Abstract
The present article examines how job demands and resources are related to indices of strain among healthcare professionals during virus pandemics. The article also presents the results of a study examining the relationships between COVID‐19 demands (e.g., lack of personal protective equipment, concerns about infecting family members), resources (meaningful work, social support), and mental health strain within a sample of emergency medicine personnel over six consecutive weeks. COVID‐19‐related demands and hours worked were hypothesized to be positively related to mental health strain, whereas meaningful work and social support were hypothesized to be negatively related to mental health strain. Hours worked the prior week were hypothesized to exacerbate the positive relationships between COVID‐19 demands and mental health strain, whereas the resources of meaningful work and social support were expected to buffer the relationships. Multilevel models controlling for mental health strain the prior week revealed that COVID‐19 demands, along with hours worked, were each related to higher mental health strain during the week. Hours worked magnified the within‐person relationship between personal COVID‐19 demands and mental health strain. In contrast to the hypotheses, social support and meaningful work were not related to mental health strain. Discussion focuses on the implications of the findings for healthcare professionals.
INTRODUCTION
The COVID‐19 pandemic has had dramatic effects on organizations and the ways employees work within organizations. Many individuals have lost their jobs as a result of the pandemic and many others have had to fundamentally alter the way they work. Healthcare professionals working on the frontlines to treat patients with COVID‐19 face the most immediate and potentially severe stressors associated with the pandemic. Reports in the media have highlighted extreme reactions to the demands associated with COVID‐19, including a physician committing suicide as a result of prolonged exposure to long work hours and an inability to help large numbers of patients (Romo, 2020). Researchers have also begun to examine the impact of the demands associated with COVID‐19 as predictors of health and well‐being among healthcare professionals (e.g., Preti, Di Mattei, Perego, Ferrari, Mazzetti, Taranto, Di Pierro, Madeddu, & Calati, 2020; Rodriguez, Medak, Baumann, Lim, Chinnock, Frazier, & Cooper, 2020). Understanding the mental health implications of COVID‐19 for frontline healthcare professionals is especially important given that before the onset of the COVID‐19 pandemic, burnout and well‐being already were spotlighted issues, with reports of up to 50 percent of physicians and 76 percent of residents experiencing burnout on a regular basis (Lin, Battaglioli, Melamed, Mott, Chung, & Robinson, 2019; Rotenstein, Torre, Ramos, Rosales, Guille, Sen, & Mata, 2018).
The present article has two primary goals. The first is to integrate the emerging research exploring mental health consequences of the COVID‐19 pandemic for healthcare professionals with prior studies examining similar issues regarding other virus epidemics and pandemics, such as the 2003 SARS epidemic. The Job Demands‐Resources (JD‐R) framework (Bakker & Demerouti, 2017) is used to understand prior research in this area and suggest directions for future research. In addition to addressing demands during virus outbreaks and pandemics, we also review prior research on the resources that may be effective in buffering healthcare professionals from the novel demands they may encounter in these contexts. Finally, we discuss gaps in the literature related to a lack of longitudinal designs, the failure to examine how demands and resources may interact to predict strain, and a lack of objective assessments of work demands.
The second goal of the article is to address these gaps in the literature by presenting a study examining different types of COVID‐19 demands as predictors of mental health strain among a sample of emergency medicine personnel addressing the current pandemic. Most of the research addressing virus epidemics and pandemics conducted with healthcare professionals has taken a between‐person approach, examining differences between medical professionals on indices of strain and work demands. The present research contributes to the under‐studied area of fluctuations in medical professionals’ strain over the course of multiple weeks addressing the pandemic and whether these fluctuations are predicted by COVID‐19 demands and resources.
A JD‐R APPROACH TO RESEARCH ON HEALTHCARE PROFESSIONALS DURING VIRUS PANDEMICS
A relatively large amount of research has been conducted on the mental health of healthcare professionals during virus epidemics, including the Severe Acute Respiratory Syndrome (SARS), Middle East Respiratory Syndrome (MERS), Ebola virus disease, influenza A virus subtype H1 N1, influenza A virus subtype H7 N9, and more recently, COVID‐19 (Kisely, Warren, McMahon, Dalais, Henry, & Siskind, 2020; Preti et al., 2020; Stuijfzand, Deforges, Sandoz, Sajin, Jaques, Elmers, & Horsch, 2020). From the standpoint of the JD‐R model, research conducted in this area is more focused on the strain outcomes for employees, including not only burnout, but also the presence or absence of different types of mental health problems. However, research in the area has also addressed the work demands and resources associated with the probability of mental health outcomes. In this section we provide an overview of the JD‐R model and then review research on the impact of virus epidemics on healthcare professionals within the context of the model.
Brief Overview of the Job Demands‐Resources Model
The Job Demands‐Resources (JD‐R) model is one of the most commonly applied models of work stress in occupational health psychology and is a useful framework for conceptualizing burnout and well‐being at multiple levels of analysis (Bakker & Demerouti, 2017). The JD‐R model posits that burnout and other adverse mental health outcomes are a function of both the job demands facing employees and the personal and job resources available to help employees meet those demands (Demerouti, Bakker, Nachreiner, & Schaufeli, 2001).
The job demands component of the model addresses those factors of work that require continuous amounts of physical, mental, or emotional effort. Sources of these demands can be found in physical aspects of the work environment (e.g., high levels of noise or crowding), social aspects of the work environment (e.g., interpersonal conflict, abusive supervision), or organizational aspects of the work environment (e.g., organizational constraints, time pressure). Chronic exposure to job demands creates a strain on employees through the continuous effort required to address the demands present in the work environment. One advantage of the JD‐R model over other models is the focus on broad categories of job demands that have the potential to apply to diverse organizational settings (Bakker & Demerouti, 2007).
The job resources of the model refer to those factors in the work environment that facilitate achievement of work‐related goals, help reduce job demands, or stimulate professional growth and development (Bakker & Demerouti, 2007). Resources can also come from various aspects of the work environment, including physical (e.g., mechanical assistance for lifting heavy equipment), psychological (e.g., positive feedback from supervisors), social (e.g., co‐worker support), or organizational (e.g., perceived support from the organization). The range of job resources included in the model also allows the JD‐R model to be applied to diverse organizational settings. Furthermore, the inclusion of personal resources within the model (e.g., self‐efficacy, optimism, hardiness) further expands the ability of the model to account for a variety of factors that reduce the probability of burnout and other mental health problems (Xanthopoulou, Bakker, Demerouti, & Schaufeli, 2007).
As noted by Bakker and Demerouti (2017), there is a large amount of support for key propositions of the JD‐R model. Given that the focus of the present research is on how virus‐related work demands are associated with strain among healthcare professionals, we are primarily focused on the health‐impairment process, where the presence of job demands creates strain on the employee, with indicators of strain including burnout, anxiety, and other health problems (Bakker & Demerouti, 2007). Figure 1 highlights the health‐impairment component of the model applied to virus outbreaks. In addition to the direct links between job demands and resources on strain, the model also posits that job resources have the capacity to moderate the job demands‐strain relationship (i.e. high resources can reduce the negative impact of job demands).
FIGURE 1.
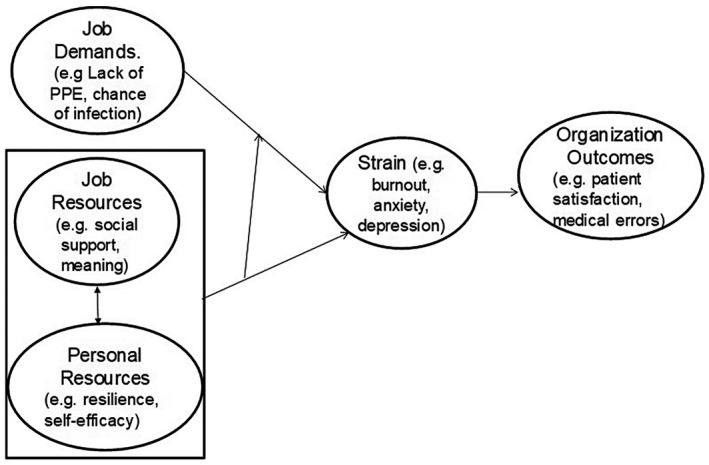
The job demands‐resources model (health‐impariment component) applied to healthcare professionals during virus epidemics.
Research on Healthcare Professionals during Virus Pandemics within the JD‐R Model
In illustrating how the JD‐R model can be used to better understand and organize the research conducted with healthcare professionals working within virus epidemics and pandemics, we start by reviewing the job and personal resources that have been linked to reduced strain among healthcare professionals during these events. We then discuss elements of the JD‐R model that have not been tested among healthcare professionals during virus epidemics, including examining job demands and resources as predictors of strain within healthcare professionals over time and the simultaneous examination of multiple demands and resources as predictors of strain.
Job Demands during Virus Epidemics
In addition to traditional work stressors such as long work hours, high levels of workload, and time pressure, healthcare professionals also face unique physical demands associated with potentially being infected by the virus (Kisely et al., 2020) and having to treat patients while wearing personal protective equipment (PPE) that may not only harm effective communication with the patient (Maunder, 2009), but also can create headaches and damage skin when worn for long periods of time (Goh, Ong, Bharatendu, Tan, & Sharma, 2020; Kantor, 2020). Furthermore, healthcare professionals are faced with the demand of potentially infecting family members or loved ones who may be at risk for severe complications from the illness (Kang et al., 2020). Researchers examining strain among healthcare professionals during virus epidemics characterize these types of job demands as risk factors for a greater likelihood of the healthcare professional developing a mental health problem.
Among studies examining demands facing healthcare professionals during prior virus epidemics and pandemics, the degree of contact with infected patients has emerged as the most consistent correlate of adverse mental health consequences (Kisely et al., 2020; Preti et al., 2020; Stuijfzand et al., 2020). Exposure to infected patients has been assessed in multiple ways, including dichotomously as either having or not having contact with infected patients, amount of contact rated on a continuous scale, and even being diagnosed with the virus or not. Maunder, Lancee, Balderson, Bennett, Borgundvaag, Evans, Fernandes, Goldbloom, Gupta, Hunter, and Wasylenki (2006) found higher levels of burnout in healthcare providers exposed to the SARS virus in comparison to those not exposed. Marjanovic, Greenglass, and Coffey (2007) found that degree of contact with infected patients was a predictor of emotional exhaustion during the SARS virus epidemic. Healthcare professionals diagnosed with the virus during the SARS epidemic were also more likely to meet diagnostic criteria for post‐traumatic stress disorder 30 months following the pandemic (Mak, Chu, Pan, Yiu, & Chan, 2009). Degree of exposure to infected patients would be classified as a job demand stemming from the physical aspects of the workplace.
Additional job demands linked to strain‐related outcomes include healthcare professionals having to be quarantined during the epidemic/pandemic and the length of time of the quarantine (Brooks, Dunn, Amlôt, Rubin, & Greenberg, 2018; Kisely et al., 2020; Preti et al., 2020). Wu, Liu, Fang, Fan, Fuller, Guan, and Litvak (2008) and Wu, Fang, Guan, Fan, Kong, Yao, Liu, Fuller, Susser, Lu, and Hoven (2009) found those hospital employees quarantined as a result of the SARS virus reported higher post‐traumatic stress symptoms and greater consumption of alcohol. In their study of nurses during the SARS epidemic, Marjanovic et al. (2007) also found that time spent in quarantine was positively correlated with emotional exhaustion, anger, and avoidance behavior. The job demand of “being quarantined” likely encapsulates a number of factors related to lack of job and personal control, as well as perceptions of injustice.
Related to quarantine resulting in a lack of job control, prior research has also examined more traditional work‐related stressors as predictors of strain‐related outcomes during virus epidemics. Tam, Pang, Lam, and Chiu (2004) combined multiple work‐related demands into a single index of “Work Factor” source of stress, including heavy workload, hazardous work environment, unclear job instructions, ambiguous infection control policies, lack of feedback, being blamed for mistakes, and lack of appreciation for work. The authors also combined other sources of stress into an index they labelled “Personal Factor.” This index included demands such as risk to own health, interference with home life, and risk of infecting relatives/friends. The authors found both stress factors were associated with a greater likelihood of psychiatric morbidity on the General Health Questionnaire (GHQ).
In terms of job demands examined in more recent studies of healthcare professionals during the COVID‐19 pandemic, Rodriguez et al. (2020) examined a number of work‐related demands related to COVID‐19 among a sample of emergency physicians, with the most frequently endorsed demands being inadequate PPE, inability to accurately diagnose COVID‐19, and exposing family members or others to the virus because of their work. The authors did not examine the link between these demands and indices of strain. Morgantini, Naha, Wang, Francavilla, Acar, Flores, Crivellaro, Moreira, Abern, Eklund, Vigneswaran, and Weine (2020) examined the determinants of burnout during COVID‐19 for a large sample of healthcare professionals (N = 2,707) from over 60 countries. Consistent with broader research on virus epidemics, the strongest predictors of burnout were work affecting household activities, exposure to COVID‐19 patients, and having to make life prioritizing decisions in treatment. Furthermore, lack of adequate PPE was also related to burnout. Sharma, Creutzfeldt, Lewis, Patel, Hartog, Jannotta, Blissitt, Kross, Kassebaum, Greer, Curtis, and Wahlster (2020) also found that lack of PPE and concerns of infecting family members with the COVID‐19 virus were predictive of burnout in a large sample of healthcare professionals.
Job and Personal Resources in Virus Epidemics
Research on healthcare professionals during virus epidemics has also identified a number of personal and job resources that are linked to lower levels of strain, identified as protective resources in most of the studies. Although personal and job resources are hypothesized to have a reciprocal relationship with one another in the JD‐R model (Bakker & Demerouti, 2017), these resources are largely examined individually in research on virus epidemics.
Job Resources
Across the different virus epidemics, the job resources most consistently associated with reports of strain included the provision of adequate PPE, as well as supervisor and co‐worker support (Kisely et al., 2020; Preti et al., 2020; Stuijfzand et al., 2020). The provision of PPE is critical for employees given that it targets the primary demands associated with potentially contracting the virus and thereby infecting friends and family members. Khalid, Khalid, Qabajah, Barnard, and Qushmaq (2016) examined healthcare professionals during the MERS‐CoV epidemic and found that strict protective measures accompanied by adequate PPE was a highly endorsed resource for addressing the demands of the pandemic. More recently, during the COVID‐19 pandemic, researchers examining healthcare professionals in Wuhan, China, found that coverage of departments with protective measures was linked to reduced likelihood of screening positive for depression or anxiety (Zhu, Xu, Wang, Liu, Wu, Li, Miao, Zhang, Yang, Sun, & Zhu, 2020).
Many studies of hospital employees during virus epidemics have also emphasized the importance of social support (Brooks et al., 2018; Kisely et al., 2020). Co‐worker and supervisor support have been identified as important job resources in broader research on organizational stress (Cooper, Dewe, & O’Driscoll, 2001). A supportive work environment was emphasized as a protective factor in studies of healthcare personnel during the Ebola crisis (Belfroid, van Steenbergen, Timen, Ellerbroek, Huis, & Hulscher, 2018), and supportive supervisors and colleagues were associated with a reduced risk of psychiatric symptoms among hospital workers during the SARS pandemic (Chan & Huak, 2004). Grace, Hershenfield, Robertson, and Stewart (2005) found that when hospital personnel were asked to indicate the best aspects of working during the SARS epidemic, the most frequently mentioned factor was staff collegiality (28.5%).
The job resource of perceived organizational support has also been linked to the reduced probability of new‐onset psychiatric disorders among hospital employees who worked during the SARS epidemic in Toronto (Lancee, Maunder, & Goldbloom, 2008). Tam et al. (2004) also found that the availability of counseling and support from the employer were associated with a reduced likelihood of a positive screening for a problem as indicated by the GHQ. In their review of factors associated with psychological outcomes among employees during virus epidemics, Brooks et al. (2018) also identified organizational support as an important resource for healthcare professionals.
Adequate communication regarding issues related to the virus epidemic is another job resource that has been associated with lower perceptions of strain among healthcare professionals. Matsuishi et al. (2012) examined hospital workers during the H1 N1 influenza epidemic in Japan and found that employees were less likely to feel unprotected when they received more frequent communication regarding the pandemic. Clear communication of hospital directives and precautions being taken was also linked to fewer symptoms as assessed by the GHQ in a sample of hospital workers during the SARS epidemic (Chan & Huak, 2004; see also Tam et al., 2004).
Personal Resources
Although personal resources are less examined within pandemics than job resources, researchers have identified personal traits and coping mechanisms that are associated with reduced reports of strain. Self‐efficacy has emerged as an important resource for employees during virus pandemics, as being confident in one's ability to perform during the pandemic has been linked to reduced reports of strain (Kisely et al., 2020; Preti et al., 2020). Additional personal resources examined as predictors of reduced strain during pandemics include personality hardiness (Park, Lee, Park, & Choi, 2018), lower use of maladaptive coping strategies (Maunder et al., 2006), and greater use of adaptive coping strategies (Cai, Zheng, Huang, Zhang, Qiu, Huang, & Wu, 2020).
Research Gaps in Understanding Healthcare Professionals’ Psychological Functioning During Virus Pandemics
Virtually all research conducted with healthcare professionals during virus epidemics and pandemics has focused on identifying individual predictors of mental health symptoms and well‐being. The research has also largely been conducted by medical and public health researchers, with a focus on identifying individual risk and protective factors associated with various indicators of strain (Brooks et al., 2018; Kisely et al., 2020; Morgantini et al., 2020; Stuijfzand et al., 2020). Although research on individual predictors of strain among healthcare professionals during virus epidemics is important, additional research is needed to examine how different demands and resources might interact with one another to predict strain.
In addition, the presence of existing work demands among healthcare professionals may exacerbate the effects of virus‐related demands. Emergency medicine personnel (EMP) encounter an array of stressors in the workplace, including high workload, overcrowding, and excessive bureaucratic tasks that are often considered illegitimate (Schneider & Weigl, 2018; Semmer et al., 2015). The presence of virus‐related demands on top of these existing work demands may magnify the mental health strain among providers. Therefore, it is important to examine how traditional work demands, such as working long hours, may exacerbate the effects of virus‐related demands on mental health symptoms.
A second gap in the literature involves the exclusive reliance on between‐participants research designs, where differences between healthcare professionals on some risk or protective factor are examined as predictors of different indices of strain between healthcare professionals. No research we are aware of has examined variations in mental health functioning within healthcare professionals over a period of time during any of the virus epidemics or pandemics. This lack of research examining predictors of fluctuations in mental health functioning over time is surprising, given the demonstrated ebbs and flows in the magnitude of individuals suffering from viruses during epidemics (Reich, Brooks, Fox, Kandula, McGowan, Moore, Osthus, Ray, Tushar, Yamana, Biggerstaff, Johansson, Rosenfeld, & Shaman, 2019). Addressing how COVID‐19 demands and resources are related to mental health strain over multiple weeks would contribute to our understanding of mental health functioning of healthcare professionals during virus epidemics and pandemics.
A third gap in research on virus‐related work demands as predictors of strain among healthcare professionals is an exclusive reliance on self‐report measures to assess the work demands that are experienced by healthcare professionals. Although self‐report measures of work demands are a valid assessment technique, additional objective work demands should be assessed, including the number of hours worked by healthcare professionals addressing the virus‐related pandemic or the number of patients seen by providers who may be contagious with a particular virus. In our empirical study we examine hours worked per week as both a predictor of mental health strain among emergency medicine personnel (EMP) and a moderator of the relationships between COVID‐19 demands and mental health strain.
COVID‐19 Demands and Resources as Predictors of Fluctuations in Mental Health Strain among Emergency Medicine Professionals
The present study was designed to address these gaps in prior research by examining EMP who were treating potential COVID‐19 positive patients over the course of 6 weeks during the pandemic as it began spreading in the United States. EMP are at the forefront of the COVID‐19 pandemic and are the initial healthcare professionals confronted with positive cases who are experiencing symptoms severe enough for them to go to the emergency room (Rodriguez et al., 2020). Therefore, this specific group of healthcare professionals provides a unique and important sample for investigating how changes in demands and resources are linked to changes in mental health strain across multiple weeks of the pandemic.
The current study was part of a process improvement effort already underway at a large non‐profit academic health organization. Participants responded to an assessment of mental health strain (Dyrbye, Satele, Sloan, & Shanafelt., 2013), COVID‐19 specific demands present in the workplace (e.g., lack of PPE; Tam et al., 2004), COVID‐19‐related personal demands associated with work (e.g., concern with getting infected; Tam et al., 2004), and resources related to social support (Preti et al., 2020) and meaningful work (Britt, Adler, & Bartone, 2001).
In addition to the assessment of these constructs via self‐report, the number of hours personnel worked each week were assessed from an administrative database to provide an objective index of workload. These demands were assessed both as predictors of mental health strain as well as moderators of the relationships between the COVID‐19 demands and mental health strain. Schneider and Weigl (2018) have detailed the numerous stressors facing EMP under non‐pandemic conditions. Existing demands related to workload such as work hours have the potential to magnify the effects of pandemic‐related work demands.
Based on the JD‐R model and prior between‐person research on correlates of strain among healthcare professionals during virus epidemics, the following hypotheses were made:
Hypotheses 1(a), 1(b), and 1(c): COVID‐19 job demands, COVID‐19 personal demands, and hours worked will each be predictive of weekly mental health strain while controlling for prior week mental health strain.
Hypotheses 2(a) and 2(b): Hours worked the prior week will magnify the relationships between COVID‐19 job demands and COVID‐19 personal demands with mental health strain.
Hypotheses 3(a) and 3(b): Social support and meaningful work will each be predictive of weekly mental health strain while controlling for prior week mental health strain.
Hypotheses 4(a) and 4(b): Social support and meaningful work will buffer the relationship between COVID‐19 personal demands and mental health strain.
Hypotheses 5(a) and 5(b): Social support and meaningful work will buffer the relationship between COVID‐19 job demands and mental health strain.
METHOD
Participants
The sample included emergency medicine attending physicians, advanced practice providers (APPs), and residents working across seven emergency departments and urgent care locations. This survey‐based effort was originally designed to provide department leadership with regular feedback using brief assessments measuring the burnout and well‐being of EMP at an academic health center in southeastern United States. The weekly survey was distributed to a total of 226–229 EMP over the course of 6 consecutive weeks. As the survey progressed, personnel changes (e.g., resignations, new hires) resulted in slightly different distribution numbers each week to ensure all currently employed personnel were invited.
Survey response rates ranged from 30–40 percent over the course of the 6 weeks. To qualify for inclusion in the current study, participants must have completed at least 2 of the 6 weekly surveys. A total of 97 clinicians were included in the final analyses (60.8% male, 39.2% female, 80.4% White, aged 27–70 [M = 40], 56 attending physicians, 26 APPs, 15 residents). Of this total sample, 15 clinicians completed 2 surveys, 20 clinicians completed 3 surveys, 18 clinicians completed 4 surveys, 21 clinicians completed 5 surveys, and 23 clinicians completed all 6 surveys. The combined dataset represented a total of 405 weekly assessments.
Measures
The weekly survey required brief measures that were easy to complete from a computer or mobile device. Therefore, checklists were primarily used to assess the constructs of interest, as has been done in similar studies of healthcare professionals during prior virus epidemics and the COVID‐19 pandemic (e.g., Schecter, Pham, Hua, Spinazzola, Sonnenklar, Li, & Milanaik, 2020; Wu et al., 2009). Total scores on the checklists are best considered formative constructs that assess the total amount of strain, demands, and resources present on a given week.
Mental Health Strain
The survey designed and administered for the present research included an adapted 7‐item version of the Mayo Clinic Physician Well‐Being Index (PWBI), for which prior research has established construct and criterion validity and reliability (Dyrbye et al., 2013). Specifically, in the current survey the first item in the 7‐item PWBI, “Have you felt burned out from your work?” was omitted and instead included the single item burnout measure from the Mini Z burnout measure (Dolan, Mohr, Lempa, Joos, Fihn, Nelson, & Helfrich, 2015). Given that all items in the measure assess strain‐related mental health issues (e.g., depression, anxiety, fatigue), for the present article we use the term mental health strain to describe scores on this measure. Therefore, the sum of the items resulted in a mental health strain score ranging from 0 (low mental health strain) to 7 (high mental health strain).
COVID‐19 Work and Personal Demands
Checklists were also utilized to assess the presence versus absence of different COVID‐19 related demands during the past week. Demands were identified from prior research examining healthcare worker demands during the 2003 SARS virus epidemic (Brooks et al., 2018; Maunder et al., 2006; Tam et al., 2004). Consistent with the research by Tam et al. (2004), two subscales were created based on COVID‐19 work demands and personal demands.
COVID‐19 job demands included 17 items that addressed stressors unique to the pandemic in the workplace (e.g., “shortage of personal protective equipment,” “shortage of medications needed to treat patients,” “feeling ill‐prepared to manage escalating work demands”). COVID‐19 personal demands included 10 items that addressed concerns unique to the pandemic related to personal health risks and the health of others (e.g., “fear of getting sick and/or dying myself,” “fear of my loved ones getting sick and/or dying,” “concern that my colleagues will get sick”). Participants selected the demands they reported experiencing during the week prior to completing the survey.
Hours Worked
Hours worked during the week prior to the survey were assessed through the Emergency Department's shift administration database. Hours worked included time spent working with patients in the emergency department and did not include vacation time.
COVID‐19 Resources
Participants were provided a checklist of different resources that had been helpful during the past week derived from prior research (Carver, 1997). For the present study, we summed four items that assessed the resource of social support (e.g., “support from my coworkers on shift,” “support from supervisors,” “regular social interactions with friends”) and four items that assessed the resource of meaningful work (e.g., “feeling that my work is meaningful,” “knowing I am helping to address the COVID‐19 pandemic”; Ben‐Itzhak, Dvash, Maor, Rosenberg, & Halpern, 2015). Participants selected the resources they identified as being helpful to them during the week immediately preceding the survey.
Procedure
As part of the process improvement effort for which this data were initially collected, emergency medicine leadership endorsed and served as champions encouraging participation in the survey at weekly town hall meetings and via email announcements. Participants also were informed that they would receive a small incentive (a $5 gift card) each time they participated in the weekly survey. All EMP in the department received a personalized survey link via email on Tuesday morning of each week and were given approximately 48 hours to submit their responses. Participants received their mental health strain score immediately upon completion of the online survey. Six weekly assessments were conducted (March 25–April 30, 2020) in total, with the first survey launching early in the COVID‐19 pandemic for the geographic region of the United States where the study was conducted, prior to the first COVID‐19‐related death in the area.
Analytic Approach
Multilevel models were used to test all hypotheses (Raudenbush & Bryk, 2002; Snijders & Bosker, 2012). While conventional univariate repeated measures analyses in the general linear model requires complete data across all measurement waves, multilevel models can be used when there is missing data on some measurement waves (Raudenbush & Bryk, 2002; Snijders & Bosker, 2012). All models were conducted using participants’ individual mental health strain index scores from the prior week to control for autoregressive effects (Beal & Weiss, 2003). Intercepts were included as random effects, given the strength of the relationship between the prior mental health strain control variable and current mental health strain. COVID‐19 work demands, COVID‐19 personal demands, weekly number of hours worked, social support, and meaningful work were examined as predictors of mental health strain within EMP. Within‐person interactions were estimated to examine whether hours worked magnified the relationships between COVID‐19 demands and mental health strain. Finally, within‐person interactions between the resources of social support and meaningful work and COVID‐19 demands were also estimated to examine whether these resources buffered the relationships between COVID‐19 demands and mental health strain.
The data for the current study were analyzed using R (R Core Team, 2020) and the nlme package (Pinheiro, Bates, DebRoy, Sarkar, & the R Development Core Team, 2013). Specifically, multilevel models were estimated using the lme function. For all models, restricted maximum likelihood was used for parameter estimation. Statistical inferences involving random effects were conducted using the likelihood ratio test while statistical inferences involving fixed effects were conducted using approximations to the t distribution (Pinheiro & Bates, 2000). For all models, residual analyses indicated that estimated errors were approximately normal (Fox, 2016) and heteroscedastic (Rosopa, Schaffer, & Schroeder, 2013). While there exist multiple approaches of calculating a pseudo‐coefficient of determination (R 2) in multilevel models (e.g., based on deviance or based on likelihoods), we calculated the marginal pseudo‐R 2 by Nakagawa and Schielzeth (2013), which is based on variance explained due to fixed effects. For all analyses, the Type I error rate was set at 0.05. Below are the results of the intraclass correlation coefficients (ICC), demands as predictors of mental health strain, and resources as predictors of mental health strain.
RESULTS
Intraclass Correlation Coefficients and Correlations among the Measured Variables
The ICCs (Shrout & Fleiss, 1979) or cluster effects (Raudenbush & Bryk, 2002; Snijders & Bosker, 2012) were calculated for all study variables to examine the degree of between‐person variance relative to total variance, which includes both between‐person and within‐person variance. The ICC for mental health strain was .64, indicating a relatively large between‐person influence, but still a significant amount of within‐person variability (Bobak, Barr, & O’Malley, 2018; Koo & Li, 2016). The ICCs for COVID‐19 job demands and COVID‐19 personal demands were .58 and .65, respectively, again indicating a relatively large between‐person influence, but still significant variability within participants (Bobak et al., 2018; Koo & Li, 2016). The ICC for hours worked was .40, indicating a lesser influence of the participant and greater variability within participants (Bobak et al., 2018; Koo & Li, 2016). Lastly, the ICCs for the resources of social support and meaningful work were .43 and .45, respectively, indicating moderate levels of both between‐person and within‐person variability (Bobak et al., 2018; Koo & Li, 2016).
Table 1 presents the descriptive statistics and within‐person correlation coefficients among the study variables. There was a positive correlation between social support and meaningful work. The correlations between COVID‐19 work demands and personal demands with mental health strain was positive and statistically significant, suggesting that as COVID‐19 demands increase, mental health strain increases.
TABLE 1.
Within‐Person Correlations among Study Variables
| Measures | M | SD | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|---|
| 1. COVID‐19 Job Demands | 4.96 | 2.84 | – | ||||
| 2. COVID‐19 Personal Demands | 3.96 | 1.97 | 0.30*** | – | |||
| 3. Hours Worked | 21.46 | 15.74 | 0.12 | 0.22** | – | ||
| 4. Social Support | 1.98 | 1.00 | −0.06 | 0.03 | 0.09 | – | |
| 5. Meaningful Work | 2.51 | 1.09 | 0.07 | −0.09 | 0.06 | 0.19** | – |
| 6. Mental Health Strain | 1.84 | 1.62 | 0.27*** | 0.29*** | 0.03 | −0.01 | −0.04 |
Abbreviations: M, mean; SD, standard deviation.
p < .01 (two‐tailed);
p < .001 (two‐tailed).
Job and Personal Demands as Predictors of Mental Health Strain
As noted above, the nlme package in R was used. Individual predictors of weekly mental health strain were examined after controlling for the prior weekly assessment of mental health strain. Random intercepts for participants were included in all models. Note that two types of analyses were conducted. First, as predictors of mental health strain, we examined each focal predictor with the control variable, separately. Second, we estimated an overall model that included COVID‐19 job demands, COVID‐19 personal demands, and hours worked, with the control variable. While the first analytic approach examined the marginal effects of each focal predictor, the second approach focused on the conditional effects of each predictor (i.e. in the presence of other demands and workload).
Covid‐19 Demands and Hours Worked
Table 2 provides a summary of the multilevel models for the two COVID‐19 demands and hours worked as individual predictors of mental health strain. COVID‐19 job demands and COVID‐19 personal demands were both positively related to perceptions of mental health strain during the week, controlling for mental health strain measured the prior week. Specifically, as COVID‐19 job demands increased one unit, mental health strain scores increased 0.07 units, and as COVID‐19 personal demands increased one unit, mental health strain scores increased 0.15 units. In terms of the objective indicator of workload during the pandemic, hours worked the prior week were positively related to participants’ mental health strain the following week. Specifically, as hours increased one unit, mental health strain scores increased 0.01 units.
TABLE 2.
COVID‐19 Job Demands, COVID‐19 Personal Demands, and Hours Worked as Individual Predictors of Emergency Medicine Personnel's Mental Health Strain
| B | SE | t | p | 95% CI | ||
|---|---|---|---|---|---|---|
| LL | UL | |||||
| Hypothesis 1(a) | ||||||
| MHS Control | 0.72 | 0.04 | 16.08 | .001*** | 0.63 | 0.81 |
| COVID‐19 Job Demands | 0.07 | 0.03 | 2.75 | .007** | 0.02 | 0.13 |
| Hypothesis 1(b) | ||||||
| MHS Control | 0.68 | 0.05 | 14.71 | .001*** | 0.59 | 0.77 |
| COVID‐19 Personal Demands | 0.15 | 0.04 | 4.04 | .001**** | 0.08 | 0.22 |
| Hypothesis 1(c) | ||||||
| MHS Control | 0.68 | 0.06 | 12.19 | .001*** | 0.57 | 0.79 |
| Hours Worked | 0.01 | 0.01 | 2.02 | .046* | 0.00 | 0.02 |
The mental health strain control variable controlled for participants’ mental health strain from the prior week. The marginal pseudo‐R 2 values for the three models testing Hypothesis 1(a), 1(b), and 1(c), respectively, were .57, .57, and .50.
Abbreviations: B, slope; CI, confidence interval; LL, lower level of the 95% CI; MHS, mental health strain; p, significance value; SE, standard error; t, t approximation; UL, upper level of the 95% CI.
p < .05 (two‐tailed);
p < .01 (two‐tailed);
p < .001 (two‐tailed).
Table 3 provides a summary of the multilevel model including both COVID‐19 demands (i.e. job and personal) and hours worked, controlling for mental health strain measured the prior week. When all variables were in the model, COVID‐19 personal demands and hours worked (marginally) have a significant effect on mental health strain. Overall, there was support for Hypothesis 1(b). There was partial support for Hypotheses 1(a) and 1(c).
TABLE 3.
A Single Model of COVID‐19 Job Demands, COVID‐19 Personal Demands, and Hours Worked as Predictors of Emergency Medicine Personnel's Mental Health Strain
| B | SE | t | p | 95% CI | ||
|---|---|---|---|---|---|---|
| LL | UL | |||||
| Mental Health Strain Control | 0.54 | 0.06 | 8.77 | .001*** | 0.42 | 0.66 |
| COVID‐19 Job Demands | 0.05 | 0.04 | 1.15 | .253 | −0.03 | 0.13 |
| COVID‐19 Personal Demands | 0.16 | 0.06 | 2.81 | .006** | 0.05 | 0.27 |
| Hours Worked | 0.01 | 0.00 | 1.91 | .060 | −0.00 | 0.02 |
The mental health strain control variable controlled for participants’ mental health strain from the prior week. The marginal pseudo‐R 2 value for the model was .51.
Abbreviations: B, slope; CI, confidence interval; LL, lower level of the 95% CI; MHS, mental health strain; p, significance value; SE, standard error; t, t approximation; UL, upper level of the 95% CI.
p < .01 (two‐tailed);
p < .001 (two‐tailed).
Interactions between COVID‐19 Demands and Workload
Results for the multilevel models examining the interactions between hours worked and the two COVID‐19 demands are provided in the first two sections of Table 4. All predictors were group mean centered (i.e. centered within person) before interaction terms were created (Aguinis, Gottfredson, & Culpepper, 2013; Enders & Tofighi, 2007). Hours worked the prior week interacted with COVID‐19 personal demands to predict mental health strain. The interaction is plotted in Figure 2 and indicates that the relationship between COVID‐19 personal demands and mental health strain was magnified when participants had worked more hours the week prior to the assessment. That is, as COVID‐19 personal demands increased, mental health strain increased. However, this relationship became stronger as hours worked the prior week increased. Thus, Hypothesis 2(b) was supported. However, hours worked the prior week did not interact with COVID‐19 job demands to predict participants’ mental health strain; thus, Hypothesis 2(a) was not supported.
TABLE 4.
Interactions among Study Variables
| B | SE | t | p | 95% CI | ||
|---|---|---|---|---|---|---|
| LL | UL | |||||
| Hypothesis 2(a) | ||||||
| Mental Health Strain Control | 0.68 | 0.06 | 12.02 | .001*** | 0.57 | 0.79 |
| COVID‐19 Job Demands (JD) | 0.11 | 0.05 | 2.09 | .039* | 0.01 | 0.21 |
| Hours Worked | 0.01 | 0.01 | 1.43 | .157 | −0.00 | 0.03 |
| COVID‐19 JD × Workload | 0.00 | 0.01 | 0.71 | .478 | −0.01 | 0.01 |
| Hypothesis 2(b) | ||||||
| Mental Health Strain Control | 0.68 | 0.06 | 12.15 | .001*** | 0.57 | 0.79 |
| COVID‐19 Personal Demands (PD) | 0.12 | 0.08 | 1.46 | .148 | −0.04 | 0.28 |
| Hours Worked | 0.01 | 0.01 | 1.24 | .219 | −0.01 | 0.03 |
| COVID‐19 PD × Workload | 0.02 | 0.01 | 2.78 | .007** | 0.01 | 0.03 |
| Hypothesis 4(a) | ||||||
| Mental Health Strain Control | 0.75 | 0.05 | 16.11 | .001*** | 0.66 | 0.85 |
| COVID‐19 Personal Demands (PD) | 0.13 | 0.07 | 1.77 | .079 | −0.02 | 0.27 |
| Social Support | 0.04 | 0.12 | 0.34 | .732 | −0.20 | 0.28 |
| COVID‐19 PD × Social Support | −0.01 | 0.09 | −0.08 | .933 | −0.20 | 0.18 |
| Hypothesis 4(b) | ||||||
| Mental Health Strain Control | 0.70 | 0.05 | 13.06 | .001*** | 0.60 | 0.81 |
| COVID‐19 Personal Demands (PD) | 0.13 | 0.08 | 1.69 | .094 | −0.02 | 0.28 |
| Meaningful Work | 0.14 | 0.12 | 1.15 | .254 | −0.10 | 0.37 |
| COVID‐19 PD × Meaningful Work | 0.02 | 0.11 | 0.15 | .883 | −0.21 | 0.24 |
| Hypothesis 5(a) | ||||||
| Mental Health Strain Control | 0.76 | 0.05 | 16.45 | .001*** | 0.67 | 0.85 |
| COVID‐19 Job Demands (JD) | 0.06 | 0.05 | 1.26 | .212 | −0.03 | 0.16 |
| Social Support | 0.06 | 0.12 | 0.46 | .643 | −0.19 | 0.30 |
| COVID‐19 JD × Social Support | 0.06 | 0.06 | 1.01 | .316 | −0.06 | 0.19 |
| Hypothesis 5(b) | ||||||
| Mental Health Strain Control | 0.71 | 0.05 | 13.33 | .001*** | 0.60 | 0.81 |
| COVID‐19 Job Demands (JD) | 0.11 | 0.05 | 2.16 | .033* | 0.01 | 0.21 |
| Meaningful Work | 0.08 | 0.12 | 0.67 | .507 | −0.16 | 0.32 |
| COVID‐19 JD × Meaningful Work | −0.02 | 0.08 | −0.28 | .782 | −0.17 | 0.13 |
The marginal pseudo‐R 2 values for the models testing Hypothesis 2(a) and 2(b), respectively, were .52 and .53. The marginal pseudo‐R 2 values for the models testing Hypothesis 4(a) and 4(b), respectively, were .56 and .50. The marginal pseudo‐R 2 values for the models testing Hypothesis 5(a) and 5(b), respectively, were .57 and .51.
Abbreviations: B, slope; CI, confidence interval; LL, lower level of the 95% CI; p, significance value; SE, standard error; t, t approximation; UL, upper level of the 95% CI.
p < .05 (two‐tailed);
p < .01 (two‐tailed);
p < .001 (two‐tailed).
FIGURE 2.
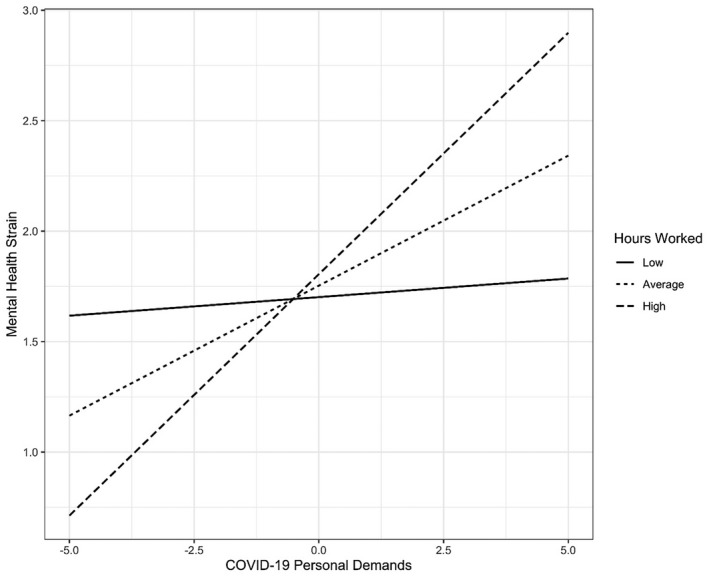
The interaction between COVID‐19 personal demands and hours worked the prior week as predictors of emergency medicine personnel's mental health strain.
Resources as Predictors of Mental Health Strain
As seen in Table 5, the resources of social support and meaningful work were not predictive of mental health strain over the course of 6 weeks. Note that a model that included both resources in the same model yielded similar results. Thus, Hypotheses 3(a) and 3(b) were not supported. The bottom four sections of Table 4 provide the results of multilevel models of social support and meaningful work as moderators of the relationships between COVID‐19 personal and job demands and mental health strain. None of the interactions were statistically significant. Thus, Hypotheses 4(a) and 4(b), as well as Hypotheses 5(a) and 5(b), were not supported.
TABLE 5.
Social Support and Meaningful Work as Predictors of Emergency Medicine Personnel's Mental Health Strain
| B | SE | t | p | 95% CI | ||
|---|---|---|---|---|---|---|
| LL | UL | |||||
| Hypothesis 3(a) | ||||||
| MHS Control | 0.77 | 0.05 | 17.02 | .001*** | 0.68 | 0.86 |
| Social Support | −0.01 | 0.08 | −0.19 | .849 | −0.16 | 0.13 |
| Hypothesis 3(b) | ||||||
| MHS Control | 0.71 | 0.05 | 13.56 | .001*** | 0.61 | 0.82 |
| Meaningful Work | −0.05 | 0.08 | −0.59 | .554 | −0.20 | 0.11 |
The mental health strain control variable controlled for participants’ mental health strain from the prior week. The marginal pseudo‐R 2 values for the models testing Hypothesis 3(a) and 3(b), respectively, were .56 and .49.
Abbreviations: B, slope; CI, confidence interval; LL, lower level of the 95% CI; MHS, mental health strain; p, significance value; SE, standard error; t, t approximation; UL, upper level of the 95% CI.
p < .001 (two‐tailed).
DISCUSSION
The COVID‐19 pandemic has been challenging in many ways for healthcare professionals, particularly in terms of the mental health strain it has added to a workforce that has been experiencing an increase in burnout and stress in recent years (Rodriguez et al., 2020). Accordingly, it is critical to understand what specific factors play a role in generating increased mental health strain as well as factors that may aid in supporting healthcare professionals and in mitigating the impacts of such strain. The purpose of this article was to address this issue by presenting an integrated review of prior literature examining healthcare professionals’ experiences during similar epidemics and pandemics, and by offering an empirical examination of weekly fluctuations in EMP mental health strain during the early stages of the COVID‐19 pandemic. In the following sections, we further synthesize the results of our review and empirical study, highlighting key contributions to theory as well as practice. We also note limitations of the study and offer several recommendations regarding important next steps for future researchers aiming to continue to expand this important area of work.
Contributions to Theory and Practice
This research makes several unique theoretical and practical contributions. First, in applying the JD‐R model to the healthcare professional context, our review of the literature contributes an overarching theoretical framework that clarifies the novel job and personal demands that healthcare professionals may face during virus epidemics and pandemics, as well as the resources that may be beneficial in addressing these demands. Overall, this review contributes to our understanding of healthcare providers’ mental health and well‐being during virus epidemics and pandemics, namely that they are likely to be impacted by an imbalance of increased unique demands and stagnated or declining resources. In light of our subsequent study, this may be especially critical for emergency departments and other frontline healthcare workers as EMP experience higher levels of stress than other occupations even during regular, non‐pandemic work (Schneider & Weigl, 2018).
Our empirical study of EMP’s demands, resources, and mental health strain serves as an important contribution towards addressing the need for an increased understanding of within‐person fluctuations in mental health strain during a virus epidemic or pandemic. Furthermore, the mixed results provide interesting insights regarding what may impact healthcare professionals on the frontline of a virus epidemic or pandemic. Notably, we found support for our hypotheses regarding the negative impacts of COVID‐19 job and personal demands on EMP’s mental health strain over time, as well as the interactive effects of personal demands and number of hours worked per week. As expected, increases in COVID‐19 personal demands, COVID‐19 job demands, and number of hours worked were each associated with an increase in EMP’s mental health strain. However, while there was not an interaction of COVID‐19 job demands and number of hours worked, the relationship between COVID‐19 personal demands and mental health strain was amplified as the number of hours worked increased.
One explanation for these results could be that several personal demands were unique to the COVID‐19 pandemic context and may have been unusually concerning, such as fear of getting loved ones sick or feeling uncertain as to how long the pandemic would last. When paired with an increasing number of hours, EMP have less time to detach from work and manage these unexpected demands, especially when personal resources that are typically available to help manage these personal demands (e.g., social support from family) may not be an option, leading to greater mental health strain (see Sonnentag & Fritz, 2015). However, an increased number of hours may not have the same effect on COVID‐19 job demands if appropriate resources were still available. Overall, these findings contribute to our growing understanding as to what demands may be more influential in regard to healthcare professionals’ mental health, especially in terms of highlighting the role of personal demands for EMP as a potential area for increased attention.
An additional explanation for the findings regarding COVID‐19 job demands and mental health strain is that the pandemic context may be exacerbating systemic issues that are typically more manageable by EMP in typical non‐pandemic settings, and that some of these organizational issues may be uniquely driven by the structure of healthcare systems within the United States. In the United States, individuals often rely much more heavily on the Emergency Department (ED) as a primary healthcare resource, leading to challenges such as overcrowding, inadequate staffing, and misuse of the ED for non‐emergency routine care (Chen et al., 2020). Accordingly, typical job demands in pandemic and virus epidemics are likely to be not only exacerbated, but to also introduce or reveal additional weaknesses in an already stressed system, such as the inadequate provision of PPE. When paired with an increasing number of work hours, these perpetual and newly introduced job demands are likely to play that much more of a role in negatively impacting EMP’s mental health strain.
Regarding the role of social support and meaningful work as potential resources for buffering against mental health strain, we were unable to demonstrate any statistically significant impact. While initially these results seem surprising, there are a few issues that may offer a clearer understanding as to why this was the case. First, it may be that while these are valuable resources, these two may not be the most needed resources for addressing EMP’s mental health strain during the early stage of the COVID‐19 pandemic. This is in alignment with the previous discussion of personal demands and resources being misaligned. If EMP are consistently and increasingly feeling personal demands such as a fear of getting others sick or being unable to share concerns about the pandemic with others, receiving social support may actually increase their concerns and result in the subsequent increase in mental health strain.
Instead, EMP may need resources such as being able to fully disconnect and detach when not at work, or adjustments to their schedules or work hours to provide recovery time. Taken as a whole, the findings of this study offer important insight as to the value of identifying specific resources that may be most beneficial to supporting EMP and other healthcare professionals during virus epidemics and pandemics. While further research is warranted, this initial within‐person study makes a contribution to our understanding in particular of personal demands and the need to rapidly identify the specific resources that may serve as buffers to ensure mental health strain does not increase over time.
Limitations and Future Directions
As with any study, there are limitations that must be considered when interpreting the results of our study. There are also future research directions that can address these limitations and enhance theory and practice in this context. First, in order to keep the survey to a manageable length so that EMP would respond on a weekly basis, we were not able to include previously validated, complete scales for variables such as meaningful work, which may have reduced our ability to capture meaningful variations over time. Regarding the measurement of demands and resources, we did rely upon similar measurement approaches implemented in studies of healthcare professionals during virus epidemics and pandemics, including the COVID‐19 pandemic (Rodriguez et al., 2020; Tam et al., 2004). We also utilized objective metrics for capturing the demand of work hours, which helped to reduce the survey length while also providing reliable and accurate data. However, the checklists were formative measures that were summed from dichotomous items, which again may have reduced the ability to capture finer grained, significant fluctuations over time.
From a future research perspective, continued refinement and testing of appropriate measures is a critical future step for this area of research, and may benefit from increased inclusion of less obtrusive, more objective measures. For example, researchers have examined the potential use of psychophysiological responses as a measure of physicians’ cognitive demands while on the job (Johannessen, Szulewski, Radulovic, White, Braund, Howes, Rodenburg, & Davies, 2020), while others are developing methods for objectively capturing physician stress using wearable sensors (Kaczor, Carreiro, Stapp, Chapman, & Indic, 2020). These types of metrics may be very useful for dynamically monitoring healthcare professionals’ physical demands and workload during virus epidemics and pandemics. However, a mixed methods approach will most likely be the optimal approach for effectively capturing and analyzing all elements of the JD‐R framework over time.
Another limitation of the study relates to the timing of the study. While we did conduct this study over a 6‐week period and were therefore able to examine fluctuations during that time period, the experiences and subsequent mental health strain of EMP during this initial phase of a virus pandemic may be different for a more extended period of time. For example, some demands—such as a shortage of PPE—may have had a greater impact on mental health strain at the start of the COVID‐19 pandemic, while other demands—such as having to quarantine multiple times due to exposure—may have greater effects later in the pandemic. Furthermore, the compounding effects of months of high demands and potentially inconsistent resources may also result in different patterns of strain over these extended periods of time. Future research is critically needed to explore these issues regarding mental health strain fluctuations in these contexts.
Finally, our sample drew from a single healthcare organization within one region of the United States and, therefore, may need to be examined in other contexts and with multiple organizations to ensure generalizability. The US healthcare system operates differently than many other countries, particularly in terms of the reliance upon EDs as a source of primary care (Chen et al., 2020). Other countries’ healthcare systems may rely less on EMP as frontline sources of care and may have different systems for managing resources such as PPE (Khalil, Alam, Arefin, Chowdhury, Huq, Chowdhury, & Khan, 2020). Therefore, the external validity of these findings is limited primarily to the United States and international healthcare systems with similar structural features. However, it is important to note that despite drawing from a single organizational entity, the sample does include responses from multiple, distributed sites, with some sites being newer to the organization than others, and urgent care sites that are more similar in their operation to general practitioner models. As such, the present study sample is likely to be more representative of EMP more broadly than if the data been collected from a single site within the organization.
CONCLUSION
The findings of this review and study of EMP’s mental health strain during the COVID‐19 pandemic, as well as the broader challenge of burnout within the medical community today, highlight that it is more imperative than ever to clarify resources and demands that impact provider mental health and well‐being. Furthermore, our findings indicate that there may be unique demands that are experienced during virus epidemics and pandemics, and that there is a need to more fully understand the specific resources needed to address these demands in order to reduce mental health strain. We have offered several recommendations regarding current needs and future directions for more rigorous, longitudinal research that dynamically examines these relationships. While it is not possible to go back and change the approach to the COVID‐19 pandemic, we hope that our recommendations can both help inform practices throughout the remainder of the pandemic as well as offer guidance for proactive preparations for the future.
ACKNOWLEDGEMENTS
The research described in the present article was supported by a transformative health seed grant from the Prisma Health Sciences Center, Greenville, SC. The authors would like to thank Ron Pirrallo for his feedback regarding the project.
REFERENCES
- Aguinis, H. , Gottfredson, R.K. , & Culpepper, S.A. (2013). Best‐practice recommendations for estimating cross‐level interaction effects using multilevel modeling. Journal of Management, 39(6), 1490–1528. [Google Scholar]
- Bakker, A.B. , & Demerouti, E. (2007). The job demands–resources model: State of the art. Journal of Managerial Psychology, 22, 309–328. 10.1108/02683940710733115 [DOI] [Google Scholar]
- Bakker, A.B. , & Demerouti, E. (2017). Job demands‐resources theory: Taking stock and looking forward. Journal of Occupational Health Psychology, 22(3), 273–285. [DOI] [PubMed] [Google Scholar]
- Beal, D.J. , & Weiss, H.M. (2003). Methods of ecological momentary assessment in organizational research. Organizational Research Methods, 6(4), 440–464. 10.1177/1094428103257361 [DOI] [Google Scholar]
- Belfroid, E. , van Steenbergen, J. , Timen, A. , Ellerbroek, P. , Huis, A. , & Hulscher, M. (2018). Preparedness and the importance of meeting the needs of healthcare workers: A qualitative study on Ebola. The Journal of Hospital Infection, 98(2), 212–218. 10.1016/j.jhin.2017.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben‐Itzhak, S. , Dvash, J. , Maor, M. , Rosenberg, N. , & Halpern, P. (2015). Sense of meaning as a predictor of burnout in emergency physicians in Israel: A national survey. Clinical and Experimental Emergency Medicine, 2(4), 217–225. http://libproxy.clemson.edu/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=mnh&AN=27752601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bobak, C.A. , Barr, P.J. , & O’Malley, A.J. (2018). Estimation of an inter‐rater intra‐class correlation coefficient that overcomes common assumption violations in the assessment of health measurement scales. BMC Medical Research Methodology, 18(1), 93–103. 10.1186/s12874-018-0550-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britt, T.W. , Adler, A.B. , & Bartone, P.T. (2001). Deriving benefits from stressful events: The role of engagement in meaningful work and hardiness. Journal of Occupational Health Psychology, 6(1), 53–63. [DOI] [PubMed] [Google Scholar]
- Brooks, S.K. , Dunn, R. , Amlôt, R. , Rubin, G.J. , & Greenberg, N. (2018). A systematic, thematic review of social and occupational factors associated with psychological outcomes in healthcare employees during an infectious disease epidemic. Journal of Occupational and Environmental Medicine, 60(3), 248–257. 10.1097/JOM.0000000000001235 [DOI] [PubMed] [Google Scholar]
- Cai, Z. , Zheng, S. , Huang, Y. , Zhang, X. , Qiu, Z. , Huang, A. , & Wu, K. (2020). Emotional and cognitive responses and behavioral coping of Chinese medical workers and general population during the pandemic of COVID‐19. International Journal of Environmental Research and Public Health, 17(17), 6198. 10.3390/ijerph17176198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver, C.S. (1997). You want to measure coping but your protocol’s too long: Consider the brief COPE. International Journal of Behavioral Medicine, 4, 92–100. 10.1207/s15327558ijbm0401_6 [DOI] [PubMed] [Google Scholar]
- Chan, A.O.M. , & Huak, C.Y. (2004). Psychological impact of the 2003 severe acute respiratory syndrome epidemic on health care workers in a medium size regional general hospital in Singapore. Occupational Medicine (Oxford, England), 54(3), 190–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, W. , Linthicum, B. , Argon, N.T. , Bohrmann, T. , Lopiano, K. , Mehrotra, A. , Travers, D. and Ziya, S. (2020). The effects of emergency department crowding on triage and hospital admission decisions. The American Journal of Emergency Medicine, 38(4), 774–779. https://doi‐org.libproxy.clemson.edu/10.1016/j.ajem.2019.06.039 [DOI] [PubMed] [Google Scholar]
- Cooper, C.L. , Dewe, P.J. , & O’Driscoll, M.P. (2001). Organizational stress: A review and critique of theory, research, and applications. London, UK: Sage Publications. [Google Scholar]
- Demerouti, E. , Bakker, A.B. , Nachreiner, F. , & Schaufeli, W.B. (2001). The job demands‐resources model of burnout. Journal of Applied Psychology, 86(3), 499–512. [PubMed] [Google Scholar]
- Dolan, E.D. , Mohr, D. , Lempa, M. , Joos, S. , Fihn, S.D. , Nelson, K.M. , & Helfrich, C.D. (2015). Using a single item to measure burnout in primary care staff: A psychometric evaluation. Journal of General Internal Medicine, 30(5), 582–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyrbye, L.N. , Satele, D. , Sloan, J. , & Shanafelt, T.D. (2013). Utility of a brief screening tool to identify physicians in distress. Journal of General Internal Medicine, 28(3), 421–427. 10.1007/s11606-012-2252-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders, C.K. , & Tofighi, D. (2007). Centering predictor variables in cross‐sectional multilevel models: A new look at an old issue. Psychological Methods, 12(2), 121–138. 10.1037/1082-989X.12.2.121 [DOI] [PubMed] [Google Scholar]
- Fox, J. (2016). Applied regression analysis and generalized linear models (3rd ed.). Thousand Oaks, CA: Sage. [Google Scholar]
- Goh, Y. , Ong, J.J.Y. , Bharatendu, C. , Tan, B.Y.Q. , & Sharma, V.K. (2020). Headaches due to personal protective equipment during COVID‐19 pandemic: A comment. Headache, 60(7), 1446–1447. 10.1111/head.13879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grace, S.L. , Hershenfield, K. , Robertson, E. , & Stewart, D.E. (2005). The occupational and psychosocial impact of SARS on academic physicians in three affected hospitals. Psychosomatics, 46(5), 385–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johannessen, E. , Szulewski, A. , Radulovic, N. , White, M. , Braund, H. , Howes, D. , Rodenburg, D. , & Davies, C. (2020). Psychophysiologic measures of cognitive load in physician team leaders during trauma resuscitation. Computers in Human Behavior, 111, 106393. [Google Scholar]
- Kaczor, E.E. , Carreiro, S. , Stapp, J. , Chapman, B. , & Indic, P. (2020). Objective measurement of physician stress in the emergency department using a wearable sensor. In Proceedings of the … Annual Hawaii International Conference on System Sciences. Annual Hawaii International Conference on System Sciences (Vol. 2020, pp. 3729–3738). NIH Public Access. [PMC free article] [PubMed] [Google Scholar]
- Kang, L. , Li, Y. , Hu, S. , Chen, M. , Yang, C. , Yang, B.X. , Wang, Y. , Hu, J. , Lai, J. , Ma, X. , Chen, J. , Guan, L. , Wang, G. , Ma, H. , & Liu, Z. (2020). The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. The Lancet Psychiatry, 7(3), e14. Retrieved from https://doi‐org.libproxy.clemson.edu/10.1016/S2215‐0366(20)30047‐X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kantor, J. (2020). Behavioral considerations and impact on personal protective equipment use: Early lessons from the coronavirus (COVID‐19) pandemic. Journal of the American Academy of Dermatology, 82(5), 1087. 10.1016/j.jaad.2020.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalid, I. , Khalid, T.J. , Qabajah, M.R. , Barnard, A.G. , & Qushmaq, I.A. (2016). Healthcare workers emotions, perceived stressors and coping strategies during a MERS‐CoV epidemic. Clinical Medicine & Research, 14(1), 7–14. 10.3121/cmr.2016.1303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalil, M.M. , Alam, M.M. , Arefin, M.K. , Chowdhury, M.R. , Huq, M.R. , Chowdhury, J.A. , & Khan, A.M. (2020). Role of personal protective measures in prevention of COVID‐19 spread among physicians in Bangladesh: A multicenter cross‐sectional comparative study. SN Comprehensive Clinical Medicine, 2(10), 1733–1739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kisely, S. , Warren, N. , McMahon, L. , Dalais, C. , Henry, I. , & Siskind, D. (2020). Occurrence, prevention, and management of the psychological effects of emerging virus epidemics on healthcare workers: Rapid review and meta‐analysis. BMJ (Clinical Research Ed.), 369, m1642. 10.1136/bmj.m1642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koo, T.K. , & Li, M.Y. (2016). A guideline of selecting and reporting intraclass correlation coefficients for reliability research. Journal of Chiropractic Medicine, 15(2), 155–163. 10.1016/j.jcm.2016.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancee, W.J. , Maunder, R.G. , & Goldbloom, D.S. (2008). Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS epidemic. Psychiatric Services (Washington, D.C.), 59(1), 91–95. Retrieved from https://doi.org.libproxy.clemson.edu/10.1176/ps.2008.59.1.91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, M. , Battaglioli, N. , Melamed, M. , Mott, S.E. , Chung, A.S. , & Robinson, D.W. (2019). High prevalence of burnout among US emergency medicine residents: Results from the 2017 National Emergency Medicine Wellness Survey. Annals of Emergency Medicine, 74(5), 682–690. [DOI] [PubMed] [Google Scholar]
- Mak, I.W.C. , Chu, C.M. , Pan, P.C. , Yiu, M.G.C. , & Chan, V.L. (2009). Long‐term psychiatric morbidities among SARS survivors. General Hospital Psychiatry, 31(4), 318–326. 10.1016/j.genhosppsych.2009.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marjanovic, Z. , Greenglass, E.R. , & Coffey, S. (2007). The relevance of psychosocial variables and working conditions in predicting nurses’ coping strategies during the SARS crisis: An online questionnaire survey. International Journal of Nursing Studies, 44(6), 991–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuishi, K. , Kawazoe, A. , Imai, H. , Ito, A. , Mouri, K. , Kitamura, N. , Miyake, K. , Mino, K. , Isobe, M. , Takamiya, S. , Hitokoto, H. , & Mita, T. (2012). Psychological impact of the pandemic (H1N1) 2009 on general hospital workers in Kobe. Psychiatry and Clinical Neurosciences, 66(4), 353–360. Retrieved from https://doi‐org.libproxy.clemson.edu/10.1111/j.1440‐1819.2012.02336.x [DOI] [PubMed] [Google Scholar]
- Maunder, R.G. (2009). Was SARS a mental health catastrophe? General Hospital Psychiatry, 31(4), 316–317. 10.1016/j.genhosppsych.2009.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maunder, R.G. , Lancee, W.J. , Balderson, K.E. , Bennett, J.P. , Borgundvaag, B. , Evans, S. , Fernandes, C.M. , Goldbloom, D.S. , Gupta, M. , Hunter, J.J. , & Wasylenki, D.A. (2006). Long‐term psychological and occupational effects of providing hospital healthcare during SARS epidemic. Emerging Infectious Diseases, 12(12), 1924–1932. 10.3201/eid1212.060584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgantini, L.A. , Naha, U. , Wang, H. , Francavilla, S. , Acar, Ö. , Flores, J.M. , Crivellaro, S. , Moreira, D. , Abern, M. , Eklund, M. , Vigneswaran, H.T. , & Weine, S.M. (2020). Factors contributing to healthcare professional burnout during the COVID‐19 pandemic: A rapid turnaround global survey. PLoS One, 15(9), e0238217. 10.1371/journal.pone.0238217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakagawa, S. , & Schielzeth, H. (2013). A general and simple method for obtaining R 2 from generalized linear mixed‐effects models. Methods in Ecology and Evolution, 4(2), 133–142. [Google Scholar]
- Park, J.S. , Lee, E.H. , Park, N.R. , & Choi, Y.H. (2018). Mental health of nurses working at a government‐designated hospital during a MERS‐CoV epidemic: A cross‐sectional study. Archives of Psychiatric Nursing, 32(1), 2–6. 10.1016/j.apnu.2017.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinheiro, J.C. , & Bates, D.M. (2000). Mixed‐effects models in S and S‐PLUS. New York, NY: Springer‐Verlag. [Google Scholar]
- Pinheiro, J. , Bates, D. , DebRoy, S. , & Sarkar, D. (2013). nlme: Linear and nonlinear mixed effects models. R package version 3.1‐150. Retrieved from https://CRAN.R‐project.org/package=nlme [Google Scholar]
- Preti, E. , Di Mattei, V. , Perego, G. , Ferrari, F. , Mazzetti, M. , Taranto, P. , Di Pierro, R. , Madeddu, F. , & Calati, R. (2020). The psychological impact of epidemic and pandemic epidemics on healthcare workers: Rapid review of the evidence. Current Psychiatry Reports, 22(8), 43. Retrieved from https://doi‐org.libproxy.clemson.edu/10.1007/s11920‐020‐01166‐z [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team . (2020). R: A language and environment for statistical computing. Vienna, Austria. Retrieved from https://www.R‐project.org/. [Google Scholar]
- Raudenbush, S. W. , & Bryk, A.S. (2002). Hierarchical linear models: Applications and data analysis methods (2nd ed.). Thousand Oaks, CA: Sage. [Google Scholar]
- Reich, N.G. , Brooks, L.C. , Fox, S.J. , Kandula, S. , McGowan, C.J. , Moore, E. , Osthus, D. , Ray, E.L. , Tushar, A. , Yamana, T.K. , Biggerstaff, M. , Johansson, M.A. , Rosenfeld, R. , & Shaman, J. (2019). A collaborative multiyear, multimodel assessment of seasonal influenza forecasting in the United States. Proceedings of the National Academy of Sciences of the United States of America, 116(8), 3146–3154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez, R.M. , Medak, A.J. , Baumann, B.M. , Lim, S. , Chinnock, B. , Frazier, R. , & Cooper, R.J. (2020). Academic emergency medicine physicians’ anxiety levels, stressors, and potential stress mitigation measures during the acceleration phase of the COVID‐19 pandemic. Academic Emergency Medicine, 27(8), 700–707. 10.1111/acem.14065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romo, V. (2020, April 28). NYC emergency room physician who treated coronavirus patients dies by suicide. NPR. Retrieved from https://www.npr.org/sections/coronavirus‐live‐updates/2020/04/28/847305408/nyc‐emergency‐room‐physician‐who‐treated‐coronavirus‐patients‐dies‐by‐suicide?t=1588799220486 [Google Scholar]
- Rosopa, P.J. , Schaffer, M. , & Schroeder, A.N. (2013). Managing heteroscedasticity in general linear models. Psychological Methods, 18(3), 335–351. 10.1037/a0032553 [DOI] [PubMed] [Google Scholar]
- Rotenstein, L.S. , Torre, M. , Ramos, M.A. , Rosales, R.C. , Guille, C. , Sen, S. , & Mata, D.A. (2018). Prevalence of burnout among physicians: A systematic review. Journal of the American Medical Association, 320(11), 1131–1150. 10.1001/jama.2018.12777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schecter, R. , Pham, T. , Hua, A. , Spinazzola, R. , Sonnenklar, J. , Li, D. , & Milanaik, R. (2020). Prevalence and longevity of PTSD symptoms among parents of NICU infants analyzed across gestational age categories. Clinical Pediatrics, 59(2), 163–169. [DOI] [PubMed] [Google Scholar]
- Schneider, A. , & Weigl, M. (2018). Associations between psychosocial work factors and provider mental well‐being in emergency departments: A systematic review. PLoS One, 13(6), e0197375. 10.1371/journal.pone.0197375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semmer, N.K. , Jacobshagen, N. , Meier, L.L. , Elfering, A. , Beehr, T.A. , Kälin, W. , & Tschan, F. (2015). Illegitimate tasks as a source of work stress. Work & Stress, 29(1), 32–56. https://doi‐org.libproxy.clemson.edu/10.1080/02678373.2014.1003996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma, M. , Creutzfeldt, C.J. , Lewis, A. , Patel, P.V. , Hartog, C. , Jannotta, G.E. , Blissitt, P. , Kross, E.K. , Kassebaum, N. , Greer, D.M. , Curtis, J.R. , & Wahlster, S. (2020). Healthcare professionals’ perceptions of critical care resource availability and factors associated with mental well‐being during COVID‐19: Results from a US survey. Clinical Infectious Diseases. 10.1093/cid/ciaa1311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout, P.E. , & Fleiss, J.L. (1979). Intraclass correlations: Uses in assessing rater reliability. Psychological Bulletin, 86(2), 420–428. 10.1037/0033-2909.86.2.420 [DOI] [PubMed] [Google Scholar]
- Snijders, T.A.B. , & Bosker, R.J. (2012). Multilevel analysis: An introduction to basic and advanced multilevel modeling (2nd ed.). London, UK: Sage. [Google Scholar]
- Sonnentag, S. , & Fritz, C. (2015). Recovery from job stress: The stressor‐detachment model as an integrative framework. Journal of Organizational Behavior, 36(S1), S72–S103. [Google Scholar]
- Stuijfzand, S. , Deforges, C. , Sandoz, V. , Sajin, C.‐T. , Jaques, C. , Elmers, J. , & Horsch, A. (2020). Psychological impact of an epidemic/pandemic on the mental health of healthcare professionals: A rapid review. BMC Public Health, 20(1), 1230. 10.1186/s12889-020-09322-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tam, C.W.C. , Pang, E.P.F. , Lam, L.C.W. , & Chiu, H.F.K. (2004). Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: Stress and psychological impact among frontline healthcare workers. Psychological Medicine, 34(7), 1197–1204. 10.1017/S0033291704002247 [DOI] [PubMed] [Google Scholar]
- Wu, P. , Fang, Y. , Guan, Z. , Fan, B. , Kong, J. , Yao, Z. , Liu, X. , Fuller, C.J. , Susser, E. , Lu, J. , & Hoven, C.W. (2009). The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. Canadian Journal of Psychiatry, 54(5), 302–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, P. , Liu, X. , Fang, Y. , Fan, B. , Fuller, C.J. , Guan, Z. , & Litvak, I.J. (2008). Alcohol abuse/dependence symptoms among hospital employees exposed to a SARS epidemic. Alcohol and Alcoholism, 43(6), 706–712. 10.1093/alcalc/agn073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xanthopoulou, D. , Bakker, A.B. , Demerouti, E. , & Schaufeli, W.B. (2007). The role of personal resources in the job demands‐resources model. International Journal of Stress Management, 14, 121–141. 10.1037/1072-5245.14.2.121 [DOI] [Google Scholar]
- Zhu, Z. , Xu, S. , Wang, H. , Liu, Z. , Wu, J. , Li, G. , Miao, J. , Zhang, C. , Yang, Y. , Sun, W. , & Zhu, S. (2020). COVID‐19 in Wuhan: Immediate psychological impact on 5062 health workers (preprint). medRxiv. 10.1101/2020.02.20.20025338.t [DOI] [PMC free article] [PubMed] [Google Scholar]


