To the Editor,
After more than half of 2020, the pandemic due to the coronavirus diseases 2019 (COVID‐19) is causing a devastating impact around the world. 1 The first line of workers against COVID‐19 is the health sector, which undoubtedly is the fundamental piece in this emergency. Studies conducted in China showed that 2.8% of the infected persons corresponded to health personnel, 2 a percentage that is currently higher in some Latin American countries, for example in Peru, 100 days after the state of emergency reported a fatality rate of 3.5% among doctors. 3 , 4
In Honduras, on August 5, 2020, the platform “Everyone Against COVID‐19” released a report of the prevalence of COVID‐19 in health personnel. According to this report, the National Emergency Coordinating Committee (SINAGER) had reported 45,098 positive cases of which 2542 (5.6%) correspond to health personnel, a percentage higher than the reported in other countries of Latin America, that have focused mainly in physicians (Table 1). 4 , 5 The majority of health personnel affected by COVID‐19 are between the ages of 20–40 years old (Figure 1).
Table 1.
Positivity in health personnel, by occupation in Honduras
| Type of health personnel | rt‐PCR tests performed | Percentage of positivity | |
|---|---|---|---|
| Total | Positives | ||
| Psychology | 135 | 47 | 34.8 |
| Pharmacy | 193 | 59 | 30.6 |
| Nursing assistant | 3500 | 1050 | 30.0 |
| Paramedic | 75 | 21 | 28.0 |
| Dentistry | 233 | 60 | 25.8 |
| Registered nurse | 723 | 183 | 25.3 |
| Health students | 179 | 44 | 24.6 |
| Public health | 274 | 66 | 24.1 |
| Surgery staff | 229 | 52 | 22.7 |
| General practitioner (MD) | 2595 | 566 | 21.8 |
| Imaging | 177 | 38 | 21.5 |
| Medical specialist | 257 | 54 | 21.0 |
| Medical residents | 103 | 13 | 12.6 |
| Anesthesia | 140 | 17 | 12.1 |
| Other health personnel | 124 | 46 | 37.1 |
| Other hospital activities | 140 | 44 | 31.4 |
| Total | 9831 | 2542 | 25.9 |
Abbreviation: rt‐PCR, real‐time polymerase chain reaction.
Source: rt‐PCR tests carried out by the LNV‐UVS‐SESAL, until July 30, 2020.
Figure 1.
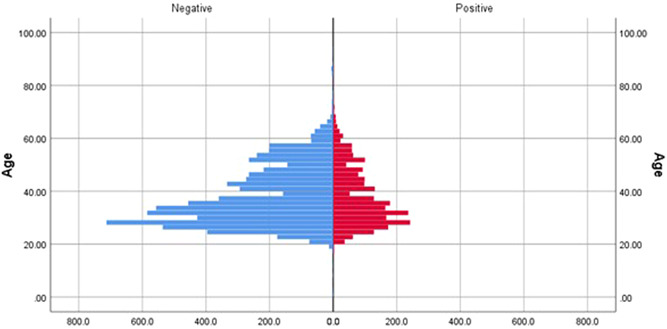
Laboratory results by age among health personnel (numbers). Source: RT‐PCR tests carried out by the LNV‐UVS‐SESAL, until July 30, 2020. RT‐PCR, reverse transcription polymerase chain reaction
In addition to poor health infrastructure, the Honduran health system tends to persist with a recurrent shortage of equipments, medicines, supplies, and human resources. The pandemic has imposed a significant toll on health services, that is insufficient to satisfy the demands of the population. The lack of personal protective equipment (PPE) for COVID‐19 associated with overexposure to the virus 3 , 6 caused a higher contagion rate in exposed personnel (Table 1). On top of this high‐risk environment, there is a need to perform a higher number of tests, compared to the current average of 1300 tests per day during the last months. The possibility of investigating the factors that contribute to the shortage of PPE should be considered, since in addition to the limited availability in the country, the inappropriate use of this can be a contributing factor. 7
There are several protective measures for health personnel, such as availability and proper use of Personal Protective Equipment (PPE). WHO recommends the use of masks (N95, FFP2, FPP3 or equivalent, and of guaranteed quality), however, in Honduras, some lots of N95 that were purchased during the emergency were not certified or were for industrial use.
Most of the national health infrastructure was built in the period 1960–1970. Therefore, the implementation of exclusive spaces for the evaluation and admission of COVID‐19 patients was a challenge and very soon, we had cross‐infections among different health services. A deficient culture on risk management and the disposition of contaminated materials was another challenge to the health system. 6
Due to the lack of opportune laboratory testing and diagnosis, only health personnel with high‐risk factors for severe disease or with signs and symptoms compatible with COVID‐19 were removed from their work. 3 , 6 Last year health students and recently under graduated health professionals were also hired to address the increasing demand.
The enormous psychological and physical burden involved in seeing a large number of patients and colleagues dying from COVID‐19 causes a psychological impact on health personnel. In addition to the risk of exposure and “Burn Out” syndrome, psychological pathologies can arise or can be exacerbated by this situation 8 , 9 Psychological assistance should be continuous to evaluate and guarantee the good psychological status of employees. 6 More studies, on the impact of COVID‐19 in healthcare workers, especially in Latin America, are needed. 4
CONFLICT OF INTERESTS
All authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
Karla Iveth Henriquez‐Marquez, Doris Carolina Lainez‐Murillo, and Lysien I. Zambrano conceived the review, developed the preliminary search strategy, and drafted the manuscript. All authors critically reviewed the manuscript for relevant intellectual content. All authors have read and approved the final version of the paper.
DATA AVAILABILITY STATEMENT
Available on request.
REFERENCES
- 1. Henriquez‐Marquez KI, Zambrano LI, Arteaga‐Livias K, Rodríguez‐Morales AJ. Prevención e identificación temprana de casos sospechosos COVID‐19 en el primer nivel de atención en Centro América. Atención Primaria. Epub Ahead June. 2020:13. 10.1016/j.aprim.2020.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Taype‐Rondan A, Hurtado‐Roca Y, Estrada‐Martínez M, Timaná‐Ruiz R. Recomendaciones clínicas para la evaluación y manejo de riesgo de COVID‐19 en personal de salud del Seguro Social del Perú (EsSalud). Acta Med Peru. 2020;37(1):84‐87. [Google Scholar]
- 3. Galán‐Rodas E, Tarazona‐Fernández A, Palacios‐Celi M. Riesgo y muerte de los médicos a 100 días del estado de emergencia por el COVID‐19 en Perú. Acta Med Peru. 2020;37(2):119‐121. [Google Scholar]
- 4. Valenzuela‐Rodriguez G, Zambrano LI, Muñoz‐Lara F, Pecho‐Silva S, Arteaga‐Livias K, Rodríguez‐Morales AJ. Intranational differences in the case fatality rates for COVID‐19 among Peruvian physicians. Int J Infect Dis. 2020;101:226‐227. 10.1016/j.ijid.2020.09.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Alger J, Alvarado T, Corrales A, et al. Prevalencia de Infeccion por SARS‐Cov.2 en personal de salud: plataforma todos contra el COVID‐19. 2020. http://www.desastres.hn/COVID-19/Plataforma/19_Plataforma%20Todos%20Contra%20COVID19_Informe_07.08.2020.pdf
- 6. Rodrigo S. COVID‐19: Cómo podemos proteger al personal sanitario expuesto? Revista Argentina de Medicina. 2020;8(1):83‐85. [Google Scholar]
- 7. Bressan S, Buonsenso D, Farrugia R, et al. Preparedness and response to pediatric COVID‐19 in European emergency departments: a survey of the REPEM and PERUKI networks. Ann Emerg Med. 2020;76:788‐800. 10.1016/j.annemergmed.2020.05.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Talevi D, Socci V, Carai M, et al. Mental health outcomes of the COVID‐19 pandemic. Riv Psichiatr. 2020;55(3):137‐144. [DOI] [PubMed] [Google Scholar]
- 9. Sun D, Yang D, Li Y, et al. Psychological impact of 2019 novel coronavirus (2019‐nCoV) outbreak in health workers in China. Epidemiol Infect. 2020;148:e96. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Available on request.


