Dear Editor,
The COVID‐19 pandemic necessitated a change in the role of medical students, with a shift to telemedicine and a temporary cessation of clinical rotations as recommended by the Association of American Medical Colleges (AAMC). 1 , 2 Here we offer an approach for medical student involvement that was piloted at the Yale School of Medicine as part of a broad outreach effort serving many clinical specialties.
Because of uncertainty regarding the risk of viral transmission in outpatient settings at the onset of the COVID‐19 pandemic, all nonurgent visits at our institution were transitioned to telemedicine. Transitioning outpatient clinics to virtual formats and rescheduling cancelled appointments was a significant undertaking that fell primarily on medical assistants. Medical students felt they could support both the medical assistants and the Department of Dermatology by assisting patients with the process of activating Epic MyChart, the HIPAA‐compliant platform used for telemedicine appointments. Students were particularly eager to support the dermatology continuity clinic, as it provides care to an underserved population insured by Medicaid.
Nine medical students who had completed at least one clinical clerkship developed the Teledermatology Student Task Force (TSTF) under the supervision of dermatology attendings and residents. The aim of this collaboration was to enhance the efficiency of care provision during the pandemic in the dermatology continuity clinic. Every patient (or proxy in the case of children) was called the week prior to the scheduled appointment to be offered a video visit. Utilizing a script developed collaboratively between residents and medical students, volunteers assisted patients with activation of Epic MyChart. For cases in which upper year dermatology residents deemed clinical images would be beneficial, volunteers helped patients upload photos in advance. TSTF volunteers ensured that patients understood the steps to prepare for MyChart visits, which require a smartphone or tablet to utilize the telemedicine video function (Figure 1).
Figure 1.
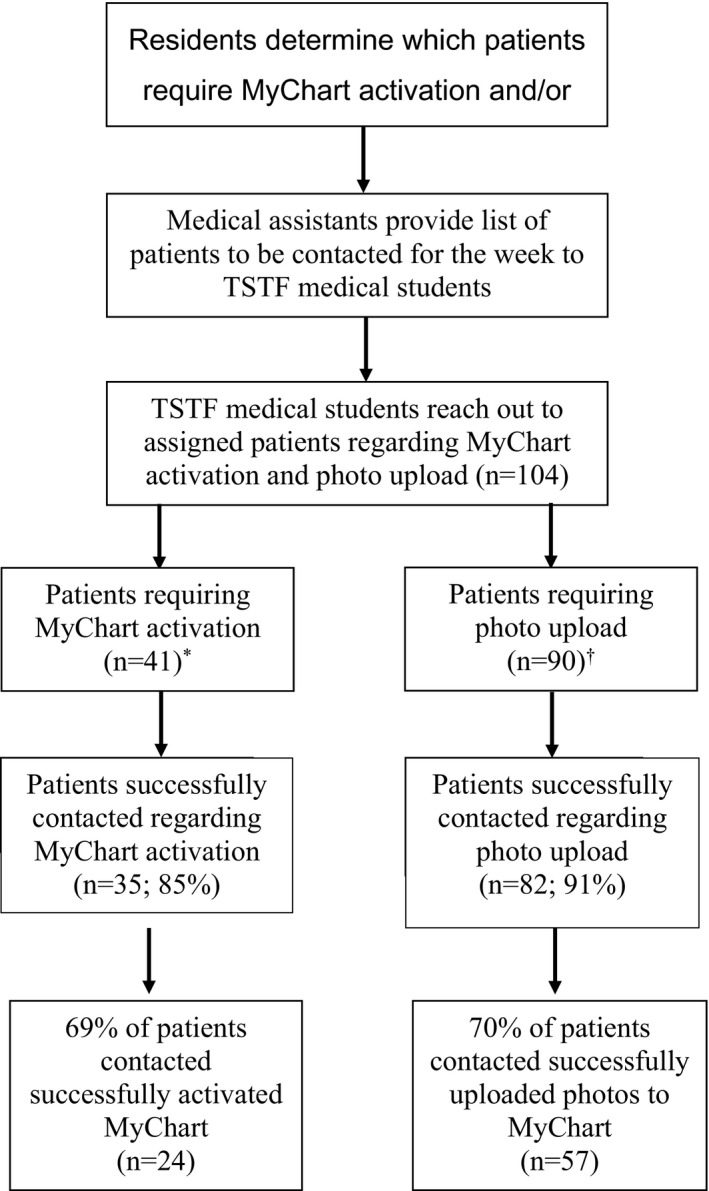
TSTF workflow from patient selection to medical student volunteer outreach. *36 patients required both MyChart activation and photo upload; 5 patients required MyChart activation only. †36 patients required both MyChart activation and photo upload; 54 patients required photo upload only
Over the 5‐week pilot (April 27–May 29, 2020), TSTF volunteers contacted 104 patients, including 55 pediatric and 49 adult patients. Forty‐one of the 104 total patients did not have an activated MyChart account at the time of outreach. TSTF volunteers were able to reach 35 of these patients, 69% of whom successfully activated their MyChart accounts in advance of their teledermatology appointments. Clinical images were requested for 90 of the 104 total patients. Eighty‐two of these patients were successfully reached, 70% of whom successfully uploaded images for their provider to review prior to video visits (Figure 1). Patients who did not require MyChart activation or photo upload were provided appointment instructions. Of the 87 patients, TSTF volunteers were able to successfully reach by phone, 93% reported that the outreach was helpful when asked at the conclusion of the call, and 78% successfully completed a video visit with their dermatologist.
The COVID‐19 pandemic has increased the administrative burden of dermatology clinics, necessitating the identification of novel strategies to optimize teledermatology. 3 Underserved populations may face disproportionate barriers when accessing telemedicine care and can benefit from dedicated coaching. Our experience underscores the potential for medical students to make a significant impact through supporting both patients and providers in the optimal use of telemedicine. Students also benefit from acquiring familiarity with telemedicine platforms and their limitations at a time when elements of clinical training are being transitioned to virtual settings nationwide. Furthermore, these skills will benefit students throughout their careers, as the utilization of telemedicine is likely to increase in the upcoming years. Given the importance of teledermatology during the COVID‐19 pandemic, this is an approach that can be replicated across institutions. Future directions of TSTF may include opportunities for volunteers to gain clinical exposure through direct participation in teledermatology visits.
Acknowledgments
We thank the student volunteers of the Teledermatology Student Task Force, as well as the faculty, residents, and medical assistants of the Department of Dermatology at Yale School of Medicine for their support.
Conflict of interest: SP: Clinical Advisor, Hims/Hers. AB, BO, RJA, IDO, MB, JMC: No conflicts.
Funding source: None.
References
- 1. Loh T, Hsiao JL, Shi VY. COVID‐19 and its impact on medical student education in dermatology. J Am Acad Dermatol 2020; 83: e163–e164. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Association of American Medical Colleges (AAMC) . Important Guidance for Medical Students on Clinical Rotations During the Coronavirus (COVID‐19) Outbreak. AAMC. 2020 March 17. https://www.aamc.org/news‐insights/press‐releases/important‐guidance‐medical‐students‐clinical‐rotations‐during‐coronavirus‐covid‐19‐outbreak#:~:text=%22The%20AAMC%20has%20issued%20new,until%20at%20least%20March%2031.
- 3. Gupta R, Ibraheim MK, Doan HQ. Teledermatology in the wake of COVID‐19: advantages and challenges to continued care in a time of disarray. J Am Acad Dermatol 2020; 83: 168–169; Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]


