Abstract
COVID‐19 pandemic affects people in various ways and continues to spread globally. Researches are ongoing to develop vaccines and traditional methods of Medicine and Biology have been applied in diagnosis and treatment. Though there are success stories of recovered cases as of November 10, 2020, there are no approved treatments and vaccines for COVID‐19. As the pandemic continues to spread, current measures rely on prevention, surveillance, and containment. In light of this, emerging technologies for tackling COVID‐19 become inevitable. Emerging technologies including geospatial technology, artificial intelligence (AI), big data, telemedicine, blockchain, 5G technology, smart applications, Internet of Medical Things (IoMT), robotics, and additive manufacturing are substantially important for COVID‐19 detecting, monitoring, diagnosing, screening, surveillance, mapping, tracking, and creating awareness. Therefore, this study aimed at providing a comprehensive review of these technologies for tackling COVID‐19 with emphasis on the features, challenges, and country of domiciliation. Our results show that performance of the emerging technologies is not yet stable due to nonavailability of enough COVID‐19 dataset, inconsistency in some of the dataset available, nonaggregation of the dataset due to contrasting data format, missing data, and noise. Moreover, the security and privacy of people's health information is not totally guaranteed. Thus, further research is required to strengthen the current technologies and there is a strong need for the emergence of a robust computationally intelligent model for early differential diagnosis of COVID‐19.
Keywords: contact tracing, COVID‐19, diagnoses, emerging technology, pandemic, screening, surveillance, tracking
1. INTRODUCTION
The outbreak of atypical and human‐to‐human transmissible pathogen which caused severe acute respiratory syndrome coronavirus 2 (SARS‐COV‐2) was first reported in Wuhan City, Hubei province, China in December 2019 (Hu et al., 2020). Later on, the pathogen was identified as novel coronavirus 2019‐nCoV, which is renamed to COVID‐19 (Boulos & Estella, 2020). Ongoing outbreak of COVID‐19 continues decimating the global population and overwhelmed health systems globally. Globally, the medical industry continues to be overwhelmed by the COVID‐19 pandemic as cases increases exponentially (Raju, Mohd, HaleemKhan, & Abid, 2020). As of November 10, 2020, there were about 51,359,570 people infected with COVID‐19 and 1,271,398 deaths worldwide (Worldometers, 2020). There has been confusion on how COVID‐19 is transmitted in asymptomatic individuals regardless of WHO recommendations. Due to accelerating number of COVID‐19 cases, the World Health Organization (WHO) declared a public health emergency in February, 2020, which led to the closure of nonessential services, schools, travelling restrictions and recursive national lockdowns (WHO, 2020). These precarious measures are severely affected with limited information on how COVID‐19 spreads during the incubation period especially in asymptomatic individuals. Some scholars including Wu, Tiantian, Qun, and Zhicong (2020), Zheng (2020), and Zhao et al. (2020) stated that COVID‐19 could be transmitted through contact, droplets, airborne, fomite, faecal‐oral, bloodborne, mother‐to‐child, and animal‐to‐human transmission (Alfonso et al., 2020). The lack of reliable information on how COVID‐19 is transmitted varies from country to country which has caused detrimental effects on world economies, education, businesses and health systems globally.
COVID‐19 affected almost all countries globally and various advanced and emerging technologies are required to tackle various problems caused by the magnitude of the pandemic in the health systems (Mohd et al., 2020). COVID‐19 is severe in countries that experience a tremendous shortage of reverse transcription‐polymerase chain reaction (RT‐PCR) COVID‐19 testing kit, detection, screening, and tracking tools which increase the chances of spreading the disease. As of November 10, 2020, there are no approved treatments for COVID‐19, thus current measures rely on prevention, surveillance, and containment (Mbunge, 2020). Globally, physical distancing, social distancing, hands sanitization, regular temperature testing, wearing of nose and face mask, as well as handwashing, have been implemented as interventions to combat the spread of COVID‐19 (Mehtar, Wolfgang, Ndèye, & Abdoulaye, 2020) but the major challenge lies on the weak health‐care systems, financial burden, overcrowding, community behavior, poverty, and COVID‐19 preparedness and response plan.
Encumbered by extended lockdowns, travelling restrictions, and continuous increase of COVID‐19 cases, people should consider the role of emerging technologies in responding to global emergency of COVID‐19 which overwhelmed health systems of the infected countries. Emerging technologies including geospatial technology, AI, big data, cloud computing, telemedicine, blockchain, 5G technology, smart applications, IoMT, robotics, and additive manufacturing are substantially important as evident in epidemiological modeling, smart life tracking and disaster management. For example, global positioning technologies provide precise disaster location positions for relief and rehabilitation purposes. The same ideology can be incorporated in fighting COVID‐19 pandemic. For instance, emerging technologies can support healthcare delivery to ensure effective COVID‐19 detection, monitoring, diagnosing, screening, surveillance, tracking, and awareness. Such technologies can help to track the spread of COVID‐19 virus, contact tracing (Elliot, 2020), identifying the high‐risk patients, mapping COVID‐19 hotspots, real‐time case surveillance, screening, real‐time communication with healthcare professionals, and COVID‐19 task force. Also, emerging technologies could play a tremendous role in developing COVID‐19 guidelines, responses, and policies which ultimately improve planning, reporting process, treatment, contact tracing, prioritizing and allocation of resources, case‐based surveillance system, development of drugs and vaccines, and creating awareness. Besides, travelling restrictions and recursive national lockdowns, several companies including the healthcare service industry are prompted to consider adopting emerging technologies to avoid human‐to‐human contact and contacting physical objects, while improving services delivery to the needy.
Emerging technologies are urgently needed to effectively improve the efficiency of the global efforts in epidemic monitoring, virus tracking, prevention, control, treatment, resource allocation, vaccine development, predicting outbreaks, and vulnerabilities in both developed and developing countries (Harold, 2013). Currently, infected countries rely on contact tracing, quarantining of cases and contacts (Whitworth, 2020), active case finding and testing. However, Greiner et al. (2015) highlighted challenges of contact tracing process from the previous experiences with Ebola outbreak. These challenges include contact‐person identification, violation of security and privacy of contact‐persons, enrolling contact‐persons, locating contact‐persons, monitoring contact tracing personnel, increasing exposure of contact tracing personnel to COVID‐19 leading to stigmatization, and contact tracing personnel could be carriers of the pandemic. For instance, some contact‐persons have no physical address, some live in rural areas where there are no street names and identification cards, some people use nicknames, thus, contact tracing personnel will have to rely solely on physical descriptions of contact‐persons. To alleviate these challenges, emerging technologies can support healthcare delivery to tackle COVID‐19.
Therefore, this study aimed at providing a comprehensive review of application, activities, and effectiveness of emerging technologies that can be utilized for detecting, monitoring, diagnosing, screening, surveillance, mapping hotspots, tracking, and creating awareness in order to prevent and tackle COVID‐19. The article addresses the following questions:
What are the emerging technologies that have been used for tackling COVID‐19?
How effective are emerging technologies in tackling COVID‐19?
Which countries have adopted the technologies to tackle COVID‐19?
2. METHOD
We applied systematic literature review (SLR) following the guidelines in Kitchenham (2004) to guide the literature search in various electronic databases on emerging technologies for detecting, monitoring, diagnosing, screening, surveillance, mapping hotspots, tracking, and creating awareness to prevent and tackling COVID‐19 (Figure 1). Electronic databases explored are Google Scholar, Scopus, Science Direct, PubMed, Institute of Electrical and Electronics Engineers (IEEE) Xplore Digital Library, Association for Computing Machinery (ACM) Digital Library, Wiley Library, and Springer Link. The steps followed by this review were guided by the procedures stated by Kitchenham (2004) namely; search strategy, study selection (inclusion/exclusion criteria), study eligibility, and quality assessment.
FIGURE 1.
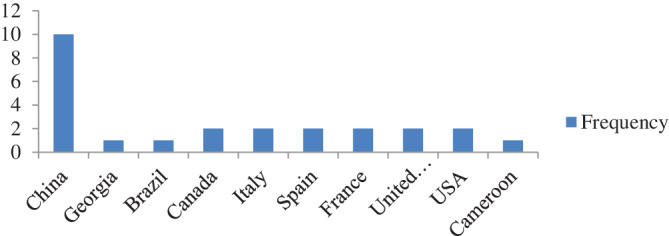
Countries that applied AI in tackling COVID‐19
2.1. Searching strategy
The previously published studies from the onset of the COVID‐19 outbreak were searched based on the following search string: Digital Technology “COVID‐19” OR Ebola OR “HIV AIDS” OR Disease OR Tuberculosis OR Malaria OR Tackling OR Tracking OR “Social Distancing” OR Diagnosis OR Treatment OR Prevention AND “Artificial intelligence” OR” Augmented Reality” OR “5G Cellular technology” OR “machine learning” OR “Internet of Medical Things.”
2.2. Study selection (inclusion and exclusion criteria)
We selected peer‐reviewed articles that were written in English, from the onset of the COVID‐19 outbreak. These articles were further screened based on title and abstract. We excluded opinion pieces, nonpeer‐reviewed articles, incomplete articles, and studies in other languages with no English translation.
2.3. Study eligibility and quality assessment
All articles were double screened for eligibility and quality assessment by all authors. Articles were examined their titles and abstracts. All duplicates were eliminated. To ensure that all articles with information about emerging technologies and related to COVID‐19 are included, we performed citations chain for additional studies for each retrieved article. The degree of accuracy and reliability of quality assessment of articles was measured using Cohen Kappa statistic (Cohen, 1968), therefore, the substantial agreement of authors was 77.3%, with Cohen's k: 0.50022.
3. RESULTS
We included 51 articles from electronic databases, published in 2020. We identified the following significant applications of emerging technologies, their roles in fighting COVID‐19 pandemic and their respective challenges as shown in Table 1. For each emerging technology, its activities and roles were further analyzed in the subsections under the discussion section. The study identified the following emerging technologies to be relevant in tackling COVID‐19: AI; Social media platforms; IoMT; Virtual Reality/Augmented Reality; Blockchain; Additive manufacturing; 5G Cellular technology and Smart Applications; Geographical Information Systems; Big Data; Autonomous Robots.
TABLE 1.
Emerging technologies in Tacking COVID‐19
| Emerging technologies | Highlights of the features of the technologies | Challenges |
|---|---|---|
| Artificial intelligence |
|
|
| Social media platforms |
|
|
| Internet of Medical Things |
|
|
| Virtual reality/Augmented Reality |
|
|
| Blockchain |
|
|
| Additive manufacturing |
|
|
| 5G cellular technology & smart applications |
|
|
| Geographical information systems |
|
|
| Big data |
|
|
| Autonomous robots |
|
|
3.1. Summary report of different COVID‐19 based technologies
Table 1 presents a summary report of different COVID‐19 based technologies. The features of these technologies are highlighted vis‐à‐vis the challenges experienced in the use of the technologies.
4. DISCUSSION
4.1. Applications of Artificial Intelligence in fighting COVID‐19 pandemic
Artificial Intelligence algorithms play a tremendous role in rapid detection, classification, identification, screening, and quantitation of patients with COVID‐19 as shown in Table 2. These AI algorithms have been used in machine learning, deep learning and computer vision to discover insightful patterns in datasets. Javaid et al. (2020) stated that there are limited uses of AI technologies due to lack of data. Also, Wim (2020) further stated that AI has not been fully explored on tracking and prediction of COVID‐19 cases in affected continents such as Europe, South and North America, and Africa. This might be attributed to the lack of a vast amount of historical data to train the AI models, which results in developing AI forecasting models that rely on noisy data and social media data. This severely affects the performance and accuracy of the forecasting model because of different data formats, lack of data standardization and interoperability, and missing values which is often inaccuracy and unreliable (Agbehadji, Bankole, Alfred, & Richard, 2020; Elliot, Fanwell, & Kinsley, 2018). The current literature, depicted in Table 2, shows that China is the leading pack in implementing AI technologies in fighting COVID‐19 pandemic. Countries such as the United States of America (USA), South Africa, Brazil, and India have recorded high COVID‐19 cases of 5,595,835; 589,886; 3,343,925; 2,701,604, respectively as of August 17, 2020; have not completely and successfully implemented AI techniques in combating COVID‐19 (Worldometers, 2020). These countries with high infection rate can utilize AI to detect, diagnose, identify and predict COVID‐19 new cases. Majority countries diagnose COVID‐19 using transcriptase‐polymerase chain reaction (RT–PCR) test which takes up to 2 days to complete and there is currently a shortage of RT–PCR test kits (Xueyan et al., 2020). Health systems are overwhelmed with increasing demand for RT–PCR test kits which led some countries to focus only on contact tracing rather than testing the affected populace. Therefore, there is a need for AI models for early detection and diagnosis of COVID‐19 using chest computed tomography (CT) images and can save radiologists' time. For example, Wang et al. (2020) developed a COVID‐Net deep learning model (with 98.9% accuracy) to diagnose COVID‐19 using chest CT images. Also, AI models can be used to develop COVID‐19 vaccine development and drug discovery. For instance, Abhimanyu, Vineet, and Oge (2020) state that Flinders University applied AI‐based program called Search Algorithm for Ligands (SAM) which generates trillions of synthetic compounds and determine the best trial candidates as vaccine adjuvants, thus reducing COVID‐19 vaccine development process. This could benefit health policymakers, health care professionals to effectively allocate resources to high‐risk zones and facilitate research (Raju et al., 2020). It is undoubtedly that AI technologies are conceivably reducing the burden of COVID‐19; however, these technologies face the following challenges such as: (1) limited access to a large COVID‐19 dataset for training and testing AI models; (2) The reliability and accuracy of AI models are also threatened with the availability of unstructured, noisy, and outlier COVID‐19 data; (3) Failing to detect asymptomatic COVID‐19 suspected individuals (Sera et al., 2020).
TABLE 2.
Applications of AI to fight COVID‐19 pandemic
| Author(s) | AI method | Activities | Country | Effectiveness of the model | Limitations |
|---|---|---|---|---|---|
| Lin et al. (2020) | Deep learning model | Identification of COVID‐19 using chest CT images | China | 96% accuracy | Overlap in the chest CT images identification with pneumonia. Also, the study does not consider other viral pneumonia for comparison and does not determine the severity of the COVID‐19 from CT images |
| Arni and Jose (2020) | Machine Learning algorithm | Identification of COVID‐19 using mobile‐phone based survey | Georgia | Not stated | The study does not consider COVID‐19 asymptomatic patients |
|
Chuansheng et al. (2020) |
Deep learning model | Detection for COVID‐19 from chest CT images | China | 90.1% accuracy | UNet model was trained using imperfect ground‐truth masks, and it could be improved using 3D segmentation |
| Fatima , Abu‐Naser, Alajrami, Abu‐Nasser, and Alashqar (2020) | Convolutional neural network | COVID‐19 Detection | China | 97% accuracy | The convolutional neural network was trained and tested with 130 CVID‐19 Chest X‐ray images. There is a need to redeploy the model with a large dataset and check the performance |
| Lu et al. (2020) | Deep learning model | COVID‐19 quantitative chest CT assessment | China | 65.5% accuracy | No systematic confirmation for all patients at the first and second follow up hence the model still needs radiologists' supervision |
| Gozes et al. (2020) | Deep learning | COVID‐19 classification using CT image analysis | China | 99.6% | The model detects, quantify, and track COVID‐19 and model is currently being expanded to a larger population to improve the quantification and tracking. Due to lack of quality dataset, the model did not perform well on the tracking of the infected person and contact persons |
| Zixin, Ge, Jin, & Xiong, (2020) | Modified Auto‐encoder | Forecasting COVID‐19 cases | China | Not stated | The study applied cluster analysis method instead of modified auto‐encoder functions because of lack of data |
| Xueyan et al. (2020) | Deep Learning (convolutional neural network) & Machine learning (support vector machine) | Rapid diagnosis of COVID‐19 patients | China | 92% | The study used a small sample which might affect the generalizability of the model. Also, the study focuses only on COVID‐19 positive cases |
| Matheus, Ramon, Viviana, and Leandro (2020) | Machine learning (support vector regression) | Forecasting COVID‐19 cases | Brazil | Accuracy of 92.77% | The study proposed to improve the performance of the model by incorporating stacking‐ensemble learning and deep learning in a sample dataset, however, data augmentation and multi‐objective optimization were not implemented to deal with small data samples. |
| Li et al. (2020a, 2020b) | XGBoost machine learning‐based model | Predict the mortality rates of COVID‐19 patients | China | Accuracy of 90% | The study developed XGBoost classifier to predict the mortality of COVID‐19 patient 10 days in advance. Since the model is data‐driven and interpretability, the results may vary based on the quality and size of the dataset hence the study is limited to clinical settings |
| Vinay and Lei (2020) | Deep learning (long short‐term memory‐LSTM) | Forecasting of COVID‐19 transmission | Canada | Accuracy of 92.67% | The sample size used was small |
| Sarbjit et al. (2020) | least square support vector machine | Prediction of COVID‐19 confirmed cases | Italy, Spain, France, United Kingdom, United States of America (USA) | 99% approximate accuracy | The model was tested using Ljung‐Box test, therefore further modeling of data series is required to check for linear dependencies and adequacy of the model |
| Abdelhafid, Fouzi, Abdelkader, and Ying (2020) | Deep learning methods (LSTM, Recurrent Neural Network, Bidirectional LSTM, Variational Auto Encoder, and Gated recurrent units) | Forecasting COVID‐19 cases using time‐series data | Italy, Spain, France, China, USA, Australia |
|
Due to the poor data quality (noisy, incomplete, format) and the limited size of the dataset, the model reported experiencing vanishing gradient problems leading to varying forecasting results for all the countries. |
| Zohair et al. (2020) | Machine learning approaches (linear models, SVM, K‐Nearest Neighbors Regressor, and Decision Tree) | Predicting COVID‐19 mortality rate | France, UK | The study shows that weather variables play an important role to predict COVID‐19 mortality rate | The study needs some improvements by including additional weather features such as wind speed and rainfall |
| Hameni, Bowong, Tewa, and Kurths et al. (2020) | Deep learning model (Ensemble Kalman filter) | Forecasts of the COVID‐19 pandemic | Cameroon | The normalized forward sensitivity index of the basic reproduction number, R 0 = 2.9495 meaning that COVID‐19 would disappear without vaccines, and increase of new COVID‐19 cases |
Generalization of results was based on short‐ term forecasting and small dataset. |
| Mohammad et al. (2020) | Deep Learning model (ResNet) | Detection of Covid‐19 from chest X‐ray images | China | 95% of accuracy | Dataset used was limited to 50 images which makes it difficult to determine its effectiveness and efficiency with a large dataset |
| Wang, Alexander, and Zhong (2020) | Deep Learning model (COVID‐Net) | Detection of COVID‐19 cases from chest X‐ray images | Canada | Accuracy of 93.3% | COVID‐Net achieves high positives hence the need for further PCR testing and it would increase the burden for the healthcare system |
There is significant progress in the implementation of AI models in tackling COVID‐19. Table 2 shows that AI concepts especially deep learning models and machine learning models have been applied to perform the following activities:
Identification of COVID‐19 using chest CT images
Detection of COVID‐19 from chest CT images
COVID‐19 quantitative chest CT assessment
Classification of COVID‐19 using CT image analysis
Rapid diagnosis of COVID‐19 patients
Forecasting COVID‐19 cases
Predicting COVID‐19 mortality rate
Tracking COVID‐19 patients and contact‐persons
However, these models performed differently based on the COVID‐19 dataset used and different algorithms applied. For instance, studies conducted by Abdelhafid et al. (2020), Vinay and Lei (2020), Muhammad and Hina (2020), and Lin et al. (2020) performed better with more than 90% accuracy. These studies have their respective limitations as depicted in Table 2. Despite the above‐mentioned limitations, AI models contribute significantly amid COVID‐19 pandemic. Table 2 shows that China is the leading country that has applied AI models for detecting, monitoring, diagnosing, screening, surveillance, mapping and tracking COVID‐19. This might be attributed to the availability of COVID‐19 datasets.
4.2. Application of IoMT in fighting COVID‐19 pandemic
IoMT involves the application of Internet of Things (IoT) concepts, tools, and principles in health and medical domains through interconnected medical equipment, smart health applications, and smart sensors (Swati & Chandana, 2020). It also consists of developing smart applications and smart wearable devices specifically for improving health care delivery. During the COVID‐19 pandemic, the IoMT changes how healthcare services are delivered, shifting physical contact to remote health service delivery due to restricted mobility. This is evident by several IoMT applications that are integrated into health systems to reduce the burden on the healthcare systems. These IoMT applications are depicted in Table 3. Several countries including the USA, China, India, Israel, Poland, Croatia, Canada, Bahrain, Singapore, Australia, Colombia, Ghana, and Austria implemented telemedicine strategies such as live webinars, remote consultation, and video conferencing; telehealth and smart thermometers to fight COVID‐19 pandemic (Vinay, Vikas, Vatsal, & Mohsen, 2020). These countries implemented IoMT applications to improve real‐time COVID‐19 data access as depicted in Table 3. The IoMT applications are used to:
TABLE 3.
Applications of IoMT in fighting COVID‐19 pandemic
| Author(s) | IoMT applications | Activities | Country |
|---|---|---|---|
| (Li et al., 2020a, 2020b) | nCapp |
|
China |
| (Nasajpour et al., 2020) | DetectaChem |
|
USA |
| (Nataliya & Nadezhda, 2020) | Social Monitoring |
|
Russia |
| (Nasajpour et al., 2020) | Selfie app |
|
Poland |
| (Kirsten et al., 2020) | Stop Corona |
|
Croatia |
| (Vinay & Lei, 2020) | Civitas |
|
Canada |
| (Nasajpour et al., 2020) | BeAware Bahrain |
|
Bahrain |
| (Benny & Eyal, 2020) | Hamagen |
|
Israel |
| (Cho, Daphne, & Yun, 2020) | TraceTogether |
|
Singapore |
| (Columbian National Institute of Health, 2020) | CoronApp |
|
Colombia |
| (David, 2020a, 2020b) | COVIDSafe |
|
Australia |
| (Kwabena & Shankar, 2020) | GH Covid‐19 Tracker |
|
Ghana |
| (Thiele, 2020) | Stopp Corona |
|
Austria |
Establish an online COVID‐19 real‐time update database
Real‐time updating of models of COVID‐19 diagnosis
Guide healthcare professionals to administer COVID‐19 treatment
Provide consultation services through front‐line healthcare professionals
Tracking of COVID‐19 patients who are on diagnosis
Mapping of COVID‐19 hotspots areas
Create COVID‐19 awareness by frequently sending notification on contact‐persons, signs, and symptoms and location
Blockchain safety system that associates person's identification with blockchain records to determine whether he/she is allowed to move out from the quarantine facility, hence, minimizing the risk
Securing electronic medical records using blockchain‐based and IoMT concepts
Despite the benefits of the IoMT in fighting COVID‐19 pandemic, its implementation faces some challenges and limitations. Such limitations include:
-
j.
Standardization of COVID‐19 dataset
-
k.
COVID‐19 data interoperability issues caused by heterogeneous data format and size
-
l.
Sharing of COVID‐19 data may breach privacy and security of the individual data
-
m.
Malicious attack of healthcare equipment could be a major drawback in interconnected IoMT infrastructure.
-
n.
Heterogeneous network protocols and smart applications could delay the implementation of IoMT in fighting COVID‐19 pandemic
4.3. Applications of Blockchain in fighting COVID‐19 pandemic
Blockchain is continuous becoming recognized in various domains including healthcare systems and biomedical in securing records among two parties to improve data security by validating whether the transactions happed or not (Antonio et al., 2020; Tivani & Ellen, 2020). There is limited evidence on the implementation of Blockchain to fight COVID‐19 pandemic. However, blockchain technology has been implemented in Canada in an application called Civitans (Vinay et al., 2020). IBM also developed a blockchain application called MiPasa, to enforce security when sharing and streaming health data and location on IBM cloud platforms as depicted in Table 4. In fighting COVID‐19, healthcare professionals, individuals can utilize these blockchain applications to ensure security and privacy of health data.
TABLE 4.
Applications of Blockchain in fighting COVID‐19 pandemic
| Author(s) | Blockchain app | Functions/Activities | Country |
|---|---|---|---|
| (Vinay et al., 2020) | Civitas |
|
Canada |
| (Vinay & Lei, 2020) | MiPasa |
|
IBM cloud |
Challenges of implementing blockchain technology in health systems are attributed to:
Lack of technical skills to integrate existing blockchain Application programming interface (API) with health information systems
Lack of awareness about the potential of blockchain in the health systems
Scalability problems since the APIs are provided by a third party
Integrating blockchain into health systems is still a challenge because of some ethical issues and the technology being relatively new and immature
Unclear WHO regulations and standards on the integration of blockchain technology in health systems
Data leakage through blockchain API and cloud‐based platforms threaten its adoption in health systems
4.4. 5G cellular technology and smart applications
The 5G technology provides the fastest internet speed and high bandwidth which is crucial for real‐time communication. During COVID‐19, this technology plays a vital role in public health management that adopted health smart applications, big data services, and the Internet of Medical Things (Karthikeyan, Upadhyaya, Vaishya & Jain, 2020). Besides the 5G conspiracy theory, there is greater realization and wider understanding of the benefits of 5G technology such as low latency, high‐speed transmission and sharing of COVID‐19 health data and reliability. For instance, installation of 5G technology in China overcame the challenges in containing the spread of COVID‐19 through remote consultation in many hospitals, smart cameras connected with 5G technology, smart thermometers (noncontact forehead infrared digital thermometer), intelligent disinfection unmanned vehicles, intelligent medical robot taking swabs and high speed live broadcast (Ouyang, 2020). 5G technology is slowly rolled out in China and the USA but it also faces challenges such as:
5G technology requires huge capital injections and overcome the bandwidth, latency, and flexibility issues inherent to the current network technology
Integration of smart applications into health systems could cause a breach of health privacy
5G is still at its nascent, and may not be supported with the existing networking infrastructure
No WHO guidelines on health data shared and transmitted through 5G technology
In some countries, the adoption of 5G technology is still debatable after its conspiracy theory and misconception (Wasim, Josep, Joseph, & López, 2020)
4.5. Applications of virtual reality in fighting COVID‐19 pandemic
Virtual reality technology has been in existence since the late 1990s but it was not fully explored up until the interest slowly faded away due to a yawning gap between public expectations and technological limitations (Virtual Reality Society, 2017). Virtual reality technological limitations including size, Nausea, dizziness, temporarily impaired vision and lack in the sense of presence were reported as adverse effects in the late 1990s (Panteleimon et al., 2017). The recent breakthrough in digital transformation such as motion detection, interactive display systems, and kinaesthetic communication brought an evolution in virtual reality technology which reached notable milestones in medical education. Virtual reality applications overcome cognitive and psychological impediments, impairments, and present unprecedented opportunities in COVID‐19 medical education and training (Javaid & Abid, 2020). Virtual reality technology provides an interactive, artificial three‐dimensional computer‐generated world that simulates physical reality in a virtual setting (Brenda, 2006). This could be utilized in training and education of healthcare professionals as it supports nonphysical contact and social distancing. The users of the virtual reality technology engage themselves with the system through the interface of the VR's input and out devices which perceive sensory information similar to the real‐world. The virtual reality technology consists of headsets integrated with input sensors which are programmed to display emotions in a virtual environment. The immersive VR system provides many facets of visual, auditory and tactile sensory fastened on Head‐Mounted Display (HMD) or Head‐Coupled Display (HCD) to ensure intrinsic experience in a safe virtual environment (Zhang, 2017). The HCD and HMD devices are more dominant in the market because of their intrinsic properties such as portability and miniaturization. These properties help health workers and community participation amid COVID‐19 prevention, awareness, education, and training to improve their knowledge, skills, mobility, and cognitive abilities to improve quality of care. The integration of immersive virtual reality and e‐learning platforms allow students in learning institutions to explore virtual 3‐dimensional COVID‐19 virus, anatomical positions and visualize how it is transmitted in a way that is impossible and difficult in physical reality. This may also help to create awareness in schools, colleges and universities. Also, virtual reality can be used for counseling people affected with COVID‐19 and experiencing mental health issues such as trauma, anxiety, psychological distress, panic, and other stress‐related psychopathological symptoms (Mohd et al., 2020).
However, the adoption of virtual reality in education and training encounters face some limitations and barriers despite its tremendous opportunities and benefits. High cost and computing power to simulate the realistic virtual environment are some of the major limitations of employing virtual reality in medical education especially low‐income countries (Brian, 2017). Even though Google Cardboard manufactured affordable virtual reality devices but due to poor supporting infrastructure and slow internet speed threatens the full realization of virtual reality technology, hence the need for 5G technology to improve internet speed. This is another drawback to adopt VR in medical education. Another limitation is the lack of technical virtual reality experts to build virtual reality applications and virtual worlds that best suit the classroom setup (Kleinermann et al., 2017). It is also time‐consuming to train healthcare professionals, patients and COVID‐19 task team how to use VR devices. For instance, images and text can blurry if the head‐mounted virtual reality devices are improperly adjusted, and the additional cognitive load of learning how to navigate virtual world requires more time for healthcare educators to plan their lessons and time to teach learners how to use the VR devices and applications (Hsin‐Kai, Silvia, Hsin‐Yi, & Jyh‐Chong, 2013; Hussein & Nätterdal, 2015).
4.6. Application of geographic information systems and global positioning system to fight COVID‐19 pandemic
Geographic information systems (GIS) and global positioning system (GPS) applications can provide real‐time mapping, tracking and combating COVID‐19 pandemic. These emerging technologies act as communication tools blossomed over a certain period and they have applied to model disaster management, understand, and tracking infectious diseases such as Malaria, Ebola, Cholera, and yellow fever.
For instance, Mukhopadhyay (2015) and Chatterjee, Suman, Sujit, and Shanta (2020) applied GPS to map cholera cases using satellite‐based recording systems to understand cholera preventive measures by providing coordinates of households and insights on how people interact with the environment. GIS tools can map and visualize the relationship between location coordinates and COVID‐19 pandemic cases to map hot spots. Amid COVID‐19 pandemic, GIS tools are paramount to analyze and visualize the spread of COVID‐19. For example, Johns Hopkins University Center for Systems Science and Engineering uses ArcGIS Online to track the spread of COVID‐19 (Maged & Estella, 2020a, 2020b), WHO also implements ArcGIS Operations Dashboard to map outbreak source (Abolfazl, Behzad, & Kiara, 2020), USA utilizes HealthMap to collate COVID‐19 data and alert people living around or near COVID‐19 confirmed cases (Ensheng, Hongru, & Lauren, 2020). GIS tools such as “close contact detector” app in China, support big data and IoT data processing tools that analyze people's migration patterns and make informed decisions (Maged & Estella, 2020a, 2020b). GIS and GPS applications can also be very useful to:
Provide real‐time COVID‐19 geolocated updates
Mapping of public events that violate social distancing and the restricted number of people
Distribute of resources through digital supply chain maps to ensure effective allocation of COVID‐19 PPEs and medicines
Spatial segmentation and dynamic mapping for COVID‐19
Determine COVID‐19 transmission risk factors such as socio‐economic and environmental variables
However, the application of GIS applications to fight COVID‐19 is influenced by the following challenges: (1) limited access to spatial COVID‐19 data for spatial mapping and visualization, (2) requires change of regulations to track contact‐persons.
5. CONCLUSION
Despite all the significant progress in the application of emerging technologies in compacting COVID‐19, there is still a need for further implementation of these technologies for detecting, monitoring, diagnosing (Tsikala et al., 2020), screening, surveillance, mapping, tracking, and creating awareness (Aishwarya, Puneet, & Ankita, 2020). The size, availability and accessibility to COVID‐19 data improve performance of AI models, GIS concepts, and IoMT applications. Future work should focus on strengthening the current technologies and there is a strong need for the emergence of a robust computationally intelligent model for early differential diagnosis of COVID‐19. Also, the future work should focus on the ethical framework and acceptable use of emerging technologies when tackling COVID‐19 pandemic while observing the security and privacy of people's data.
CONFLICT OF INTEREST
The authors declare no potential conflict of interest.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1002/hbe2.237.
Biographies
Elliot Mbunge is a Lecturer in the Department of Computer Science at the University of Eswatini (formerly the University of Swaziland), Kwaluseni, Eswatini. He is a holder of BSc, MSc, and currently pursuing his PhD in the field of Information Technology with Durban University of Technology, South Africa. He is a member of IEEE and Computational Intelligence and Health Informatics Research Group in the Department of Computer Science at the University of Eswatini. His research interests are in ICT for development, health informatics, soft computing, deep learning, and machine learning.

Boluwaji Akinnuwesi is working in the Department of Computer Science in the Faculty of Science and Engineering at the University of Eswatini (formerly University of Swaziland), Kwaluseni, Eswatini. He obtained his degrees (BSc, MSc, and PhD) in Computer Science. He focuses on Software Engineering and Intelligence‐based Medicine and the applications. He applies software development methodologies, soft computing, and machine learning techniques to model and solves real‐life problems. He has developed several software frameworks for solving some life problems. He is a full member of the following professional bodies: Computer Professional Registration Council of Nigeria, Nigeria Computer Society and Association of Computing Machinery IAENG, and Computational Intelligence and Health Informatics Research Group. He has vast experience in the computing field including software development (engineering), soft computing, deep learning, and machine learning techniques.

Stephen G. Fashoto is currently a Senior Lecturer in the Department of Computer Science in University of Swaziland, Kwaluseni, Swaziland. He was also a Lecturer in the Department of Computer Science in Redeemer's University, Ede, Osun State, Nigeria between 2007 and 2014. He obtained his B.Sc. (Honours) in Computer Science & Mathematics and MSc in Computer Science both from the University of Port Harcourt, Nigeria and PhD in Computer Science from University of Ilorin, Nigeria. He has over 15 years of teaching and research experience at the university. His research interests are in Computer Science Education, Machine Learning, and Computational Intelligence, Health informatics, Data mining, and application of optimization techniques. He is the Chair of the Computational Intelligence and Health Informatics Research Group in the Department of Computer Science at the University of Eswatini.

Andile S. Metfula is a Senior Lecturer and the Head of the Computer Science Department housed under the Faculty of Science and Engineering in University of Eswatini (formerly the University of Swaziland), Kwaluseni, Eswatini (formerly Swaziland). He has a PhD from the University of Cape Town (South Africa), MSc from Rensselaer Polytechnic Institute (USA) and BSc from the University of Swaziland (now the University of Eswatini). His passion is in Information Systems and Innovation. In the past few years, his team in the Department has been able to organize the first‐ever ICT Fair in the country.

Petros Mashwama is currently lecturing in the Department of Computer Science in the University of Eswatini, Eswatini (formerly Swaziland). He has served as a Tutor of the Faculty of Science in the same University between 1997 and 2005, and as the Head of the Department of Computer Science between 2005 and 2012, at the same time, he was roped into the national panel of Scientists that manage the Science curriculum of High Schools in the Kingdom of Eswatini. He obtained his BSc degree in Mathematics and Physics in 1986, the University of Swaziland (now Eswatini). In 1988, he obtained his Master's degree in Computer Science (Conversion programme) in Dundee, Scotland (UK). He returned to the UK, the University of Leeds in 1992 to start his PhD, which he graduated in 1996. His research interests are in Computer Graphics, Computer Science Education, and Machine Learning.

Mbunge E, Akinnuwesi B, Fashoto SG, Metfula AS, Mashwama P. A critical review of emerging technologies for tackling COVID‐19 pandemic. Hum Behav & Emerg Tech. 2021;3:25–39. 10.1002/hbe2.237
DATA AVAILABILITY STATEMENT
Not applicable
REFERENCES
- Abdelhafid, Z. , Fouzi, H. , Abdelkader, D. , & Ying, S. (2020). Deep learning methods for forecasting COVID‐19 time‐Series data: A Comparative study. Chaos, Solitons & Fractals, 140, 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abhimanyu, S. , Vineet, P. , & Oge, M. (2020). Artificial intelligence and COVID‐19: A multidisciplinary approach. Integrative Medicine Research, 9(3), 111–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abolfazl, M. , Behzad, V. , & Kiara, M. (2020). GIS‐based spatial modeling of COVID‐19 incidence rate in the continental United States. Science of the Total Environment, 728(1), 67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agbehadji, I. E. , Bankole, O. A. , Alfred, B. , & Richard, C. M. (2020). Review of big data analytics, artificial intelligence and nature‐inspired computing models towards accurate detection of COVID‐19 pandemic cases and contact tracing. International Journal of Environmental Research and Public Health, 17(15), 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aishwarya, K. , Puneet, K. , & Ankita, S. (2020). A review of modern technologies for tackling COVID‐19 pandemic. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 14(4), 569–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alfonso Rodriguez‐Morales, A. J., Cardona‐Ospina, J. A., Gutiérrez‐Ocampo, E., Villamizar‐Peña, R., Holguin‐Rivera, Y., Escalera‐Antezana, J. P. … Paniz‐Mondolfi, A. (2020). Clinical, laboratory and imaging features of COVID‐19: A systematic review and meta‐analysis. Travel Medicine and Infectious Disease, 34(12), 1333–1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antonio, C. , Ruggeri, A. , Fazio, M. , Galletta, A. , Villari, M. , & Romano, A. (2020). Blockchain‐based healthcare workflow for tele‐medical laboratory in federated hospital IoT clouds. Sensors, 20(9), 2590–2600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arni, S. R. S. R. , & Jose, A. V. (2020). Identification of COVID‐19 can be quicker through artificial intelligence framework using a mobile phone–based survey when cities and towns are under quarantine. Infection Control & Hospital Epidemiology, 41(7), 826–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benny, P. & Eyal, R. (2020). A proposal for a privacy‐preserving bluetooth based contact tracing scheme for hamagen . Available from https://www.cs.technion.ac.il/~biham/Workshops/Cyberday/2020/Slides/benny-pinkas.slides.pdf.
- Boulos, M. K. , & Estella, M. G. (2020). Geographical tracking and mapping of coronavirus disease COVID‐19/severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) epidemic and associated events around the world: how 21st century GIS technologies are supporting the global fight against outbr. International Journal of Health Geographics, 19(8), 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenda, W. (2006). The potential for virtual reality to improve health care. The Virtual Reality Medical Center.
- Brian, B. (2017). Available from https://www.usma.edu/cfe/Literature/Boyles_17.pdf.
- Chatterjee, P. , Suman, K. , Sujit, K. , & Shanta, D. (2020). Mapping cholera outbreaks and antibiotic resistant Vibrio cholerae in India: An assessment of existing data and a scoping review of the literature. Vaccine, 38(1), A93–A104. [DOI] [PubMed] [Google Scholar]
- Cho, H. , Daphne, I. , & Yun, W.Y. . (2020). Contact tracing mobile apps for COVID‐19: Privacy considerations and related trade‐offs. Arxiv, pp. 1–12.
- Chuansheng, Z., Xianbo, D., Qing, F., Qiang, Z., Jiapei, F., Hui, M., … Xinggang, W. (2020). Deep learning‐based detection for COVID‐19 from chest CT using weak label. Medrxiv, pp.1–13.
- Cohen, J. (1968). Weighted kappa: Nominal scale agreement provision for scaled disagreement or partial credit. Psychological Bulletin, 70(4), 213–220. [DOI] [PubMed] [Google Scholar]
- Columbian National Institute of Health . (2020). CORONAPP. Available from https://coronaviruscolombia.gov.co/Covid19/aislamiento-saludable/coronapp.html.
- David, W. (2020a). COVIDSafe, Australia’s Digital Contact Tracing App: The Legal Issues. SSRN Electronic Journal, 12(10), 1–13. 10.2139/ssrn.3591622. [DOI] [Google Scholar]
- David, L. (2020b). Tackling COVID‐19 through responsible AI innovation: Five steps in the right direction. Harvard Data Science Review, 5(1), 4–15. [Google Scholar]
- Elliot, M. (2020). Integrating emerging technologies into COVID‐19 contact tracing: Opportunities, challenges and pitfalls. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 14(6), 1631–1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliot, M. , Fanwell, V. , & Kinsley, K. (2018). A tool to predict the possibility of social unrest using sentiments analysis‐case of Zimbabwe politics 2017‐2018. International Journal of Science and Research, 6(10), 1541–1545. [Google Scholar]
- Ensheng, D. , Hongru, D. , & Lauren, G. (2020). An interactive web‐based dashboard to track COVID‐19 in real time. The Lancet, 20(5), 533–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fatima, M. S. , Abu‐Naser, S. S. , Alajrami, E. , Abu‐Nasser, B. S. , & Alashqar, B. A. (2020). COVID‐19 Detection using Artificial Intelligence. International Journal of Academic Engineering Research, 4(3), 18–25. [Google Scholar]
- Gozes, O., Frid‐Adar, M., Greenspan, H., Browning, P.D., Zhang, H., Ji, W., … Siegel, E. (2020). Rapid AI development cycle for the coronavirus (COVID‐19) pandemic: Initial results for automated detection & patient monitoring using deep learning CT image analysis. Arvix, pp.1–120.
- Greiner, A. L. , Angelo, K. M. , McCollum, A. M. , Mirkovic, K. , Arthur, R. , & Angulo, F. J. (2015). Addressing contact tracing challenges—critical to halting Ebola virus disease transmission. International Journal of Infectious Diseases, 41(12), 53–55. [DOI] [PubMed] [Google Scholar]
- Hameni, N. , Bowong, S. , Tewa, J. J. , & Kurths, J. (2020). Short‐term forecasts of the COVID‐19 pandemic: study case of Cameroon. Chaos, Solitons & Fractals, 2020, 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harold, T. (2013). Technology and the Future of Healthcare. Journal of Public Health Research, 3(e28), 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsin‐Kai, W. , Silvia, W.‐Y. L. , Hsin‐Yi, C. , & Jyh‐Chong, L. (2013). Current status, opportunities and challenges of augmented reality in education. Computers and Education, 62, 41–49. [Google Scholar]
- Hu, Z. , Song, C. , Xu, C. , Jin, G. , Chen, Y. , Xu, X. , … Shen, H. (2020). Clinical characteristics of 24 asymptomatic infections with COVID‐19 screened among close contacts in Nanjing, China. Science China Life Sciences, 63(5), 706–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussein, M. & Nätterdal, C. . (2015). The benefits of virtual reality in education—A comparision study. Semantic Scholar .
- Javaid, M. , & Abid, H. (2020). Virtual reality applications toward medical field. Clinical Epidemiology and Global Health, 8(2), 600–605. [Google Scholar]
- Javaid, M. , Haleem, A. , Vaishya, R. , Bahl, S. , Suman, R. , & Vaish, A. (2020). Industry 4.0 technologies and their applications in fighting COVID‐19 pandemic. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 14(4), 419–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karthikeyan, I. , Gaurav, K. , Raju, V. , & Vijay, J. (2020). COVID‐19 and applications of smartphone technology in the current pandemic. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 14(5), 733–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirsten, B., Kühne, C. R., Mühlhoff, R., Ost, M. R., Pohle, J. & Rehak, R. (2020). Data protection impact assessment for the corona app. SSN, pp. 6–97.
- Kitchenham, B. (2004). Procedures for performing systematic reviews . Available from http://www.inf.ufsc.br/~aldo.vw/kitchenham.pdf.
- Kleinermann, F., De Troyer, O., Mansouri, H., Romero, R., Pellens, B. & Bille, W. (2017). Designing semantic virtual reality applications. Citeseerx .
- Kwabena, A. , & Shankar, K. (2020). Application of geospatial technologies in the COVID‐19 fight of Ghana. Transactions of the Indian National Academy of Engineering, 5, 193–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, B., Yang, D., Wang, X., Tong, L., Zhu, X., Zhong, N., … Song, Y. (2020a). Chinese experts' consensus on the internet of things‐aided diagnosis and treatment of coronavirus disease 2019 (COVID‐19). Clinical eHealth, 3, 7–15. [Google Scholar]
- Li, Y., Zhang, H.T., Goncalves, J., Xiao, Y., Wang, M., Guo, Y., … Huang, X. (2020b). An interpretable mortality prediction model for COVID‐19 patients. Nature Machine Intelligence, 2(2), 283–288. [Google Scholar]
- Lin, L., Qin, L., Xu, Z., Yin, Y., Wang, X., Kong, B., … Cao, K. (2020). Artificial intelligence distinguishes COVID‐19 from community acquired pneumonia on chest CT. Radiology, 30(16), 50–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu, H., Han, R., Ai, T., Yu, P., Kang, H., Tao, Q., & Xia, L. (2020). Serial quantitative chest CT assessment of COVID‐19: Deep‐learning approach. Radiology: Cardiothoracic Imaging, 2(2), e200075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maged, N. B. , & Estella, M. G. (2020a). Geographical tracking and mapping of coronavirus disease COVID‐19/severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) epidemic and associated events around the world: How 21st century GIS technologies are supporting the global fight against outbr. International Journal of Health Geographics, 19(8), 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maged, N. K. , & Estella, M. G. (2020b). Geographical tracking and mapping of coronavirus disease COVID‐19/severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) epidemic and associated events around the world: How 21st century GIS technologies are supporting the global fight against outbr. International Journal of Health Geographics, 19(8), 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matheus, H. D. M. , Ramon, G. S. , Viviana, C. , & Leandro, D. S. (2020). Short‐term forecasting COVID‐19 cumulative confirmed cases: Perspectives for Brazil. Chaos, Solitons & Fractals, 135(34), 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mbunge, E. (2020). Effects of COVID‐19 in South African health system and society: An explanatory study. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 14(6), 1809–1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehtar, S. , Wolfgang, P. , Ndèye, A. L. , & Abdoulaye, B. (2020). Limiting the spread of COVID‐19 in Africa: one size mitigation strategies do not fit all countries. The Lancet Global Health, 8(7), E881–E883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohammad, N., Pouriyeh, S., Parizi, R. M., Dorodchi, M., Valero, M., & Arabnia, H. R. (2020). Internet of Things for Current COVID‐19 and Future Pandemics: an Exploratory Study. Journal of Healthcare Informatics Research, 4(4), 325–364. 10.1007/s41666-020-00080-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohd, J. , Haleem, A. , Vaishya, R. , Bahl, S. , Suman, R. , & Vaish, A. (2020). Industry 4.0 technologies and their applications in fighting COVID‐19 pandemic. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 14(4), 419–422. 10.1016/j.dsx.2020.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muhammad, I. , Hina, R. & Amine, N.‐A. (2020). Detection of Covid‐19 from chest X‐ray images using artificial intelligence: An early review. Arxiv, pp.1–18.
- Mukhopadhyay, A. (2015). Mapping of cholera cases using satellite based recording systems to investigate the outbreak. The Indian Journal of Medical Research, 142(5), 509–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasajpour, M., Pouriyeh, S., Parizi, R. M., Dorodchi, M., Valero, M., & Arabnia, H. R (2020). Internet of Things for Current COVID‐19 and Future Pandemics: an Exploratory Study. Journal of Healthcare Informatics Research, 4(4), 325–364. 10.1007/s41666-020-00080-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nataliya, S. , & Nadezhda, B. (2020). How soviet legacies shape Russia's response to the pandemic: Ethical consequences of a culture of non‐disclosure. KIE Journal, 12(3), 22–32. [Google Scholar]
- Ouyang, R. (2020). 5G's indispensable role in China's fight against COVID‐19 . Available from https://news.cgtn.com/news/2020-07-09/5G-s-indispensable-role-in-China-s-fight-against-COVID-19-RXRu9TlZ9S/index.html.
- Panteleimon, P., Chorti, A., Papagiouvanni, I., Paparoidamis, G., Drosos, C., Panagiotakopoulos, T., … Sideris, M. (2017). Virtual and augmented reality in medical education. intechopen, pp. 78–96.
- Raju, V. , Mohd, J. , HaleemKhan, I. , & Abid, H. (2020). Artificial Intelligence (AI) applications for COVID‐19 pandemic. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 14(4), 337–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarbjit, S. , Parmar, K. S. , Makkhan, S. J. S. , Kaur, J. , Peshoria, S. , & Kumar, J. (2020). Study of ARIMA and least square support vector machine (LS‐SVM) models for the prediction of SARS‐CoV‐2 confirmed cases in the most affected countries. Chaos, Solitons & Fractals, 139, 110086. 10.1016/j.chaos.2020.110086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sera, W. , Mamas, A. M. , Eric, T. , & Harriette, G. C. V. S. (2020). Applications of digital technology in COVID‐19 pandemic planning and response. The Lancet, 2(8), 435–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swati, S. , & Chandana, M. (2020). Application of cognitive Internet of Medical Things for COVID‐19 pandemic. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 14(5), 911–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiele, C. (2020). Stop Corona–Theses and antitheses on the use of tracking apps in the corona crisis. Journal of Information Law, 7(2), 152–158. [Google Scholar]
- Tivani, P. M.‐T. , & Ellen, D. C. (2020). Blockchain and artificial intelligence technology for novel coronavirus disease 2019 self‐testing. Diagnostics, 10(4), 198–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsikala Vafea, M. , Atalla, E. , Georgakas, J. , Shehadeh, F. , Mylona, E. K. , Kalligeros, M. , & Mylonakis, E. (2020). Emerging Technologies for Use in the Study, Diagnosis, and Treatment of Patients with COVID‐19. Cellular and Molecular Bioengineering, 13(4), 249–257. 10.1007/s12195-020-00629-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinay, C. , Vikas, H. , Vatsal, G. , & Mohsen, G. (2020). A comprehensive review of the COVID‐19 pandemic and the role of IoT, Drones, AI, Blockchain, and 5G in Managing its. IEEE Access, 8, 1–41. [Google Scholar]
- Vinay, K.R. & Lei, Z. (2020). Time series forecasting of COVID‐19 transmission in Canada using LSTM networks. Chaos, Solitons & Fractals, 135. [DOI] [PMC free article] [PubMed]
- Virtual Reality Society . (2017). How did virtual reality begin? Available from https://www.vrs.org.uk/virtual-reality/who-coined-the-term.html.
- Wang, L. , Alexander, W. & Zhong, Q.L. (2020). COVID‐Net: A tailored deep convolutional neural network design for detection of COVID‐19 cases from chest X‐ray images. Arvix, pp. 1–14. [DOI] [PMC free article] [PubMed]
- Wasim, A. , Josep, V.‐A. , Joseph, D. , & López, S. (2020). COVID‐19 and the 5G conspiracy theory: Social network analysis of Twitter data. Journal of Medical Internet Research, 22(5), e19458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitworth, J. (2020). COVID‐19: a fast evolving pandemic. Transactions of the Royal Society of Tropical Medicine and Hygiene, 114(4), 241–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . (2020). COVID‐19 strategy update . Available from https://www.who.int/docs/default-source/coronaviruse/covid-strategy-update-14april2020.pdf?sfvrsn=29da3ba0_19.
- Wim, N. (2020). Artificial intelligence vs COVID‐19: limitations, constraints and pitfalls. Springer Nature, 23(10), 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worldometers . (2020). Coronavirus cases . Available from https://www.worldometers.info/coronavirus/.
- Wu, D. , Tiantian, W. , Qun, L. , & Zhicong, Y. (2020). The SARS‐CoV‐2 outbreak: What we know. International Journal of Infectious Diseases, 94(8), 44–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xueyan, M., Lee, H. C., Diao, K.Y., Huang, M., Lin, B., Liu, C., … Bernheim, A. (2020). Artificial intelligence–enabled rapid diagnosis of patients with COVID‐19. Nature Medicine, 26(10), 1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, H. (2017). Head‐mounted display‐based intuitive virtual reality training system for the mining industry. International Journal of Mining Science and Technology, 27(4), 717–722. [Google Scholar]
- Zhao, X.‐Y. , Xu, X. X. , Yin, H. S. , Hu, Q. M. , Xiong, T. , Tang, Y. Y. , … Huang, Z. P. (2020). Clinical characteristics of patients with 2019 coronavirus disease in a non‐Wuhan area of Hubei Province, China: A retrospective study. BMC Infectious Diseases, 20(311), 311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng, J. (2020). SARS‐CoV‐2: An emerging coronavirus that causes a global threat. International Journal of Biological Sciences, 16(10), 1678–1685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zixin, H., Ge, Q., Jin, L. & Xiong, M. (2020). Artificial intelligence forecasting of Covid‐19 in China. Arxiv, 34(15), 1–20. [Google Scholar]
- Zohair, M. , Atlam, E.‐S. , Hassanien, A. E. , Dagnew, G. , Elhosseini, M. A. , & Gad, I. (2020). Association between weather data and COVID‐19 pandemic predicting mortality rate: Machine learning approaches. Chaos, Solitons & Fractals, 138, 110137. 10.1016/j.chaos.2020.110137. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable


