Abstract
Cyberchondria is an excessive or repeated online health information seeking that is associated with increasing levels of health anxiety or distress. This article presents a model of cyberchondria during public health crises such as the COVID‐19 pandemic. The factors that contribute to cyberchondria at this time include (a) a heightened perception of threat and fear of a newly identified and poorly understood disease; (b) difficulty in coping with uncertainty associated with the pandemic; (c) lack of authoritative and trustworthy sources of relevant health information; (d) difficulty in coping with abundance of information that is often confusing, conflicting, unverified and constantly updated, along with a decreased ability to filter out unnecessary information; and (e) inability of excessive online health information seeking to provide the necessary information and deliver reassurance. These factors amplify fear and distress, which increases the perception of threat and uncertainty and perpetuates further online health searches. Cyberchondria has significant public health implications because of the associated distress or functional impairment and effects on health behaviors. Cyberchondria should be addressed by targeting a heightened perception of threat, improving management of uncertainty and online health information and promoting an ability to critically appraise the results of online health searches. This should contribute to a better online health information literacy. The model of cyberchondria during the COVID‐19 pandemic explains the hypothesized rise in cyberchondria during public health emergencies and helps to formulate a framework for prevention of cyberchondria and its effective management.
Keywords: COVID‐19, cyberchondria, information overload, intolerance of uncertainty, online health information, online health information literacy, online health searching, public health, reassurance seeking, uncertainty
1. INTRODUCTION
The COVID‐19 pandemic has had a far‐reaching impact on the modern world. It has changed living conditions drastically and produced a disruption in all areas of life, including a breakdown of the sense of safety, increased social isolation, decreased trust in political and social institutions and economic devastation. Governments around the world have limited personal freedoms by ordering people to stay at home, only allowing office work under certain circumstances and imposing strict “physical distancing” rules to prevent the spread of COVID‐19. Considering the nature of the pandemic and its consequences, this situation also poses various challenges to mental health (e.g., Brooks et al., 2020).
Compared to previous large‐scale epidemics, one issue of immediate relevance for mental health that is novel for the COVID‐19 pandemic is a potentially increased problematic Internet use (PIU; Király et al., 2020). This may occur because of the restrictions on face‐to‐face contacts and the requirement to spend prolonged periods of time at home due to which people may experience more distress and seek an escape through online activities. PIU encompasses various behaviors, and a concern has been expressed about the rise in online gaming (King, Delfabbro, Billieux, & Potenza, 2020) and gambling (Håkansson, Fernández‐Aranda, Menchón, Potenza, & Jiménez‐Murcia, 2020), inappropriate use of social media (Wiederhold, 2020) and increased consumption of online pornography (Mestre‐Bach, Blycker, & Potenza, 2020) during the COVID‐19 pandemic. One problematic online activity that is particularly relevant at the time of public health emergencies is an excessive online health research (OHR). In the context of the COVID‐19 pandemic, this activity relates mainly to seeking information about COVID‐19. The purpose of this article is to present a model that aims to explain problematic OHR (i.e., cyberchondria) during public health crises such as the COVID‐19 pandemic.
2. CYBERCHONDRIA
Cyberchondria has been conceptualized as an excessive or repeated OHR that is associated with increasing levels of health anxiety or distress (Starcevic, 2017). It has also been described as a “multidimensional construct” that reflects both “anxiety and an element of compulsiveness” and encompasses repetitious and time‐consuming OHR, negative emotional states or distress associated with OHR and the consequent interruption or neglect of other activities (McElroy & Shevlin, 2014). Cyberchondria has been considered to represent a 21st century counterpart to hypochondriasis, with the two constructs overlapping in terms of the specific problematic behaviors (excessive health information seeking, persistent health‐related checking and/or reassurance seeking), negative emotional state (health anxiety or distress), persistence of problematic behaviors despite their negative consequences (compulsivity) and interference with functioning.
Cyberchondria has been strongly associated with a heightened health anxiety (Bajcar & Babiak, 2019; Bajcar, Babiak, & Olchowska‐Kotala, 2019; Barke, Bleichhardt, Rief, & Doering, 2016; Fergus, 2014; McMullan, Berle, Arnáez, & Starcevic, 2019; Norr, Albanese, Oglesby, Allan, & Schmidt, 2015; Starcevic, Baggio, Berle, Khazaal, & Viswasam, 2019) and PIU (Fergus & Spada, 2017; McElroy & Shevlin, 2014; Singh & Brown, 2014; Starcevic et al., 2019). Cyberchondria is also related to obsessive–compulsive disorder (OCD; Bajcar et al., 2019; Bajcar & Babiak, 2019; Fergus, 2014; Fergus & Russell, 2016; Fergus & Spada, 2018; Vismara et al., 2020). According to the reassurance‐seeking model of cyberchondria (Starcevic & Berle, 2013), cyberchondria is maintained by uncertainty embedded in OHR, intolerance of ambiguity and uncertainty, dilemmas about the trustworthiness of the sources of online health information, need for a “definitive” or “straightforward” explanation and difficulty coping with an abundance of information (“information overload”), especially if much of that information is conflicting or contradictory.
While some people with heightened levels of health anxiety develop cyberchondria, this behavioral pattern may also occur in the absence of a preexisting, heightened health anxiety (Starcevic, 2017). Regardless of whether or not high levels of health anxiety precede cyberchondria, OHR perpetuates itself despite causing or amplifying distress under the circumstances of a perceived threat to one's health and wellbeing, intolerable uncertainty, difficulty coping with information overload and confusion as to who could be trusted to provide accurate information and deliver reassurance online. These circumstances reflect the COVID‐19 pandemic and may help explain the hypothesized rise in cyberchondria during this time.
3. COVID‐19 PANDEMIC AND CYBERCHONDRIA: THE NATURAL BEDFELLOWS
Our proposed model of cyberchondria during the COVID‐19 pandemic is an applied version of the reassurance‐seeking model of cyberchondria. Moreover, the trigger for cyberchondria in the model of cyberchondria during the COVID‐19 pandemic is the overall context of the pandemic rather than the occurrence of a new symptom in the generic reassurance‐seeking model of cyberchondria. The proposed model is presented in Figure 1, which illustrates the dynamic relationships between its components. These are discussed below and include a heightened perception of threat and fear of COVID‐19, difficulties in coping with uncertainty, questionable trustworthiness of online information, difficulties in coping with information overload and ineffective online reassurance seeking.
FIGURE 1.
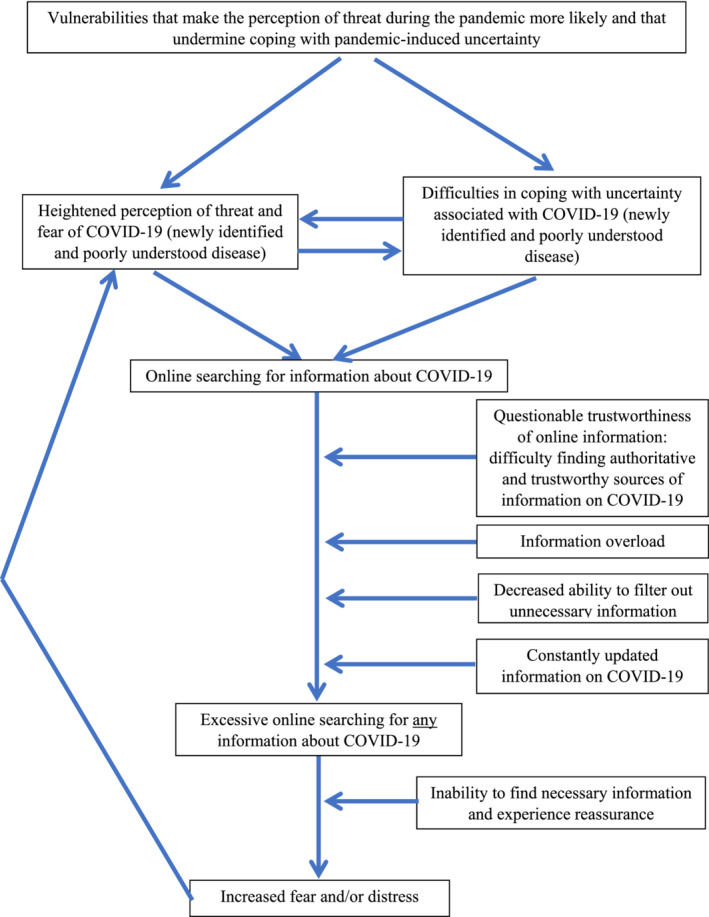
Model of cyberchondria during the COVID‐19 pandemic
3.1. Heightened perception of threat and fear of COVID‐19
COVID‐19 has only recently been identified, it is highly contagious, it can have a lethal outcome and there is currently no evidence‐based treatment for it. As such, COVID‐19 understandably elicits fear, similar to the fear of other incurable and deadly infectious diseases in the past. Therefore, the perception of threat associated with COVID‐19 is not unreasonable on its own. Nevertheless, there seem to be large differences between individuals in terms of the perception of threat and the consequent fear. For example, some studies have reported higher anxiety levels during the COVID‐19 pandemic among younger individuals who are not considered to be at a higher risk of developing a severe form of COVID‐19 (e.g., Moghanibashi‐Mansourieh, 2020; Ozamiz‐Etxebarria, Dosil‐Santamaria, Picaza‐Gorrochategui, & Idoiaga‐Mondragon, 2020). Reasons for unexpectedly high levels of the fear of COVID‐19 are diverse and may include biological factors (e.g., genetic predisposition), psychological factors (e.g., personality traits such as neuroticism, perceived susceptibility to disease and emotional vulnerabilities such as proneness to worry and poor tolerance of uncertainty) and environmental factors (e.g., panic‐like societal attitude toward the disease). The role of these factors is likely to vary from one person to another.
The perception of threat during the COVID‐19 pandemic does not only pertain to one's physical health (i.e., fear of becoming infected or dying from the disease (Schimmenti, Billieux, & Starcevic, 2020; Taylor et al., 2020), which is the fear domain with obvious implications for cyberchondria. The experience of fear in the context of the pandemic is multifaceted and includes other aspects that are relevant for cyberchondria, such as fear of infecting others, fear of not knowing what one needs to know about COVID‐19 and fear of being paralyzed and of not taking whatever action may be necessary to protect oneself or others (Schimmenti et al., 2020). In addition, other fears (e.g., fear of the economic repercussions of the pandemic (Taylor et al., 2020) may also drive excessive OHR and thereby contribute to cyberchondria.
3.2. Difficulties in coping with uncertainty
A pervasive uncertainty has been one of the hallmarks of the COVID‐19 pandemic. For the most part, this is also because COVID‐19 is a newly identified and poorly understood disease for which the societies and healthcare systems around the world have not been prepared. In this context, uncertainty is invariably experienced negatively. In fact, “uncertainty distress” is the term introduced in the setting of the COVID‐19 pandemic and defined as “the subjective negative emotions experienced in response to the as yet unknown aspects of a given situation” (Freeston, Tiplady, Mawn, Bottesi, & Thwaites, 2020).
Given this experience of uncertainty, the way people cope with it is of immediate relevance. In the digital age, many try to cope with health‐related uncertainty by turning to the Internet to find answers to their questions (e.g., Singh, Fox, & Brown, 2016); this may have been the case with COVID‐19‐related queries, too. Effectively managing uncertainty may depend on various factors, including the ability to tolerate it.
Intolerance of uncertainty has been defined in several ways. According to one definition, it denotes a need for “cognitive closure,” whereby such a closure reflects a desire for “an answer on a given topic, any answer” (Kruglansky, 1990). Another definition suggests that intolerance of uncertainty is an excessive tendency to consider the occurrence of a negative event unacceptable and threatening, regardless of the probability of its occurrence (Carleton, Norton, & Asmundson, 2007; Dugas, Gosselin, & Ladouceur, 2001). Irrespective of the definition, the concept of intolerance of uncertainty combines the lack of needed information with a lack of assurance that such information would become available in the foreseeable future.
Intolerance of uncertainty is a transdiagnostic construct, associated with various anxiety and related disorders. Several studies have found intolerance of uncertainty to be moderately correlated with cyberchondria (Fergus, 2013, 2015; Fergus & Spada, 2017, 2018; Norr et al., 2015; Zangoulechi, Yousefi, & Keshavarz, 2018). While some of these studies suggested that intolerance of uncertainty might be a risk factor for cyberchondria (Fergus, 2013, 2015; Norr et al., 2015; Zangoulechi et al., 2018), others found that intolerance of uncertainty was not uniquely associated with cyberchondria (Fergus & Spada, 2017, 2018). Although both inhibitory intolerance of uncertainty (referring to a paralyzing effect of uncertainty) and prospective intolerance of uncertainty (referring to an anxious apprehension about uncertainty and desire for predictability of future events) were significantly associated with cyberchondria, the former was associated more strongly than the latter. This suggests that feeling “paralyzed” and possibly being preoccupied with threats may be a somewhat more common response to uncertainty in cyberchondria than seeking information to reduce uncertainty. Consequently, there are two effects of a difficulty in tolerating COVID‐19‐related uncertainty (Figure 1). The first is experiencing an inability to take action and increased perception of threat from COVID‐19. The second is engaging in online health information seeking about COVID‐19. Both effects may make cyberchondria more likely.
3.3. Questionable trustworthiness of online information
The Internet is a repository of a huge amount of information, but a large proportion of that information may be unreliable and untrustworthy. Distinguishing between trustworthy and untrustworthy information is not always easy and difficulties in making this distinction have been associated with cyberchondria (e.g., Starcevic & Berle, 2013). What makes the COVID‐19 pandemic situation particularly challenging in this regard relates back to the fact that so little is known about COVID‐19. Therefore, sources of health information that are usually regarded as reliable because they provide accurate and unambiguous information are not necessarily perceived as authoritative and trustworthy when it comes to COVID‐19. This “crisis of confidence” undermines a notion that it is possible to distinguish between trustworthy and untrustworthy sources of online information on COVID‐19. As a result, people may feel that they are left to their own devices when trying to make this distinction.
A diminished trust in social and political institutions during the pandemic (e.g., Balog‐Way & McComas, 2020; Bargain & Aminjonov, 2020) may make COVID‐19 information obtained from the “official” sources (e.g., websites of public health agencies and governments) and COVID‐19 information obtained from “alternative” sources (e.g., social media) equally credible. This situation is likely to make cyberchondria flourish because the large amount of information on COVID‐19 found on various websites (e.g., Cuan‐Baltazar, Muñoz‐Perez, Robledo‐Vega, Pérez‐Zepeda, & Soto‐Vega, 2020) or shared on social media (e.g., Laato, Najmul Islam, Nazrul Islam, & Whelan, 2020) is misleading, inaccurate or false. Indeed, misinformation on COVID‐19 is increasingly being recognized as a significant public health issue and a risk in its own right (Krause, Freiling, Beets, & Brossard, 2020). In particular, various social media have been implicated in what has been termed a “pandemic of misinformation” (Li, Bailey, Huynh, & Chan, 2020) and “COVID‐19 misinformation epidemic” (Kouzy et al., 2020). Given these findings, perception of social media as a trustworthy source of COVID‐19‐related information is likely to intensify searches for more information and increase a sense of confusion and distress, thereby contributing to cyberchondria during the pandemic.
3.4. Difficulties in coping with information overload
Information processing is a challenge in the digital age. This is largely a function of the abundance of information, that is, information overload. According to Bawden and Robinson (2009), information overload occurs when the amount of information that one is exposed to becomes “a hindrance rather than a help.” Overload of information derived from online sources has been found to have negative effects on general health and to increase distress (Misra & Stokols, 2012). Furthermore, a perceived information overload has been associated with negative affect, anxiety, depressive symptoms and anger in the context of OHR (Swar, Hameed, & Reychav, 2017). The World Health Organization has recently introduced the term “infodemic” to refer to an “overabundance of information—some accurate and some not—that makes it hard for people to find trustworthy sources and reliable guidance when they need it” (World Health Organization, 2020).
A common way of coping with information overload is filtering out of information that is irrelevant, vague or that seems untrustworthy—a process that may not be too arduous in the setting of a relative safety, social stability, predictability, and a semblance of certainty. However, effective filtering out of information may become more difficult when the world is under the specter of a pandemic that threatens individual lives and weakens a sense of safety, stability, and certainty. This is compounded by a need for the available information to be updated “on the run” as experts continue to seek understanding of the key aspects (patterns of transmission, associated symptoms, recovery, recurrence, and immunity) of a disease caused by a virus that has emerged only recently. As a result, this situation may undermine one's capacity to distinguish between relevant and irrelevant information about COVID‐19 and between information that is important and information that is useless. Without these distinctions, every piece of information has similar value and is worthy of attention. Moreover, less credible sources of information may seem relatively more appealing. For example, information about conspiracy theories that is normally ignored suddenly becomes potentially relevant (e.g., van Bavel et al., 2020).
An indiscriminate consumption of COVID‐19‐related information, most of which is found on various websites or on social media, often leads to confusion—and ultimately a pervasive fear. This is especially the case when much of that information is conflicting or contradictory and when it is being constantly updated. Indeed, a recent study has demonstrated that individuals who used social media as their main source of information during the COVID‐19 pandemic suffered from more information overload and exhibited a more prominent cyberchondria (Farooq, Laato, & Najmul Islam, 2020).
3.5. Ineffective online reassurance seeking
People who are troubled by fears of COVID‐19 and/or distressed by uncertainty may seek information on COVID‐19 online for the purpose of reassurance. They may hope to find an explanation for incongruent pieces of information, seek to understand the disease better or understand how to prevent it and protect themselves—and feel safer. Ideally, this information would be clear, easy to understand and definitive, which might obviate a need for further OHR. Those who need much information to feel reassured may be more prone to developing cyberchondria because they may continue looking for it ad infinitum. The point at which the amount and quality of information becomes sufficient is difficult to determine, which is similar to a difficulty that many people with OCD encounter when trying to figure out what constitutes a “just right” feeling. This is one domain in which cyberchondria resembles OCD. Moreover, the abundance of online information also means that vulnerable individuals may encounter frightening information that triggers new worries and prompts them to look for further information and seek reassurance for concerns that did not originally trigger OHR. However, the Internet was not designed to provide reassurance, there is much uncertainty during the process of OHR itself and the outcome of OHR is largely unpredictable. Many people may not be aware of this and instead, have unrealistic expectations of the Internet. Therefore, when their OHR fails to provide them with necessary information and reassurance, many may feel frustrated, overwhelmed, disappointed and more distressed or fearful.
Despite the mounting fear or distress caused by OHR, people with cyberchondria continue searching for more COVID‐19‐related information. This makes OHR compulsive and leads to a loss of control over this behavior, which is another link with OCD. Compulsivity in cyberchondria may be fueled by a fear of missing some presumably vital information and people may continue online searches as an attempt to reduce fear and alleviate a sense of uncertainty. A particularly pernicious contributor to such continued searching during the COVID‐19 pandemic may be the constant updating of online information about the disease as our understanding of it evolves, leading anxious individuals to recheck the current recommendations and what is known about COVID‐19. These people may believe that if they were to stop online searches, they might miss something important on COVID‐19 that has appeared in the meantime, thus overestimating the reassuring effect of the information and feeling compelled to continue with OHR.
3.6. Putting the components of cyberchondria during the COVID‐19 pandemic together
The model of cyberchondria during the COVID‐19 pandemic as presented in Figure 1 starts with the biological and psychological vulnerabilities that make the perception of threat during the pandemic more likely and that undermine coping with pandemic‐induced uncertainty. Online searching for COVID‐19‐related information is a response to a COVID‐19‐related threat and uncertainty because COVID‐19 is a newly identified and poorly understood disease. This response is likely to be stronger if the perceived threat from COVID‐19 is amplified or in the setting of ineffective coping with COVID‐19‐related uncertainty. Online searching for COVID‐19‐related information is made difficult by a questionable trustworthiness of much online information and a challenge of identifying authoritative and trustworthy sources of information. The sheer volume of this information that is also continuously updated and a decreased ability to filter out unnecessary information further complicate online searches; they become excessive, with almost any information on COVID‐19 being taken into account, regardless of how relevant it is. Inability to find necessary and reassuring information leads to more fear and distress, which amplifies the perception of threat and uncertainty. Cyberchondria perpetuates itself via further compulsive online searches and reassurance seeking in a fear‐amplifying spiral.
4. PUBLIC HEALTH SIGNIFICANCE OF CYBERCHONDRIA DURING PUBLIC HEALTH CRISES
Cyberchondria is a dysfunctional behavioral pattern, considering the distress associated with it and interference with functioning due to preoccupation with online health‐related information, time spent on OHR and neglect of other activities. Indeed, cyberchondria has been associated with functional impairment, even after taking into account the effects of health anxiety (Mathes, Norr, Allan, Albanese, & Schmidt, 2018). A specific aspect of this impairment relates to disrupted communication and relationships with health care providers and negative effects on the seeking and receiving of health care, such as avoidance of doctors and poor treatment adherence (McElroy & Shevlin, 2014; Singh & Brown, 2014). Cyberchondria has also been associated with an increased health care utilization, measured by the number of visits to general practitioners and other health professionals (Barke et al., 2016). In view of this, cyberchondria qualifies as a public health problem.
Based on the model that we have presented, cyberchondria is expected to be more likely during public health crises, such as the COVID‐19 pandemic. Public health implications of cyberchondria during the COVID‐19 pandemic should be assessed by ascertaining its impact on functioning and health‐related behaviors. It is also important to examine any specific features and consequences of cyberchondria during this time (e.g., panic‐like response to health information obtained online, joining “alternative” online health communities and reluctance to seek the necessary medical care because of the fear of contracting COVID‐19) because that might help efforts to plan for public health emergencies in the future. Issues that have also been identified in this regard relate to handling of health information on the Internet and social media and being cognizant of the effects of large‐scale epidemics and the attendant uncertainties on trust in public health authorities and institutions.
5. PREVENTING AND MANAGING CYBERCHONDRIA
Due to accessibility of OHR, people will continue to search for health information online, especially during large‐scale epidemics and when public health is jeopardized in any other way. Therefore, it would be unrealistic and counterproductive to suggest “abstinence” from this activity. Instead, Internet users need to achieve a high level of online health information literacy and feel confident about their ability to manage this information. This entails several measures, which are related to our model of cyberchondria during the COVID‐19 pandemic (Table 1). The first is understanding of what the Internet can do for an anxious person and its limitations when using it to obtain reassurance about health‐related threats. The second is a better management of online health information, especially when it is conflicting, inconsistent, and abundant. The third is coming to terms with the fact that some proportion of online health information cannot be trusted and reliance for the most part on the official and reputable sources of such information, despite their limitations and lack of absolute authority with new outbreaks and obscure illnesses. The fourth is avoidance of social media as the only or predominant source of online health information and encouraging efficient self‐control strategies when social media are used. The fifth is promoting an ability to critically appraise the results of OHR, perhaps via user‐friendly consumer guides (e.g., Australian Government, 2019; Charnock & Shepperd, 2004; Victoria State Government, 2015) that provide simple and clear instructions about factors to consider when encountering online health information. Finally, the acceptance of the limitations of medical knowledge should help at least some Internet users learn to live with unavoidable uncertainty and allow them to cease their futile online searches. With implementation of these measures, OHR during public health crises may not be experienced as threatening and overwhelming and people will be able to perform OHR feeling more empowered, without necessarily escalating their health concerns.
TABLE 1.
Model of cyberchondria during the COVID‐19 pandemic: components, explanations, and corrective strategies
| Components | Explanations | Corrective strategies |
|---|---|---|
| Difficulties in coping with uncertainty |
|
|
| Questionable trustworthiness of online information, including the negative role of social media |
|
|
|
|
|
| Difficulties in coping with information overload |
|
|
| Ineffective online reassurance seeking |
|
|
Abbreviation: OHR, online health research.
If the features of cyberchondria are more severe and especially if there is a significant interference with functioning, additional approaches may be needed. These include a good understanding and aggressive targeting of the specific precipitants of cyberchondria (e.g., high levels of health anxiety, heightened perception of threat and disruptive sense of uncertainty), the purpose of cyberchondria (e.g., reassurance seeking and alleviation of uncertainty), maintaining factors (e.g., misinterpretation of online health information, perfectionist tendencies, confusion about whom to trust, intolerance of uncertainty and fear of missing out on important health information if one stops OHR), and consequences (e.g., an almost exclusive preoccupation with the pandemic, difficulty shifting the focus of attention onto other aspects of life and loss of the sense of agency and the corresponding ability to make important decisions, to plan and act). These factors should be addressed depending on the extent to which they are present in a particular individual.
6. CONCLUSION
The fear and uncertainty induced by the COVID‐19 pandemic and the abundance of online, unverified and constantly updated information related to this global threat to public health are a fertile soil for the development of cyberchondria, which is itself increasingly recognized as having significant public health implications. We can effectively fight against this new hazard by addressing the amplified perception of threat and improving uncertainty management and online health information literacy. Our model of cyberchondria during the COVID‐19 pandemic contributes to the literature by helping to understand the hypothesized rise in cyberchondria during public health emergencies and formulate a framework for prevention of cyberchondria and effective responding to it.
AUTHOR CONTRIBUTIONS
Vladan Starcevic: Drafted the first version of the paper. Adriano Schimmenti, Joël Billieux, and David Berle: Provided critical comments and participated in the revision of the paper. All authors approved the final (submitted) version of the paper.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1002/hbe2.233.
Biographies
vladan starcevic is an associate professor at the Sydney Medical School and Faculty of Medicine and Health of the University of Sydney, Australia. He is also a visiting professor at the University of Belgrade, Serbia and Consultant Psychiatrist and Head of the Academic Department of Psychiatry at Nepean Hospital in Sydney. His main professional and research interests include anxiety and obsessive–compulsive and related disorders, complex emotional states, health anxiety and hypochondriasis, personality disorders, psychopharmacological treatment of anxiety disorders and mental health issues associated with digital technologies. He has done some pioneering work in the area of cyberchondria.
adriano schimmenti is a full professor of psychopathology at the UKE ‐ Kore University of Enna, where he is also delegate of the Rector for students with physical and learning disabilities and director of the Master course in Clinical Psychology. He is Deputy Director of the Italian Society of Psychological Assessment (SIPDC), Research Director of the Italian Institute of Psychoanalytic Psychotherapy (IIPP), and Scientific Guarantor of the Italian Centre of Analytical Psychology (CIPA). His main area of research concerns the psychodynamics of addictive behaviors and the effects of psychological trauma on mental and behavioral functioning.
joël billieux recently joined the University of Lausanne (UNIL) in Switzerland as an associate professor of Clinical Psychology, Psychopathology, and Psychological Assessment. In the past years, he worked as a professor of Clinical Psychology at the University of Luxembourg (2017–2020) and at the Catholic University of Louvain in Belgium (2011–2017). His main area of research concerns the psychological factors (cognitive, affective, motivational, and interpersonal) involved in the etiology of addictive behaviors, with a particular focus on self‐regulation‐related processes. Other research interests include the conceptualization and diagnosis of behavioral addictions, and the effect of emerging technologies on human behavior and cognition.

david berle is a clinical psychologist and associate professor in the Discipline of Clinical Psychology at the University of Technology Sydney (UTS). His research interests include cognitive–behavioral models and therapies for posttraumatic stress disorder (PTSD), obsessive–compulsive disorder (OCD), depression, and anxiety disorders. Other interests include problematic and compulsive patterns of technology use.

Starcevic V, Schimmenti A, Billieux J, Berle D. Cyberchondria in the time of the COVID‐19 pandemic. Hum Behav & Emerg Tech. 2021;3:53–62. 10.1002/hbe2.233
DATA AVAILABILITY STATEMENT
The authors elect to not share data.
REFERENCES
- Australian Government . (2019). Health information online. Retrieved from https://www.healthdirect.gov.au/health-information-online
- Bajcar, B. , & Babiak, J. (2019). Self‐esteem and cyberchondria: The mediation effects of health anxiety and obsessive‐compulsive symptoms in a community sample. Current Psychology. 10.1007/s12144-019-00216-x [DOI] [Google Scholar]
- Bajcar, B. , Babiak, J. , & Olchowska‐Kotala, A. (2019). Cyberchondria and its measurement. The polish adaptation and psychometric properties of the Cyberchondria Severity Scale CSS‐PL. Psychiatria Polska, 53, 49–60. 10.12740/PP/81799 [DOI] [PubMed] [Google Scholar]
- Balog‐Way, D. H. P. , & McComas, K. A. (2020). COVID‐19: Reflections on trust, tradeoffs, and preparedness. Journal of Risk Research, 1–11. 10.1080/13669877.2020.1758192 [DOI] [Google Scholar]
- Bargain, O. , & Aminjonov, U. (2020). Trust and compliance to public health policies in times of COVID‐19. (Bordeaux Economics Working Papers, BxWP2020‐06). [DOI] [PMC free article] [PubMed]
- Barke, A. , Bleichhardt, G. , Rief, W. , & Doering, B. K. (2016). The Cyberchondria Severity Scale (CSS): German validation and development of a short form. International Journal of Behavioral Medicine, 23, 595–605. 10.1007/s12529-016-9549-8 [DOI] [PubMed] [Google Scholar]
- Bawden, D. , & Robinson, L. (2009). The dark side of information: Overload, anxiety and other paradoxes and pathologies. Journal of Information Science, 35, 180–191. 10.1177/0165551508095781 [DOI] [Google Scholar]
- Brooks, S. K. , Webster, R. K. , Smith, L. E. , Woodland, L. , Wessely, S. , Greenberg, N. , & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet, 395, 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carleton, R. N. , Norton, M. , & Asmundson, G. J. (2007). Fearing the unknown: A short version of the intolerance of uncertainty scale. Journal of Anxiety Disorders, 21, 105–117. 10.1016/j.janxdis.2006.03.014 [DOI] [PubMed] [Google Scholar]
- Charnock, D. , & Shepperd, S. (2004). Learning to DISCERN online: Applying an appraisal tool to health websites in a workshop setting. Health Education Research, 19, 440–446. 10.1093/her/cyg046 [DOI] [PubMed] [Google Scholar]
- Cuan‐Baltazar, J. Y. , Muñoz‐Perez, M. J. , Robledo‐Vega, C. , Pérez‐Zepeda, M. F. , & Soto‐Vega, E. (2020). Misinformation of COVID‐19 on the internet: Infodemiology study. JMIR Public Health Surveillance, 6, e18444. 10.2196/18444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dugas, M. J. , Gosselin, P. , & Ladouceur, R. (2001). Intolerance of uncertainty and worry: Investigating narrow specificity in a non‐clinical sample. Cognitive Therapy and Research, 25, 551–558. 10.1023/A:1005553414688 [DOI] [Google Scholar]
- Farooq, A. , Laato, S. , & Najmul Islam, A. K. M. (2020). The impact of online information on self‐isolation intention during the COVID‐19 pandemic: A cross‐sectional study. Journal of Medical Internet Research, 6, 22, e19128. 10.2196/19128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergus, T. A. (2013). Cyberchondria and intolerance of uncertainty: Examining when individuals experience health anxiety in response to internet searches for medical information. Cyberpsychology, Behavior and Social Networking, 16, 735–739. 10.1089/cyber.2012.0671 [DOI] [PubMed] [Google Scholar]
- Fergus, T. A. (2014). The Cyberchondria Severity Scale (CSS): An examination of structure and relations with health anxiety in a community sample. Journal of Anxiety Disorders, 28, 504–510. 10.1016/j.janxdis.2014.05.006 [DOI] [PubMed] [Google Scholar]
- Fergus, T. A. (2015). Anxiety sensitivity and intolerance of uncertainty as potential risk factors for cyberchondria: A replication and extension examining dimensions of each construct. Journal of Affective Disorders, 184, 305–309. 10.1016/j.jad.2015.06.017 [DOI] [PubMed] [Google Scholar]
- Fergus, T. A. , & Russell, L. H. (2016). Does cyberchondria overlap with health anxiety and obsessive‐compulsive symptoms? An examination of latent structure and scale interrelations. Journal of Anxiety Disorders, 38, 88–94. 10.1016/j.janxdis.2016.01.009 [DOI] [PubMed] [Google Scholar]
- Fergus, T. A. , & Spada, M. M. (2017). Cyberchondria: Examining relations with problematic internet use and metacognitive beliefs. Clinical Psychology and Psychotherapy, 24, 1322–1330. 10.1002/cpp.2102 [DOI] [PubMed] [Google Scholar]
- Fergus, T. A. , & Spada, M. M. (2018). Moving toward a metacognitive conceptualization of cyberchondria: Examining the contribution of metacognitive beliefs, beliefs about rituals, and stop signals. Journal of Anxiety Disorders, 60, 11–19. 10.1016/j.janxdis.2018.09.003 [DOI] [PubMed] [Google Scholar]
- Freeston, M. H. , Tiplady, A. , Mawn, L. , Bottesi, G. , & Thwaites, S. (2020). Towards a model of uncertainty distress in the context of coronavirus (Covid‐19). Cognitive Behaviour Therapist, 13, e31. 10.1017/S1754470X2000029X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Håkansson, A. , Fernández‐Aranda, F. , Menchón, J. M. , Potenza, M. N. , & Jiménez‐Murcia, S. (2020). Gambling during the COVID‐19 crisis—A cause for concern? Journal of Addiction Medicine, 14, e10–e12. 10.1097/ADM.0000000000000690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King, D. L. , Delfabbro, P. H. , Billieux, J. , & Potenza, M. N. (2020). Problematic online gaming and the COVID‐19 pandemic. Journal of Behavioral Addictions, 9, 184–186. 10.1556/2006.2020.00016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Király, O. , Potenza, M. N. , Stein, D. J. , King, D. L. , Hodgins, D. C. , Saunders, J. B. , … Demetrovics, Z. (2020). Preventing problematic internet use during the COVID‐19 pandemic: Consensus guidance. Comprehensive Psychiatry, 100, 152180. 10.1016/j.comppsych.2020.152180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kouzy, R. , Abi Jaoude, J. , Kraitem, A. , El Alam, M. B. , Karam, B. , Adib, E. , … Baddour, K. (2020). Coronavirus goes viral: Quantifying the COVID‐19 misinformation epidemic on twitter. Cureus, 12, e7255. 10.7759/cureus.7255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause, N. M. , Freiling, I. , Beets, B. , & Brossard, D. (2020). Fact‐checking as risk communication: The multi‐layered risk of misinformation in times of COVID‐19. Journal of Risk Research, 1–8. 10.1080/13669877.2020.1756385 [DOI] [Google Scholar]
- Kruglansky, A. W. (1990). Motivations for judging and knowing: Implications for causal attribution. In Higgins E. T. & Sorrentino R. M. (Eds.), The handbook of motivation and cognition: Foundation of social behavior (Vol. 2, pp. 333–368). New York, NY: Guilford Press. [Google Scholar]
- Laato, S. , Najmul Islam, A. K. M. , Nazrul Islam, M. , & Whelan, E. (2020). Why do people share misinformation during the COVID‐19 pandemic? arXiv e‐prints, April 2020. arXiv:2004.09600
- Li, H. O.‐Y. , Bailey, A. , Huynh, D. , & Chan, J. (2020). YouTube as a source of information on COVID‐19: A pandemic of misinformation? BMJ Global Health, 5, e002604. 10.1136/bmjgh-2020-002604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathes, B. M. , Norr, A. M. , Allan, N. P. , Albanese, B. J. , & Schmidt, N. B. (2018). Cyberchondria: Overlap with health anxiety and unique relations with impairment, quality of life, and service utilization. Psychiatry Research, 261, 204–211. 10.1016/j.psychres.2018.01.002 [DOI] [PubMed] [Google Scholar]
- McElroy, E. , & Shevlin, M. (2014). The development and initial validation of the Cyberchondria Severity Scale (CSS). Journal of Anxiety Disorders, 28, 259–265. 10.1016/j.janxdis.2013.12.007 [DOI] [PubMed] [Google Scholar]
- McMullan, R. D. , Berle, D. , Arnáez, S. , & Starcevic, V. (2019). The relationships between health anxiety, online health information seeking, and cyberchondria: Systematic review and meta‐analysis. Journal of Affective Disorders, 245, 270–278. 10.1016/j.jad.2018.11.037 [DOI] [PubMed] [Google Scholar]
- Mestre‐Bach, G. , Blycker, G. , & Potenza, M. (2020). Pornography use in the setting of the COVID‐19 pandemic. Journal of Behavioral Addictions, 9, 181–183. 10.1556/2006.2020.00015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Misra, S. , & Stokols, D. (2012). Psychological and health outcomes of perceived information overload. Environment and Behavior, 44, 737–759. 10.1177/0013916511404408 [DOI] [Google Scholar]
- Moghanibashi‐Mansourieh, A. (2020). Assessing the anxiety level of Iranian general population during the COVID‐19 outbreak. Asian Journal of Psychiatry, 51, 102076. 10.1016/j.ajp.2020.102076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norr, A. M. , Albanese, B. J. , Oglesby, M. E. , Allan, N. P. , & Schmidt, N. B. (2015). Anxiety sensitivity and intolerance of uncertainty as potential risk factors for cyberchondria. Journal of Affective Disorders, 174, 64–69. 10.1016/j.jad.2014.11.023 [DOI] [PubMed] [Google Scholar]
- Ozamiz‐Etxebarria, N. , Dosil‐Santamaria, M. , Picaza‐Gorrochategui, M. , & Idoiaga‐Mondragon, N. (2020). Stress, anxiety, and depression levels in the initial stage of the COVID‐19 outbreak in a population sample in the northern Spain. Cadernos de Saúde Pública, 36, e00054020. 10.1590/0102-311x00054020 [DOI] [PubMed] [Google Scholar]
- Schimmenti, A. , Billieux, J. , & Starcevic, V. (2020). The four horsemen of fear: An integrated model of understanding fear experiences during the COVID‐19 pandemic. Clinical Neuropsychiatry, 17, 41–45. 10.36131/CN20200202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh, K. , & Brown, R. J. (2014). Health‐related internet habits and health anxiety in university students. Anxiety, Stress, and Coping, 27, 542–554. 10.1080/10615806.2014.888061 [DOI] [PubMed] [Google Scholar]
- Singh, K. , Fox, J. R. E. , & Brown, R. J. (2016). Health anxiety and internet use: A thematic analysis. Cyberpsychology: Journal of Psychosocial Research on Cyberspace, 10, 4. 10.5817/CP2016-2-4 [DOI] [Google Scholar]
- Starcevic, V. (2017). Cyberchondria: Challenges of problematic online searches for health‐related information. Psychotherapy and Psychosomatics, 86, 129–133. 10.1159/000465525 [DOI] [PubMed] [Google Scholar]
- Starcevic, V. , Baggio, S. , Berle, D. , Khazaal, Y. , & Viswasam, K. (2019). Cyberchondria and its relationships with related constructs: A network analysis. Psychiatric Quarterly, 90, 491–505. 10.1007/s11126-019-09640-5 [DOI] [PubMed] [Google Scholar]
- Starcevic, V. , & Berle, D. (2013). Cyberchondria: Towards a better understanding of excessive health‐related internet use. Expert Review of Neurotherapeutics, 13, 205–213. 10.1586/ern.12.162 [DOI] [PubMed] [Google Scholar]
- Swar, B. , Hameed, T. , & Reychav, I. (2017). Information overload, psychological ill‐being, and behavioral intention to continue online healthcare information search. Computers in Human Behavior, 70, 416–425. 10.1016/j.chb.2016.12.068 [DOI] [Google Scholar]
- Taylor, S. , Landry, C. , Paluszek, M. , Fergus, T. A. , McKay, D. , & Asmundson, G. J. G. (2020). Development and initial validation of the COVID Stress Scales. Journal of Anxiety Disorders, 72, 102232. 10.1016/j.janxdis.2020.102232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Bavel, J. J. , Baicker, K. , Boggio, P. S. , Capraro, V. , Cichocka, A. , Cikara, M. , … Willer, R. (2020). Using social and behavioural science to support COVID‐19 pandemic response. Nature Human Behaviour, 4, 460–471. 10.1038/s41562-020-0884-z [DOI] [PubMed] [Google Scholar]
- Victoria State Government . (2015). Finding reliable health information. Retrieved from https://www.betterhealth.vic.gov.au/health/servicesandsupport/finding-reliable-health-information
- Vismara, M. , Caricasole, V. , Starcevic, V. , Cinosi, E. , Dell'Osso, B. , Martinotti, G. , & Fineberg, N. A. (2020). Is cyberchondria a new transdiagnostic digital compulsive syndrome? A systematic review of the evidence. Comprehensive Psychiatry, 99, 152167. 10.1016/j.comppsych.2020.152167 [DOI] [PubMed] [Google Scholar]
- Wiederhold, B. K. (2020). Social media use during social distancing. Cyberpsychology, Behavior and Social Networking, 23, 275–276. 10.1089/cyber.2020.29181.bkw [DOI] [PubMed] [Google Scholar]
- World Health Organization . (2020). Novel coronavirus (2019‐nCov): Situation report – 13. Retrieved from https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200202-sitrep-13-ncov-v3.pdf
- Zangoulechi, Z. , Yousefi, Z. , & Keshavarz, N. (2018). The role of anxiety sensitivity, intolerance of uncertainty, and obsessive‐compulsive symptoms in the prediction of cyberchondria. Advances in Bioscience and Clinical Medicine, 6, 1–6. 10.7575/aiac.abcmed.v.6n.4p.1 29780691 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors elect to not share data.


