Abstract
Health anxiety has been linked with fear and anxiety regarding COVID‐19. Higher levels of health anxiety likely increased social distancing and self‐isolating during the pandemic. We investigated relations among health anxiety, fear of missing out (FOMO) on rewarding social experiences from social distancing, and consequential levels of problematic smartphone use (PSU) and gaming disorder (GD). We surveyed a broad sample of 812 U.S. and Canadian participants during the pandemic, in late‐May 2020, using the Short Health Anxiety Inventory, FOMO Scale, Smartphone Addiction Scale‐Short Version, and GD test. Significant bivariate relationships were found among health anxiety, FOMO, PSU, and GD severity. Using structural equation modeling, FOMO mediated relations between health anxiety and both PSU and GD severity. We discuss FOMO as an important variable explaining problematic digital technology use to compensate for unmet social needs from social distancing. We discuss these findings within the context of the Interaction of Person‐Affect‐Cognition‐Execution theoretical model of problematic internet use. Results offer novel insight into the role of health anxiety on FOMO from unmet social needs during the COVID‐19 pandemic, and consequential problematic internet use.
Keywords: COVID‐19, fear of missing out, gaming disorder, health anxiety, pandemics, problematic smartphone use
1. INTRODUCTION
In 2020, to combat the global COVID‐19 pandemic, stay‐at‐home restrictions and social distancing were introduced globally (Lewnard & Lo, 2020). Social restrictions consequently decreased the ability for many to maintain their prior extent of in‐person social relationships (Xiao, Zhang, Kong, Li, & Yang, 2020). Social distancing also increased digital technology use at home, for purposes of work, relieving boredom, and also online social contact (Elhai, Yang, McKay, & Asmundson, 2020; King, Delfabbro, Billieux, & Potenza, 2020; Kiraly et al., 2020). Yet, individual differences were observed in social distancing (Carvalho, Pianowski, & Goncalves, 2020), resulting in part from variation in anxiety and fear about contracting COVID‐19 and its health consequences (Jungmann & Witthöft, 2020; Mertens, Gerritsen, Duijndam, Salemink, & Engelhard, 2020; Taylor et al., 2020b). We examined how health anxiety may have impacted the fear of missing out (FOMO) on rewarding social experiences because of social distancing and stay‐at‐home restrictions as virus containment strategies. We additionally explored associations between FOMO and increased levels of problematic smartphone use (PSU) and gaming disorder (GD) to satisfy missed social needs.
Health anxiety is a trait‐based variable involving worry about one's physical health because of perceived changes in bodily sensations (Asmundson, Abramowitz, Richter, & Whedon, 2010). Health anxiety is relevant during a pandemic. Individuals high in health anxiety readily misinterpret innocuous symptoms (e.g., cough/body ache) as virus symptoms, increasing anxiety and unnecessary (but limited) healthcare utilization (Asmundson & Taylor, 2020). Health anxiety increased virus‐related fears during prior pandemics (Blakey & Abramowitz, 2017; Blakey, Reuman, Jacoby, & Abramowitz, 2015; Wheaton, Abramowitz, Berman, Fabricant, & Olatunji, 2011), and the COVID‐19 pandemic (Jungmann & Witthöft, 2020; Mertens et al., 2020; Taylor et al., 2020b).
During a pandemic, greater health anxiety can increase social distancing and staying home, in order to prevent contracting the virus (Gonçalves et al., 2020; Oosterhoff, Palmer, Wilson, & Shook, 2020). This fueling of social distancing, and associated decreases in socializing and social capital, during the pandemic can lead to greater levels of FOMO (Casale & Flett, 2020). FOMO is a personality construct (and process) defined by reluctance to miss important experiences, and desire for constant contact with one's social network (Przybylski, Murayama, DeHaan, & Gladwell, 2013). FOMO is conceptualized to develop from unmet social relatedness needs (Przybylski et al., 2013), correlates with negative affect (Elhai et al., 2018), and is particularly associated with depression and anxiety symptoms (reviewed in Elhai, Yang, & Montag, in press). FOMO is important because unmet social needs are implicated in poor mental health (Wang, Mann, Lloyd‐Evans, Ma, & Johnson, 2018; Williams, 2007).
Relevant to the COVID‐19 pandemic, social distancing and stay‐at‐home restrictions have resulted in increased levels of home internet technology use (Elhai, Yang, McKay, & Asmundson, 2020; King et al., 2020). In fact, FOMO is an important influence driving excessive digital technology use to satisfy social relatedness needs (reviewed in Elhai et al., in press). FOMO demonstrates moderate‐to‐large relations with levels of excessive smartphone use (Elhai, Gallinari, Rozgonjuk, & Yang, 2020; Elhai, Yang, Rozgonjuk, & Montag, 2020; Sha, Sariyska, Riedl, Lachmann, & Montag, 2019), social networking site use (Casale & Fioravanti, 2020; Dempsey, O'Brien, Tiamiyu, & Elhai, 2019; Sha et al., 2019), and internet gaming (Duman & Ozkara, in press).
We should emphasize that using digital technology devices and applications, such as smartphones and internet gaming, offers positive advantages. Internet gaming can relieve stress and build social capital through playing and online socialization with friends (Brand, Rumpf, King, Potenza, & Wegmann, 2020; Teng, 2018). Healthy/adaptive smartphone use can promote productivity (Doargajudhur & Dell, 2020), social capital (Choi, 2018), and academic learning (Crompton & Burke, 2018). And, because of stay‐at‐home restrictions during the COVID‐19 pandemic, computer technology (such as video calls) helped many people meet work and school demands remotely, especially in developed countries (Crawford, Butler‐Henderson, Rudolph, & Glowatz, 2020; Keesara, Jonas, & Schulman, 2020). However, consequences of computer technology use represent an inverted U‐shaped curve, where moderate use has beneficial effects over nominal use, but excessive use has deleterious effects (Montag & Walla, 2016).
GD is a distinct diagnosis in the International Classification of Diseases‐11 (ICD‐11), encompassing both online and offline gaming activity (World Health Organization, 2019). Unlike ICD‐11, however, the Diagnostic and Statistical Manual of Mental Disorders‐5 (DSM‐5) does not officially recognize GD but instead includes Internet GD as a condition requiring further research (American Psychiatric Association, 2013). New work suggests that WHO GD criteria are somewhat more conservative compared to the older DSM‐5 Internet GD criteria (Montag et al., 2019). PSU is not currently included in ICD‐11/DSM‐5, but nonetheless widely demonstrates adverse consequences (reviewed in Busch & McCarthy, 2020; Montag, Wegmann, Sariyska, Demetrovics, & Brand, in press). GD and PSU are conceptualized to involve excessive levels of digital technology use, with symptoms similar to those observed in substance use disorders, such as loss of control and preoccupation with use in daily life, continued use despite adverse consequences, and associated functional impairment (Costa & Kuss, 2019; Elhai, Levine, & Hall, 2019). GD and PSU can result in decreased work and school productivity, lower social intimacy, skipping meals, and worse physical health (Billieux, Flayelle, Rumpf, & Stein, 2019; Montag et al., in press). Recent work suggests overlap between PSU and (Internet) GD (Leung et al., 2020).
2. AIMS
Our primary aim was to understand the role of FOMO (from social distancing during the COVID‐19 pandemic) in explaining relations between health anxiety and levels of PSU and GD. We used a North American sample of community participants recruited online, examining associations between health anxiety, FOMO, and severity of GD and PSU.
2.1. Theory
Body‐related fears, as well as fears involving decreased socialization, are important components of the nature of fear and anxiety during the COVID‐19 pandemic (Schimmenti, Billieux, & Starcevic, 2020). We propose that health/body anxiety should increase social distancing (to protect oneself from COVID‐19), yet lead to fear involving decreased socialization such as FOMO. FOMO should in turn be associated with increased PSU and GD severity to fulfill unmet social needs.
We used the Interaction of Person‐Affect‐Cognition‐Execution (I‐PACE) theoretical framework of maladaptive Internet use (Brand et al., 2019; Brand, Young, Laier, Wolfling, & Potenza, 2016) to guide hypotheses. I‐PACE conceptualizes background/predispositional variables as important influences of problematic Internet use (PIU) (e.g., PSU and GD). Such background variables include psychopathology (e.g., trait health anxiety), personality traits, core cognitions, and biological predispositions. I‐PACE also theorizes that such predispositional variables can lead to affective and cognitive response variables, and these affective/cognitive responses are also important influences of PIU. Affective/cognitive responses include coping styles, Internet‐related cognitive biases (e.g., FOMO), impaired executive functioning, and mood dysregulation. Within the I‐PACE framework, affective and cognitive responses are conceptualized as mediating/moderating mechanisms explaining relations between background variables and PIU (Brand et al., 2016; Brand et al., 2019).
2.2. Hypotheses
Greater levels of anxiety, specifically health anxiety, should increase social distancing and staying home to avoid contracting COVID‐19 (Gonçalves et al., 2020; Oosterhoff et al., 2020). Within the context of unmet social relatedness needs from social distancing, FOMO should consequently increase (Casale & Flett, 2020; Przybylski et al., 2013). Health anxiety represents a background/predispositional variable in I‐PACE (Brand et al., 2016; Brand et al., 2019). FOMO represents an affective/cognitive response involving Internet‐related cognitive bias in I‐PACE (Elhai, Yang, & Montag, 2019; Wegmann, Oberst, Stodt, & Brand, 2017). Therefore, we hypothesized the following:
Hypothesis (H1)
Health anxiety should positively associate with FOMO.
FOMO contributes to PIU, in an attempt to fulfill social relatedness needs through online social contact (Przybylski et al., 2013). Prior work found FOMO related to increased levels of PSU (Elhai, Gallinari, Rozgonjuk, & Yang, 2020; Elhai, Yang, Rozgonjuk, & Montag, 2020; Sha et al., 2019), and GD (Duman & Ozkara, in press). Therefore, we hypothesized the following:
Hypothesis (H2)
FOMO should positively relate to greater PSU and GD severity.
Based on the above hypotheses, health anxiety related to COVID‐19 should associate with FOMO, in turn relating to increased PSU and GD severity. We expect a mediating mechanism, such that FOMO should mediate relations between health anxiety and PSU/GD severity. I‐PACE conceptualizes affective/cognitive responses (e.g., FOMO) as mechanisms explaining associations between background variables and PIU (Brand et al., 2016; Brand et al., 2019). Recent work predating the current pandemic showed that FOMO mediated relations between negative affectivity (depression/anxiety) and levels of problematic smartphone and social networking use (Dempsey et al., 2019; Elhai, Yang, Fang, Bai, & Hall, 2020; Wang et al., 2019; Yuan, Elhai, & Hall, 2021). Therefore, we hypothesized the following:
Hypothesis (H3)
FOMO should mediate relations between health anxiety and both GD and PSU severity.
2.3. Research model
Our research model is depicted in Figure 1. Health anxiety is represented by two variables (discussed below)—health anxiety and perceived negative consequences from illness (PNCI) (Alberts, Hadjistavropoulos, Jones, & Sharpe, 2013). These health anxiety variables should relate to FOMO (Hypothesis (H1)). FOMO in turn should correlate with PSU and GD severity (Hypothesis (H2)). Because studies often find women with greater PSU (Elhai, Dvorak, Levine, & Hall, 2017), and men with greater GD (Mihara & Higuchi, 2017), we controlled for sex in paths to PSU/GD. Because younger individuals engage in greater PSU (Elhai et al., 2017) and GD (Mihara & Higuchi, 2017), we controlled for age. Finally, younger individuals evidence greater FOMO (Elhai et al., in press), so we controlled for age on FOMO.
FIGURE 1.
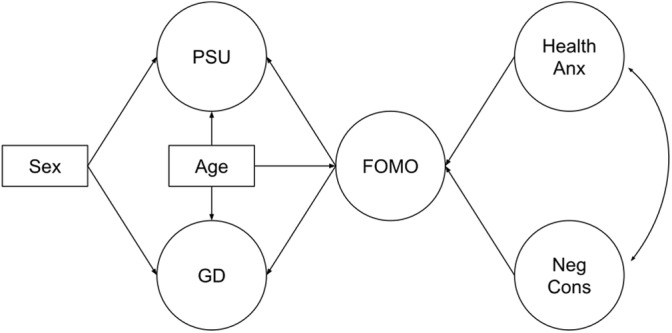
Hypothesized model. FOMO, fear of missing out; GD, gaming disorder; Health Anx, Health Anxiety; Neg Cons, Perceived Negative Consequences of Illness (PNCI); PSU, problematic smartphone use. Latent variables are depicted with circles, while observed variables are depicted with rectangles. For visual simplicity, factor loading paths from the latent variables are not displayed
3. METHODS
3.1. Procedure and participants
After receiving approval from the second author's institutional review board (abiding by U.S. federal law on human subjects protection), we conducted a cross‐sectional Internet panel survey of adult participants (age 18+ years), equally recruiting men and women. We used Qualtrics for online panel recruitment, a survey research firm, currently with 90 million online panel respondents. Qualtrics recruited participants in late‐May 2020 from Canada, and various regions in the United States. Participants were presented an online consent statement, and if consenting, the instruments discussed below. Participants were each compensated $4.
A total of 834 individuals participated. We removed six participants for excessive missing data, and 16 participants for inputting the same response consecutively for dozens of items, resulting in a final sample of 812 participants. Age averaged 44.45 years (SD = 17.21). Then, 405 men (49.9%) and 407 women (50.1%) participated. About half the sample reported being in Canada (n = 402, 49.5%); 410 (50.5%) participants were in the United States (40.2% in the South, 20.2% Northeast, 20.0% Midwest, 19.6% West). Racial and ethnic minority representation were evident from 95 Hispanic (11.7%), 96 Asian (11.8%), and 80 African‐American (9.9%) individuals. Completed education primarily included university (n = 237, 29.2%), high school (n = 226, 27.8%), or 2‐year college (n = 181, 22.4%).
3.2. Instruments
In addition to assessing demographic characteristics, we used the following web surveys. Internal consistency estimates for this sample are presented in Table 1.
TABLE 1.
Internal consistency estimates, and descriptive statistics separated by sex for the primary continuous variables
| Variable | Alpha | Men M (SD) | Women M (SD) | Sex F(1,810) | p | η 2 p |
|---|---|---|---|---|---|---|
| 1. Health Anx | .91 | 13.69 (8.46) | 12.96 (8.40) | 1.53 | .22 | .002 |
| 2. Neg Cons | .79 | 3.60 (2.76) | 3.12 (2.61) | 6.48 | .01 | .008 |
| 3. FOMO | .94 | 25.53 (10.91) | 22.48 (10.09) | 17.07 | <.001 | .021 |
| 4. PSU | .94 | 30.20 (15.08) | 26.62 (12.35) | 13.64 | <.001 | .017 |
| 5. GD | .92 | 9.19 (5.12) | 7.34 (4.10) | 32.47 | <.001 | .039 |
Note: Sex was coded “1” for men, and “2” for women.
Abbreviations: FOMO, fear of missing out; GD, gaming disorder; Health Anx, health anxiety; Neg Cons, perceived negative consequences of illness (PNCI); PSU, problematic smartphone use.
3.2.1. Short Health Anxiety Inventory
The Short Health Anxiety Inventory (SHAI; Salkovskis, Rimes, Warwick, & Clark, 2002) assesses health anxiety using a Likert‐type response scale from “0” to “3” with higher scores indicating greater health anxiety. The scale has a 14‐item health anxiety subscale and 4‐item PNCI subscale, extensively validated (Alberts et al., 2013). The health anxiety subscale involves current and anticipatory health‐related preoccupation, and interoceptive awareness. The PNCI subscale involves expected outcomes (e.g., quality of life, healing, etc.) from a serious illness.
3.2.2. FOMO scale
This scale is a 10‐item measure of FOMO (Przybylski et al., 2013). The scale uses a Likert‐type format from “1 = Not at all true of me” to “5 = Extremely true of me.” The instrument has been widely validated (Elhai et al., in press).
3.2.3. Smartphone Addiction Scale‐Short Version
The Smartphone Addiction Scale‐Short Version (SAS‐SV; Kwon, Kim, Cho, & Yang, 2013) is a 10‐item measure of PSU, using a Likert‐type scale from “1 = Strongly disagree” to “6 = Strongly agree.” We voiced items in the first‐person for improved consistency (Duke & Montag, 2017). The SAS‐SV has been validated previously (Harris, McCredie, & Fields, 2020; Lopez‐Fernandez, 2017).
3.2.4. GD test
The GD test (GDT) (Pontes et al., in press) is a four‐item measure of GD symptoms in line with ICD‐11 criteria. It uses a Likert‐type scale from “1 = Never” to “5 = Very often.” The GDT demonstrates adequate validity (Montag et al., 2019; Pontes et al., in press).
3.3. Analysis
We used R software v.4.0.1 (R Core Team, 2020) for data pre‐processing, and descriptive/correlational analysis. We used R packages pastecs (for descriptives), careless (careless responding), fmsb (internal consistency), corrplot (correlations), and sjstats (analysis of variance [ANOVA] effects). We utilized the mice package to impute small amounts of missing item‐level data with maximum likelihood procedures. We summed scale scores for health anxiety variables, FOMO, PSU, and GD, all normally distributed. We computed a Pearson correlation matrix, and tested for differences by sex using ANOVA.
We used Mplus v.8.1 (Muthén & Muthén, 1998–2019) to compute confirmatory factor analyses (CFAs) for psychological scale items. We treated items for each CFA as ordinal, using a polychoric covariance matrix, probit factor loadings, and weighted least squares estimation with a mean‐ and variance‐adjusted (WLSMV) chi‐square (Lei & Shiverdecker, 2020). We implemented residual error covariances for the (a) first (involving work impairment) and second (school impairment) items on the SAS‐SV, and (b) first and second items (both indicating that others “have more rewarding experiences than me”) on the FOMO Scale. We judged goodness of fit by comparative fit index (CFI) and Tucker–Lewis index (TLI) values > .94, standardized root mean square residual (SRMR) <.08, and root mean square error of approximation (RMSEA) <.06 (Maydeu‐Olivares, 2017); however, RMSEA too often rejects well‐fitting models using ordinal data (Shi, Maydeu‐Olivares, & Rosseel, 2020).
We tested the model shown in Figure 1 with structural equation modeling (SEM) using the analytic approach above. Health anxiety and PNCI paths to FOMO test Hypothesis (H1). FOMO paths to PSU and GD severity test (Hypothesis (H2)). We also tested model variations, removing/adding several demographic variable paths, but these variations worsened or did not enhance fit. Next, we tested mediation by computing path coefficient cross‐products from the paths shown in Figure 1. We used the Delta method to estimate indirect effect (mediation) SEs, with 1,000 nonparametric bootstrapped replications (Hayes, 2017). We conducted four mediation tests to examine Hypothesis (H3) (i.e., that FOMO would mediate relations between health anxiety and PSU/GD severity; see Table 2 for mediation details).
TABLE 2.
Mediation tests
| Mediation tests | β | SE | z | p |
|---|---|---|---|---|
| Health Anx‐ > FOMO‐ > PSU | .403 | .056 | 7.144 | <.001 |
| Neg Cons‐ > FOMO‐ > PSU | −.035 | .056 | −.631 | .528 |
| Health Anx‐ > FOMO‐ > GD | .395 | .056 | 7.061 | <.001 |
| Neg Cons‐ > FOMO‐ > GD | −.035 | .055 | −.633 | .527 |
Abbreviations: FOMO, fear of missing out; GD, gaming disorder; Health Anx, health anxiety; Neg Cons, perceived negative consequences of illness (PNCI); PSU, problematic smartphone use.
4. RESULTS
Table 1 displays descriptive statistics for psychological scales, separated by sex. Men scored higher on several scales, though effects were rather small in magnitude. Scale intercorrelations are displayed in Figure 2. Health anxiety and PNCI showed moderate‐to‐large associations with FOMO (Hypothesis (H1)). FOMO demonstrated rather large associations with PSU and GD severity (Hypothesis (H2)). Age was inversely correlated with all scales.
FIGURE 2.
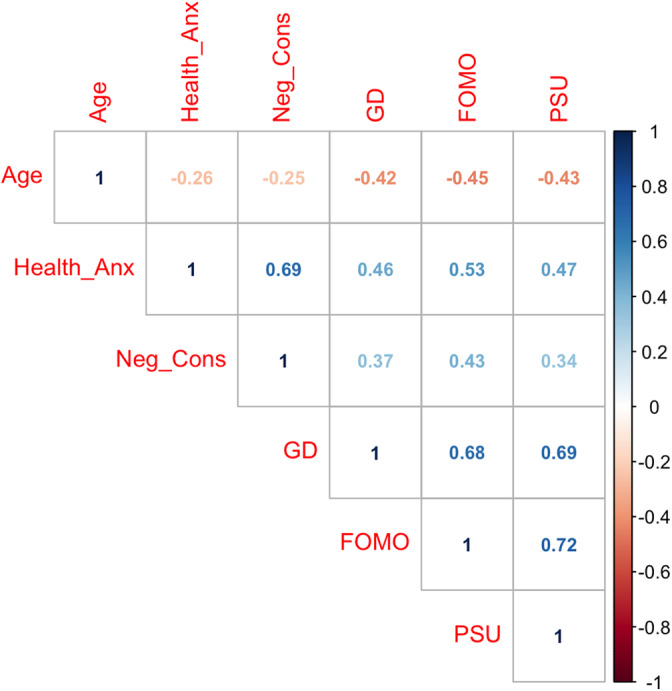
Correlation matrix of primary variables. FOMO, fear of missing out; GD, gaming disorder; Health Anx, Health Anxiety; Neg Cons, Perceived Negative Consequences of Illness (PNCI); PSU, problematic smartphone use. Correlations with a darker shade indicate stronger correlations, with blue indicating positive and red indicating negative correlations. All correlation ps < .001
CFAs fit well, besides worse fit from RMSEA which is expected (Shi et al., 2020). The health anxiety/PNCI two‐factor CFA fit well, WLSMV χ 2(134, N = 812) = 748.35, p < .001, CFI = .96, TLI = .95, SRMR = .04, RMSEA = .08 (90% CI: .07–.08). The FOMO CFA fit well, WLSMV χ 2(34, N = 812) = 577.06, p < .001, CFI = .97, TLI = .97, SRMR = .04, RMSEA = .14 (90% CI: .13–.15). The PSU CFA fit well, WLSMV χ 2(34, N = 812) = 460.24, p < .001, CFI = .98, TLI = .97, SRMR = .03, RMSEA = .12 (90% CI: .11–.13). Finally, the GD CFA fit well, WLSMV χ 2(2, N = 812) = 6.99, p = .03, CFI = 1.00, TLI = .99, SRMR < .01, RMSEA = .06 (90% CI: .02–.10).
The SEM depicted in Figure 1 yielded some evidence for adequate fit, WLSMV χ 2(890, N = 812) = 3,193.77, p < .001, CFI = .94, TLI = .94, SRMR = .09, RMSEA = .06 (90% CI: .05–.06). Figure 3 demonstrates that after adjusting for age, health anxiety (but not PNCI) was significantly associated with FOMO, supporting Hypothesis (H1). Adjusting for age and sex, FOMO was related to both PSU and GD severity, supporting H2.
FIGURE 3.
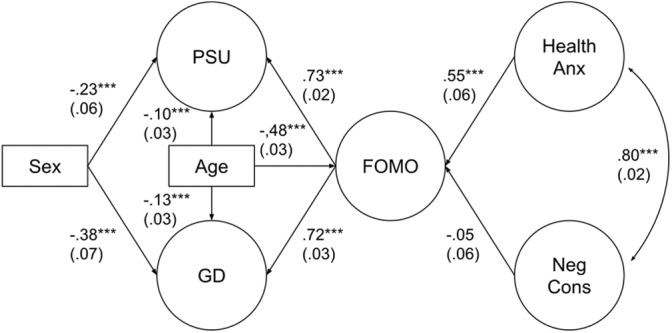
Hypothesized model with standardized path coefficients. FOMO, fear of missing out; GD, gaming disorder; Health Anx, Health Anxiety; Neg Cons, Perceived Negative Consequences of Illness (PNCI); PSU, problematic smartphone use. Latent variables are depicted with circles, while observed variables are depicted with rectangles. SEs are displayed in parentheses. For visual simplicity, factor loading paths from the latent variables are not displayed, but estimates can be requested from the first author. Sex was coded “1” for men, and “2” for women. *p < .05, **p < .01, ***p < .001
Mediation results are displayed in Table 2, supporting Hypothesis (H3). FOMO mediated relations between health anxiety (but not PNCI) and PSU severity. FOMO also mediated relations between health anxiety (but not PNCI) and GD severity.
Finally, we present findings from a revised model, where we added paths from PSU and GD to both health anxiety variables. This revised model demonstrated adequate fit, χ 2(887, N = 812) = 3,291.69, p < .001, CFI = .94, TLI = .94, SRMR = .06, RMSEA = .06 (90% CI: .05–.06). However, improvement in fit was negligible, with a change in CFI value (Cheung & Rensvold, 2002) of only .002. Nonetheless, significant associations among the added paths were found between GDT severity with both health anxiety (β = .29, SE = .05, p < .001) and PNCI (β = .33, SE = .06, p < .001); and between PSU severity with health anxiety (β = .15, SE = .05, p = .002) but not PNCI (β = .02, SE = .06, p = .74).
5. DISCUSSION
Among a broad North American sample surveyed during the COVID‐19 pandemic, we found support for positive associations between health anxiety and FOMO (Hypothesis (H1)), and between FOMO with greater GD and PSU severity (Hypothesis (H2)). We also discovered that FOMO mediated relations between health anxiety and both GD and PSU severity (Hypothesis (H3)).
Results partially supported Hypothesis (H1) regarding positive associations between health anxiety and FOMO. Specifically, FOMO was related to both health anxiety and PNCI in bivariate analyses but not with PNCI in SEM. Prior work has not tested FOMO in relation to health anxiety, though a plethora of research supports the association of FOMO with other forms of anxiety (Elhai et al., in press). Our finding fits with the notion that anxiety, and especially health anxiety, experienced within COVID‐19 social distancing (Gonçalves et al., 2020; Oosterhoff et al., 2020) would drive FOMO because of unmet social needs (Casale & Flett, 2020). Results also fit with the I‐PACE conceptualization that background variables (e.g., anxiety) influence affective/coping responses such as Internet‐related cognitive bias (e.g., FOMO) (Brand et al., 2016; Brand et al., 2019).
Results supported (Hypothesis (H2)) in that FOMO related to GD and PSU severity, in bivariate and SEM analyses. These findings fit with the I‐PACE conceptualization of affective/cognitive response variables such as FOMO (Elhai, Yang, & Montag, 2019; Wegmann et al., 2017) driving PIU. Results also corroborate prior work linking FOMO with PIU, such as PSU/GD (Elhai et al., in press). In fact, we found quite large relationships for FOMO with severity of PSU (bivariate r = .72, SEM β = .73) and GD (bivariate r = .68, SEM β = .72) compared to prior work (Elhai et al., in press). Perhaps because of pandemic‐related social distancing and stay‐at‐home restrictions, participants had fewer (in‐person) socialization options besides digital technology use to alleviate their FOMO, therefore increasing the strength of association for FOMO with GD/PSU severity. These results may speak to gaming and smartphone use as self‐medication for negative emotion among participants during the COVID pandemic, supporting recent findings (Taylor et al., 2020a).
We found partial support for Hypothesis (H3): FOMO mediated relations between health anxiety (but not PNCI) with both GD and PSU severity. This finding is consistent with the I‐PACE conceptualization that affective/cognitive responses such as FOMO serve as mechanisms explaining relations between background/predispositional variables and PIU. Thus, during a pandemic, trait health anxiety alone may not solely drive PSU and GD symptoms; FOMO, likely resulting from social distancing, may account for this relationship. In fact, prior work revealed that FOMO mediated associations between trait anxiety and PIU (Casale & Fioravanti, 2020; Dempsey et al., 2019; Duman & Ozkara, in press; Elhai, Gallinari, Rozgonjuk, & Yang, 2020; Elhai, Yang, Rozgonjuk, & Montag, 2020; Sha et al., 2019).
We found that age was inversely related to health anxiety, at first glance appearing counter‐intuitive. However, other work revealed that changes in bodily sensations are more common and accepted as normal among older individuals (because of experience), but more concerning among younger people (Mahoney, Segal, & Coolidge, 2015). Additionally, we unexpectedly discovered greater PSU severity in men than women, while much prior work found the opposite pattern (Elhai et al., 2017). Yet, during the COVID‐19 pandemic, women more often served as frontline workers in the healthcare and food industry, while men more often remotely worked from home (Wenham, Smith, & Morgan, 2020). Therefore, men may have had greater access and time spent on smartphones at home.
We acknowledge the cross‐sectional nature of our research design prevents us from inferring causal relationships among our study variables. Repeated measures/longitudinal work could clarify the temporal nature of associations (Elhai, Rozgonjuk, Liu, & Yang, 2020; Yuan et al., 2021). Additionally, we relied on self‐report measures, while objective behavioral assessment of PSU and GD would be more accurate (Ryding & Kuss, 2020). Generalizability is limited because we only surveyed North American participants. Other countries managed social distancing differently, and thus results may not cross‐validate. Nonetheless, these results offer insight into the role of health anxiety on FOMO from unmet social needs during the COVID‐19 pandemic, and consequential PIU.
CONFLICTS OF INTEREST
Dr J. D. E. notes that he receives royalties for several books published on posttraumatic stress disorder (PTSD); is a paid, full‐time faculty member at University of Toledo; is a paid, visiting scientist at Tianjin Normal University; occasionally serves as a paid, expert witness on PTSD legal cases; and receives grant research funding from the U.S. National Institutes of Health. Dr D. M. notes that he receives royalties for several books written on anxiety disorders in adults and children, obsessive–compulsive disorder, and research methodology; is a paid full‐time faculty member at Fordham University; holds a research fellow position in a joint relationship between Fordham University and Columbia University; and has private grant funding from a venture capital research corporation to investigate methods of reducing public speaking fears. Dr C. M. mentions that he has received (to Ulm University and earlier University of Bonn) grants from agencies such as the German Research Foundation (DFG). Dr C. M. has performed grant reviews for several agencies; has edited journal sections and articles; has given academic lectures in clinical or scientific venues or companies; and has generated books or book chapters for publishers of mental health texts. For some of these activities he received royalties, but never from the gaming or social media industry. Dr. C. M. mentions that he is part of a discussion circle (Digitalität und Verantwortung: https://about.fb.com/de/news/h/gespraechskreis-digitalitaet-und-verantwortung/) debating ethical questions linked to social media, digitalization, and society/democracy at Facebook. In this context, he receives no salary for his activities. Finally, he mentions that he currently functions as independent scientist on the scientific advisory board of the Nymphenburg group. This activity is financially compensated. Dr G. J. G. A. is the Editor‐in‐Chief of the Journal of Anxiety Disorders and Development Editor of Clinical Psychology Review. He receives financial support through payments for his editorial work on the aforementioned journals and royalties from various book publishers. He also currently hold research grants awarded by the Canadian Institutes of Health Research. The other authors declare no conflicts of interest.
ETHICS STATEMENT
IRB approval was received from the Fordham University's IRB before the project was conducted.
PATIENT CONSENT
All participants provided consent via an informed consent statement before participating.
ACKNOWLEDGMENTS
A portion of this study was supported by a grant from the Canadian Institute for Health Research (PI: G. J. G. A.). The funding agency had no role in the conduct of data collection, analysis, or write‐up.
Biographies
jon d. elhai is a professor of Psychology and Psychiatry at the University of Toledo, and has an academic affiliation with Tianjin Normal University. His primary area of research is in posttraumatic stress disorder (PTSD), studying the disorder's underlying dimensions, and relations with cognitive coping processes and externalizing behaviors. He also has a program of research on cyberpsychology, examining problematic internet, and smartphone use.

dean mckay is a professor of Psychology at Fordham University. His research is primarily in anxiety disorders and obsessive–compulsive disorder, as well as the role of disgust in psychopathology. He also has an ongoing program of research on misophonia (selective sound sensitivity).

haibo yang is a professor in the Academy of Psychology and Behavior at Tianjin Normal University. His primary area of research is cognitive processing in children and adolescents with posttraumatic stress disorder (PTSD), studying attentional bias, and execution control. In recent years, he has focused on the study of cyberpsychology and overuse of smartphones among adolescents.

charlene minaya is a second year doctoral student in the Clinical Psychology PhD program at Fordham University. Her primary research interests are the etiology, maintenance, and treatment of anxiety, and obsessive–compulsive and related disorders (OCRDs).

dr christian montag is a professor for Molecular Psychology at Ulm University (Ulm, Germany). He studied psychology at University of Giessen (Giessen, Germany) and then worked on his PhD and habilitation dissertation at University of Bonn (Bonn, Germany). C. M. is interested in Personality Neuroscience. Here, he also combines molecular genetics with brain imaging techniques such as structural/functional MRI to better understand individual differences in human nature. Adding to this he conducts research in the fields of Neuroeconomics, Technological Use Disorders, and Psychoinformatics. In the realm of Psychoinformatics, he applies mobile sensing and digital phenotyping principles to predict psychological traits and states.

gordon j. g. asmundson is a full professor of Psychology and Director of the Psychology of Pandemics Network at the University of Regina. He serves as the Editor‐in‐Chief of the Journal of Anxiety Disorders and of Clinical Psychology Review. His research and clinical interests are in assessment and basic mechanisms of fear, anxiety and related disorders (e.g., posttraumatic stress disorder, social anxiety disorder, health anxiety), childhood adversity, and chronic pain, and the association of these with each other, maladaptive coping, and disability.

Elhai JD, McKay D, Yang H, Minaya C, Montag C, Asmundson GJG. Health anxiety related to problematic smartphone use and gaming disorder severity during COVID‐19: Fear of missing out as a mediator. Hum Behav & Emerg Tech. 2021;3:137–146. 10.1002/hbe2.227
Funding information Canadian Institute for Health Research
DATA AVAILABILITY STATEMENT
Anonymized data used in this study may be requested from the second author, and provided upon reasonable request.
REFERENCES
- Alberts, N. M. , Hadjistavropoulos, H. D. , Jones, S. L. , & Sharpe, D. (2013). The short health anxiety inventory: A systematic review and meta‐analysis. Journal of Anxiety Disorders, 27(1), 68–78. 10.1016/j.janxdis.2012.10.009 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- Asmundson, G. J. G. , Abramowitz, J. S. , Richter, A. A. , & Whedon, M. (2010). Health anxiety: Current perspectives and future directions. Current Psychiatry Reports, 12(4), 306–312. 10.1007/s11920-010-0123-9 [DOI] [PubMed] [Google Scholar]
- Asmundson, G. J. G. , & Taylor, S. (2020). How health anxiety influences responses to viral outbreaks like COVID‐19: What all decision‐makers, health authorities, and health care professionals need to know. Journal of Anxiety Disorders, 71, 102211. 10.1016/j.janxdis.2020.102211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billieux, J. , Flayelle, M. , Rumpf, H.‐J. , & Stein, D. J. (2019). High involvement versus pathological involvement in video games: A crucial distinction for ensuring the validity and utility of gaming disorder. Current Addiction Reports, 6(3), 323–330. 10.1007/s40429-019-00259-x [DOI] [Google Scholar]
- Blakey, S. M. , & Abramowitz, J. S. (2017). Psychological predictors of health anxiety in response to the Zika virus. Journal of Clinical Psychology in Medical Settings, 24(3–4), 270–278. 10.1007/s10880-017-9514-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blakey, S. M. , Reuman, L. , Jacoby, R. J. , & Abramowitz, J. S. (2015). Tracing "Fearbola": Psychological predictors of anxious responding to the threat of Ebola. Cognitive Therapy and Research, 39(6), 816–825. 10.1007/s10608-015-9701-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand, M. , Rumpf, H. J. , King, D. L. , Potenza, M. N. , & Wegmann, E. (2020). Clarifying terminologies in research on gaming disorder and other addictive behaviors: Distinctions between core symptoms and underlying psychological processes. Current Opinion in Psychology, 36, 49–54. 10.1016/j.copsyc.2020.04.006 [DOI] [PubMed] [Google Scholar]
- Brand, M. , Wegmann, E. , Stark, R. , Muller, A. , Wolfling, K. , Robbins, T. W. , & Potenza, M. N. (2019). The interaction of person‐affect‐cognition‐execution (I‐PACE) model for addictive behaviors: Update, generalization to addictive behaviors beyond internet‐use disorders, and specification of the process character of addictive behaviors. Neuroscience and Biobehavioral Reviews, 104, 1–10. 10.1016/j.neubiorev.2019.06.032 [DOI] [PubMed] [Google Scholar]
- Brand, M. , Young, K. S. , Laier, C. , Wolfling, K. , & Potenza, M. N. (2016). Integrating psychological and neurobiological considerations regarding the development and maintenance of specific internet‐use disorders: An interaction of person‐affect‐cognition‐execution (I‐PACE) model. Neuroscience and Biobehavioral Reviews, 71, 252–266. 10.1016/j.neubiorev.2016.08.033 [DOI] [PubMed] [Google Scholar]
- Busch, P. A. , & McCarthy, S. (2020). Antecedents and consequences of problematic smartphone use: A systematic literature review of an emerging research area. Computers in Human Behavior, 114, 106414. 10.1016/j.chb.2020.106414 [DOI] [Google Scholar]
- Carvalho, L. F. , Pianowski, G. , & Goncalves, A. P. (2020). Personality differences and COVID‐19: Are extroversion and conscientiousness personality traits associated with engagement with containment measures? Trends in Psychiatry and Psychotherapy, 42(2), 179–184. 10.1590/2237-6089-2020-0029 [DOI] [PubMed] [Google Scholar]
- Casale, S. , & Fioravanti, G. (2020). Factor structure and psychometric properties of the Italian version of the fear of missing out scale in emerging adults and adolescents. Addictive Behaviors, 102, 106179. 10.1016/j.addbeh.2019.106179 [DOI] [PubMed] [Google Scholar]
- Casale, S. , & Flett, G. L. (2020). Interpersonally‐based fears during the COVID‐19 pandemic: Reflections on the fear of missing out and the fear of not mattering constructs. Clinical Neuropsychiatry, 17(2), 88–93. 10.36131/CN20200211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung, G. W. , & Rensvold, R. B. (2002). Evaluating goodness‐of‐fit indexes for testing measurement invariance. Structural Equation Modeling, 9(2), 233–255. 10.1207/S15328007SEM0902_5 [DOI] [Google Scholar]
- Choi, S. (2018). The roles of media capabilities of smartphone‐based SNS in developing social capital. Behaviour & Information Technology, 38(6), 609–620. 10.1080/0144929x.2018.1546903 [DOI] [Google Scholar]
- Costa, S. , & Kuss, D. J. (2019). Current diagnostic procedures and interventions for gaming disorders: A systematic review. Frontiers in Psychology, 10, 578. 10.3389/fpsyg.2019.00578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford, J. , Butler‐Henderson, K. , Rudolph, J. , & Glowatz, M. (2020). COVID‐19: 20 countries' higher education intra‐period digital pedagogy responses. Journal of Applied Learning and Teaching, 3(1), 9–28. 10.37074/jalt.2020.3.1.7 [DOI] [Google Scholar]
- Crompton, H. , & Burke, D. (2018). The use of mobile learning in higher education: A systematic review. Computers & Education, 123, 53–64. 10.1016/j.compedu.2018.04.007 [DOI] [Google Scholar]
- Dempsey, A. E. , O'Brien, K. D. , Tiamiyu, M. F. , & Elhai, J. D. (2019). Fear of missing out (FoMO) and rumination mediate relations between social anxiety and problematic Facebook use. Addictive Behaviors Reports, 9, 100150. 10.1016/j.abrep.2018.100150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doargajudhur, M. S. , & Dell, P. (2020). The effect of bring your own device (BYOD) adoption on work performance and motivation. Journal of Computer Information Systems. 10.1080/08874417.2018.1543001 60(6), 518–529. [DOI] [Google Scholar]
- Duke, E. , & Montag, C. (2017). Smartphone addiction, daily interruptions and self‐reported productivity. Addictive Behaviors Reports, 6, 90–95. 10.1016/j.abrep.2017.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duman, H. , & Ozkara, B. Y. (in press). The impact of social identity on online game addiction: The mediating role of the fear of missing out (FoMO) and the moderating role of the need to belong. Current Psychology. 10.1007/s12144-019-00392-w [DOI] [Google Scholar]
- Elhai, J. D. , Dvorak, R. D. , Levine, J. C. , & Hall, B. J. (2017). Problematic smartphone use: A conceptual overview and systematic review of relations with anxiety and depression psychopathology. Journal of Affective Disorders, 207, 251–259. 10.1016/j.jad.2016.08.030 [DOI] [PubMed] [Google Scholar]
- Elhai, J. D. , Gallinari, E. F. , Rozgonjuk, D. , & Yang, H. (2020). Depression, anxiety and fear of missing out as correlates of social, non‐social and problematic smartphone use. Addictive Behaviors, 105, 106335. 10.1016/j.addbeh.2020.106335 [DOI] [PubMed] [Google Scholar]
- Elhai, J. D. , Levine, J. C. , Alghraibeh, A. M. , Alafnan, A. , Aldraiweesh, A. , & Hall, B. J. (2018). Fear of missing out: Testing relationships with negative affectivity, online social engagement, and problematic smartphone use. Computers in Human Behavior, 89, 289–298. 10.1016/j.chb.2018.08.020 [DOI] [Google Scholar]
- Elhai, J. D. , Levine, J. C. , & Hall, B. J. (2019). The relationship between anxiety symptom severity and problematic smartphone use: A review of the literature and conceptual frameworks. Journal of Anxiety Disorders, 62, 45–52. 10.1016/j.janxdis.2018.11.005 [DOI] [PubMed] [Google Scholar]
- Elhai, J. D. , Rozgonjuk, D. , Liu, T. , & Yang, H. (2020). Fear of missing out is related to repeated measurements of negative affect using experience sampling methodology. Journal of Affective Disorders, 262, 298–303. 10.1016/j.jad.2019.11.026 [DOI] [PubMed] [Google Scholar]
- Elhai, J. D. , Yang, H. , Fang, J. , Bai, Y. , & Hall, B. J. (2020). Depression and anxiety symptoms are related to problematic smartphone use severity in Chinese young adults: Fear of missing out as a mediator. Addictive Behaviors, 101, 105962. 10.1016/j.addbeh.2019.04.020 [DOI] [PubMed] [Google Scholar]
- Elhai, J. D. , Yang, H. , McKay, D. , & Asmundson, G. J. G. (2020). COVID‐19 anxiety symptoms associated with problematic smartphone use severity in Chinese adults. Journal of Affective Disorders, 274, 576–582. 10.1016/j.jad.2020.05.080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elhai, J. D. , Yang, H. , & Montag, C. (2019). Cognitive‐ and emotion‐related dysfunctional coping processes: Transdiagnostic mechanisms explaining depression and anxiety's relations with problematic smartphone use. Current Addiction Reports, 6, 410–417. 10.1007/s40429-019-00260-4 [DOI] [Google Scholar]
- Elhai, J. D. , Yang, H. , & Montag, C. (in press). Fear of missing out (FOMO): Overview, theoretical underpinnings, and literature review on relations with severity of negative affectivity and problematic technology use. Brazilian Journal of Psychiatry. 10.1590/1516-4446-2020-0870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elhai, J. D. , Yang, H. , Rozgonjuk, D. , & Montag, C. (2020). Using machine learning to model problematic smartphone use severity: The significant role of fear of missing out. Addictive Behaviors, 103, 106261. 10.1016/j.addbeh.2019.106261 [DOI] [PubMed] [Google Scholar]
- Gonçalves, A. P. , Zuanazzi, A. C. , Salvador, A. P. , Jaloto, A. , Pianowski, G. , & Carvalho, L. F. (2020). Preliminary findings on the associations between mental health indicators and social isolation during the COVID‐19 pandemic. Archives of Psychiatry and Psychotherapy, 22(2), 10–19. 10.12740/APP/122576 [DOI] [Google Scholar]
- Harris, B. , McCredie, M. , & Fields, S. (2020). Examining the psychometric properties of the smartphone addiction scale and its short version for use with emerging adults in the U.S. Computers in Human Behavior Reports, 1, 100011. 10.1016/j.chbr.2020.100011 [DOI] [Google Scholar]
- Hayes, A. F. (2017). Introduction to mediation, moderation, and conditional process analysis: A regression‐based approach (2nd ed.). New York, NY: Guilford. [Google Scholar]
- Jungmann, S. M. , & Witthöft, M. (2020). Health anxiety, cyberchondria, and coping in the current COVID‐19 pandemic: Which factors are related to coronavirus anxiety? Journal of Anxiety Disorders, 73, 102239. 10.1016/j.janxdis.2020.102239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keesara, S. , Jonas, A. , & Schulman, K. (2020). Covid‐19 and health care's digital revolution. New England Journal of Medicine, 382(23), e82. 10.1056/NEJMp2005835 [DOI] [PubMed] [Google Scholar]
- King, D. L. , Delfabbro, P. H. , Billieux, J. , & Potenza, M. N. (2020). Problematic online gaming and the COVID‐19 pandemic. Journal of Behavioral Addictions, 9(2), 184–186. 10.1556/2006.2020.00016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiraly, O. , Potenza, M. N. , Stein, D. J. , King, D. L. , Hodgins, D. C. , Saunders, J. B. , … Demetrovics, Z. (2020). Preventing problematic internet use during the COVID‐19 pandemic: Consensus guidance. Comprehensive Psychiatry, 100, 152180. 10.1016/j.comppsych.2020.152180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon, M. , Kim, D. J. , Cho, H. , & Yang, S. (2013). The smartphone addiction scale: Development and validation of a short version for adolescents. PLoS One, 8(12), e83558. 10.1371/journal.pone.0083558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lei, P. W. , & Shiverdecker, L. K. (2020). Performance of estimators for confirmatory factor analysis of ordinal variables with missing data. Structural Equation Modeling: A Multidisciplinary Journal, 27(4), 584–601. 10.1080/10705511.2019.1680292 [DOI] [Google Scholar]
- Leung, H. , Pakpour, A. H. , Strong, C. , Lin, Y. C. , Tsai, M. C. , Griffiths, M. D. , … Chen, I. H. (2020). Measurement invariance across young adults from Hong Kong and Taiwan among three internet‐related addiction scales: Bergen Social Media Addiction Scale (BSMAS), Smartphone Application‐Based Addiction Scale (SABAS), and Internet Gaming Disorder Scale‐Short Form (IGDS‐SF9) (Study Part A). Addictive Behaviors, 101, 105969. 10.1016/j.addbeh.2019.04.027 [DOI] [PubMed] [Google Scholar]
- Lewnard, J. A. , & Lo, N. (2020). Scientific and ethical basis for social‐distancing interventions against COVID‐19. The Lancet: Infectious Diseases, 20(6), 631–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez‐Fernandez, O. (2017). Short version of the Smartphone Addiction Scale adapted to Spanish and French: Towards a cross‐cultural research in problematic mobile phone use. Addictive Behaviors, 64, 275–280. 10.1016/j.addbeh.2015.11.013 [DOI] [PubMed] [Google Scholar]
- Mahoney, C. T. , Segal, D. L. , & Coolidge, F. L. (2015). Anxiety sensitivity, experiential avoidance, and mindfulness among younger and older adults: Age differences in risk factors for anxiety symptoms. The International Journal of Aging and Human Development, 81(4), 217–240. 10.1177/0091415015621309 [DOI] [PubMed] [Google Scholar]
- Maydeu‐Olivares, A. (2017). Assessing the size of model misfit in structural equation models. Psychometrika, 82(3), 533–558. 10.1007/s11336-016-9552-7 [DOI] [PubMed] [Google Scholar]
- Mertens, G. , Gerritsen, L. , Duijndam, S. , Salemink, E. , & Engelhard, I. M. (2020). Fear of the coronavirus (COVID‐19): Predictors in an online study conducted in March 2020. Journal of Anxiety Disorders, 74, 102258. 10.1016/j.janxdis.2020.102258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mihara, S. , & Higuchi, S. (2017). Cross‐sectional and longitudinal epidemiological studies of internet gaming disorder: A systematic review of the literature. Psychiatry and Clinical Neurosciences, 71(7), 425–444. 10.1111/pcn.12532 [DOI] [PubMed] [Google Scholar]
- Montag, C. , Schivinski, B. , Sariyska, R. , Kannen, C. , Demetrovics, Z. , & Pontes, H. (2019). Psychopathological symptoms and gaming motives in disordered gaming: A psychometric comparison between the WHO and APA diagnostic frameworks. Journal of Clinical Medicine, 8(10), 1691. 10.3390/jcm8101691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montag, C. , & Walla, P. (2016). Carpe diem instead of losing your social mind: Beyond digital addiction and why we all suffer from digital overuse. Cogent Psychology, 3(1), 1157281. 10.1080/23311908.2016.1157281 [DOI] [Google Scholar]
- Montag, C. , Wegmann, E. , Sariyska, R. , Demetrovics, Z. , & Brand, M. (in press). How to overcome taxonomical problems in the study of internet use disorders and what to do with “smartphone addiction”? Journal of Behavioral Addictions. 10.1556/2006.8.2019.59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén, L. K. , & Muthén, B. O. (1998. –2019). Mplus user's guide (8th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Oosterhoff, B. , Palmer, C. A. , Wilson, J. , & Shook, N. (2020). Adolescents' motivations to engage in social distancing during the COVID‐19 pandemic: Associations with mental and social health. Journal of Adolescent Health, 67(2), 179–185. 10.1016/j.jadohealth.2020.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pontes, H. M. , Schivinski, B. , Sindermann, C. , Li, M. , Becker, B. , Zhou, M. , & Montag, C. (in press). Measurement and conceptualization of gaming disorder according to the World Health Organization framework: The development of the gaming disorder test. International Journal of Mental Health and Addiction. 10.1007/s11469-019-00088-z [DOI] [Google Scholar]
- Przybylski, A. K. , Murayama, K. , DeHaan, C. R. , & Gladwell, V. (2013). Motivational, emotional, and behavioral correlates of fear of missing out. Computers in Human Behavior, 29(4), 1841–1848. 10.1016/j.chb.2013.02.014 [DOI] [Google Scholar]
- R Core Team . (2020). R: A language and environment for statistical computing Vienna, Austria: R Foundation for Statistical Computing. Retrieved from https://www.R-project.org/. [Google Scholar]
- Ryding, F. C. , & Kuss, D. J. (2020). Passive objective measures in the assessment of problematic smartphone use: A systematic review. Addictive Behaviors Reports, 11, 100257. 10.1016/j.abrep.2020.100257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salkovskis, P. M. , Rimes, K. A. , Warwick, H. M. C. , & Clark, D. M. (2002). The health anxiety inventory: Development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychological Medicine, 32(5), 843–853. 10.1017/S0033291702005822 [DOI] [PubMed] [Google Scholar]
- Schimmenti, A. , Billieux, J. , & Starcevic, V. (2020). The four hoursemen of fear: An integrated model of understanding fear experiences during the COVID‐19 pandemic. Clinical Neuropsychiatry, 17(2), 41–45. 10.36131/CN20200202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sha, P. , Sariyska, R. , Riedl, R. , Lachmann, B. , & Montag, C. (2019). Linking internet communication and smartphone use disorder by taking a closer look at the Facebook and WhatsApp applications. Addictive Behaviors Reports, 9, 100148. 10.1016/j.abrep.2018.100148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi, D. , Maydeu‐Olivares, A. , & Rosseel, Y. (2020). Assessing fit in ordinal factor analysis models: SRMR vs. RMSEA. Structural Equation Modeling, 27(1), 1–15. 10.1080/10705511.2019.1611434 [DOI] [Google Scholar]
- Taylor, S. , Landry, C. A. , Paluszek, M. M. , Fergus, T. A. , McKay, D. , & Asmundson, G. J. G. (2020a). COVID stress syndrome: Concept, structure, and correlates. Depression and Anxiety, 37(8), 706–714. 10.1002/da.23071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor, S. , Landry, C. A. , Paluszek, M. M. , Fergus, T. A. , McKay, D. , & Asmundson, G. J. G. (2020b). Development and initial validation of the COVID Stress Scales. Journal of Anxiety Disorders, 72, 102232. 10.1016/j.janxdis.2020.102232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teng, C.‐I. (2018). Managing gamer relationships to enhance online gamer loyalty: The perspectives of social capital theory and self‐perception theory. Computers in Human Behavior, 79, 59–67. 10.1016/j.chb.2017.10.024 [DOI] [Google Scholar]
- Wang, J. , Mann, F. , Lloyd‐Evans, B. , Ma, R. , & Johnson, S. (2018). Associations between loneliness and perceived social support and outcomes of mental health problems: A systematic review. BMC Psychiatry, 18(1), 156. 10.1186/s12888-018-1736-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, J. , Wang, P. , Yang, X. , Zhang, G. , Wang, X. , Zhao, F. , … Lei, L. (2019). Fear of missing out and procrastination as mediators between sensation seeking and adolescent smartphone addiction. International Journal of Mental Health and Addiction, 17(4), 1049–1062. 10.1007/s11469-019-00106-0 [DOI] [Google Scholar]
- Wegmann, E. , Oberst, U. , Stodt, B. , & Brand, M. (2017). Online‐specific fear of missing out and internet‐use expectancies contribute to symptoms of internet‐communication disorder. Addictive Behaviors Reports, 5, 33–42. 10.1016/j.abrep.2017.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenham, C. , Smith, J. , & Morgan, R. (2020). COVID‐19: The gendered impacts of the outbreak. The Lancet, 395(10227), 846–848. 10.1016/s0140-6736(20)30526-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheaton, M. G. , Abramowitz, J. S. , Berman, N. C. , Fabricant, L. E. , & Olatunji, B. O. (2011). Psychological predictors of anxiety in response to the H1N1 (swine flu) pandemic. Cognitive Therapy and Research, 36(3), 210–218. 10.1007/s10608-011-9353-3 [DOI] [Google Scholar]
- Williams, K. D. (2007). Ostracism. Annual Review of Psychology, 58, 425–452. 10.1146/annurev.psych.58.110405.085641 [DOI] [PubMed] [Google Scholar]
- World Health Organization . (2019). Gaming disorder. ICD‐11. Retrieved from https://icd.who.int/browse11/l-m/en
- Xiao, H. , Zhang, Y. , Kong, D. , Li, S. , & Yang, N. (2020). Social capital and sleep quality in individuals who self‐isolated for 14 days during the coronavirus disease 2019 (COVID‐19) outbreak in January 2020 in China. Medical Science Monitor, 26, e923921. 10.12659/MSM.923921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan, G. , Elhai, J. , & Hall, B. J. (2021). The influence of depressive symptoms and fear of missing out on severity of problematic smartphone use and internet gaming disorder among Chinese young adults: A three‐wave mediation model. Addictive Behaviors, 112, 106648. 10.1016/j.addbeh.2020.106648 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Anonymized data used in this study may be requested from the second author, and provided upon reasonable request.


