Abstract
Background and Aim
During this COVID‐19 pandemic, Taiwan is one of the few countries where fecal immunochemical test and endoscopic activity for colorectal cancer screening keeps ongoing. We aimed to investigate how screening uptake and colonoscopy rate were affected in one of the biggest screening hubs in Northern Taiwan.
Methods
We conducted a prospective observational study tracing and analyzing the screening uptake and the trend of compliance to diagnostic colonoscopy in fecal immunochemical test‐positive subjects in the National Taiwan University Hospital screening hub since the outbreak of COVID‐19 and compared it with that of the corresponding periods in the past 3 years. Cancellation and rescheduling rates of colonoscopy and related reasons were also explored.
Results
Screening uptake during December 2019 to April 2020 was 88.8%, which was significantly lower than that in the corresponding period of the past 3 years (91.2–92.7%, P for trend < 0.0001). Colonoscopy rate in this period was 66.1%, which was also significantly lower than that in the past 3 years (70.2–77.5%, P for trend = 0.017). Rescheduling or cancellation rate was up to 10.9%, which was significantly higher than that in the past 3 years (P for trend = 0.023), and half of them was due to the fear of being infected.
Conclusion
Fecal immunochemical test screening was significantly affected by COVID‐19 pandemic. In order to resume the practice in COVID‐19 era, screening organizers should consider various approaches to secure timely diagnosis of colorectal cancer.
Keywords: Colonoscopy, Colorectal cancer, COVID‐19, Screening
Introduction
Fecal immunochemical test (FIT) is the most widely used test for population colorectal cancer (CRC) screening, and it can select high‐risk subjects for colonoscopy from a large population. The risk of having invasive CRC in FIT‐positive subjects is around 4% to 5% in asymptomatic populations aged 50 to 75 years, which is 20 times higher than that in the general population. 1 Accordingly, those with positive FIT should be all referred for diagnostic colonoscopy and subsequent treatment if any neoplasm is detected. Timely referral for colonoscopy is crucial for securing the effectiveness of an FIT screening program, but it may be affected by several factors, including that of the patients or the health‐care providers. Several recent studies have demonstrated that delay in colonoscopy after positive FIT was associated with a higher risk of CRC and advanced stage CRC at colonoscopy or even subsequent CRC death. 2 , 3 , 4
Taiwan was originally expected to have a catastrophic outbreak of COVID‐19 due to its geographic proximity to China, but as of October 2, 2020, there were only 517 confirmed cases, mostly imported, and 7 deaths. 5 , 6 , 7 The first confirmed case in Taiwan was announced on January 21, and the government chartered flight and brought back 247 evacuees from Wuhan on February 3, and on February 6, suspended docking of international cruises. On February 16, Taiwan announced the first reported death from COVID‐19 and widened testing criteria to anyone with travel or contact history or in high‐risk groups. The number of confirmed cases reached its peak during mid‐March when there was a surge of homeward bound tide from endemic countries and then decreased gradually (Fig. 1). Nevertheless, the endemic is rather well controlled in Taiwan; those events, either aforementioned domestic events or foreign ones, might have affected the willingness of the people to seek ordinary health‐care service, including CRC screening and diagnostic colonoscopy after a positive FIT. Since the outbreak of COVID‐19, several guidelines from major endoscopy societies recommended deferment of elective endoscopies to help to preserve the surge capacity for hospitals to manage a massive number of suspected or confirmed COVID‐19 cases and also to safeguard the potential transmission of COVID‐19 between patients and health‐care providers. 8 , 9 , 10 , 11 , 12 , 13 Unlike other countries, endoscopy service in Taiwan is not totally shut down during the COVID‐19 pandemic, but on the contrary, CRC screening activity and ordinary endoscopy service has been kept ongoing.
Figure 1.
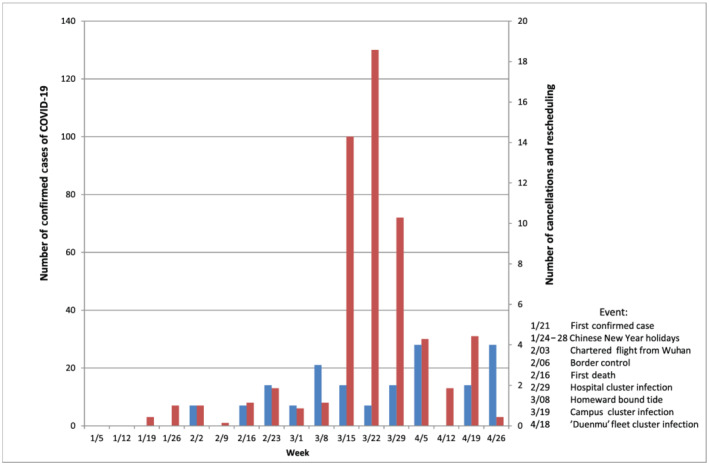
Chronological events showing the correlation between confirmed cases and cancellations and rescheduling cases
Because COVID‐19 pandemic is considered as a potential barrier to endoscopic procedures, for both patients and health‐care providers, we hypothesized that it may affect the compliance to diagnostic colonoscopy in the FIT screening program and concurrently the willingness to go for FIT screening. In this study, we aim to investigate how FIT screening and colonoscopy rates were affected by the COVID‐19 pandemic in Taiwan during the pandemic period by analyzing the CRC screening activity data in one of the biggest screening hubs in Northern Taiwan.
Methods
Study setting
Beginning in 2004, the Taiwan CRC Screening Program currently invites residents ages 50 to 75 years for biennial FIT screening. To cover more than 7 million eligible residents in 25 municipalities, the Health Promotion Administration of Ministry of Health and Welfare, the screening organizer of this program, provides FIT in either in‐reach (hospital or clinic) or out‐reach (regional health bureau or community health center) fashion. Details of this screening program have been described elsewhere. 1 , 14 In this screening program, a cut‐off of 20 μg hemoglobin/g of stool was used to determine positivity of FIT, and those with positive tests are notified with postcard or telephone and referred for verification colonoscopy. Subjects with positive FIT are advised to go for diagnostic colonoscopy within 3 months.
National Taiwan University Hospital (NTUH) is a 2000‐bed tertiary referral center located at Taipei, which is one of the biggest in‐reach screening hubs in Northern Taiwan. In 2019, there were totally 17 584 subjects that obtained FIT kits (OC‐Sensor, Eiken Chemical Ltd. Co., Tokyo, Japan) from our hub, and 74.2% received diagnostic colonoscopy for positive FIT. In the NTUH hub, a dedicated Cancer Administration and Coordination Center is in charge of cancer screening tasks and provides an integrated service of colorectal, oral, breast, and cervical cancer screening at once for outpatient, inpatient, community, and even staff of the hospital. It is functioning in a full day session from 9 AM to 5 PM with six case managers, one assistant, and a physician‐in‐charge. Take CRC screening as an example, people eligible for screening can obtain FIT kit in this unit, and the case managers collect FIT from patients, send postal reports to the patients, make phone calls to those with positive findings, arrange colonoscopy appointments for FIT‐positive cases, and upload the final result to the governmental screening organizer (Taiwan CRC Screening Program). All of the aforementioned screening activities were monitored and recorded regularly.
Study design and population
This is a prospective observational study tracing and analyzing the trend of compliance to diagnostic colonoscopy in FIT‐positive subjects in the NTUH screening hub since the outbreak of COVID‐19, which was defined as the appearance of the first confirmed case in Taiwan (January 21, 2020) and compared it with that of the corresponding periods in the past 3 years. We have noticed there is a decrease in the FIT screening uptake ever since the first outbreak in Taiwan and inspired to conduct the study by the end of January 2020. During this pandemic, there is no drastic change in terms of screening guideline, methods except infection control measures such as washing hands, wearing masks, and taking temperatures for all patients receiving CRC screening or diagnostic colonoscopy. For this purpose, we reviewed individuals aged 50 to 75 years who had participated in the FIT screening program at our hospital from Q4 of 2019 to Q1 of 2020, during which COVID‐19 pandemic was most prominent, and compared with that of Q4 of 2016 to Q1 of 2017, Q4 of 2017 to Q1 of 2018, and Q4 of 2018 to Q1 of 2019. Those with missing data were excluded. Relevant data, including contact information for those who were screened, were obtained from the screening program database, which is managed by the Health Promotion Administration. Ethical approval of this study was obtained from Taiwan University Hospital Institutional Review Board (reference number: 202006032W).
Definition
Screening uptake is defined as the number of subjects who submitted FIT kits divided by the number of subjects to whom FIT kits were given. Positivity rate is defined as the number of subjects with positive FIT divided by the number of subjects who submitted FIT kits. Colonoscopy rate is defined as the number of subjects who underwent colonoscopy divided by the number of subjects with positive FIT. As per the guidelines of the government, diagnostic colonoscopy is recommended within 3 months of positive FIT; therefore, the colonoscopy rate of each month in this study refers to the cumulated colonoscopy completion rate for those who received FIT and had positive tests 3 months before.
Of those who were referred for colonoscopy, some canceled or postponed their colonoscopy schedule. Cancellation rate is defined as the number of subjects who asked for canceling their colonoscopy schedule or did not show up for colonoscopy divided by the number of subjects to whom colonoscopy has been scheduled. Reschedule rate is defined as the number of subjects who asked for postponing their colonoscopy schedule divided by the number of subjects to whom colonoscopy has been scheduled.
Data processing and analysis
Data pertaining to this in‐reach screening was stored in the hospital database. Descriptive analysis was performed to demonstrate the sample characteristics by using frequency, percentage, and range for categorical data and mean and SD for continuous data. Comparison of FIT screening uptake, colonoscopy rate, and cancellation or rescheduling rates with corresponding period of the past 3 years was made using Cochran–Armitage trend test. Excel software (Microsoft Co. Ltd., WA, USA) was used for data analysis. P < 0.05 was considered as statistically significant.
Results
Demographics of screened invited for fecal immunochemical test screening at National Taiwan University Hospital screening hub
Table 1 showed the mean age and gender proportion of eligible people invited for FIT screening in the Q4 to Q1 season of 2020 and the past 3 years. The average age is 62 years old. The number of subjects visited for obtaining FIT was apparently decreased during Q4 2019 to Q1 2020 as compared with the past 3 years.
TABLE 1.
Demographics of subjects invited for fecal immunochemical test screening during Q4 to Q1 in National Taiwan University Hospital hub in recent 4 years
| Q4 2019 to Q1 2020 | Q4 2018 to Q1 2019 | Q4 2017 to Q1 2018 | Q4 2016 to Q1 2017 | |
|---|---|---|---|---|
| n = 6392 | n = 8627 | n = 7730 | n = 7922 | |
| Mean age (SD) | 62.3 ± 7.1 | 63.1 ± 7.1 | 62.9 ± 7.2 | 62 ± 6.9 |
| Male gender, n (%) | 3221 (50.4) | 4008 (46.5) | 3676 (47.6) | 3859 (48.7) |
Screening uptake for fecal immunochemical test in National Taiwan University Hospital screening hub
Table 2 showed the overall 4‐year screening uptake at NTUH screening hub. Screening uptake during Q4 2019 to Q1 2020 was 88.1%, which was significantly lower than that in the past 3 years (92.1%, 91.2%, and 92.7% in Q4 2018 to Q1 2019, Q4 2017 to Q1 2018, and Q4 2016 to Q1 2017) (P for trend < 0.0001).
TABLE 2.
Screening uptake for fecal immunochemical test (FIT) in National Taiwan University Hospital hub in recent 5 years
| Q4 2019 to Q1 2020 | Q4 2018 to Q1 2019 | Q4 2017 to Q1 2018 | Q4 2016 to Q1 2017 | |
|---|---|---|---|---|
| FIT kits delivered | 6392 | 8627 | 7730 | 7922 |
| FIT kits returned | 5675 | 7944 | 7053 | 7345 |
| Screening uptake (%) | 88.8 | 92.1 | 91.2 | 92.7 |
| Positive tests | 431 | 591 | 501 | 507 |
| Positivity rate (%) | 7.6% | 7.4% | 7.1% | 6.9% |
P value of Cochran–Armitage test for screening uptake < 0.0001.
Screening uptake = Number of subjects who submitted FIT kits/Number of subjects to whom FIT kits were given. Positivity rate = Number of subjects with positive FIT/Number of subjects who submitted FIT kits.
Completion rate of confirmatory colonoscopy in Q1 of each year
The chronological trend of the number of confirmed COVID‐19 cases together with the number of rescheduling or cancellation of diagnostic colonoscopy after positive FIT is demonstrated in Figure 1. Table 3 demonstrated the diagnostic colonoscopy rate in Q1 of 2020 and in the past 3 years. The colonoscopy rate was 66.1% in Q1 of 2020, which was significantly lower than that in the corresponding period of the past 3 years (70.2%, 77.5%, and 75.4% in 2017, 2018, and 2019, P for trend = 0.017). In this year, there is a rescheduling rate, which is defined as a change of initially scheduled timing of colonoscopy up to 7.8% and cancellation rate of 3.1%, both possibly due to the pandemic. The overall rescheduling or cancellation rate of 10.9% was significantly higher than that of the past 3 years (P for trend = 0.023).
TABLE 3.
Colonoscopy completion rate in Q1 of each year in recent 4 years
| Q1 2020 | Q1 2019 | Q1 2018 | Q1 2017 | |
|---|---|---|---|---|
| Colonoscopy scheduled, n † | 180 | 181 | 191 | 203 |
| Colonoscopy completed, n (%) | 119 (66.1) | 127 (70.2) | 148 (77.5) | 153 (75.4) |
| Total number of appointments | 128 | 130 | 152 | 155 |
| Cancellation, n (%) | 4 (3.1) | 3 (2.3) | 4 (2.6) | 2 (1.3) |
| Reschedule, n (%) | 10 ‡ (7.8) | 1 (0.8) | 5 (3.3) | 3 (1.9) |
P value of Cochran–Armitage test for colonoscopy rate = 0.017.
P value of Cochran–Armitage test for cancellation or rescheduling rate = 0.023.
The number of subjects to whom colonoscopy was scheduled in this period was based on the number of fecal immunochemical test (FIT) positive in the previous 3 months and therefore is not exactly the same as FIT‐positive subjects in Table 2.
Five of them has yet received colonoscopy and rescheduled to a date later than May.
Colonoscopy rate = Number of subjects who received colonoscopy/Number of subjects with positive FIT (this number trace back 3 months as per the guidelines by our screening program, which recommend diagnostic colonoscopy within 3 months). Reschedule rate = Number of subjects who asked of postponing colonoscopy schedule/Number of subjects to whom colonoscopy has been scheduled.
Reasons of changing schedule and cancellation for colonoscopy after positive fecal immunochemical test
From Table 4, two of four (50%) FIT‐positive subjects declined diagnostic colonoscopy in Q1 2020 due to the fear of being infected. As for rescheduling, 5 of 10 (50%) FIT‐positive screened rescheduled due to fear of being infected. Such a reason for cancellation or changing the schedule of colonoscopy never appeared in the past 3 years.
TABLE 4.
Specific reasons for changing or cancellation of colonoscopy schedule
| Q1 2020 | Q1 2019 | Q1 2018 | Q1 2017 | |
|---|---|---|---|---|
| Cancellation, n | 4 | 3 | 4 | 2 |
| Comorbidity | 1 (25%) | 3 (100%) | 1 (25%) | 1 (50%) |
| Wait too long | 1 (25%) | 0 | 1 (25%) | 0 |
| Refuse further contact or no show on colonoscopy day | 0 | 0 | 2 (50%) | 1 (50%) |
| Fear of infection † | 2 (50%) | 0 | 0 | 0 |
| Rescheduling, n | 10 | 1 | 5 | 3 |
| Comorbidity | 2 (20%) | 1 (100%) | 2 (40%) | 3 (100%) |
| No accompany person on initially scheduled date | 3 (30%) | 0 | 3 (60%) | 0 |
| Fear of infection † | 5 (50%) | 0 | 0 | 0 |
Fear of infection: fear of being infected on the way to or back from hospital, or fear of being infected in the hospital.
Discussion
In this prospective observational study tracing and analyzing the trend of FIT screening activity in a big CRC screening hub in Northern Taiwan since the outbreak of COVID‐19, we observed decreased FIT screening uptake rate and the rate of diagnostic colonoscopy after positive FIT. Specifically, the cancellation rate and rescheduling rate fluctuated along with each significant endemic event such as the appearance of the first confirmed case, first death case, hospital cluster infection, homeward bound tide, and navy fleet cluster infection. 7 The fear of nosocomial infection on the way or during the stay in hospital are among those most likely reasons for such phenomenon.
Our study emphasized the importance of timely completion of a positive FIT test as published by previous studies; Corley et al. conducted a retrospective cohort study and concluded that among patients with a positive FIT result, compared with follow‐up colonoscopy at 8 to 30 days, follow‐up after 10 months was associated with a higher risk of CRC and more advanced‐stage disease at the time of diagnosis. 2 A cohort study conducted in Taiwan using data from the Taiwan CRC Screening Program found that among patients with positive results from an FIT, risks of CRC and advanced‐stage disease increase with time. 3 A study conducted in Israel also demonstrated, compared to colonoscopy follow‐up within 0–3 months, risks for any CRC and advanced‐stage disease were higher for a follow‐up of 12–24 months: odds ratio, 1.97 (95% confidence interval, 1.51–2.56) and 1.88 (95% confidence interval, 1.43–2.46), respectively. 4 Recent study has also indicated such a concern on delayed diagnosis of CRC due to COVID‐19 pandemic and the projected results of simulation revealing remarkably increased cases of CRC, CRC death, and loss of life‐years.
Previous studies revealed that there are sociodemographic factors affecting non‐adherence to CRC screening uptake, which include ethnicity, gender, age, and possessing insurance. 15 , 16 , 17 , 18 , 19 In a large‐scale, population‐based survey, our previous study concluded that younger age, being married, higher perceived threat, higher cues for action, and a higher health behavior score were associated with the willingness of having a diagnostic colonoscopy in the FIT screening setting. On the other hand, a perceived barrier was negatively associated with having a colonoscopy. 20 The spread of COVID‐19 pandemic has significantly reduced patient number of hospital visits in fear of being infected; patients might feel insecure with the hospital environment, colonoscopy procedure, and any possible contact with the pathogen. Adding the chronological coincidence of such a trend and endemic events, pandemic is therefore considered as the new barrier to completion of diagnostic colonoscopy. As an ancillary analysis, we also compared the demographic characteristics of subjects who canceled or rescheduled colonoscopy with those who were compliant to FIT screening or to colonoscopy after positive FIT and did not find any significant difference (Tables S1–S3). Accordingly, we may conclude that the impact on the willingness to undergo diagnostic colonoscopy is universal across different age, gender, and educational levels and reassurance of the necessity and safety of timely colonoscopy after positive FIT to the entire population is indispensable.
The impact of COVID‐19 on health service is tremendous and beyond imagination, ranging from vaccine coverage, sex and reproductive health, trauma in mental health, and cancer care delivery. 21 , 22 , 23 , 24 As for endoscopy, risk of transmission may occur during endoscopy, from patient to doctor or vice versa. The European Society of Gastrointestinal Endoscopy, the European Society of Gastroenterology and Endoscopy Nurses Associates, and the Asian Pacific Society for Digestive Endoscopy have developed position papers including patient triage and risk assessment before endoscopy, resource prioritization and allocation, regular monitoring of personal protective equipment, infection control measures, protective device training, and implementation of a stepwise strategy for resumption of endoscopy services after control of the COVID‐19 outbreak. 8 , 10 It is, however, unclear at what level of endemic that we should resume endoscopy.
While a majority of endoscopy units worldwide only perform emergent procedures as the result of lockdown and social distancing, the American Gastroenterological Association suggested measures to resume routine practices. At the time of canceling the endoscopy appointment, the nurse and medical staff should perform a brief interview on the indication of the individual procedure and double check it with the medical prescription, register in the hospital database, categorizing them as time sensitive (TS) or not TS. In the first group, exams required for symptoms of recent onset (4–6 weeks) should be included. The TS group includes the following two subgroups: subgroup A, chronic symptoms or post‐polypectomy surveillance for high‐risk lesions, or for any dysplastic lesion in the upper gastrointestinal tract; and subgroup B, post‐polypectomy surveillance for low‐risk lesions and for screening, or surveillance of an upper gastrointestinal pre‐neoplastic risk condition but without dysplasia. 11 , 13
Diagnostic colonoscopy after positive FIT obviously belongs to TS procedure as FIT‐positive population carries a 20‐fold to 30‐fold risk of CRC compared with the general population, representing a very high‐risk group for CRC. 1 Delay of diagnostic colonoscopy may lead to increased likelihood of detecting a lesion at a more advanced or non‐curable stage. Rescheduling of or prolongation of waiting for colonoscopy is related with cancellation of colonoscopy, which may lead to more grave outcomes. 25 Our previous study has demonstrated that if people are not compliant to colonoscopy after positive FITs, then there was 60% higher risk of CRC death compared with those who were compliant. 26 In the long run, the effectiveness of the entire screening program would be hampered.
In order to resume the CRC screening and diagnostic colonoscopy, in the era of COVID‐19, in addition to establishing guidelines, the health‐care professionals need to reassure to the public the importance of continuing FIT screening and timely completion of diagnostic colonoscopy if the test is positive, develop the stool rapid test for COVID‐19 to secure the safety, advocate the general public to obtain the FIT kit and return the stool sample by postal mail, and arrange screening activity outside of the hospitals to avoid the possibility of cluster infection.
Taiwan is one of a few countries where CRC screening and endoscopy are normally functioning under the threat of COVID‐19 pandemic. Our record of cancellation or rescheduling of diagnostic colonoscopy is rather comprehensive and evidence based; however, it is a single center study, and the external validity may be limited. In addition, we only evaluate the first quarter of the year; the long run effect due to the pandemic is unclear at the present stage. Even if the colonoscopy rate could be made up in the upcoming months, delayed time might have caused some irreversible loss (i.e. progression to advanced stage cancers), and the impact on the effectiveness of the entire screening program should be carefully monitored.
Along with the stabilized endemic in Taiwan, the number of patients visiting hospitals increased gradually, but it is unclear whether COVID‐19 would enter into long‐term circulation in an annual, biennial, or sporadic pattern, which is dependent on whether the population could acquire long‐term immunity or effective vaccine and antiviral agent could be developed. 27 From the policy perspective, screening organizers should construct a fast‐track diagnostic colonoscopy for FIT‐positive cases within the screening program or prioritize the FIT‐positive subjects stratified by fecal hemoglobin concentration, which has very close association with the likelihood of having advanced neoplasm at colonoscopy. 28 , 29
Conclusion
In a normally functioning screening hub and endoscopy unit, we still observed a decreased CRC screening uptake and apparent cancellation or rescheduling rate of diagnostic colonoscopy after positive FIT under the impact of COVID‐19 pandemic, which is detrimental to the detection of possible CRC or advanced adenoma. In order to resume the practice in such a COVID‐19 era, several measures such as public education, patient reassurance, or designing a fast‐track colonoscopy for FIT‐positive subjects should be considered to secure timely diagnosis of CRC.
Supporting information
Table S1. Comparison of characteristics of FIT screening participants and those who cancelled or rescheduled colonoscopy.
Table S2. Comparison of characteristics of subjects with positive FIT and those who cancelled or rescheduled colonoscopy.
Table S3. Comparison of colonoscopy compilers after positive FIT and those who cancelled or rescheduled colonoscopy.
Acknowledgment
The authors thank Cancer Administration and Coordination Center, National Taiwan University Hospital for full support.
Cheng, S.‐Y. , Chen, C.‐F. , He, H.‐C. , Chang, L.‐C. , Hsu, W.‐F. , Wu, M.‐S. , and Chiu, H.‐M. (2021) Impact of COVID‐19 pandemic on fecal immunochemical test screening uptake and compliance to diagnostic colonoscopy. Journal of Gastroenterology and Hepatology, 36: 1614–1619. 10.1111/jgh.15325.
Declaration of conflict of interest: The authors declare no conflict or competing interests.
Finacial support: Health Promotion Administration, Ministry of Health and Welfare (A1081113), Taiwan.
References
- 1. Chiu HM, Chen SL, Yen AM et al. Effectiveness of fecal immunochemical testing in reducing colorectal cancer mortality from the One Million Taiwanese Screening Program. Cancer 2015; 121: 3221–3229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Corley DA, Jensen CD, Quinn VP et al. Association between time to colonoscopy after a positive fecal test result and risk of colorectal cancer and cancer stage at diagnosis. JAMA 2017; 317: 1631–1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lee YC, Fann JC, Chiang TH et al. Time to colonoscopy and risk of colorectal cancer in patients with positive results from fecal immunochemical tests. Clin. Gastroenterol. Hepatol. 2019; 17: 1332–1340 e3. [DOI] [PubMed] [Google Scholar]
- 4. Beshara A, Ahoroni M, Comanester D et al. Association between time to colonoscopy after a positive guaiac fecal test result and risk of colorectal cancer and advanced stage disease at diagnosis. Int. J. Cancer 2020; 146: 1532–1540. [DOI] [PubMed] [Google Scholar]
- 5. Wang CJ, Ng CY, Brook RH. Response to COVID‐19 in Taiwan: big data analytics, new technology, and proactive testing. JAMA 2020; 323: 1341–1342. [DOI] [PubMed] [Google Scholar]
- 6. University JH . COVID‐19 dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University.
- 7. Coronavirus disease 2019 (COVID‐19) . Taiwan Center for Disease Control.
- 8. Chiu PWY, Ng SC, Inoue H et al. Practice of endoscopy during COVID‐19 pandemic: position statements of the Asian Pacific Society for Digestive Endoscopy (APSDE‐COVID statements). Gut 2020; 69: 991–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Repici A, Maselli R, Colombo M et al. Coronavirus (COVID‐19) outbreak: what the department of endoscopy should know. Gastrointest. Endosc. 2020. (In Press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gralnek IM, Hassan C, Beilenhoff U et al. ESGE and ESGENA Position Statement on gastrointestinal endoscopy and the COVID‐19 pandemic. Endoscopy 2020. (In Press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sultan S, Lim JK, Altayar O et al. AGA Institute rapid recommendations for gastrointestinal procedures during the COVID‐19 pandemic. Gastroenterology 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Repici A, Pace F, Gabbiadini R et al. Endoscopy units and the COVID‐19 outbreak: a multi‐center experience from Italy. Gastroenterology 2020; 159: 363–366.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Amato A, Rondonotti E, Radaelli F. Lay‐off of endoscopy services for the COVID‐19 pandemic: how can we resume the practice of routine cases? Gastroenterology 2020; S0016–5085(20)30568–0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chou CK, Chen SL, Yen AM et al. Outreach and inreach organized service screening programs for colorectal cancer. PLoS One. 2016; 11: e0155276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Crawford ND, Jones CP, Richardson LC. Understanding racial and ethnic disparities in colorectal cancer screening: Behavioral Risk Factor Surveillance System, 2002 and 2004. Ethn. Dis. 2010; 20: 359–365. [PubMed] [Google Scholar]
- 16. Goel MS, Wee CC, McCarthy EP, Davis RB, Ngo‐Metzger Q, Phillips RS. Racial and ethnic disparities in cancer screening: the importance of foreign birth as a barrier to care. J. Gen. Intern. Med. 2003; 18: 1028–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Koo JH, You MY, Liu K et al. Colorectal cancer screening practise is influenced by ethnicity of medical practitioner and patient. J. Gastroenterol. Hepatol. 2012; 27: 390–396. [DOI] [PubMed] [Google Scholar]
- 18. Wong MC, Ching JY, Hirai HH et al. Perceived obstacles of colorectal cancer screening and their associated factors among 10,078 Chinese participants. PLoS One. 2013; 8: e70209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Malila N, Oivanen T, Malminiemi O, Hakama M. Test, episode, and programme sensitivities of screening for colorectal cancer as a public health policy in Finland: experimental design. BMJ 2008; 337: a2261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cheng SY, Li MC, Chia SL et al. Factors affecting compliance with confirmatory colonoscopy after a positive fecal immunochemical test in a national colorectal screening program. Cancer 2018; 124: 907–915. [DOI] [PubMed] [Google Scholar]
- 21. Hungerford D, Cunliffe NA. Coronavirus disease (COVID‐19)—impact on vaccine preventable diseases. Euro Surveill. 2020; 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Riley T, Sully E, Ahmed Z, Biddlecom A. Estimates of the potential impact of the COVID‐19 pandemic on sexual and reproductive health in low‐ and middle‐income countries. Int. Perspect. Sex. Reprod. Health 2020; 46: 73–76. [DOI] [PubMed] [Google Scholar]
- 23. Lima CKT, Carvalho PMM, Lima I et al. The emotional impact of Coronavirus 2019‐nCoV (new Coronavirus disease). Psychiatry Res. 2020; 287: 112915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Shankar A, Saini D, Roy S et al. Cancer care delivery challenges amidst coronavirus disease‐19 (COVID‐19) outbreak: specific precautions for cancer patients and cancer care providers to prevent spread. Asian Pac. J. Cancer Prev. 2020; 21: 569–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Jen HH, Hsu CY, Chen SL et al. Rolling‐out screening volume affecting compliance rate and waiting time of FIT‐based colonoscopy. J. Clin. Gastroenterol. 2018; 52: 821–827. [DOI] [PubMed] [Google Scholar]
- 26. Lee YC, Li‐Sheng Chen S, Ming‐Fang Yen A et al. Association between colorectal cancer mortality and gradient fecal hemoglobin concentration in colonoscopy noncompliers. J. Natl. Cancer Inst. 2017; 109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kissler SM, Tedijanto C, Goldstein E, Grad YH, Lipsitch M. Projecting the transmission dynamics of SARS‐CoV‐2 through the postpandemic period. Science 2020. (In Press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Auge JM, Pellise M, Escudero JM et al. Risk stratification for advanced colorectal neoplasia according to fecal hemoglobin concentration in a colorectal cancer screening program. Gastroenterology 2014; 147: 628–636 e1. [DOI] [PubMed] [Google Scholar]
- 29. Chiu SY, Chuang SL, Chen SL et al. Faecal haemoglobin concentration influences risk prediction of interval cancers resulting from inadequate colonoscopy quality: analysis of the Taiwanese Nationwide Colorectal Cancer Screening Program. Gut 2017; 66: 293–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Comparison of characteristics of FIT screening participants and those who cancelled or rescheduled colonoscopy.
Table S2. Comparison of characteristics of subjects with positive FIT and those who cancelled or rescheduled colonoscopy.
Table S3. Comparison of colonoscopy compilers after positive FIT and those who cancelled or rescheduled colonoscopy.


