Dear Editor,
Since the onset of the COVID‐19 pandemic, an abrupt behavioural change in the form of the widespread wearing of masks has become prominent. 1 Wearing a mask is beneficial in lowering the risk of virus transmission. However, this measure is also known to cause various facial skin problems, 2 , 3 and their incidence might differ with the type of mask used.
The primary objective of this study was to determine and compare the incidences of adverse skin reactions for the mask types used by the general population during the COVID‐19 pandemic. This survey study was conducted in Thailand in May 2020, during the national lockdown. Self‐administered questionnaires were distributed via an online platform. Healthcare workers were excluded.
A total of 1231 participants completed the questionnaires. Most respondents were female (73.8%) and aged above 30 years (72.1%). The most common baseline skin type was oily skin (45.3%) and mild acne (55.8%). Most participants wore facial masks for less than 4 h per day (53.8%). As to the type of mask, 644 participants (52.3%) wore fabric masks, whereas 552 (44.8%) wore surgical masks. Only 35 participants (2.8%) were using N95 respirators during the pandemic.
In all, 767 participants (62.3%) complained of 1,594 adverse skin events following mask usage. The flare‐up of acne accounted for the highest proportion of reports (32.2%), followed by pruritus (22.1%) and greasy skin (14.7%). The remaining skin reactions included erythematous rash (12.7%), pain on mask border (9.3%), dry skin (4.7%), worsening of pre‐existing dermatoses (3.6%) and abrasion (0.6%).
Comparing the adverse skin reaction between different types of masks (Fig. 1), the incidence of adverse skin reactions from surgical mask usage was higher than that for fabric masks for every type of adverse skin reaction, with statistically significant differences for acne, pruritus and greasy skin. Most surgical masks are typically composed of 3–4 layers of the fabric, supplemented by two filter sheets. 4 In comparison, cloth masks are made from various textiles, such as cotton, polyester or silk fabric. 5 The greater number of layers in surgical masks might produce a more pronounced occlusion effect than cloth masks.
Figure 1.
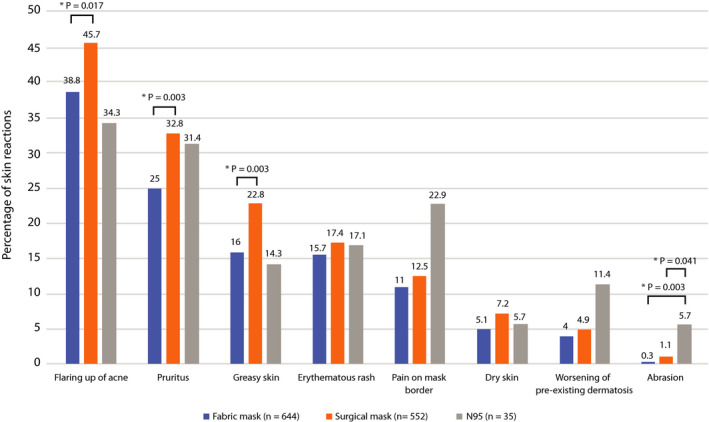
Percentage of skin reactions from fabric, surgical and N95 masks.
Of the three mask types, N95 respirator usage in general population demonstrated the highest incidence for only three skin reaction types: abrasion, pain at mask borders and a worsening of pre‐existing dermatoses. The incidence of common adverse skin reactions arising from N95 respirator usage, such as acne, was lower than for the two other types of mask. However, our participants were non‐medical personnel, and they might not have known the proper wearing method for N95 respirator. Their respirators might not have fitted tightly against their faces. Hence, the rate of adverse skin reactions from N95 respirator usage in this study was also lower than those previously reported for healthcare workers. 6 , 7
The factors associated with the adverse skin reactions were analysed (Table 1). Being female, an age below 40 years, having oily skin, having acne before starting to wear masks and long durations of mask usage (>4 h daily) were significantly associated with skin reactions. Interestingly, mask reuse did not increase the risk of skin reactions, whereas reuse with cleaning seemed to lower the risk. If mask reuse is unavoidable, prior cleaning should alleviate the risk of skin reactions.
Table 1.
Factors associated with skin reactions in mask wearers during the COVID‐19 pandemic
| Skin reactions (n = 767) | No skin reactions (n = 464) | Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|---|---|
| N (%) | N (%) | Crude OR (95% CI) | P‐value | Adjusted OR (95% CI) | P‐value | |
| Sex | ||||||
| F | 591 (65.1) | 317 (34.9) | 1.56 (1.20–2.02) | 0.001 | 1.67 (1.25–2.23) | 0.001 |
| M | 176 (54.5) | 147 (45.5) | Reference | — | Reference | — |
| Age (year) | ||||||
| 18–30 | 266 (77.3) | 78 (22.7) | 4.18 (3.05–5.73) | <0.001 | 2.53 (1.78–3.60) | <0.001 |
| 31–40 | 302 (68.0) | 142 (32.0) | 2.61 (1.98–3.43) | <0.001 | 1.93 (1.43–2.59) | <0.001 |
| > 40 | 199 (44.9) | 244 (55.1) | Reference | — | Reference | — |
| Education | ||||||
| Below undergraduate | 56 (58.9) | 39 (41.1) | 0.84 (0.55–1.29) | 0.428 | NA | NA |
| Undergraduate and above | 711 (62.6) | 425 (37.4) | Reference | — | Reference | — |
| Skin type | ||||||
| Dry skin | 162 (59.3) | 111 (40.7) | 1.47 (1.08–2.01) | 0.014 | 1.31 (0.94–1.83) | 0.117 |
| Normal skin | 199 (49.8) | 201 (50.2) | Reference | — | Reference | — |
| Oily skin | 406 (72.8) | 464 (27.2) | 2.70 (2.06–3.54) | <0.001 | 1.80 (1.33–2.44) | <0.001 |
| Degree of acne before starting to wear masks | ||||||
| No acne | 210 (44.8) | 259 (55.2) | Reference | — | Reference | |
| Mild acne | 495 (72.1) | 192 (27.9) | 3.18 (2.48–4.07) | <0.001 | 2.08 (1.57–2.76) | <0.001 |
| Moderate acne | 56 (82.4) | 12 (17.6) | 5.76 (3.01–11.02) | <0.001 | 2.82 (1.40–5.68) | 0.004 |
| Severe acne | 6 (85.7) | 1 (14.3) | 7.4 (0.88–61.95) | 0.065 | 2.14 (0.25–18.75) | 0.491 |
| Time wearing mask per day (h) | ||||||
| 0–4 h | 357 (53.9) | 305 (46.1) | Reference | — | Reference | — |
| 4–8 h | 316 (70.5) | 132 (29.5) | 2.05 (1.59–2.64) | <0.001 | 1.83 (1.38–2.39) | <0.001 |
| > 8 h | 94 (77.7) | 27 (22.3) | 2.97 (1.88–4.69) | <0.001 | 2.44 (1.51–3.95) | <0.001 |
| Disposing of mask every day | 218 (70.6) | 91 (29.4) | Reference | — | Reference | — |
| Reusing mask | 549 (59.5) | 373 (40.5) | — | — | — | — |
| Reusing with cleaning | 445 (58.4) | 317 (41.6) | 0.59 (0.44–0.78) | <0.001 | 0.69 (0.51–0.94) | 0.020 |
| Reusing without cleaning | 104 (65.0) | 56 (35.0) | 0.78 (0.52–1.16) | 0.220 | 0.85 (0.54–1.33) | 0.471 |
Significant P values (<0.05) are in Bold.
In conclusion, this study revealed and compared the incidences of adverse skin reactions arising from the usage of three types of masks in daily life. Our data indicated that acne flare‐up was the most common reaction and that fabric, or cloth, masks had the lowest rates of skin reactions. About one‐third of the respondents reported being comfortable with wearing masks.
Conflicts of interest
All authors do not have any conflicts of interest or financial support to declare.
Funding source
None.
References
- 1. Taylor M. Thailand scores highest for mask‐wearing in survey of ASEAN nations. https://thethaiger.com/coronavirus/thailand‐scores‐highest‐for‐mask‐wearing‐in‐survey‐of‐asean‐nations (last accessed: 20 June 2020).
- 2. Szepietowski JC, Matusiak Ł, Szepietowska M, Krajewski PK, Białynicki‐Birula R. Face mask‐induced itch: a self‐questionnaire study of 2,315 responders during the COVID‐19 pandemic. Acta Derm Venereol 2020; 100: adv00152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Veraldi S, Angileri L, Barbareschi M. Seborrheic dermatitis and anti‐COVID‐19 masks. J Cosmet Dermatol 2020. 10.1111/jocd.13669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chellamani KP, Veerasubramanian D, Vignesh Balaji RS. Surgical face masks: manufacturing methods and classification. J Acad Indus Res 2013; 2: 320–324. [Google Scholar]
- 5. Zhao M, Liao L, Xiao W et al. Household materials selection for homemade cloth face coverings and their filtration efficiency enhancement with triboelectric charging. Nano Lett 2020; 20: 5544–5552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Foo CC, Goon AT, Leow YH, Goh CL. Adverse skin reactions to personal protective equipment against severe acute respiratory syndrome–a descriptive study in Singapore. Contact Dermatitis 2006; 55: 291–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lan J, Song Z, Miao X et al. Skin damage among health care workers managing coronavirus disease‐2019. J Am Acad Dermatol 2020; 82: 1215–1216. [DOI] [PMC free article] [PubMed] [Google Scholar]


