & Kosco‐Vilbois, M.H. Interleukin 6 influences germinal center development and antibody production via a contribution of C3 complement component. J. Exp. Med. 188, 1895–1906 (1998). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Huang, H.‐Y. et al. Identification of a new subset of lymph node stromal cells involved in regulating plasma cell homeostasis. Proc. Natl. Acad. Sci. USA 115, E6826–E6835 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Patel, A. et al. Low‐dose abiraterone in metastatic prostate cancer: is it practice changing? Facts and facets. JCO Glob. Oncol. 6, 382–386 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ratain, M.J. , Goldstein, D.A. & Lichter, A.S. Interventional pharmacoeconomics‐a new discipline for a cost‐constrained environment. JAMA Oncol. 5, (2019). 10.1001/jamaoncol.2019.1341 [DOI] [PubMed] [Google Scholar]
- 24. Serritella, A.V. , Strohbehn, G.W. , Goldstein, D.A. , Lichter, A.S. & Ratain, M.J. Interventional pharmacoeconomics: a novel mechanism for unlocking value. Clin. Pharmacol. Ther. 108, 487–493 (2020). [DOI] [PubMed] [Google Scholar]
- 25. Williamson E.J. et al. Factors associated with COVID‐19‐related death using OpenSAFELY. Nature 584(7821), 430–436 (2020). 10.1038/s41586-020-2521-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hinton, D.M. Remdesivir EUA Letter of Authorization (ed. Food and Drug Administration of the United States of America ) 1–6 (United States Food and Drug Administration, Montgomery County, 2020). [Google Scholar]
- 27. Pepys, M.B. & Hirschfield, G.M. C‐reactive protein: a critical update. J. Clin. Invest. 111, 1805–1812 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Beigel J.H. et al. Remdesivir for the treatment of Covid‐19 — final report. N. Engl. J. Med. 383(19), 1813–1826 (2020). 10.1056/nejmoa2007764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Goldman, J.D. et al. Remdesivir for 5 or 10 days in patients with severe Covid‐19. N. Engl. J. Med. 383, 1817–1837 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. University of Chicago . Low‐dose tocilizumab versus standard of care in hospitalized patients with COVID‐19 (COVIDOSE‐2). Available from: https://clinicaltrials.gov/ct2/show/NCT04479358. NLM Identifier: NCT04479358. Accessed August 7, 2020.
- 31. Strohbehn, G.W. COVIDOSE: low‐dose tocilizumab in the treatment of COVID‐19 pneumonitis. AACR Virtual Meeting: Covid‐19 and Cancer,July 20–22, 2020.
- 32. Hoffmann‐La Roche . A study to evaluate the safety and efficacy of tocilizumab in patients with severe COVID‐19 pneumonia (COVACTA). Available from: https://clinicaltrials.gov/ct2/show/NCT04320615. NLM Identifier: NCT04320615. Accessed March 30, 2020.
- 33. Assistance Publique–Hôpitaux de Paris. Tocilizumab improves significantly clinical outcomes of patients with moderate or severe COVID‐19 pneumonia <https://www.aphp.fr/contenu/tocilizumab‐improves‐significantly‐clinical‐outcomes‐patients‐moderate‐or‐severe‐covid‐19> (2020). Accessed April 28, 2020.
- 34. Sterne, J.A.C. et al. Association between administration of systemic corticosteroids and mortality among critically Ill patients with COVID‐19: a meta‐analysis. JAMA 324, 1330–1341 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Prescott, H.C. & Rice, T.W. Corticosteroids in COVID‐19 ARDS: evidence and hope during the pandemic. JAMA 324, 1292–1295 (2020). [DOI] [PubMed] [Google Scholar]
- 36. PR Newswire Association . Baricitinib in combination with remdesivir reduces time to recovery in hospitalized patients with COVID‐19 in NIAID‐sponsored ACTT‐2 trial <https://www.prnewswire.com/news‐releases/baricitinib‐in‐combination‐with‐remdesivir‐reduces‐time‐to‐recovery‐in‐hospitalized‐patients‐with‐covid‐19‐in‐niaid‐sponsored‐actt‐2‐trial‐301129865.html> (2020). Accessed September 14, 2020.
- 37. Hoffmann‐La Roche . A study to evaluate the efficacy and safety of remdesivir plus tocilizumab compared with remdesivir plus placebo in hospitalized participants with severe COVID‐19 pneumonia (REMDACTA). Available from: https://clinicaltrials.gov/ct2/show/NCT04409262. NLM Identifier: NCT04409262. Accessed June 9, 2020.
- 38. Stone, J.H. , Klearman, M. & Collinson, N. Trial of tocilizumab in giant‐cell arteritis. N. Engl. J. Med. 377, 1494–1495 (2017). [DOI] [PubMed] [Google Scholar]
- 39. Cabanov, A. et al. Treatment with tocilizumab does not inhibit induction of anti‐COVID antibodies in patients with severe SARS‐CoV‐2 infection. AACR Virtual Meeting: COVID and Cancer, July 20–22, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fig S1
Supplementary Material1
Supplementary Material2


