Abstract
The lockdown measures of the ongoing COVID‐19 pandemic have disengaged patients with cancer from formal health care settings, leading to an increased use of social media platforms to address unmet needs and expectations. Although remote health technologies have addressed some of the medical needs, the emotional and mental well‐being of these patients remain underexplored and underreported. We used a validated artificial intelligence framework to conduct a comprehensive real‐time analysis of two data sets of 2,469,822 tweets and 21,800 discussions by patients with cancer during this pandemic. Lung and breast cancer are most prominently discussed, and the most concerns were expressed regarding delayed diagnosis, cancellations, missed treatments, and weakened immunity. All patients expressed significant negative sentiment, with fear being the predominant emotion. Even as some lockdown measures ease, it is crucial that patients with cancer are engaged using social media platforms for real‐time identification of issues and the provision of informational and emotional support.
Short abstract
Oncology patients have been severely affected by the ongoing COVID‐19 pandemic that has caused disruption in the traditional health care setting. Although remote health technologies have addressed some of the medical needs, the emotional and mental well‐being of these patients remain underreported. This article reports the primary challenges experienced by cancer patients due to COVID‐19 lockdown measures.
The COVID‐19 pandemic has disrupted all aspects of human society with more than 10 million confirmed cases and more than half a million deaths in 180 days after the first case was reported. Following stringent social distancing and lockdown measures, hospital systems have increasingly transitioned to telemedicine for nonpandemic health care services. Oncology patients in particular have been severely affected by this transition as they are disconnected from a formal and familiar health care setting that is intertwined with their cancer trajectory. Despite many research endeavors on cancer and COVID‐19, such as the severity on immunocompromised patients with cancer [1], cancer care management [2], nonpharmaceutical interventions [3], and hospital hygiene [4], none has focused on this disconnect and the corresponding impact on mental health and emotional well‐being. In fact, patients with cancer have addressed this void by seeking informational and emotional support on diverse social media platforms. Twitter has been the most widely used platform, with more than two million tweets during this pandemic. Although the short‐form expressions on Twitter are well suited for the fast‐evolving nature of the pandemic and associated challenges, more substantial conversations and discussions are taking place on online cancer support groups (OCSGs). Given that mental health and emotional well‐being of patients with cancer are underreported and underexplored, we postulate that patient‐reported information on these social media platforms can be used for real‐time analysis of patient needs and expectations for the delivery of effective oncology care during this period.
Patient‐reported information during COVID‐19 (from February 1 to April 30) was extracted and compiled in the form of two data sets: 2,469,822 tweets from Twitter and 21,800 posts from a combination of general and specific OCSGs. All data sources are publicly available, and the entire data extraction process was anonymized. We applied a validated artificial intelligence framework, the Patient‐Reported Information Multidimensional Exploration (PRIME) framework [5, 6] on both data sets. The PRIME framework has been effectively used for the extraction, analysis and synthesis of patient‐reported information on physical and mental well‐being, such as symptoms, side effects, treatment decisions, real‐life experiences, mental health issues, and emotional burden of patients with cancer, cancer survivors, and caregivers [7].
After the initial application of PRIME on the Twitter data set, we observed a sharp threefold increase in the volume of tweets on March 11, 2020, when the World Health Organization declared COVID‐19 a global pandemic. Most of these tweets focused on the propagation of guidelines issued by health care providers, such as the criticality of social distancing for patients with cancer and the anticipated delays in access to formal care. The next level of analysis was the type of patient with cancer contributing this increase in volume. We observed that the highest was 38.3% related to lung cancer and second highest was 23.8% related to breast cancer.
In applying the PRIME framework on the OCSG data set, we analyzed the emotional burden of the pandemic on patients with cancer, based on more substantial discussions, which were semantically rich and context‐aware in comparison with tweets. We used an ensemble of machine learning algorithms to extract two sentiments (negative and positive) and eight emotions (anger, fear, anticipation, trust, surprise, sadness, joy, and disgust) [8]. As visualized in Figure 1, the overall positive sentiment gradually decreased from February 1 to April 30. The most prominent emotions were “fear” and “joy,” with “fear” being consistently expressed during this period, whereas “joy” underwent a significant drop soon after the pandemic was declared, followed by a gradual decrease with occasional spikes of positivity that were triggered by media releases on the development of treatments for COVID‐19.
Figure 1.
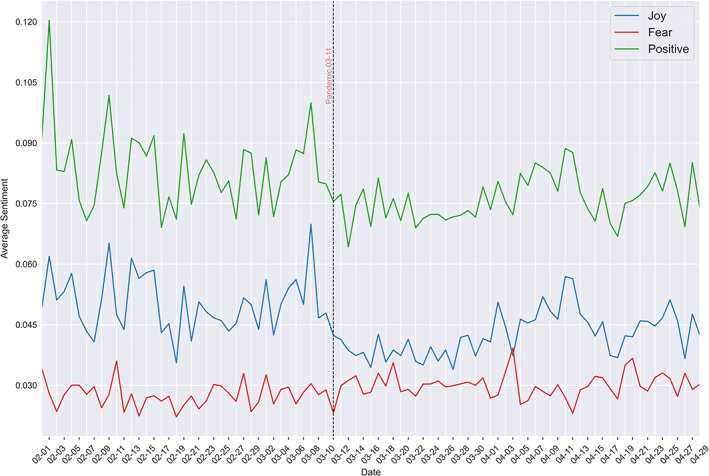
Emotions expressed by patients with cancer before and after the COVID‐19 outbreak was formally declared a global pandemic.
In terms of patient needs, we used the natural language processing techniques followed by artificial intelligence algorithms in PRIME to explore the key patient issues expressed in both data sets, based on high‐level themes and corresponding topics. Tweets mainly focused on treatment delays, diagnosis delays, and weakened immunity, whereas cancellation of consultations, missed scans, and risks of undergoing chemotherapy were the main focus in OCSG discussions. These concerns align with a recent study that reports individuals on active chemotherapy or radical radiotherapy for lung cancer, and patients with blood or bone marrow cancers are the highest risk group [9]. Delays in diagnosis of hematologic cancers such as acute leukemia, which require immediate treatment, put patients' lives at more risk and lower life expectancy [10]. Going beyond these medical concerns, both data sets contained a significant volume of concerns expressed on mental health, adjusting to the “new normal,” and daily physical activity. We formulated these findings of patient needs in terms of key themes and corresponding topics as illustrated in the sunburst diagram (Fig. 2). The inner circle represents the themes, the intermediate circle denotes the emotions for each theme, and the outer circle represents the topics of concern for each theme. The themes are ordered 1 to 6, in descending order of most significant to least. The most prominent emotion across all themes is “fear,” except “ongoing care,” which is positive with “anticipation” at 30% intensity.
Figure 2.
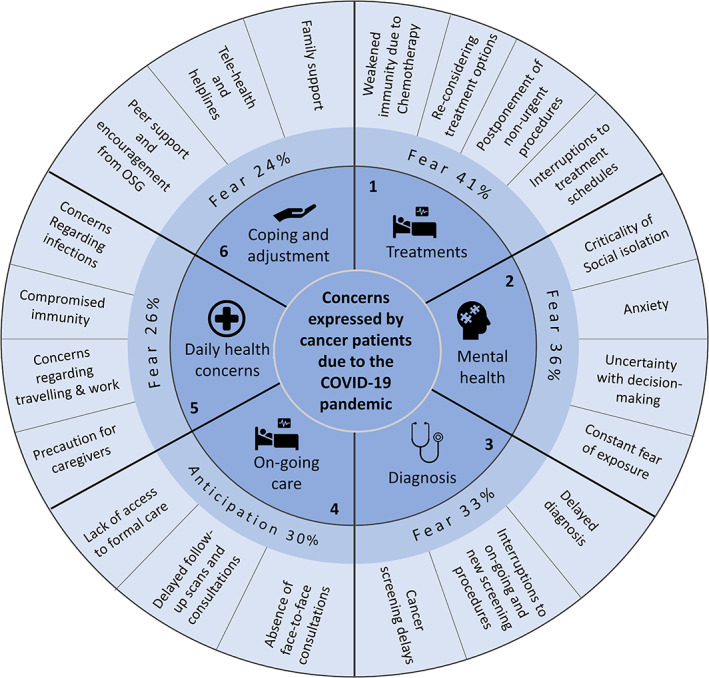
Sunburst diagram of patient needs and corresponding emotions. The inner circle represents themes numbered by significance in descending order. The outer circle represents the main topics of concern for each theme. The intermediate circle represents the most significant emotion and intensity of expression for each theme and its main topics.
We have successfully applied the PRIME framework to develop a deep understanding of the “pulse” of patients with cancer in terms of their information needs, health care expectations, mental health, and emotional well‐being during this pandemic. These findings are particularly significant as they formalize the health care value of online patient‐reported information during a time when formal care is compromised and clinical resources are exhausted. The robust correlation between the sustained threefold increase in social media participation and the steady decrease in positive emotions is a grave concern for the effective management of cancer care during the pandemic. We have demonstrated how PRIME can be used to precisely detect emotions in real time, including sensitive emotional fluctuations due to media announcements on coronavirus treatment development. This means that telemedicine and remote health care technologies can be used to provide proactive and responses to patients with cancer in distress and actively prioritize patients who require urgent support. The COVID‐19 pandemic is far from over, and it is prudent and practical for formal health care systems to incorporate the findings of this study for the real‐time identification and delivery of effective care for oncology patients.
Disclosures
The authors indicated no financial relationships.
References
- 1. Zhang L, Zhu F, Xie L et al. Clinical characteristics of COVID‐19‐infected cancer patients: A retrospective case study in three hospitals within Wuhan, China. Ann Oncol 2020;31:894–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Al‐Shamsi HO, Alhazzani W, Alhuraiji A et al. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (COVID‐19) pandemic: An international collaborative group. The Oncologist 2020;25:e936–e945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Flaxman S, Mishra S, Gandy A et al. Estimating the effects of non‐pharmaceutical interventions on COVID‐19 in Europe. Nature 2020;584:257–261. [DOI] [PubMed] [Google Scholar]
- 4. Chia PY, Coleman KK, Tan YK et al.; Singapore 2019 Novel Coronavirus Outbreak Research Team. Detection of air and surface contamination by SARS‐CoV‐2 in hospital rooms of infected patients. Nature Commun 2020;11:2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Adikari A, de Silva D, Ranasinghe WKB et al. Can online support groups address psychological morbidity of cancer patients? An artificial intelligence based investigation of prostate cancer trajectories. PLoS One 2020;15:e0229361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. De Silva D, Ranasinghe W, Bandaragoda T et al. Machine learning to support social media empowered patients in cancer care and cancer treatment decisions. PLoS One 2018;13:e0205855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Stone L. You've got a friend online. Nat Rev Urol 2020;17:320. [DOI] [PubMed] [Google Scholar]
- 8. Plutchik R. The nature of emotions: Human emotions have deep evolutionary roots, a fact that may explain their complexity and provide tools for clinical practice. Am Sci 2001;89:344–350. [Google Scholar]
- 9. Burki TK. Cancer guidelines during the COVID‐19 pandemic. Lancet Oncol 2020;21:629–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kutikov A, Weinberg DS, Edelman MJ et al. A war on two fronts: Cancer care in the time of COVID‐19. Ann Intern Med 2020;172:756–758. [DOI] [PMC free article] [PubMed] [Google Scholar]


