ABSTRACT
BACKGROUND AND PURPOSE
The effect of coronavirus disease 2019 (COVID‐19) pandemic on performance of neuroendovascular procedures has not been quantified.
METHODS
We performed an audit of performance of neuroendovascular procedures at 18 institutions (seven countries) for two periods; January‐April 2019 and 2020, to identify changes in various core procedures. We divided the region where the hospital was located based on the median value of total number of COVID‐19 cases per 100,00 population‐into high and low prevalent regions.
RESULTS
Between 2019 and 2020, there was a reduction in number of cerebral angiograms (30.9% reduction), mechanical thrombectomy (8% reduction), carotid artery stent placement for symptomatic (22.7% reduction) and asymptomatic (43.4% reduction) stenoses, intracranial angioplasty and/or stent placement (45% reduction), and endovascular treatment of unruptured intracranial aneurysms (44.6% reduction) and ruptured (22.9% reduction) and unruptured brain arteriovenous malformations (66.4% reduction). There was an increase in the treatment of ruptured intracranial aneurysms (10% increase) and other neuroendovascular procedures (34.9% increase). There was no relationship between procedural volume change and intuitional location in high or low COVID‐19 prevalent regions. The procedural volume reduction was mainly observed in March‐April 2020.
CONCLUSIONS
We provided an international multicenter view of changes in neuroendovascular practices to better understand the gaps in provision of care and identify individual procedures, which are susceptible to change.
Keywords: COVID‐19, corona virus, neuroendovascular procedures, carotid stent, mechanical thrombectomy
Introduction
An estimated 182,485 and 269,383 patients with ischemic stroke and coronavirus disease 2019 (COVID‐19) may be diagnosed, assuming that 9,988,254 patients were infected with Covid‐19 in the world on June 27, 2020, with an estimated 21‐31% of patients required hospitalization. 1 Some procedures, such as mechanical thrombectomy for acute ischemic stroke, carotid angioplasty, and stent placement, were expected to increase with increasing numbers of acute ischemic stroke patients. 1 Paradoxically, there was a decrease in the early phase of the pandemic in some centers. 2 Certain elective procedures are likely to decrease 3 due to declining hospital visits. A 32‐60% decrease between March 1 and 29, compared against pre‐COVID‐19 volumes, was reported in an analysis of more than 500 hospitals in the United States of America (USA). 4 One of the research priorities identified by an international panel 1 was changes in aspects of care for patients with cerebrovascular diseases during the COVID‐19 pandemic to better understand the unmet needs and guide resource allocation.
Methods
The study was performed as a collaborative effort between 11 institutions from the USA and 7 international institutions (from Egypt, China, Turkey, South Korea, France each, and two from Poland). All investigators who were a part of an internal collaboration developed to form guidelines for management of acute ischemic stroke in patients with COVID‐19, were invited to the study. 1 , 5 Additional centers were added based on referral of original investigators. Each institution provided data for number of practitioners (including fellows), number of cerebral angiograms, mechanical thrombectomy for acute ischemic stroke, carotid stent placement for internal carotid artery (ICA) stenosis separated by symptomatic and asymptomatic ICA stenosis, endovascular treatment of intracranial aneurysms, separated by ruptured and unruptured status, endovascular treatment of brain arteriovenous malformations (BAVMs), separated by ruptured and unruptured status, intracranial angioplasty and/or stent placement, other neuroendovascular (spinal angiogram and WADA) and nonendovascular (vertebroplasty, lumbar puncture, and lumbar catheter placement) procedures. The neuroendovascular procedures were selected as they have been used in previous studies of benchmarking procedural capability. 6 , 7 , 8 The data were provided for each month for a total of 8 months; January‐April 2019 and January‐April 2020. All sites except two provided data on number of patients who underwent procedures and had either suspected or confirmed COVID‐19 at time of procedure.
Statistical Analysis
The analysis was predominantly descriptive. The changes were quantified for each period as percentage change in 2020 using the values from 2019 as denominator. We further estimated the change for January and February in 2020 (early phase) and March and April 2020 (established phase for COVID‐19 pandemic). The median number of each procedure per center for the period under study was compared between 2019 and 2020 using quantile regression method. We divided the region where the hospital was located based on the median value of number of COVID‐19 cases per 100,00 population on April 30th, 2020 into high and low prevalent regions with values above the median considered as high prevalence and values below as low prevalence. All analysis was performed using SAS studio (Release: 3.8; Enterprise Edition) software.
Results
A total of 9,738 procedures were performed during the two study periods, 5,539 during pre‐COVID‐19 period in 2019 and 4,199 in 2020. There was a decrease in the total number of practitioners from 759 to 589 in pre‐COVID‐19 and during COVID‐19 periods. The average number of procedures per practitioner decreased from 7.29 to 7.12 in pre‐COVID‐19 and during COVID‐19 periods. Fifty‐three patients with confirmed COVID‐19 infection and 135 with suspected COVID‐19 infection underwent procedures during COVID‐19 period. The procedure numbers are presented for each neuroendovascular procedure for each month in Figure 1.
Fig 1.
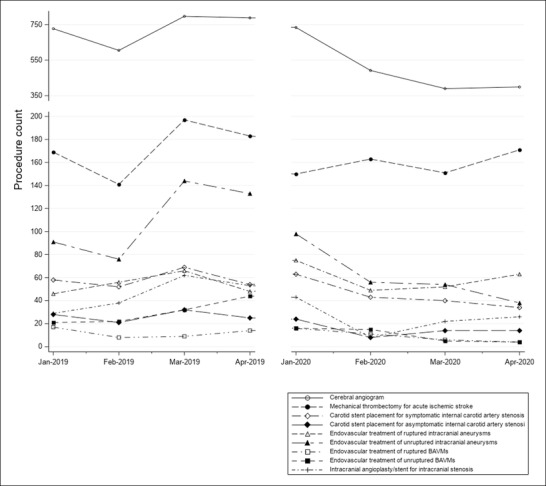
Procedure numbers are presented for each neuroendovascular procedure for each month.
Overall Comparison of Pre‐COVID‐19 and During COVID‐19 Periods
Between 2019 and 2020, there were reductions in cerebral angiograms (30.9%), mechanical thrombectomies (8%), carotid stent placement for symptomatic (22.7%) and asymptomatic (43.4%) ICA stenoses, and intracranial angioplasty and/or stent placements (45%), treatment of unruptured intracranial aneurysms (44.6%) and ruptured (22.9%), and unruptured (66.4%) BAVMs. There were increases in endovascular treatment of ruptured intracranial aneurysms (10%) and other neuroendovascular procedures (34.9%). The slight increase in endovascular treatment of ruptured intracranial aneurysms was more prominent in low COVID‐19 prevalent regions and non‐USA institutions (Table 1).
Table 1.
Neuroendovascular Procedures for January‐April 2019 and 2020
| Study or subgroup | Total number in 2019 | Total number in 2020 | Change % |
Median number in 2019 (95% confidence interval) |
Median number in 2020 (95% confidence interval) |
Quantile regression P‐value |
|---|---|---|---|---|---|---|
| Cerebral angiogram | ||||||
| Overall | 2,917 | 2,015 | –30.9% | 27.5(15‐41) | 17.5(12‐30) | .2106 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 1,620 | 935 | –42.3% | 9(7‐42) | 9(5‐30) | 1 |
| High | 1,297 | 1,080 | –16.7% | 32.5(19‐46) | 22(17‐49) | .291 |
| Institutional location | ||||||
| USA | 1,354 | 1,163 | –14.1% | 29.5(19‐41) | 20(14‐35) | .2417 |
| Non‐USA | 1,563 | 852 | –45.5% | 7.5(3‐55) | 6(2‐30) | .946 |
| Mechanical thrombectomy for acute ischemic stroke | ||||||
| Overall | 690 | 635 | –8.0% | 7(6‐10) | 7(6‐8) | 1 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 262 | 263 | .4% | 5(3‐10) | 6(5‐8) | .6018 |
| High | 428 | 372 | –13.1% | 9(7‐12) | 8(6‐11) | .5062 |
| Institutional location | ||||||
| USA | 341 | 332 | –2.6% | 7(6‐9) | 7(6‐8) | 1 |
| Non‐USA | 349 | 303 | –13.2% | 7.5(3‐14) | 7.5(4‐12) | .8121 |
| Carotid stent placement for symptomatic internal carotid artery stenosis | ||||||
| Overall | 233 | 180 | –22.7% | 3(2‐3) | 2(1‐3) | .0814 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 136 | 100 | –26.5% | 3(1‐5) | 2(1‐3) | .3789 |
| High | 97 | 80 | –17.5% | 2.5(2‐3) | 1.5(1‐3) | 1 |
| Institutional location | ||||||
| USA | 121 | 120 | –.8% | 3(2‐3) | 2(1‐4) | .1715 |
| Non‐USA | 112 | 60 | –46.4% | 3(1‐5) | .5(0‐2) | .0334 |
| Carotid stent placement for asymptomatic internal carotid artery stenosis | ||||||
| Overall | 106 | 60 | –43.4% | 0(0‐0) | 0(0‐0) | – |
| Location according to COVID‐19 prevalence | ||||||
| Low | 95 | 54 | –43.2% | 1(0‐2) | 0(0‐1) | .0135 |
| High | 11 | 6 | –45.5% | 0(0‐0) | 0(0‐0) | – |
| Institutional location | ||||||
| USA | 13 | 11 | –15.4% | 0(0‐0) | 0(0‐0) | – |
| Non‐USA | 93 | 49 | –47.3% | 1.5(0‐3) | 0(0‐1) | .0901 |
| Endovascular treatment of ruptured intracranial aneurysms | ||||||
| Overall | 216 | 239 | 10.6% | 2(1‐3) | 2(1‐3) | 1 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 88 | 112 | 27.3% | 1(0‐2) | 2(1‐3) | .1857 |
| High | 128 | 127 | –.8% | 3(2‐4) | 2(1‐4) | .3196 |
| Institutional location | ||||||
| USA | 93 | 98 | 5.4% | 2(1‐2) | 2(1‐2) | 1 |
| Non‐USA | 123 | 141 | 14.6% | 3.5(1‐4) | 4(1‐7) | 1 |
| Endovascular treatment of unruptured intracranial aneurysms | ||||||
| Overall | 444 | 246 | –44.6% | 3(2‐4) | 1(1‐3) | .0125 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 253 | 100 | –60.5% | 2(0‐3) | 1(0‐2) | .2606 |
| High | 191 | 146 | –23.6% | 4(3‐7) | 3(1‐5) | .5062 |
| Institutional location | ||||||
| USA | 136 | 98 | –27.9% | 3(1‐4) | 1.5(0‐3) | .1715 |
| Non‐USA | 308 | 148 | –51.9% | 3.5(2‐11) | 1(0‐7) | .493 |
| Endovascular treatment of ruptured brain arteriovenous malformations | ||||||
| Overall | 48 | 37 | –22.9% | 0(0‐1) | 0(0‐0) | 1 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 26 | 16 | –38.5% | 0(0‐1) | 0(0‐0) | – |
| High | 22 | 21 | –4.5% | 0(0‐1) | 0(0‐1) | 1 |
| Institutional location | ||||||
| USA | 23 | 20 | –13.0% | 0(0‐1) | 0(0‐1) | 1 |
| Non‐USA | 25 | 17 | –32.0% | 0(0‐1) | 0(0‐0) | 1 |
| Endovascular treatment of unruptured brain arteriovenous malformations | ||||||
| Overall | 119 | 40 | –66.4% | 0(0‐1) | 0(0‐0) | – |
| Location according to COVID‐19 prevalence | ||||||
| Low | 94 | 22 | –76.6% | .5(0‐2) | 0(0‐0) | – |
| High | 25 | 18 | –28.0% | 0(0‐1) | 0(0‐1) | 1 |
| Institutional location | ||||||
| USA | 27 | 13 | –51.9% | 0(0‐1) | 0(0‐0) | – |
| Non‐USA | 92 | 27 | –70.7% | 0(0‐3) | 0(0‐1) | 1 |
| Intracranial angioplasty/stent for intracranial stenosis | ||||||
| Overall | 182 | 99 | –45.6% | 0(0‐1) | 0(0‐0) | 1 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 144 | 63 | –56.3% | 0(0‐1) | 0(0‐1) | 1 |
| High | 38 | 36 | –5.3% | 0(0‐1) | 0(0‐1) | 1 |
| Institutional location | ||||||
| USA | 42 | 42 | .0% | 0(0‐0) | 0(0‐1) | 1 |
| Non‐USA | 140 | 57 | –59.3% | 0(0‐1) | 0(0‐1) | 1 |
| Other neuroendovascular procedures (spinal angiograms, WADA, others) | ||||||
| Overall | 243 | 328 | 35.0% | 1(0‐2) | 1.5(0‐3) | 1 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 86 | 88 | 2.3% | 1(0‐2) | 0(0‐4) | .209 |
| High | 157 | 240 | 52.9% | 0(0‐3) | 2(1‐4) | .0489 |
| Institutional location | ||||||
| USA | 113 | 143 | 26.5% | 2(0‐2) | 3(2‐4) | .2452 |
| Non‐USA | 130 | 185 | 42.3% | 0(0‐2) | 0(0‐0) | 1 |
| Other nonendovascular procedures | ||||||
| Overall | 341 | 320 | –6.2% | 0(0‐0) | 0(0‐0) | – |
| Location according to COVID‐19 prevalence | ||||||
| Low | 302 | 277 | –8.3% | 0(0‐6) | 0(0‐3) | 1 |
| High | 39 | 43 | 10.3% | 0(0‐0) | 0(0‐0) | – |
| Institutional location | ||||||
| USA | 293 | 294 | .3% | 0(0‐1) | 0(0‐0) | 1 |
| Non‐USA | 48 | 26 | –45.8% | 0(0‐0) | 0(0‐0) | – |
Comparison of Pre‐COVID‐19 and During COVID‐19 Periods (January‐February)
There was a minor reduction in the number of cerebral angiograms more prominent in low COVID‐19 prevalent regions and non‐USA institution (Table 2). There was no change in mechanical thrombectomy and carotid stent placement for symptomatic ICA stenosis. Carotid stent placement for symptomatic ICA stenosis increased in USA but decreased in non‐USA centers. There was a reduction in carotid stent placement for asymptomatic ICA stenosis and intracranial angioplasty and/or stent placement and no change in endovascular treatment of unruptured intracranial aneurysms and ruptured and unruptured BAVMs. There was a slight increase in endovascular treatment of ruptured intracranial aneurysms, other neuroendovascular procedures, and nonendovascular procedures.
Table 2.
Neuroendovascular Procedures for January and February 2019 and 2020
| Study or subgroup | Total number in 2019 | Total number in 2020 | Change % |
Median number in 2019 (95% confidence interval) |
Median number in 2020 (95% confidence interval) |
Quantile regression P‐value |
|---|---|---|---|---|---|---|
| Cerebral angiogram | ||||||
| Overall | 1,332 | 1,226 | –8.6% | 24(13‐41) | 21(15‐45) | .9128 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 690 | 539 | –21.9% | 9(3‐45) | 14(2‐44) | .8139 |
| High | 642 | 687 | 7.0% | 29.5(14‐46) | 37(17‐53) | .7888 |
| Institutional location | ||||||
| USA | 625 | 723 | 15.7% | 29.5(14‐42) | 30(17‐49) | .8227 |
| Non‐USA | 707 | 503 | –28.9% | 7.5(2‐103) | 7(2‐82) | .9729 |
| Mechanical thrombectomy for acute ischemic stroke | ||||||
| Overall | 310 | 313 | 1.0% | 7(5‐10) | 6.5(6‐10) | .5686 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 103 | 127 | 23.3% | 4(2‐10) | 7(4‐12) | .4321 |
| High | 207 | 186 | –10.1% | 8(7‐13) | 6.5(5‐12) | .7105 |
| Institutional location | ||||||
| USA | 163 | 162 | –.6% | 7(5‐11) | 6(5‐10) | .571 |
| Non‐USA | 147 | 151 | 2.7% | 6.5(1‐20) | 11(4‐13) | .5273 |
| Carotid stent placement for symptomatic internal carotid artery stenosis | ||||||
| Overall | 110 | 106 | –3.6% | 2(1‐4) | 2.5(1.4) | 1 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 66 | 58 | –12.1% | 3(0‐5) | 2.5(0‐5) | 1 |
| High | 44 | 48 | 9.1% | 2(1‐3) | 2.5(0‐5) | 1 |
| Institutional location | ||||||
| USA | 51 | 71 | 39.2% | 2(1‐4) | 3(1‐5) | .3573 |
| Non‐USA | 59 | 35 | –40.7% | 3.5(1‐5) | 0(0‐6) | .0965 |
| Carotid stent placement for asymptomatic internal carotid artery stenosis | ||||||
| Overall | 49 | 32 | –34.7% | 0(0‐1) | 0(0‐0) | 1 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 44 | 29 | –34.1% | 1(0‐2) | 1.5(0‐1) | 1 |
| High | 5 | 3 | –40.0% | 0(0‐0) | 0(0‐0) | – |
| Institutional location | ||||||
| USA | 5 | 7 | 40.0% | 0(0‐0) | 0(0‐1) | 1 |
| Non‐USA | 44 | 25 | –43.2% | 1.5(0‐4) | 0(0‐2) | .3246 |
| Endovascular treatment of ruptured intracranial aneurysms | ||||||
| Overall | 102 | 124 | 21.6% | 2(1‐3) | 2(1‐4) | 1 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 39 | 55 | 41.0% | 1(0‐3) | 2(1‐4) | .3158 |
| High | 63 | 69 | 9.5% | 3(1‐4) | 2.5(1‐7) | .485 |
| Institutional location | ||||||
| USA | 41 | 49 | 19.5% | 1.5(1‐3) | 2(1‐3) | 1 |
| Non‐USA | 61 | 75 | 23.0% | 4(0‐9) | 4.5(1‐11) | .7413 |
| Endovascular treatment of unruptured intracranial aneurysms | ||||||
| Overall | 167 | 154 | –7.8% | 3(2‐4) | 2(1‐4) | .2606 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 74 | 64 | –13.5% | 1.5(0‐3) | 1(0‐3) | 1 |
| High | 93 | 90 | –3.2% | 4(2‐8) | 3.5(2‐7) | 1 |
| Institutional location | ||||||
| USA | 59 | 59 | .0% | 2(1‐4) | 2(1‐4) | 1 |
| Non‐USA | 108 | 95 | –12.0% | 3.5(1‐13) | 2(0‐13) | 1 |
| Endovascular treatment of ruptured brain arteriovenous malformations | ||||||
| Overall | 25 | 27 | 8.0% | 0(0‐1) | 0(0‐1) | 1 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 14 | 14 | .0% | .5(0‐1) | 0(0‐1) | 1 |
| High | 11 | 13 | 18.2% | 0(0‐1) | 1(0‐1) | .002 |
| Institutional location | ||||||
| USA | 10 | 12 | 20.0% | 0(0‐1) | 0(0‐1) | 1 |
| Non‐USA | 15 | 15 | .0% | 0(0‐2) | 0(0‐2) | 1 |
| Endovascular treatment of unruptured brain arteriovenous malformations | ||||||
| Overall | 43 | 31 | –27.9% | 0(0‐1) | 0(0‐1) | 1 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 33 | 17 | –48.5% | .5(0‐2) | 0(0‐1) | 1 |
| High | 10 | 14 | 40.0% | 0(0‐1) | .5(0‐1) | 1 |
| Institutional location | ||||||
| USA | 11 | 11 | .0% | 0(0‐1) | 0(0‐1) | 1 |
| Non‐USA | 32 | 20 | –37.5% | 0(0‐4) | 0(0‐3) | 1 |
| Intracranial angioplasty/stent for intracranial stenosis | ||||||
| Overall | 67 | 51 | –23.9% | 0(0‐1) | 0(0‐1) | 1 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 52 | 29 | –44.2% | 0(0‐1) | 0(0‐1) | 1 |
| High | 15 | 22 | 46.7% | 0(0‐2) | 0(0‐1) | 1 |
| Institutional location | ||||||
| USA | 14 | 23 | 64.3% | 0(0‐1) | 0(0‐1) | 1 |
| Non‐USA | 53 | 28 | –47.2% | 1(0‐2) | 0(0‐2) | .1245 |
| Other neuroendovascular procedures (spinal angiograms, WADA, others) | ||||||
| Overall | 99 | 162 | 63.6% | .5(0‐2) | 1(0‐4) | 1 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 29 | 46 | 58.6% | 1.5(0‐2) | 0(0‐5) | .4891 |
| High | 70 | 116 | 65.7% | 0(0‐4) | 1.5(0‐7) | .635 |
| Institutional location | ||||||
| USA | 43 | 79 | 83.7% | 2(0‐2) | 2.5(1‐7) | 1 |
| Non‐USA | 56 | 83 | 48.2% | 0(0‐8) | 0(0‐9) | 1 |
| Other nonendovascular procedures | ||||||
| Overall | 153 | 204 | 33.3% | 0(0‐1) | 0(0‐0) | 1 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 133 | 170 | 27.8% | 0(0‐7) | 0(0‐11) | 1 |
| High | 20 | 34 | 70.0% | 0(0‐1) | 0(0‐1) | 1 |
| Institutional location | ||||||
| USA | 138 | 190 | 37.7% | 0(0‐8) | 0(0‐13) | 1 |
| Cerebral angiogram | 15 | 14 | –6.7% | 0(0‐1) | 0(0‐0) | – |
Comparison of Pre‐COVID‐19 and During COVID‐19 Periods (March‐April)
There were reductions of cerebral angiograms, mechanical thrombectomy, and carotid stent placement for symptomatic and asymptomatic ICA stenosis (Table 3). There were reductions in endovascular treatment of unruptured intracranial aneurysms, ruptured and unruptured BAVMs, and intracranial angioplasty and/or stent placement. There was no change in the treatment of ruptured intracranial aneurysms and slight increase in low COVID‐19 prevalent regions.
Table 3.
Neuroendovascular Procedures for 2019 and 2020 (March‐April)
| Study or subgroup | Total number in 2019 | Total number in 2020 | Change % |
Median number in 2019 (95% confidence interval) |
Median number in 2020 (95% confidence interval) |
Quantile regression P‐value |
|---|---|---|---|---|---|---|
| Cerebral angiogram | ||||||
| Overall | 1,585 | 789 | –50.2% | 27.5(15‐49) | 12(6‐30) | .1184 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 930 | 396 | –57.4% | 11.5(2‐50) | 6.5(1‐39) | .9431 |
| High | 655 | 393 | –40.0% | 38(18‐51) | 20(7‐34) | .1387 |
| Institutional location | ||||||
| USA | 729 | 440 | –39.6% | 31.5(18‐49) | 13.5(7‐35) | .133 |
| Non‐USA | 856 | 349 | –59.2% | 7.5(2‐69) | 4(1‐43) | .9129 |
| Mechanical thrombectomy for acute ischemic stroke | ||||||
| Overall | 380 | 322 | –15.3% | 8(6‐12) | 7(5‐10) | 1 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 159 | 136 | –14.5% | 5.5(2‐14) | 5.5(4‐8) | .7408 |
| High | 221 | 186 | –15.8% | 9.5(6‐14) | 8.5(7‐13) | 1 |
| Institutional location | ||||||
| USA | 178 | 170 | –4.5% | 7(5‐12) | 7(5‐11) | 1 |
| Non‐USA | 202 | 152 | –24.8% | 11.5(2‐30) | 6.5(3‐24) | .6183 |
| Carotid stent placement for symptomatic internal carotid artery stenosis | ||||||
| Overall | 123 | 74 | –39.8% | 3(2‐4) | 1.5(1‐2) | .2606 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 70 | 42 | –40.0% | 3(0‐4) | 2(1‐3) | .485 |
| High | 53 | 32 | –39.6% | 3(2‐4) | 1(0‐3) | .0496 |
| Institutional location | ||||||
| USA | 70 | 49 | –30.0% | 3(2‐5) | 2(1‐4) | .4156 |
| Non‐USA | 53 | 25 | –52.8% | 2.5(1‐6) | 1(0‐3) | .5092 |
| Carotid stent placement for asymptomatic internal carotid artery stenosis | ||||||
| Overall | 57 | 28 | –50.9% | 0(0‐1) | 0(0‐0) | – |
| Location according to COVID‐19 prevalence | ||||||
| Low | 51 | 25 | –51.0% | 1(0‐2) | 0(0‐1) | .1167 |
| High | 6 | 3 | –50.0% | 0(0‐0) | 0(0‐0) | – |
| Institutional location | ||||||
| USA | 8 | 4 | –50.0% | 0(0‐0) | 0(0‐0) | – |
| Non‐USA | 49 | 24 | –51.0% | 1.5(0‐4) | 0(0‐1) | .2862 |
| Endovascular treatment of ruptured intracranial aneurysms | ||||||
| Overall | 114 | 115 | .9% | 2(1‐4) | 2(1‐4) | 1 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 49 | 57 | 16.3% | 1(0‐4) | 2(1‐4) | .4321 |
| High | 65 | 58 | –10.8% | 2.5(2‐5) | 2(1‐5) | 1 |
| Institutional location | ||||||
| USA | 52 | 49 | –5.8% | 2(1‐4) | 2(1‐3) | 1 |
| Non‐USA | 62 | 66 | 6.5% | 3(1‐9) | 3.5(0‐10) | .7413 |
| Endovascular treatment of unruptured intracranial aneurysms | ||||||
| Overall | 277 | 92 | –66.8% | 3(2‐5) | .5(0‐3) | .0809 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 179 | 36 | –79.9% | 2.5(0‐4) | 1(0‐3) | .3887 |
| High | 98 | 56 | –42.9% | 4.5(1‐8) | 0(0‐6) | .0999 |
| Institutional location | ||||||
| USA | 77 | 39 | –49.4% | 3(1‐5) | 0(0‐3) | .0078 |
| Non‐USA | 200 | 53 | –73.5% | 4(0‐16) | 1(0‐9) | .6288 |
| Endovascular treatment of ruptured BAVMs | ||||||
| Overall | 23 | 10 | –56.5% | 0(0‐1) | 0(0‐0) | – |
| Location according to COVID‐19 prevalence | ||||||
| Low | 12 | 2 | –83.3% | 0(0‐1) | 0(0‐0) | – |
| High | 11 | 8 | –27.3% | .5(0‐1) | 0(0‐1) | 1 |
| Institutional location | ||||||
| USA | 13 | 8 | –38.5% | .5(0‐1) | 0(0‐1) | 1 |
| Non‐USA | 10 | 2 | –80.0% | 0(0‐2) | 0(0‐0) | – |
| Endovascular treatment of unruptured BAVMs | ||||||
| Overall | 76 | 9 | –88.2% | 0(0‐2) | 0(0‐0) | – |
| Location according to COVID‐19 prevalence | ||||||
| Low | 61 | 5 | –91.8% | .5(0‐2) | 0(0‐0) | – |
| High | 15 | 4 | –73.3% | 0(0‐2) | 0(0‐0) | – |
| Institutional location | ||||||
| USA | 16 | 2 | –87.5% | 0(0‐1) | 0(0‐0) | – |
| Non‐USA | 60 | 7 | –88.3% | .5(0‐4) | 0(0‐1) | 1 |
| Intracranial angioplasty/stent for intracranial stenosis | ||||||
| Overall | 115 | 48 | –58.3% | 0(0‐1) | 0(0‐1) | 1 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 92 | 34 | –63.0% | 0(0‐1) | 0(0‐1) | 1 |
| High | 23 | 14 | –39.1% | 0(0‐2) | 0(0‐1) | 1 |
| Institutional location | ||||||
| USA | 28 | 19 | –32.1% | 0(0‐2) | 0(0‐1) | 1 |
| Non‐USA | 87 | 29 | –66.7% | 0(0‐2) | 0(0‐1) | 1 |
| Other neuroendovascular procedures (spinal angiograms, WADA, others) | ||||||
| Overall | 144 | 166 | 15.3% | 1(0‐3) | 2(0‐4) | .3789 |
| Location according to COVID‐19 prevalence | ||||||
| Low | 57 | 42 | –26.3% | 1(0‐5) | 0(0‐4) | .4764 |
| High | 87 | 124 | 42.5% | 0(0‐6) | 2.5(1‐5) | .288 |
| Institutional location | ||||||
| USA | 70 | 64 | –8.6% | 1.5(0‐5) | 3(1‐4) | .4694 |
| Non‐USA | 74 | 102 | 37.8% | .5(0‐7) | 0(0‐9) | 1 |
| Other nonendovascular procedures | ||||||
| Overall | 188 | 116 | –38.3% | 0(0‐1) | 0(0‐0) | – |
| Location according to COVID‐19 prevalence | ||||||
| Low | 169 | 107 | –36.7% | 0(0‐14) | 0(0‐6) | 1 |
| High | 19 | 9 | –52.6% | 0(0‐1) | 0(0‐0) | – |
| Institutional location | ||||||
| USA | 155 | 104 | –32.9% | 0(0‐6) | 0(0‐1) | 1 |
| Non‐USA | 33 | 12 | –63.6% | 0(0‐4) | 0(0‐0) | ‐ |
Comparison of January and February (Early Phase) and March and April (Established Phase) in 2020
There were reductions in cerebral angiograms (55.4%) carotid artery stent placement for symptomatic (30.2%) and asymptomatic (12.5%) stenoses, intracranial angioplasty and/or stent placement (45%), and endovascular treatment of unruptured intracranial aneurysms (40.3%) and ruptured (63.9%) and unruptured (71.0%) BAVMs, and endovascular treatment of ruptured intracranial aneurysms (7.3%). There was a minor increase in mechanical thrombectomy (2.9%).
Discussion
Comparisons of procedures between January to April 2019 and 2020 demonstrated a reduction in almost all neuroendovascular procedures, except the treatment of ruptured intracranial aneurysms in 2020 compared with 2019. In January and February, there was some heterogeneity in changes in various neuroendovascular procedures. In March and April, there was a reduction in almost all neuroendovascular procedures except the treatment of ruptured intracranial aneurysms in 2020 compared with 2019. There was no clear relationship between location of hospital (high or low COVID‐19 prevalent regions) and changes in procedures.
One surprising finding was the reduction in mechanical thrombectomy for acute ischemic stroke and carotid stent placement for symptomatic ICA stenosis, given that COVID‐19 leads to an increased risk of ischemic stroke. 1 Another analysis from 32 centers in French administrative regions reported a 21% reduction in mechanical thrombectomy volumes during the epidemic period. 2 This may be due to less patients seeking medical attention, and challenges in preforming mechanical thrombectomy and carotid stent placement with implementation of screening protocols to reduce the risk of transmission to medical professionals. 1 A reduction in mechanical thrombectomy may increase the rate of death and disability among acute ischemic stroke patients. 9 , 10 A reduction and/or delay in performance of carotid stent placement for symptomatic ICA stenosis may increase the risk of recurrent ischemic stroke among eligible patients. 11 , 12 There was no change in endovascular treatment of ruptured intracranial aneurysms and possibly aneurysmal subarachnoid hemorrhage (aSAH). In contrast, a previous study in France had noted that the number of admissions for aSAH had decreased with institution of social distancing measures. 13 There may be preferential use of endovascular treatment 14 if a larger segment of patients with aSAH are presenting in a delayed manner similar to that observed in acute ischemic stroke patients. 1
The large reduction in elective procedures, such as carotid stent placement for asymptomatic ICA stenosis and endovascular treatment of unruptured intracranial aneurysms and BAVMs, was expected. 1 Several local and regional authorities had issued mandates to defer all elective procedures. 3 A survey reported that more than 27% of patients in the United States had an elective surgery, appointment, or procedure delayed or cancelled due to the COVID‐19 pandemic. 4 Many patients may also avoid elective procedures due to loss of employment and medical insurance. 15 We also noted an unexpected decrease in total number of practitioners from 759 to 589 in pre‐COVID‐19 and during COVID‐19 periods, respectively. The exact reasons for this decrease are not known. Possible reasons could be exclusion of practitioners who may be at high risk for acquiring COVID‐19 and/or reallocation to other hospitals or services to meet increasing demands due to COVID‐19. We acknowledge that a reduction in number of practitioners may have influenced the number of neuroendovascular procedures performed. However, there was also a reduction in the number of procedures per practitioner during the COVID‐19 pandemic.
There are certain limitations that must be considered prior to the interpretation of our study. The data were derived from large stroke institution from various geographical settings with their own COVID‐19 related restrictions and timelines of implementation, which may have introduced heterogeneity within observed results. While such data provide a broader perspective of neuroendovascular practice changes, in‐depth analysis of eligible patients and procedures performed was not possible and therefore, we are unable to comment upon any changes in patient demographics or clinical characteristics among those undergoing procedures during the COVID‐19 pandemic. We used a sampling period of 2 months post epidemic and previous year data from same months as reference as has been used in previous studies. 16 , 17 , 18 , 19 Some studies have used even a shorter period of 2 weeks to study changes in acute stroke admissions and mechanical thrombectomy procedures to study the effect of COVID‐19 pandemic. 2 , 20 However, the pandemic has been prolonged beyond initial projections with dynamic changes in regional prevalence of COVID‐19. Such dynamic changes pose challenges in defining in regions where hospitals were located as high prevalence and low prevalence. Many of the regions would have been reclassified particularly in the resurgence of COVID‐19 in months that followed. These changes were not anticipated when the study was first designed.
We provided an international multicenter view of changes in neuroendovascular practices to better understand the gaps in provision of care to address the previously unmet needs of the ongoing COVID‐19 pandemic. Any gaps in the provision of care during COVID‐19 pandemic must be identified in future analyses to avoid increasing the rate of unfavorable outcomes among patients with ischemic stroke and transient ischemic attack.
Acknowledgments and Disclosures: None.
Contributor Information
Adnan I. Qureshi, Email: qureshiai@health.missouri.edu.
Ossama Yassin Mansour, Email: yassinossama@yahoo.com.
References
- 1. Qureshi AI, Abd‐Allah F, Al‐Senani F, et al. Management of acute ischemic stroke in patients with COVID‐19 infection: report of an international panel. Int J Stroke 2020;15:540‐4. [DOI] [PubMed] [Google Scholar]
- 2. Kerleroux B, Fabacher T, Bricout N, et al. Mechanical thrombectomy for acute ischemic stroke amid the COVID‐19 outbreak: decreased activity, and increased care delays. Stroke 2020;51:2012‐7. [DOI] [PubMed] [Google Scholar]
- 3. COVID‐19: guidance for triage of non‐emergent surgical procedures. Available from: https://www.facs.org/COVID-19/clinical-guidance/triage. Accessed July 16, 2020.
- 4. Pecci AW. 3 revenue cycle hurdles for resuming elective procedures. Available from: https://www.healthleadersmedia.com/finance/3-revenue-cycle-hurdles-resuming-elective-procedures. Accessed July 16, 2020.
- 5. Qureshi AI, Abd‐Allah F, Al‐Senani F, et al. Management of acute ischemic stroke in patients with COVID‐19 infection: insights from an international panel. Am J Emerg Med 2020;38:1548.e5‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Day AL, Siddiqui AH, Meyers PM, et al. Training standards in neuroendovascular surgery: program accreditation and practitioner certification. Stroke 2017;48:2318‐25. [DOI] [PubMed] [Google Scholar]
- 7. Grigoryan M, Chaudhry SA, Hassan AE, et al. Neurointerventional procedural volume per hospital in United States: implications for comprehensive stroke center designation. Stroke 2012;43:1309‐14. [DOI] [PubMed] [Google Scholar]
- 8. Qureshi AI, Abou‐Chebl A, Jovin TG. Qualification requirements for performing neurointerventional procedures: a report of the practice guidelines committee of the American Society of Neuroimaging and the Society of Vascular and Interventional Neurology. J Neuroimaging 2008;18:433‐47. [DOI] [PubMed] [Google Scholar]
- 9. Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large‐vessel ischaemic stroke: a meta‐analysis of individual patient data from five randomised trials. Lancet 2016;387:1723‐31. [DOI] [PubMed] [Google Scholar]
- 10. Qureshi AI, Ishfaq MF, Rahman HA, et al. Endovascular treatment versus best medical treatment in patients with acute ischemic stroke: a meta‐analysis of randomized controlled trials. AJNR Am J Neuroradiol 2016;37:1068‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. De Rango P, Brown MM, Chaturvedi S, et al. Summary of evidence on early carotid intervention for recently symptomatic stenosis based on meta‐analysis of current risks. Stroke 2015;46:3423‐36. [DOI] [PubMed] [Google Scholar]
- 12. Savardekar AR, Narayan V, Patra DP, et al. Timing of carotid endarterectomy for symptomatic carotid stenosis: a snapshot of current trends and systematic review of literature on changing paradigm towards early surgery. Neurosurgery 2019;85:E214‐25. [DOI] [PubMed] [Google Scholar]
- 13. Bernat AL, Giammattei L, Abbritti R, et al. Impact of COVID‐19 pandemic on subarachnoid hemorrhage. J Neurosurg Sci 2020;64:409‐10. [DOI] [PubMed] [Google Scholar]
- 14. Goertz L, Pflaeging M, Hamisch C, et al. Delayed hospital admission of patients with aneurysmal subarachnoid hemorrhage: clinical presentation, treatment strategies, and outcome. J Neurosurg 2020. 10.3171/2020.2.JNS20148 [DOI] [PubMed] [Google Scholar]
- 15. Hospital visits down sharply and patients may not be in a rush to reschedule appointments. Available from: https://newsroom.transunion.com/hospital-visits-down-sharply-and-patients-may-not-be-in-a-rush-to-reschedule-appointments. Accessed July 23, 2020.
- 16. Kim J, Kim J, Lee SK, et al. Effects of epidemic disease outbreaks on financial performance of restaurants: event study method approach. J Hosp Tour Manage 2020;43:32‐41. [Google Scholar]
- 17. Pop R, Hasiu A, Bolognini F, et al. Stroke thrombectomy in patients with COVID‐19: initial experience in 13 cases. AJNR Am J Neuroradiol 2020. 10.3174/ajnr.A6750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Qureshi AI, Huang W, Khan S, et al. Mandated societal lockdown and road traffic accidents. Accid Anal Prev 2020;146:105747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Qureshi AI, Siddiq F, French BR, et al. Effect of COVID‐19 pandemic on mechanical thrombectomy for acute ischemic stroke treatment in United States. J Stroke Cerebrovasc Dis 2020;29:105140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kansagra AP, Goyal MS, Hamilton S, et al. Collateral effect of COVID‐19 on stroke evaluation in the United States. N Engl J Med 2020;383:400‐1. [DOI] [PMC free article] [PubMed] [Google Scholar]


