Abstract
SARS‐CoV‐2 is the virus causing COVID‐19 and is spread through close person‐to‐person contact. The use of face masks has been described as an important strategy to slow its transmission. We evaluated the effects of coaching caregivers via telehealth technologies to teach face mask wearing to children with autism spectrum disorder. Six participants with a history of challenging behavior associated with mask wearing were recruited from different parts of the world, and trained using graduated exposure, shaping, and contingent reinforcement. By the end of the intervention, all participants wore a face mask for a period of 10 min without exhibiting challenging behavior. The skills generalized to a novel mask or a community setting. Mask wearing did not affect the percentage of oxyhemoglobin saturation of participants, and caregivers found the intervention useful. The findings support previous tolerance training treatment evaluations in children with developmental disorders exhibiting resistance to healthcare routines.
Keywords: ASD, COVID‐19, global dissemination, masks, telehealth
As of November 2020, more than 48 million cases of COVID‐19 have been diagnosed worldwide, and more than 1.2 million people have died from complications of the disease. The disease affects the lungs, heart, kidneys, gut, and brain, but the respiratory symptoms (pneumonia) induced by an inflammatory cytokine response have proved to be life‐threatening (Lake, 2020; Wang et al., 2020). While most individuals infected with SARS‐CoV‐2 present with mild or no symptoms, COVID‐19 complications can be lethal among individuals with preexisting medical conditions and the elderly (Shahid et al., 2020; Zhou et al., 2020). Mitigating actions to reduce the rate of infection have included emergency lockdowns, travel restrictions (Ji et al., 2020), and behavioral recommendations such as thorough and frequent hand‐washing, social distancing, and avoiding hand‐to‐face contact (Güner et al., 2020). Ongoing research studies offer support for the effectiveness of nonpharmacological strategies to slow the spread of the disease (e.g., social distancing, Ghanbari et al., 2020; hand‐washing, Pogrebna & Kharlamov, 2020). In addition, the use of face masks has been suggested as an important risk mitigation strategy against virus transmission (Cheng et al., 2020; Esposito & Principi, 2020). Mask wearing can prevent onward respiratory droplet transmission from an infected person (e.g., surgical masks; see MacIntyre & Chughtai, 2020, for a review) and filter airborne particles, offering protection to an uninfected person (e.g., N95/FFP2 masks; Bartozko et al., 2020).
Most countries that have eased home confinement and domestic travel restrictions have advised their citizens to wear a face mask when in public to prevent future outbreaks. For example, in Belgium and the United Kingdom, a face mask is mandatory on public transport and in all shopping areas for all individuals over 12 years of age. A face mask is also recommended in crowded situations when social distancing is not possible. In population‐dense countries like India, wearing a mask is required at all times in all public spaces. There is evidence to suggest that wearing a surgical or a reusable cotton face mask can protect against SARS‐CoV‐2 infection in public and health care settings (Chu et al., 2020).
Due to their abnormal immune response, children with autism spectrum disorder (ASD) may be a population vulnerable to COVID‐19 (Lima et al., 2020). Moreover, individuals with ASD may lack the instructional control to adhere to hand washing, refrain from face touching, and, particularly, wear a face mask. It is possible that the discomfort caused by wearing a mask may evoke escape‐maintained refusal among children with ASD. Previous research indicates that individuals with ASD exhibit reactions to various types of tactile stimuli, and their adaptation to novel tactile stimuli may be delayed or altered (Kohn, 2007; Puts et al., 2014). Abnormal behavioral reactions (e.g., aggression) to stimuli such as tags on clothing and food textures have been commonly reported (Marco et al., 2012). Escape‐maintained refusal of wearable items has also been described for earplugs (Cox et al., 2017) and prescription glasses (DeLeon et al., 2008) in this population (see also Piazza et al., 2003).
Behavioral strategies such as graduated exposure (stimulus fading), contingent positive reinforcement, and response prompting have previously been tested for their efficacy in improving compliance with healthcare routines. For example, Buckley et al. (2020) used graduated exposure and positive reinforcement to teach two adolescent males with autism to tolerate a haircut. The exposure hierarchy involved gradually increasing proximity to the haircutting equipment and then increased contact duration with the equipment. Following the intervention, both boys tolerated hair clipping for a mean duration of 15 min. Graduated exposure also has been evaluated in this population in combination with response prompting for toothbrushing (Bishop et al., 2013), increasing food repertoire (Tanner & Andreone, 2015), and undergoing a neuroimaging scan (Cox et al., 2017). In addition to graduated exposure, participants in these studies also received brief breaks contingent on the omission of escape‐maintained problem behavior or differential reinforcement of other behavior. Moreover, Cook et al. (2015) evaluated differential negative reinforcement of other behavior (DNRO) to increase compliance with wearing a medical bracelet in a boy with autism. The authors reinforced progressively longer periods of bracelet wearing with the contingent removal of the bracelet. Bracelet wearing increased steadily to a target duration of 7 daily hours.
DeLeon et al. (2008) evaluated the effects of noncontingent reinforcement (NCR) on the use of prescription glasses in four individuals with intellectual disability. Their study showed NCR alone to be effective for one participant, whereas the other three required response blocking and response cost to establish compliance. Similarly, Richling et al. (2011) evaluated the effectiveness of NCR in increasing compliance with wearing foot orthotics in two individuals with a developmental disability. The authors reported that receiving preferred items on a fixed‐time schedule increased the duration of orthotics wearing relative to baseline.
The current context of the COVID‐19 pandemic poses severe restrictions to face‐to‐face interventions in many world regions. Therefore, telehealth delivery would add social validity to a mask wearing intervention (Degli Espinosa et al., 2020). An emerging literature has demonstrated the feasibility and effectiveness of training caregivers via telehealth to implement interventions for children with autism, including interventions to reduce challenging behavior (Wacker et al., 2013), increase communication (Barkaia et al., 2017), and improve joint attention (Neely et al., 2016) and imitation (Wainer & Ingersoll, 2015). In addition, telehealth has the potential to expand behavioral services to geographically and culturally diverse clients (e.g., Barkaia et al., 2017; Tsami et al., 2019).
The purpose of the current study was to evaluate the effectiveness of coaching caregivers via telehealth to implement graduated exposure and shaping to teach mask‐wearing to children with ASD.
Method
Participants, Setting and Cultural Adaptations
Six consecutively admitted children with ASD and their families and/or therapists were recruited from four countries (Belgium, India, Mexico, Costa Rica). Recruitment was supported by social media groups in Belgium, Spain, and India using information that was translated into the relevant languages. Inclusion criteria consisted of: a clinical diagnosis of ASD conducted by a medical professional or psychologist, being between 2 and 12 years of age, and having a history of problem behavior associated with mask wearing (e.g., mask refusal, property destruction, aggression). Table 1 presents a summary of participant sociodemographic information.
Table 1.
Participant Sociodemographic Information
| Gender (age) | Technician (age) | Country | Ethnicity | Autism severity | |||
|---|---|---|---|---|---|---|---|
| ADOS | CARS | DSM | |||||
| Thomas | Male (8) |
Mother (38) |
Belgium | Mixed |
17 (1.62) |
||
| Abhi | Male (6) |
Mother (36) |
India | Indian |
35 (30‐37) |
||
| Juan | Male (7.5) | Therapist (25) | Mexico | Hispanic |
14 (1.06) |
||
| Maria | Female (6.5) |
Mother (33) |
Costa Rica | Hispanic |
2 (1‐3) |
||
| Selva | Male (7) |
Mother (34) |
India | Indian |
33 (30‐37) |
||
| Mateo | Male (6) | Therapist (40) | Mexico | Hispanic |
15 (1.24) |
||
Note. ADOS = Autism Diagnostic Observation Schedule, 2nd ed. (ADOS social affect score followed by the number of standard deviations above the score of neurotypical reference population; normative data by Gotham et al., 2009); CARS = Childhood Autism Rating Scale (mild to moderate autism score range in parenthesis; see Shopler et al., 2010); DSM = Level of support required (range, 1 to 3), Diagnostic and Statistical Manual of Mental Disorders. All ages in years.
Thomas was an 8‐year‐old boy from Belgium. His parents were originally from Russia and France. The family spoke French and English at home. Thomas had a score of 17 on the Autism Diagnostic Observation Scale, Second Edition (ADOS‐2; Lord & Rutter, 2012), which was administered 6 months before the study. He spoke in short sentences in both English and French, used nouns (e.g., “flower”), actions (e.g., “crying”), and adjectives (e.g., “wet”) when shown pictures, and followed simple instructions (e.g., “get your cap”). He did not engage in a conversation, make unprompted comments about events, or ask questions. Abhi was a 6‐year‐old boy from India. His family spoke English and Tamil at home. His score on the Childhood Autism Rating Scale (CARS; Schopler et al., 1980) was 35, based on administration 2 years before the study. Abhi spoke using single words, asked for approximately 10 different items, and receptively identified approximately 50 items (e.g., “find the bag” from a series of 4‐6 pictures). He emitted no spontaneous labels and did not answer questions. Juan was a 7.5‐year‐old boy from Mexico. He wore prescription glasses and participated in the study with his therapist. His score on the ADOS, administered 1 year before the study, was 15. Juan spoke in simple phrases (e.g., he could say, “give me big train”), responded to instructions (e.g., “find all the vehicles in the picture”), and asked and answered questions. He did not engage in conversations on a topic, narrate, or describe events. Maria was a 6.5‐year‐old girl from Costa Rica. She required “substantial support” as per the DSM level of support scale, completed 1 year before the study. She requested items using single words (e.g., “ball”), labeled items upon request (e.g., when asked “what is this?” while holding up a ball), and engaged in identity match‐to‐sample with objects and pictures. She did not answer questions, identify colors or shapes (either as a listener or as a speaker), or match nonidentical pictures (e.g., matching animals with their young ones, or matching items belonging to the same category). Selva was a 7‐year‐old boy from India. He spoke English and Tamil at home. His score on the CARS was 33. Selva, primarily communicated using gestures, followed basic instructions delivered with accompanying gestures (e.g., “sit down here” while pointing to the chair), and performed identity match‐to‐sample tasks. He did not engage in any vocal verbal behavior besides simple echoics (e.g., repeating monosyllabic sounds following a model). Mateo was a 6‐year‐old‐boy from Mexico. His score on the ADOS, which was administered 1 year before the study, was 14. He made requests using short phrases, followed simple, context‐relevant instructions (e.g., bring the crayons, let us do some art), and tacted simple and complex objects and activities when presented with pictures (e.g., “eating a banana”). He did not answer questions or label items or events spontaneously.
All participants had a reported history of challenging behavior when asked to wear a mask prior to the study. The experimenter (first author) trained the mothers of Thomas, Abhi, Maria, and Selva and the therapists of Juan and Mateo (both psychologists pursuing ABA training) to provide the intervention. The experimenter was a masters' level behavior analyst with 7 years of direct experience in behavioral interventions with children with ASD, and 3 years of experience providing telehealth interventions for children with ASD and their families. The experimenter could speak in English and Tamil with the participants. All participating parents and therapists, hereinafter, the caregiver, had past experience implementing behavior‐analytic procedures.
Sessions were conducted via telehealth with the experimenter present in her home or office, and the participants present in their respective homes or therapy centers. Caregivers conducted sessions in the living room (Thomas, Selva, and Maria), bedroom (Abhi), child's therapy classroom (Juan and Mateo), home balcony (Thomas), garage (Juan, Maria, Selva, and Mateo) and terrace (Abhi).
Materials
The experimenter used a video‐calling platform on her laptop to conduct the sessions. The participants' families had access to either a smartphone device or a laptop for the sessions. In addition, participants were provided with face masks (10 surgical masks and three cloth masks) and a finger‐tip pulse oximeter for the study. The surgical masks were identical, while cloth masks varied in their color and texture. The masks used in the study were consistent with the recommendations of Esposito and Principi (2020) for the pediatric population. Surgical masks were approximately 16 cm by 8 cm, cloth masks were approximately 12 cm by 6 cm, and masks were attached to the participant's head by ear loops on the sides. Masks had a good fit with participants' faces and no modifications were required. The cotton mask was washed in hot water (approximately 60°C based on the recommendations of the World Health Organization; WHO, 2020) after each appointment and surgical masks were discarded after two appointments. Fingertip pulse oximeters monitored participant oxygen saturation throughout the sessions. Pulse oximeter manufacturers varied across participants depending on what was available at each location.
Response Measurement and Interobserver Agreement
Data were collected on the number of graduated exposure steps completed and the duration of mask wearing in seconds per session. Table 2 displays the graduated exposure steps. When worn correctly, a face mask covers the nose and mouth, and therefore is in contact with the entire bottom half of the face (Esposito & Principi, 2020). Thus, mask wearing was defined as the participant having the face mask loops fit around their ears such that the top of the mask was in contact with the bridge of the nose, the nostrils and mouth were entirely covered, and the lower edge of the mask fully covered the mental protuberance. Abhi and Maria's caregivers reported that they had a history of escape‐maintained problem behaviors and therefore, it was determined prior to treatment, that the exposure hierarchy for these two participants would include an additional step (Step #12’).
Table 2.
Exposure Hierarchy
| Step # | Description |
|---|---|
| 1 | Face mask within 30 cm for 5 s |
| 2 | Face mask within 15 cm for 5 s |
| 3 | Touches the loops of the face mask |
| 4 | Holds mask by loops |
| 5 | Attaches one loop to the ear |
| 6 | Fits second ear loop by pulling the mask with one or both hands |
| 7 | Pulls and pushes top edge of the mask for a tight nose bridge adjustment |
| 8 | Wears mask on face for at least 3 s |
| 9 | Wears mask on face for at least 5 s |
| 10 | Wears mask on face for at least 10 s |
| 11 | Wears mask on face for at least 30 s |
| 12 | Wears mask on face for at least 60 s |
| 12’ | Wears mask for at least 150 s |
| 13 | Wears mask on face for at least 5 min |
| 14 | Wears face mask for at least 10 min |
| 15 | Removes face mask using loops |
Note. Step 7 allows for caregiver physical prompts. Abhi and Maria were the only participants completing Step 12’, and the only ones skipping Step 5 and 6.
Each step in the hierarchy was scored as correct if the participant completed the step independently without the occurrence of problem behavior. Problem behaviors reportedly associated with mask wearing included (a) throwing the mask (Thomas, Maria), (b) shouting above conversational level and/or crying with or without tears (Thomas, Abhi, Selva), (c) removing or attempting to remove the mask (all participants), (d) using hands to push against or pull away from the care provider implementing the intervention (Maria, Mateo), and (e) wearing the mask over the prescription glasses and blowing through it with or without fogging up the glasses (Juan). Data were collected on the frequency of problem behavior. A new instance of shouting/crying and glass blowing was recorded every time these behaviors occurred for more than 3 consecutive seconds.
We measured the percentage of oxygen‐saturated hemoglobin in the blood (SpO2) using a fingertip pulse oximeter as a precautionary measure to detect hypoxia. We completed three consecutive readings separated by a 3‐s interval at the end of each session and reported the mean SpO2 as a percentage. To minimize potential artifacts, participants sat still during readings with their arm approximately at heart level. The same finger was used consistently to obtain the SpO2 value. The complete measuring routine was repeated in the event of a reading below 90% SpO2. If the low saturation value was not replicated, the outlier reading was removed (Buekers et al., 2019). Over‐the‐counter fingertip class pulse oximeters are known to have a ± 2% SpO2 accuracy when a gas exchange oximeter is used as reference for comparison (American Thoracic Society, 2018).
The social acceptability of the training procedure was measured after the training by asking the parent or therapist to complete a modified version of the Treatment Acceptability Rating Form‐Revised (TARF‐R; Reimers & Wacker, 1992; Wacker et al., 1998). The modified form contained six items scored on a 5‐point Likert‐type scale from 1 (strongly disagree) to 5 (strongly agree). Questions covered training acceptability, the perceived usefulness of the training, ease of procedural implementation, and overall satisfaction.
All behavioral outcomes were scored retrospectively from videos recorded during the sessions. The first author recorded the complete collection of session videos for all participants, and a second observer independently scored at least 40% of sessions in each condition for each participant. An agreement for each completed step in the hierarchy was scored if both observers recorded the step. We divided the total number of agreements by the total number of agreements plus disagreements and transformed this ratio into a percentage. Mask wearing episodes within each session were divided into 10‐s intervals. For each interval, we divided the shorter duration per interval by the longer duration per interval and computed the mean duration interobserver agreement across all 10‐s intervals for each participant. Finally, we obtained interobserver agreement of problem behavior by dividing the session into consecutive 10‐s intervals and comparing the observers' frequency recordings on an interval‐by‐interval basis. The smaller number of responses in each interval was divided by the larger number of responses; these fractions were averaged across all intervals and reported as a percentage.
Interobserver agreement (IOA) across all participants was 100% for steps in the hierarchy. For Thomas, IOA was 94% (range, 91% to 99%) for duration of mask wearing and 96% (range, 93% to 100%) for problem behavior. For Abhi, IOA was 96% (range, 93% to 100%) for mask wearing and 95% (range, 92% to 99%) for problem behavior. For Juan, IOA was 96% (range, 95% to 100%) for mask wearing and 98% (range, 93% to 100%) for problem behavior. For Maria, IOA was 95% (range, 92% to 99%) for mask wearing, and 93% (range, 90% to 100%) for problem behavior. For Selva, IOA was 97% (range, 95% to 100%) for mask wearing and 100% for problem behavior. For Mateo, IOA was 93% (range, 91% to 99%) for mask wearing and 100% for problem behavior.
Observers also collected data on the caregivers' adherence to the coaching procedures during each session. Treatment integrity was calculated as a percentage of the number of the following steps implemented correctly, with or without an experimenter prompt: present instruction and mask, provide prompts if required, deliver verbal praise and preferred item/initiate preferred activity, and terminate session if problem behavior occurs or if mastery criterion is met. Treatment integrity averaged across sessions was 100% for five of the six caregivers, and 96.8% (range, 75% to 100%) for Abhi's mother. IOA for treatment integrity was collected for at least 40% of sessions in each condition, and averaged 99% (range, 75% to 100%) across all six participants.
Procedure
We used a nonconcurrent multiple‐baseline design across six participants to evaluate the effects of our telehealth intervention. During all sessions, the experimenter interacted with the child's caregiver (i.e., trainer) in English. The caregiver interacted with the child in Spanish (Juan, Maria, and Mateo), English (Thomas, and Abhi), and Tamil (Selva). All caregivers sanitized their hands with alcoholic disinfectant prior to the start of each session. Caregivers conducted each session with live coaching from the experimenter. Coaching included providing instructions (e.g., “Now you can take a new pulse oximeter reading”), prompting (e.g., “Please, help Maria fitting the left loop”), and intermittent behavior‐specific praise (e.g., “Good job! you praised the child for wearing the mask”). The experimenter signaled to the caregiver the start (i.e., “please, start now”) and end (i.e., “stop!”) of all baseline, treatment, and generalization sessions. Prior to each session, the experimenter listed the teaching steps to be carried out during that session, and had the caregiver vocally repeat the sequence. The caregivers also had a written version of the steps next to them during each session. The experimenter prompted the caregivers as needed, throughout the study. If the caregiver paused or erred (e.g., the caregiver did not provide access to the preferred item after the successful completion of a step), the experimenter provided vocal instructions immediately (e.g., “please provide access to the musical drum now”). The experimenter provided feedback to the caregiver intermittently during the session and after terminating the session.
Intake Appointment
The researcher completed one intake appointment session with each caregiver prior to the commencement of the study. During the appointment, the experimenter obtained information related to the ASD diagnosis and verbal behavior repertoire of each child. The experimenter and caregiver also identified topographies of problem behavior that occurred when the child was asked to wear a mask (either by observation during the appointment or caregiver report) and developed preliminary operational definitions of these behaviors. The experimenter provided a general overview of the study and the procedures that would be used during the training phase and the caregiver chose a mask (i.e., surgical or cloth) to be used during the training. The caregivers were provided with written instructions for each phase of the study and were instructed to keep these with them during the sessions.
Baseline
The caregiver stated the instruction, “It is time to wear a mask” and presented a mask at a 30 cm distance from the child. If the participant displayed problem behavior, the caregiver removed the mask and terminated the session. Problem behaviors were not followed by verbal responses or prompts of any kind. If the participant completed the first four steps of the hierarchy, the caregiver provided a verbal prompt (i.e., “Put the loops over the ear” while pointing to the loops and the child's ears). Two participants reached Step 4 and both put away the mask immediately. If the participant completed Steps 1 through 7 of the hierarchy, the caregiver stated the instruction, “Now we are going to do [activity name] while wearing the mask,” and then initiated the activity. However, none of the participants reached Step 7 of the graduated exposure hierarchy during baseline. We terminated a baseline session when more than 5 s elapsed without the participant completing a new step of the hierarchy.
Treatment
Treatment sessions started with a multiple‐stimulus preference assessment without replacement (MSWO) with a three‐stimulus array that had been previously identified by the caregiver (DeLeon & Iwata, 1996). During the first two treatment sessions, the caregiver started by stating “it is time to wear a mask” and then modeled mask wearing by presenting smartphone images of anecdotally‐identified favorite children and familiar adults wearing masks. The caregiver then stated that the purpose of wearing a mask was to keep others from getting sick. The caregiver also modeled mask wearing by fitting a mask themselves. We included both in‐vivo and picture prompts because the pictures served as a static model with preferred individuals and the in‐vivo model served as a dynamic model of the steps involved. After the adult had worn the mask for 3 s, they placed a face mask within 30 cm of the child, thereby starting the graduated exposure hierarchy. No particular response other than remaining within the specified distance range and omitting mask‐related problem behaviors was required to complete Steps 1 and 2. The caregiver withdrew all model prompts after the child had successfully completed Steps 1 and 2 twice.
Every time the child completed a new graduated hierarchy step that had not been completed in the preceding sessions, and did so independently and without engaging in problem behavior, the caregiver delivered praise, provided access to a preferred item identified during the preference assessment, and terminated the session. The child was allowed to interact with the preferred item for 30 s to 1 min before the start of the next session. Prompted responses were followed by praise. The same session was implemented again to ensure two successful occurrences of each step of the hierarchy before targeting subsequent steps. Then, the next steps in the graduated exposure hierarchy were targeted. Unprompted jumps ahead within the hierarchy occurred if the participant completed a new step without prompting. For example, if the session targeted holding the mask by the loops, but the participant correctly held the mask and also attached one loop to the ear, this was taken as evidence that the previous steps did not require additional training. The highest step in the hierarchy that was completed was set as the new target and practiced until the participant completed this step twice independently. Such unprompted jumps occurred across steps 4 (hold mask by loops), 5 (attach one loop to ear), and 6 (attach second loop to ear with one/both hands). The session immediately terminated contingent on problem behavior.
For Steps 3, 4, 5, 6, 7 and 14, the caregiver delivered verbal and physical prompts (e.g., saying “put the loop over your ear” and physically guiding the child to insert their fingers around the loop and place it over their ear) if the child did not respond for 3 s after completing the preceding step. The caregiver also provided prompts if the child engaged in the wrong response (e.g., removed the face mask without using the loops). From sessions targeting Step 7 onward, we finished the session by training Step 15 (i.e., mask removal). Before that point, the caregiver removed the mask for the participant. Abhi and Maria required prompts for Steps 5 and 6 until the end of the study. We decided to proceed with training the subsequent steps of the exposure hierarchy for these participants because the caregivers reported fine motor difficulties for both these participants and the primary aim of the intervention was to tolerate wearing a mask. This decision was made after four treatment sessions for both Abhi and Maria at Step 4 of the hierarchy. Once Step 7 was mastered, the participant engaged in a preferred or moderately‐preferred activity (reported anecdotally by the caregiver before each session) while attaining the target mask‐wearing time. Once the participant acquired Step 9, we withdrew end‐of‐session access to a preferred activity. From Step 12 onwards, the participant engaged in a preferred or moderately‐preferred activity in an outdoor setting (e.g., terrace, garage) while accruing mask‐wearing time for the session. We terminated end‐of‐session access to a preferred activity and conducted outdoor sessions to use naturalistic reinforcement contingencies and increase social validity. The outdoor sessions were conducted in the terrace (Thomas, Juan and Mateo), garden (Abhi and Selva), and garage (Maria). Contingent on problem behavior, the caregiver terminated the outdoor session and activity and returned indoors.
If the child did not reach their maximum performance within the hierarchy by one step, we repeated two training sessions at the criterion of their maximum performance. If the child did not reach their maximum performance within the hierarchy by more than one step for two consecutive sessions, we retrained the complete hierarchy from the start. The terminal mastery criterion was defined as wearing a mask continuously for 10 min over two consecutive sessions. We chose 10 min as the terminal criterion in consultation with caregivers in the study based on anecdotal information about the situations in which the children were required to stay outdoor in communal areas.
Generalization
Procedures were identical to those in baseline during two generalization probe sessions using a different type of mask (e.g., surgical mask if the child had used a cotton mask during training). Generalization probes took place in an indoor or outdoor setting, including a garage (Thomas, Abhi, Juan, Mateo), a train journey (Thomas), the street (Mateo), a terrace (Maria), and a basement in their building (Selva). Abhi and Maria required prompts for Steps 5 and 6 during the generalization sessions. The generalization probe was terminated if the terminal criterion was met (i.e., 10 min of continuous mask wearing) or if the child engaged in problem behavior.
Results
Figures 1 and 2 present the results for all participants. During baseline, Thomas (Figure 1, top graph) did not perform beyond Step 3 of the graduated exposure hierarchy and did not exhibit mask wearing. During the treatment phase, the number of steps completed independently increased steadily over the course of 28 sessions. Thomas eventually mastered all 15 steps of the hierarchy. He also wore the mask for the terminal criterion of 10 min at the end of the training phase, and demonstrated independent mask wearing for 10 min during two generalization probes: the first conducted with a novel cotton mask, and the second conducted during a train journey. Thomas demonstrated one instance of shouting during baseline, and one instance of mask removal during the training.
Figure 1.
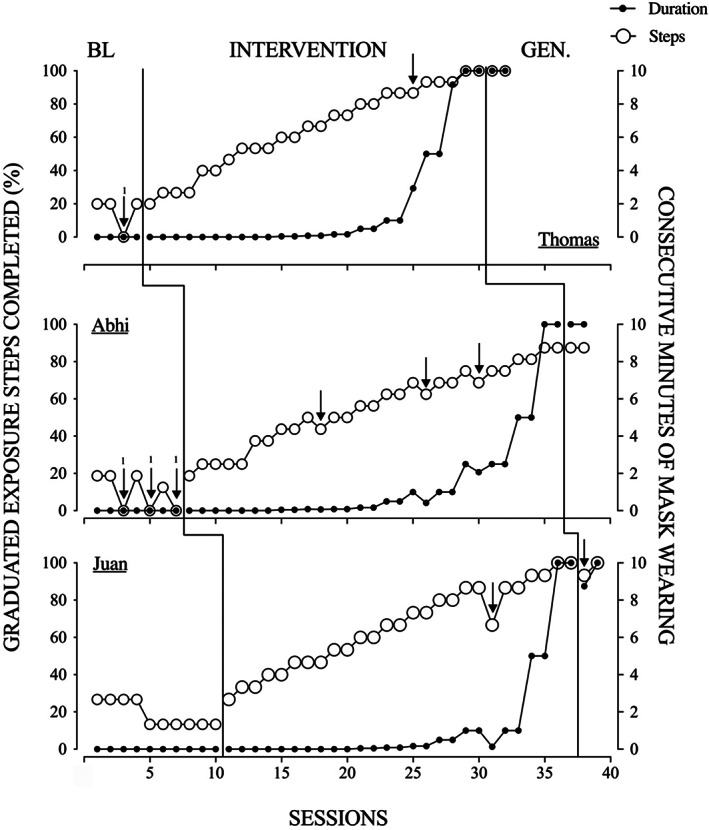
Effects of Graduated Exposure and Shaping on Mask Wearing for Thomas, Abhi, and Juan
Note. Arrows denote sessions with problem behavior (frequency above arrows for baseline sessions). Intervention sessions were terminated upon the first occurrence of problem behavior.
Figure 2.
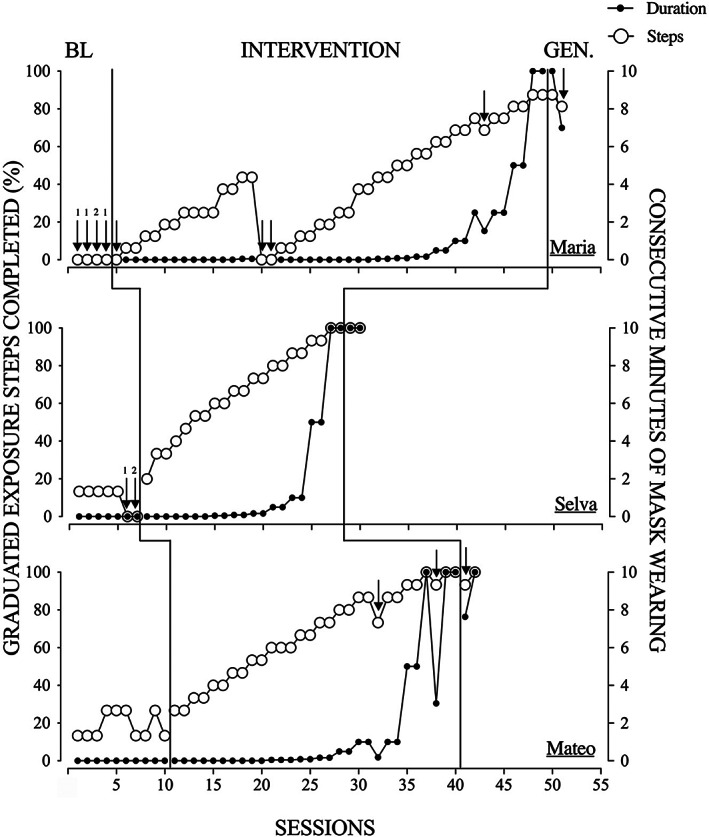
Effects of Graduated Exposure and Shaping on Mask Wearing for Maria, Selva, and Mateo
Note. Arrows denote sessions with problem behavior (frequency above arrows for baseline sessions). Intervention sessions were terminated upon the first occurrence of problem behavior.
Abhi's (Figure 1, center graph) performance during baseline ranged from zero to Step 3. Over the course of 31 intervention sessions, he mastered 14 of the total 16 steps (including step #12’) in the hierarchy, and tolerated mask wearing for the target 10 min. Abhi experienced motor difficulties when fitting the mask loops around his ears. His mother fully prompted Steps 5 and 6 and proceeded with training the subsequent steps in the exposure hierarchy. He continued to require parental support (physical prompting) for fitting and removing the loops of the mask until the end of the study. Abhi completed two generalization probes with new masks (i.e., novel cloth mask, and a surgical mask). He reached the targeted 10 min of mask wearing during both probes. Abhi demonstrated a total of six instances of problem behavior throughout the study. These included three instances of crying during baseline, and one instance of crying and two instances of mask removal during training.
Juan (Figure 1, bottom graph) completed two to four steps of the hierarchy during baseline and never wore the mask. He required 29 intervention sessions to achieve the terminal mask wearing criterion of 10 min and completed all 15 steps in the exposure hierarchy independently. He demonstrated mask wearing for 10 min during one of the two generalization probes each conducted with a novel cotton mask. Juan engaged in two occurrences of problem behavior during training: one instance of wearing the mask over his glasses, and one instance of mask removal.
Maria (Figure 2, top graph) did not complete any step in the exposure hierarchy during baseline. She either picked up the mask and threw it or pushed it away once it was presented. During the course of 47 intervention sessions, Maria mastered 14 of the 16 total steps (including step #12’) of the exposure hierarchy. She required parental support (physical prompting) for Steps 6 and 7 throughout the study. She wore the mask for 10 min by the end of the training. She required adult support for attaching the loops and adjusting the front of the mask. She completed two generalization probes conducted with a novel mask, and wore the cotton mask for 10 min and the surgical mask for 7 min. Maria demonstrated nine instances of problem behavior, including four instances of mask throwing during baseline. She demonstrated five instances of problem behavior during the training phase, including two instances each of throwing and pushing, and one instance of mask removal.
Selva (Figure 2, center graph) completed between zero to two hierarchy steps during baseline and did not demonstrate mask wearing. He required 23 intervention sessions to acquire all 15 steps in the exposure hierarchy and achieved the terminal mask wearing criterion of 10 min. He also wore the mask for 10 min during both generalization probes conducted with novel cotton and surgical masks. Selva engaged in two instances of shouting during baseline. He did not engage in problem behavior during training.
Mateo (Figure 2, bottom panel) completed between 2 to 4 steps of the exposure hierarchy during baseline, but did not wear the mask. Over the course of 32 intervention sessions, he mastered all 15 steps in the exposure hierarchy and wore the mask for 10 min. He achieved the terminal mask‐wearing criterion during one of the two generalization probes conducted with a surgical mask, and wore the mask for 7.5 min before removing it during the second generalization probe, which was conducted in the community. Mateo did not engage in problem behavior during baseline, but showed three instances of problem behavior during the training phase, including one instance of pushing, and two instances of mask removal.
Table 3 presents the oxygen saturation values for all participants throughout the study. These data show no evidence of low oxygen saturation due to mask wearing for any of the participants. Table 4 presents the total duration of the evaluation, average session duration and average number of sessions conducted per appointment for each participant. The evaluation (baseline and training) was completed in a mean of 68 min per participant, excluding the caregiver coaching conducted prior to each session and feedback provided after the session. The social validity data are shown in Table 5. These data indicate that all caregivers found the training highly acceptable and were satisfied with the results.
Table 3.
Oxygen Saturation Percentage Recorded during Baseline and Training Sessions
| Oxygen saturation | ||
|---|---|---|
| Baseline | Training | |
| Thomas | 98% (96% ‐ 100%) | 96% (92% ‐ 100%) |
| Abhi | 96% (93% ‐ 99%) | 98% (96% ‐ 99%) |
| Juan | 99% (98% ‐ 100%) | 100% (97% ‐ 100%) |
| Maria | 98% (94% ‐ 100%) | 95% (93% ‐ 100%) |
| Selva | 97% (95% ‐ 99%) | 98% (95% ‐ 100%) |
| Mateo | 98% (96% ‐ 100%) | 97% (96% ‐ 100%) |
Note. The mean and range are included (minimum – maximum).
Table 4.
Session Durations, Number of Sessions per Appointment, and Total Evaluation Time
| Mean and range session duration (min) | Mean and range sessions conducted per appointment | Total evaluation time (min) | |
|---|---|---|---|
| Thomas | 2.2 (0.08 – 10.2) | 5 (4 – 7) | 72 |
| Abhi | 1.9 (0.08 – 10.2) | 5 (2 – 6) | 74 |
| Juan | 1.6 (0.1 – 10.2) | 5 (3 – 7) | 61 |
| Maria | 1.3 (0.03 – 10.2) | 6 (4 – 8) | 68 |
| Selva | 1.9 (0.1 – 10.3) | 6 (4 – 7) | 58 |
| Mateo | 1.8 (0.1 – 10.2) | 5 (3 – 6) | 76 |
Note. The mean and range are included (minimum – maximum).
Table 5.
Participant Responses on the Social Validity Questionnaire
| Items | Mean (SD) |
|---|---|
| I found this training to be an acceptable way to acquire the skills necessary to teach my child to wear a mask | 4.8 (0.4) |
| I believe that my child did not have any adverse reaction to the training | 4.7 (0.5) |
| I liked the training. | 4.8 (0.4) |
| I found it easy to implement the procedures. | 4.3 (0.8) |
| I believe it would be acceptable to use this training with caregivers who intend to teach their children to tolerate wearing a mask. | 5 (0.0) |
| I believe that the training is likely to result in my child generalizing the skills acquired. | 4.7 (0.5) |
| Overall, I had a positive reaction to this training. | 4.8 (0.4) |
| I am satisfied with the results obtained with my child during the training | 4.8 (0.4) |
Note. All items were scored on a Likert‐type scale ranging from 1 (strongly disagree) to 5 (strongly agree). In all therapist forms, the words “my child's” were replaced with “my student's”.
Discussion
The present study aimed to evaluate the effectiveness of telehealth services for delivering graduated exposure and shaping to establish mask‐wearing in children with ASD. Caregivers conducted the training with high integrity with coaching from the experimenter, and all six participants tolerated wearing a mask for the target duration of 10 min. All participants wore either a novel mask or the trained mask in a community setting at the conclusion of the training. An oximetry analysis indicated that mask wearing did not affect oxygen saturation levels in our participants. Finally, caregivers found the training useful and practical.
Mask wearing increased across sessions even though the caregiver terminated the sessions contingent on problem behavior. Thus, caregivers did not have to implement extinction and other potentially restrictive procedures. These results are consistent with studies with individuals with disabilities that targeted compliance with healthcare routines such as wearing eye glasses (DeLeon et al., 2008), tolerating a haircut (Buckley et al., 2020) and undergoing a neuroimaging scan (Cox et al., 2017). Further, we obtained similar outcomes across culturally diverse participants regardless of whether the caregiver conducted sessions in English, Spanish, or Tamil. Although no direct internet connectivity data were collected, none of the caregivers experienced technical difficulties when conducting sessions, with the exception of one appointment with Maria's caregiver that was terminated due to network problems.
Increased durations of mask wearing were programmed gradually, and the specific periods by which target durations increased were individualized. For example, according to the caregivers' reports, Abhi and Maria had a history of escape‐maintained problem behavior and had difficulty with fine motor activities such as opening zippers and buttons. Therefore, target duration increments were more gradual for them to keep the procedure as minimally demanding as practically possible. However, the design of the study did not allow us to evaluate whether this gradual increase was indeed necessary. In addition, both Abhi and Maria required caregiver support throughout the study for fitting the mask loops. It is possible that additional training sessions specifically targeting the steps in the exposure hierarchy that required full physical prompts might have led to better outcomes for these participants. In addition, it must be noted that we did not provide physical prompts when the participants did not put on the mask during baseline. Therefore, the possibility exists that the participants did have mask‐wearing skills during baseline in spite of caregiver report. Future studies may consider physically prompting the child through all of the mask‐placement steps in baseline and only provide escape contingent on problem behavior or mask removal. However, such a rigorous approach may evoke problem behavior and compromise the caregiver's adherence to the procedure.
Given the under‐representation of culturally diverse participants in the behavioral literature and in intervention studies with individuals with ASD more generally (West et al., 2016), an interesting aspect of our analysis was the inclusion of culturally and geographically diverse caregiver–child dyads. Our findings suggest that the proposed procedures may be applicable to individuals from various cultural backgrounds. However, it should be noted that all caregivers could speak English as a second language and we could not offer caregiver training in the vernacular language for all participants, which might have been ideal (see for example Barkaia et al., 2017; Tsami et al., 2019).
The existing literature on mask‐induced deoxygenation offers mixed results. Although studies featuring surgeons as participants have found minor decrements in oxygen saturation after prolonged mask use (e.g., Beder et al., 2008), other analyses have reported no physiological burden due to mask wearing (Roberge et al., 2012). The pulse oximetry data reported in this study suggest that mask wearing did not lead to low oxygen saturation in our participants. Nevertheless, our assessment of pulse oximetry should be verified with a larger sample using gas exchange oximeter readings in comparable settings.
A few additional limitations should be noted. First, we did not conduct a functional analysis of problem behavior related to mask wearing. However, four participants engaged in problem behavior during baseline during which the caregiver provided contingent escape. Second, we did not establish mask wearing for periods longer than 10 min or conduct follow‐up probes. Additional research is needed to monitor mask wearing for longer periods, in a variety of different contexts (e.g., during low preference activities, school settings, group activities etc.), and to determine the specific mechanisms contributing to the continued tolerance of face masks. Evaluating the effects of mask choice is also an avenue for future research. Comparing baseline preference for face mask types (e.g., surgical, cloth mask) with posttraining tolerance for mask‐wearing could provide more robust generalization data. Third, we did not conduct stimulus preference assessments to select the high‐preference activities provided to participants while wearing the mask. Instead, we informally verified preference by monitoring continued activity engagement during sessions.
A fourth limitation is that it is not clear whether positive (i.e., delivery of a preferred item contingent upon completing the targeted steps in the exposure hierarchy) or negative reinforcement (i.e., termination of the session contingent on compliance with the target steps in the exposure hierarchy) was the lead contributor to the current outcomes. Fifth, we included prompted responses in our treatment integrity data, making it difficult to form conclusions about the caregivers' ability to implement the procedures independently. We also did not measure fidelity of the experimenter's telehealth coaching. Finally, we must assume a potential role for the various levels of instructional control shown by caregivers before the start of the intervention (Shimoff et al., 1981). As described earlier, all caregivers had prior experience implementing behavioral programs with the participants.
Some of the shortcomings listed above are in part due to the limited complexity imposed by the telehealth delivery format and also to a conscientious attempt to evaluate a treatment model that would be simple and practical. Previous telehealth studies focusing on challenging behaviors in individuals with ASD have offered mixed results (see Ferguson et al., 2019 for a review). The current analysis adds to the small but increasing body of evidence supporting telehealth as an effective way to deliver behavioral interventions and services. Although our analysis did not reveal the mechanisms necessary and sufficient for continued mask wearing in children with ASD, the overall treatment package was effective.
In sum, the current study adds to the literature by evaluating graduated exposure and shaping to teach mask wearing and (indirectly) abate mask‐induced problem behavior in children with ASD. Our findings support the efficacy of these procedures despite the diverse cultural backgrounds of our participants.
This study was partially supported by the Marguerite‐Marie Delacroix Support Fund and in‐kind contributions from ABA España (Spain) both awarded to M. Sivaraman.
Footnotes
Action Editor, Dorothea Lerman
REFERENCES
- American Thoracic Society (2018). Pulse Oximetry . Downloaded from https://www.thoracic.org/patients/patient-resources/resources/pulse-oximetry.pdf
- Barkaia, A. , Stokes, T. F. , & Mikiashvili, T. (2017). Intercontinental telehealth coaching of therapists to improve verbalizations by children with autism. Journal of Applied Behavior Analysis, 50(1), 582–589. 10.1002/jaba.391 [DOI] [PubMed] [Google Scholar]
- Bartoszko, J. J. , Farooqi, M. A. M. , Alhazzani, W. , & Loeb, M. (2020). Medical masks vs N95 respirators for preventing COVID‐19 in health care workers a systematic review and meta‐analysis of randomized trials. Influenza and Other Respiratory Viruses, 14(4), 365‐373. 10.1111/irv.12745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beder, A. , Buyukkocak, U. , Sabuncuoglu, H. , Keskil, Z. A. , & Keskil, S. (2008). Preliminary report on surgical mask induced deoxygenation during major surgery. Neurocirugia, 19(2), 121–126. 10.1016/S1130-1473(08)70235-5 [DOI] [PubMed] [Google Scholar]
- Bishop, M. R. , Kenzer, A. L. , Coffman, C. M. , Tarbox, M. C. , Tarbox, M. J. , & Lanagan, M. T. (2013). Using stimulus fading without escape extinction to increase compliance with toothbrushing in children with autism. Research in Autism Spectrum Disorders, 7(6), 680–686. 10.1016/j.rasd.2013.02.004 [DOI] [Google Scholar]
- Buckley, J. , Luiselli, K. J. , Harper, M. J. , & Shlesinger, A. (2020). Teaching students with autism spectrum disorder to tolerate haircutting. Journal of Applied Behavior Analysis, 53(4), 2081‐2089. 10.1002/jaba.713 [DOI] [PubMed] [Google Scholar]
- Buekers, J. , Theunis, J. , De Boever, P. , Vaes, A. W. , Koopman, M. , Janssen, E. V. , Wouters, E. F. , Spruit, M. A. , & Aerts, J. M. (2019). Wearable finger pulse oximetry for continuous oxygen saturation measurements during daily home routines of patients with chronic obstructive pulmonary disease (COPD) over one week: Observational study. Journal of Medical Internet Research mHealth and uHealth, 7(6), e12866. 10.2196/12866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng, V. C. , Wong, S. C. , Chuang, V. W. , So, S. Y. , Chen, J. H. , Sridhar, S. , To, K. K ., Chan, J. F. , Hung, I. F. , Ho, P. L. , & Yuen, K. Y. (2020). The role of community‐wide wearing of face mask for control of coronavirus disease 2019 (COVID‐19) epidemic due to SARS‐CoV‐2. The Journal of Infection, 81(1), 107–114. 10.1016/j.jinf.2020.04.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu, D. K. , Akl, E. A. , Duda, S. , Solo, K. , Yaacoub, S. , & Schunemann, J. H. (2020). Physical distancing, face masks, and eye protection to prevent person‐to‐person transmission of SARS‐CoV‐2 and COVID‐19: A systematic review and meta‐analysis. Lancet, 395(10242), 1973‐1987. 10.1016/S0140-6736(20)31142-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook, J. L. , Rapp, J. T. , & Schulze, K. A. (2015). Differential negative reinforcement of other behavior to increase wearing of a medical bracelet. Journal of Applied Behavior Analysis, 48(4), 901–906. 10.1002/jaba.228 [DOI] [PubMed] [Google Scholar]
- Cox, A. D. , Virues‐Ortega, J. , Julio, F. , & Martin, T. L. (2017). Establishing motion control in children with autism and intellectual disability: Applications for anatomical and functional MRI. Journal of Applied Behavior Analysis, 50(1), 8‐26. 10.1002/jaba.351 [DOI] [PubMed] [Google Scholar]
- Degli Espinosa, F. , Metko, A. , Raimondi, M. , Impenna, M. , & Scognamiglio, E. (2020). A model of support for families of children with autism living in the COVID‐19 lockdown: Lessons from Italy. Behavior Analysis in Practice, 13(3), 1–9. 10.1007/s40617-020-00438-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLeon, I. G. , Hagopian, L. P. , Rodriguez‐Catter, V. , Bowman, L. G. , Long, E. S. , & Boelter, E. W. (2008). Increasing wearing of prescription glasses in individuals with mental retardation. Journal of Applied Behavior Analysis, 41(1), 137–142. 10.1901/jaba.2008.41-137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLeon, I. G. , & Iwata, B. A. (1996). Evaluation of a multiple‐stimulus presentation format for assessing reinforcer preferences. Journal of Applied Behavior Analysis, 29(4), 519–533. 10.1901/jaba.1996.29-519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esposito, S. , & Principi, N. (2020). To mask or not to mask children to overcome COVID‐19. European Journal of Pediatrics, 179(8), 1267–1270. 10.1007/s00431-020-03674-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson, J. , Craig, E. A. , & Dounavi, K. (2019). Telehealth as a model for providing behaviour analytic interventions to individuals with autism spectrum disorder: A systematic review. Journal of Autism and Developmental Disorders, 49(2), 582–616. 10.1007/s10803-018-3724-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghanbari, K. M. , Behzadifar, M. , & Imani‐Nasab, H. M. (2020). The impact of the social distancing policy on COVID‐19 new cases in Iran: Insights from an interrupted time series analysis. Health Policy. Advance Online Publication. https://www.researchsquare.com/article/rs-25818/v1 [PMC free article] [PubMed] [Google Scholar]
- Gotham, K. , Pickles, A. , & Lord, C. (2009). Standardizing ADOS scores for a measure of severity in autism spectrum disorders. Journal of Autism and Developmental Disorders, 39(5), 693–705. 10.1007/s10803-008-0674-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Güner, R. , Hasanoğlu, I. , & Aktaş, F. (2020). COVID‐19: Prevention and control measures in community. Turkish Journal of Medical Sciences, 50(SI‐1), 571–577. 10.3906/sag-2004-146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji, T. , Chen, H‐L. , Xu, J. , Wu, L. N. , Li, J.‐J. , Chen, K. , & Qin, G. (2020). Lockdown contained the spread of 2019 novel coronavirus disease in Huangshi City, China: early epidemiological findings. Clinical Infectious Diseases, ciaa390. 10.1093/cid/ciaa390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohn, A . (2007). Visual adaptation: Physiology, mechanisms, and functional benefits. Journal of Neurophysiology, 97(5), 3155–3164. 10.1152/jn.00086.2007 [DOI] [PubMed] [Google Scholar]
- Lake, M. A. (2020). What we know so far: COVID‐19 current clinical knowledge and research. Clinical Medicine (London, England), 20(2), 124–127. 10.7861/clinmed.2019-coron [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lima, M. , Barros, L. , & Aragão, G. F. (2020). Could autism spectrum disorders be a risk factor for COVID‐19? Medical Hypotheses, 144, 109899. 10.1016/j.mehy.2020.109899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord, C. , & Rutter, M. (2012). Autism Diagnostic Observation Schedule™, 2nd ed. (ADOS™‐2) . Western Psychological Services. [Google Scholar]
- MacIntyre, C. R. , & Chughtai, A. A. (2020). A rapid systematic review of the efficacy of face masks and respirators against coronaviruses and other respiratory transmissible viruses for the community, healthcare workers and sick patients. International Journal of Nursing Studies, 108, 103629. 10.1016/j.ijnurstu.2020.103629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marco, E. J. , Khatibi, K. , Hill, S. S. , Siegel, B. , Arroyo, M. S. , Dowling, A. F. , Neuhaus, J. M. , Sherr, E. H. , Hinkley, L. N. , & Nagarajan, S. S. (2012). Children with autism show reduced somatosensory response: An MEG study. Autism Research, 5(5), 340–351. 10.1002/aur.1247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neely, L. , Rispoli, M. , Gerow, S. , & Hong, E. R. (2016). Preparing interventionists via telepractice in incidental teaching for children with autism. Journal of Behavior Education, 25(4), 393–416. 10.1007/s10864-016-9250-7 [DOI] [Google Scholar]
- Piazza, C. C. , Fisher, W. W. , Brown, K. A. , Shore, B. A. , Patel, M. R. , Katz, R. M. , Sevin, B. M. , Gulotta, C. S. , & Blakely‐Smith, A. (2003). Functional analysis of inappropriate mealtime behaviors. Journal of Applied Behavior Analysis, 36(2), 187–204. 10.1901/jaba.2003.36-187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pogrebna, G. , & Kharlamov, A. (2020). The impact of cross‐cultural differences in hand washing patterns on the COVID‐19 outbreak magnitude. Regulation and Governance. Advance Online Publication. 10.13140/RG.2.2.23764.96649 [DOI] [Google Scholar]
- Puts, N. A. , Wodka, E. L. , Tommerdahl, M. , Mostofsky, S. H. , & Edden, R. A. (2014). Impaired tactile processing in children with autism spectrum disorder. Journal of Neurophysiology, 111(9), 1803–1811. 10.1152/jn.00890.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reimers, T. M. , & Wacker, D. P. (1992). Acceptability of behavioral treatments for children: Analog and naturalistic evaluations by parents. School Psychology Review, 21, 628–643. [Google Scholar]
- Richling, S. M. , Rapp, J. T. , Carroll, R. A. , Smith, J. N. , Nystedt, A. , & Siewert, B. (2011). Using noncontingent reinforcement to increase compliance with wearing prescription prostheses. Journal of Applied Behavior Analysis, 44(2), 375–379. 10.1901/jaba.2011.44-375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberge, R. J. , Kim, J‐H. , & Benson, S. M. (2012). Absence of consequential changes in physiological, thermal and subjective responses from wearing a surgical mask. Respiratory Physiology and Neurobiology, 181(1), 29–35. 10.1016/j.resp.2012.01.010 [DOI] [PubMed] [Google Scholar]
- Schopler, E. , Reichler, R. J. , DeVellis, R. F. , & Daly, K. (1980). Toward objective classification of childhood autism: Childhood Autism Rating Scale (CARS). Journal of Autism and Developmental Disorders, 10(1), 91–103. 10.1007/BF02408436 [DOI] [PubMed] [Google Scholar]
- Schopler, E. , Van Bourgondien, M. , Wellman, G. , & Love, S. (2010). CARS‐2: Childhood Autism Rating Scale‐Second Edition. Western Psychological Services.
- Shahid, Z. , Kalayanamitra, R. , McClafferty, B. , Kepko, D. , Ramgobin, D. , Patel, R. , Aggarwal, C. S. , Vunnam, R. , Sahu, N. , Bhatt, D. , Jones, K. , Golamari, R. , & Jain, R. (2020). COVID‐19 and older adults: What we know. Journal of the American Geriatrics Society, 68(5), 926–929. 10.1111/jgs.16472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimoff, E. , Catania, A. C. , & Matthews, B. A. (1981). Uninstructed human responding: Sensitivity of low‐rate performance to schedule contingencies. Journal of the Experimental Analysis of Behavior, 36(2), 207–220. 10.1901/jeab.1981.36-207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner, A. , & Andreone, B. E. (2015). Using graduated exposure and differential reinforcement to increase food repertoire in a child with autism. Behavior Analysis in Practice, 8(2), 233–240. 10.1007/s40617-015-0077-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsami, L. , Lerman, D. , & Toper‐Korkmaz, O. (2019). Effectiveness and acceptability of parent training via telehealth among families around the world. Journal of Applied Behavior Analysis, 52(4), 1113–1129. 10.1002/jaba.645 [DOI] [PubMed] [Google Scholar]
- Wacker, D. P. , Berg, W. K. , Harding, J. W. , Derby, K. M. , Asmus, J. M. , & Healy, A. (1998). Evaluation and long‐term treatment of aberrant behavior displayed by young children with developmental disabilities. Developmental and Behavioral Pediatrics, 19, 260–266. 10.1097/00004703-199808000-00004 [DOI] [PubMed] [Google Scholar]
- Wacker, D. P. , Lee, J. F. , Padilla Dalmau, Y. C. , Kopelman, T. G. , Lindgren, S. D. , Kuhle, J. , Pelzel, K. E. , Dyson, S. , Schieltz, K. M. , & Waldron, D. B. (2013). Conducting functional communication training via telehealth to reduce the problem behavior of young children with autism. Journal of Developmental and Physical Disabilities, 25(1), 35–48. 10.1007/s10882-012-9314-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wainer, A. L. , & Ingersoll, B. R. (2015). Increasing access to an ASD imitation intervention via a telehealth parent training program. Journal of Autism and Developmental Disorders, 45(12), 3877–3890. 10.1007/s10803-014-2186-7 [DOI] [PubMed] [Google Scholar]
- Wang, J. , Jiang, M. , Chen, X. , & Montaner, L. J. (2020). Cytokine storm and leukocyte changes in mild versus severe SARS‐CoV‐2 infection: Review of 3939 COVID‐19 patients in China and emerging pathogenesis and therapy concepts. Journal of Leukocyte Biology, 108(1), 17–41. 10.1002/JLB.3COVR0520-272R [DOI] [PMC free article] [PubMed] [Google Scholar]
- West, E. A. , Travers, J. C. , Kemper, T. D. , Liberty, L. M. , Cote, D. L. , McCollow, M. M. , & Stansberrry Brusnahan, L. L. (2016). Racial and ethnic diversity of participants in research supporting evidence‐based practices for learners with Autism Spectrum Disorder. The Journal of Special Education, 50(3), 151–163. 10.1177/0022466916632495. [DOI] [Google Scholar]
- World Health Organization . (2020). Advice on the use of masks in the context of COVID‐19. WHO. Retrieved from https://www.who.int/publications/i/item/advice‐on‐the‐use‐of‐masks‐in‐the‐community‐during‐home‐care‐and‐in‐healthcare‐settings‐in‐the‐context‐of‐the‐novel‐coronavirus‐(2019‐ncov)‐outbreak [Google Scholar]
- Zhou, F. , Yu, T. , Du, R. , Fan, G. , Liu, Y. , Liu, Z. , Xiang, J. , Wang, Y. , Song, B. , Gu, X. , Guan, L. , Wei, Y. , Li, H. , Wu, X. , Xu, J. , Tu, S. , Zhang, Y. , Chen, H. , & Cao, B. (2020). Clinical course and risk factors for mortality of adult inpatients with COVID‐19 in Wuhan, China: A retrospective cohort study. Lancet, 395(10229), 1054–1062. 10.1016/S0140-6736(20)30566-3 [DOI] [PMC free article] [PubMed] [Google Scholar]


