Abstract
Objectives
The aim of this study was to assess the impact of the coronavirus disease 2019 (COVID‐19) outbreak on incidence, delays, and outcomes of ST‐elevation myocardial infarction (STEMI) patients undergoing primary percutaneous coronary intervention (PPCI) in France.
Methods
We analyzed all patients undergoing PPCI <24 hours STEMI included in the prospective France PCI registry. The 2 groups were compared on mean monthly number of patients, delays in the pathway care, and in‐hospital major adverse cardiac events (MACE: death, stent thrombosis, myocardial infarction, unplanned coronary revascularization, stroke, and major bleeding).
Results
From January 15, 2019 to April 14, 2020, 2064 STEMI patients undergoing PPCI were included: 1942 in the prelockdown group and 122 in the lockdown group. Only 2 cases in the lockdown group were positive for COVID‐19. A significant drop (12%) in mean number of STEMI/month was observed in the lockdown group compared with prelockdown (139 vs 122, P < 0.04). A significant increase in “symptom onset to first medical contact” delay was found for patients who presented directly to the emergency department (ED) (238 minutes vs 450 minutes; P = 0.04). There were higher rates of in‐hospital MACE (7.7% vs 12.3%; P = 0.06) and mortality (4.9% vs 8.2%; P = 0.11) in the lockdown group but the differences were not significant.
Conclusion
According to the multicenter France PCI registry, the COVID‐19 outbreak in France was associated with a significant decline in STEMI undergoing PPCI and longer transfer time for patients who presented directly to the ED. Mortality rates doubled, but the difference was not statistically significant.
Keywords: Acute coronary syndrom, COVID‐19, Myocardial infarction, Percutaneous coronary intervention, STEMI
1. INTRODUCTION
1.1. Background
Acute ST‐elevation myocardial infarction (STEMI) is the major cardiac emergency that most hospital cardiologists deal with daily. Rapid reperfusion of the culprit artery by primary percutaneous coronary intervention (PPCI) is recommended for optimal outcomes. 1 , 2
Emergency medical systems (EMS) are organized to minimize the time required to transfer patients to the catheterization laboratory (cath lab). 3
1.2. Importance
The coronavirus disease 2019 (COVID‐19) outbreak has threatened European health care systems, potentially overshadowing other emergencies including STEMI. This has led to a change in the organization of the health care system for the management of patients without COVID‐19. All non‐emergency interventions have been downgraded and postponed. The Society for Cardiac Angiography and Interventions (SCAI) and the European Association of Percutaneous Cardiovascular Interventions (EAPCI) continue to recommend PPCI as the standard treatment of STEMI patients during the current pandemic. 4 , 5 However, there are no data available on the effects of this strategy during a pandemic.
In many countries, a lockdown was imposed by the authorities in order to slow the progression of the virus and avoid hospital crowding. In France, the lockdown was implemented throughout the country. This situation may have discouraged patients from coming to the hospital. An impact on time from onset to first medical contact (FMC) for STEMI patients can be expected, but it may be influenced by opposing factors: overwhelmed EMSs would delay care, for example, but reduced intensity of road traffic would speed up transfer to care centers.
1.3. Goal of this investigation
The aim of this study was to assess the impact of the COVID‐19 outbreak on incidence, delays, and outcomes of STEMI in patients undergoing PPCI in France.
2. METHODS
2.1. Registry design
The prospective multicenter France PCI registry, started on January 1, 2014, collects all patients undergoing coronary angiography or coronary angioplasty at 16 interventional cardiology centers (ICC) participating in 3 different French regions (Centre Val de Loire, Auvergne Rhône Alpes, and Normandie; Figure 1). The basic methodology for the France PCI registry (originally named CRAC) has been previously described. Out‐of‐hospital, clinical, and procedural data are collected prospectively by cardiologists at the time of the patient's admission to ICC and recorded in electronic reporting software (CardioReport; CVX Medical, Croissy‐Beaubourg, France). The data are of high quality, 99.6% of completeness and with 89% of consistency. 6 The registry is registered with clinicaltrials.org (NCT02778724).
FIGURE 1.
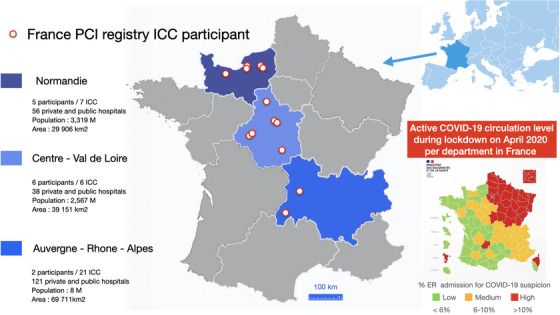
Participating centers in the France PCI percutaneous coronary intervention (PCI) registry. The 11 interventional cardiology centers (ICCs) included were located in 3 administrative regions in western France (Normandie, Centre Val de Loire, and Auvergne Rhône Alpes), which were less affected by the COVID‐19 outbreak than the eastern part during lockdown on April 2020
The study was conducted according to contemporary clinical practice guidelines and French regulations (Advisory Committee on Information Processing in Material Research in the Field of Health no. 13.245). The French Persons Protection Committee (IRB00003888) approved the study protocol (no. 15–231). Data file collection and storage were approved by the French National Commission for Data Protection and Liberties (no. 2014–073). All patients were informed of the aims of the survey. All included patients gave their informed consent to participate before data collection.
2.1.1. Selection of subjects
The current analysis included all consecutive patients undergoing PPCI for STEMI between January 15, 2019 and April 14, 2020. Four ICC centers that started their inclusion after January 15, 2019 and 1 center with incomplete data were excluded from the study. We also excluded fibrinolysis, late presentation STEMI (>24 hours), and patients without PPCI. The study population was divided into 2 groups: the prelockdown group (patients included before March 15, 2020, that is, date of national lockdown announcement) and the lockdown group (patients included from March 15 to April 14, 2020).
The Bottom Line
Societal “lockdowns” for coronavirus disease 2019 (COVID‐19) have indirectly affected the care of other critical illness. In this analysis of 2064 patients from 16 hospitals in the France percutaneous coronary intervention (PCI) registry, COVID‐19 lockdown resulted in a 12% reduction in monthly ST‐elevation myocardial infarctions (STEMIs) but a more than 200‐minute increase in STEMI symptom reporting delays. Major adverse cardiovascular events and mortality were slightly higher, but the differences were not statistically significant. These results illustrate the effects of COVID‐19 societal lockdown upon STEMI care and outcomes.
2.1.2. Follow‐up
Patient follow‐up was conducted by local on‐site research technicians in the participating centers. Data were anonymized before automatic and daily transfer to the central France PCI database. Regional data monitoring was coordinated by the France PCI clinical research associate. External independent quality control (appropriate procedures, completeness, and consistency of data) was made periodically at each site by a multicenter research assistant.
2.1.3. Exposure
From March 16 to May 10, 2020, the French government ordered a large‐scale lockdown to counter the wave of COVID‐19 infections in the country. The lockdown halted non‐essential economic, educational, and entertainment activities, mandated people to remain at home and venture out only for essential reasons. Food retailers and health care institutions remained operational.
During the COVID 19 outbreak and according to current guidelines, 4 , 5 , 7 any STEMI patient was considered a carrier of COVID‐19. Accordingly, additional measures were introduced for the care of this population, including systematic protection of health care personnel and careful questioning of the patient. In order not to lengthen delays, PPCI was carried out with all the precautions considering the patient as a suspect at COVID‐19; testing for the virus and possibly chest computed tomography were performed only after the revascularization procedure. Patients were tested for the virus only if there was a clinical suspicion of COVID‐19 infection. This approach was taken by all interventional centers in France.
2.2. Outcome measures
The following outcomes were analyzed: (1) mean monthly number of patients undergoing PPCI for STEMI; (2) delays in the care pathway: patient delay, defined as the overall time from symptom onset to FMC; system delay, defined as the overall time from FMC to PPCI; and total ischemic time, defined as time from symptom onset to PPCI. In‐hospital outcomes were analyzed on a composite of death, definite stent thrombosis (Academic Research Consortium), myocardial infarction, unplanned coronary revascularization, stroke, and major bleeding (Bleeding Academic Research Consortium ≥3). FMC was defined as the time point for the qualifying electrocardiogram. 8
2.3. Statistical analysis
A descriptive method was used for the data analysis. The comparisons between periods for categorical data were performed using chi‐square or Fisher's exact tests. A mixed model with random intercepts corrected for time as a continuous variable was used to estimate the percent change between periods. All tests were 2‐sided, with a type I error set at 5%. All analyses were performed using Stata 15 (StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC).
3. RESULTS
From January 15, 2019 to April 14, 2020, 2064 STEMI patients undergoing PPCI were included: 1942 in the prelockdown group and 122 in the lockdown group (Figure 2). There were no significant differences in baseline characteristics between the 2 groups (Table 1). Only 2 patients in the lockdown group had a COVID‐19 infection, confirmed by a positive reverse transcription polymerase chain reaction test. Cardiogenic shock was almost twice as common in the lockdown group (2.9% vs 5.7%; P = 0.07).
FIGURE 2.
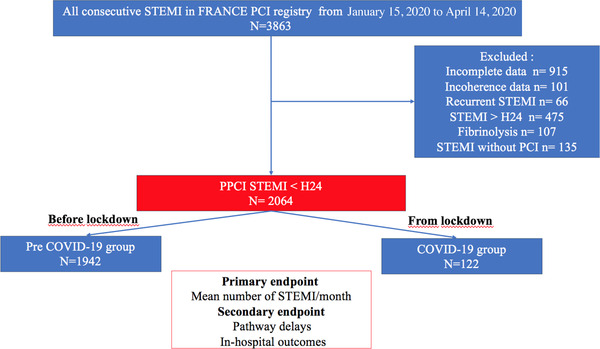
Flow chart. PCI, percutaneous coronary intervention; PPCI, primary percutaneous coronary intervention; STEMI, ST‐elevation myocardial infarction
TABLE 1.
Characteristics of STEMI patients undergoing PPCI according to lockdown period January 15, 2019 to April 14, 2020
| Overall population (N = 2064) | Pre‐lockdown group (N = 1942) | Lockdown group (N = 122) | |||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | P value | |
| Risk factors | |||||||
| Age ≥75 years | 489 | 23.8 | 463 | 23.8 | 26 | 21.3 | 0.52 |
| Age median [SD] | 63.56 [54–73] | 63.60 [54–73] | 62.93 [54–72] | 0.59 | |||
| Women | 501 | 24.3 | 465 | 23.9 | 36 | 29.5 | 0.16 |
| BMI ≥25 kg/m2 | 1297 | 63.8 | 1226 | 64.1 | 71 | 58.2 | 0.18 |
| Diabetes mellitus | 308 | 15.2 | 285 | 14.9 | 23 | 19 | 0.23 |
| Hypercholesterolemia | 629 | 33.4 | 596 | 33.8 | 33 | 28.2 | 0.21 |
| Hypertension | 857 | 42.4 | 802 | 42.2 | 55 | 45.8 | 0.43 |
| Current smoker | 780 | 38.4 | 732 | 38.3 | 48 | 39.7 | 0.26 |
| Medical history | |||||||
| Family history of CAD | 409 | 20.8 | 387 | 20.8 | 25 | 20.8 | 0.98 |
| Prior myocardial infarction | 140 | 6.8 | 135 | 7 | 5 | 4.1 | 0.22 |
| Prior PCI | 247 | 12 | 236 | 12.1 | 11 | 9 | 0.29 |
| Prior CABG | 35 | 1.7 | 35 | 1.8 | 0 | 0 | 0.13 |
| History of CADa | 271 | 13.1 | 259 | 13.3 | 12 | 9.8 | 0.26 |
| History of PAD | 77 | 3.8 | 73 | 3.8 | 4 | 3.3 | 0.75 |
| History of stroke | 63 | 3 | 60 | 3.1 | 3 | 2.5 | 0.69 |
| History of CKD | 61 | 3.3 | 55 | 3.1 | 6 | 5.4 | 0.20 |
| Clinical presentation | |||||||
| COVID‐19 status | 2 | 0.1 | 0 | 0 | 2 | 1.6 | / |
| Ischemia localization | |||||||
| Anterior | 859 | 42.5 | 802 | 42.3 | 57 | 46.7 | 0.33 |
| Inferior or lateral | 1161 | 57.5 | 1096 | 57.7 | 65 | 53.3 | 0.33 |
| LVEF < 40% | 220 | 22 | 204 | 21.9 | 16 | 23.9 | 0.70 |
| Cardiogenic shock | 63 | 3 | 56 | 2.9 | 7 | 5.7 | 0.07 |
| Cardiac arrest | 65 | 3.1 | 60 | 3.08 | 5 | 4.1 | / |
| Prehospital pathway | |||||||
| EMS call | 1333 | 64.6 | 1258 | 64.8 | 75 | 61.5 | 0.45 |
| FMC | 0.21 | ||||||
| EMS | 1345 | 65.3 | 1270 | 65.5 | 75 | 61.5 | |
| ED | 535 | 26 | 504 | 26 | 31 | 25.4 | |
| Others | 181 | 8.8 | 165 | 8.5 | 16 | 13.1 | |
| Optimal care pathwayb | 813 | 39.4 | 764 | 39.3 | 49 | 40.2 | 0.85 |
| Preprocedure medication | |||||||
| Antiplatelet therapy | |||||||
| Aspirin | 1985 | 96.3 | 1868 | 96.2 | 117 | 96.7 | 0.79 |
| P2Y12 inhibitor | 1919 | 93 | 1803 | 92.8 | 116 | 95.1 | 0.34 |
| Heparin | 1813 | 87.9 | 1700 | 87.6 | 113 | 93.4 | 0.05 |
| Procedural characteristics | |||||||
| Radial access | 1913 | 92.7 | 1803 | 92.9 | 110 | 90.2 | 0.26 |
| Number of diseased vessels | 0.84 | ||||||
| 0 | 5 | 0.2 | 5 | 0.3 | 0 | 0 | |
| 1 | 861 | 41.7 | 809 | 41.7 | 52 | 42.6 | |
| ≥2 | 1198 | 58 | 1128 | 58.1 | 70 | 57.38 | |
| Left main | 76 | 3.7 | 69 | 3.5 | 7 | 5.7 | 0.21 |
| N PCI site, mean | 2064 | 1.30 | 1942 | 1.29 | 122 | 1.37 | 0.24 |
| Drug eluting stent | 1817 | 88 | 1704 | 87.7 | 113 | 92.6 | 0.10 |
| N stents per procedure, mean | 2064 | 1.27 | 1942 | 1.26 | 122 | 1.37 | 0.18 |
| AGP2b3a | 469 | 22.8 | 444 | 22.9 | 25 | 20.7 | 0.32 |
| Thromboaspiration | 455 | 22 | 432 | 22.2 | 23 | 18.8 | 0.38 |
| PCI success | 2015 | 98.1 | 1898 | 98.2 | 117 | 96 | 0.06 |
AGP2b3, antiglycoprotein 2b3a; BMI, body mass index; CABG, coronary arterial bypass graft; CAD, coronary artery disease; CKD, chronic kidney disease; COVID‐19, coronavirus disease 2019; EMS, emergency medical system; ED, emergency department; FMC, first medical contact; LVEF, left ventricular ejection fraction; m [SD], mean (standard deviation); N, number; PAD, peripheral arterial disease; PCI, percutaneous coronary intervention; PPCI, primary percutaneous coronary intervention; STEMI, ST‐elevation myocardial infarction.
a Combination of the 3 previous variables.
b Pathway with only 1 medical practitioner before PCI.
There was a significant difference between the mean numbers of STEMI patients undergoing PPCI per month in the prelockdown and the lockdown groups (139 vs 122; P < 0.04) (Table 2). The “symptom onset‐FMC” delay in patients who presented directly to the ED was significantly longer in the lockdown group (450 minutes vs 238 minutes; P = 0.04). For the overall population, non‐significant increases in symptom onset‐to‐FMC (181 minutes vs 263 minutes; P = 0.09), FMC‐to‐PPCI (119 minutes vs 125 minutes; P = 0.14), and symptom onset‐to‐PPCI delays (294 minutes vs 337 minutes; P = 0.16) were observed in the lockdown group. The median duration of hospitalization was similar in both groups: 5 days (range 3–7) versus 4 days (range 3–6), P = 0.30. Rates of in‐hospital composite outcomes were higher in the lockdown group (7.7% vs 12.3% v; P = 0.06) and mortality almost doubled (4.9% vs 8.2%; P = 0.10) (Table 3) but the differences for these comparisons were not statistically significant.
TABLE 2.
Incidence and pathway delays of STEMI patients undergoing PPCI according to lockdown period, from January 15, 2019 to April 14, 2020
| Overall population (N = 2064) | Prelockdown group (N = 1942) | Lockdown group (N = 122) | |||||
|---|---|---|---|---|---|---|---|
| N | Median or Mean | N | Median or Mean | N | Median or Mean | P value | |
| Number of PPCI/month, mean | 2064 | 138 [131;146] | 1942 | 139 | 122 | 122 | 0.04 |
| Patient delay, median | |||||||
| Symptom onset to FMC (min) | |||||||
| Overall population | 2059 | 186 [51;100] | 1937 | 181 [51;100] | 122 | 263 [57;121] | 0.09 |
| According to FMC | |||||||
| EMS | 1343 | 155 [50;164] | 1268 | 154 [50;164] | 75 | 175 [51–176] | 0.65 |
| ED | 532 | 251[77;328] | 501 | 238 [77;305] | 31 | 450 [95;761] | 0.04 |
| Others | 181 | 226 [15;281] | 165 | 218 [12;280] | 16 | 310 [72;329] | 0.23 |
| System delay, median | |||||||
| FMC to PPCI (min) | 2061 | 119 [69;137] | 1939 | 119 [69;136] | 122 | 125 [72;144] | 0.14 |
| Symptom onset to PPCI (min), median | 2040 | 296 [146;340] | 1923 | 294 [145;340] | 117 | 337 [160;360] | 0.16 |
EMS, emergency medical system; ED, emergency department; FMC, first medical contact; min, minutes; N, number; PPCI, primary percutaneous coronary intervention; STEMI, ST‐elevation myocardial infarction.
TABLE 3.
In‐hospital outcomes of STEMI patients undergoing PPCI according to lockdown period, from January 15, 2019 to April 14, 2020
| Overall population (N = 2064) | Prelockdown group (N = 1942) | Lockdown group (N = 122) | |||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | P value | |
| Outcomes | |||||||
| Composite outcomes | 164 | 7.9 | 149 | 7.7 | 15 | 12.3 | 0.06 |
| Death | 105 | 5.1 | 95 | 4.9 | 10 | 8.2 | 0.10 |
| Definite stent thrombosis (ARC) | 5 | 0.2 | 5 | 0.3 | 0 | 0 | 0.58 |
| Urgent revascularization | 20 | 1 | 18 | 0.9 | 2 | 1.8 | 0.37 |
| Recurrent MI | 21 | 1 | 20 | 1 | 1 | 0.9 | 0.88 |
| Stroke | 10 | 0.5 | 9 | 0.5 | 1 | 0.9 | 0.56 |
| Severe bleeding ≥BARC 3) | 41 | 2 | 38 | 2 | 3 | 2.6 | 0.60 |
ARC, Academic Research Consortium; BARC, Bleeding Academic Research Consortium; MI, myocardial infarction; PPCI, primary percutaneous coronary intervention; STEMI, ST‐elevation myocardial infarction.
3.1. Limitations
The main limitation of this study is the modest sample size and duration of follow‐up in the postlockdown data that reduced the statistical power of the analysis. Several differences did not reach statistical significance. The location of centers in French regions less affected by the outbreak may have minimized the impact of lockdown on STEMI care. A longer study period may confirm the trends. Exclusion of fibrinolysis patients from the analysis may limit the overview of revascularization modalities during the COVID‐19 period. However, the rate of fibrinolysis in our practice was very low (5.1% before lockdown and 2.4% during lockdown) and not likely to influence the results of the study. There is a possibility for bias if French patients became averse to seeking care prior to lockdown, as news spread about the pandemic. However, we did not find a decline in STEMI in the months prior to lockdown, which indicates that this did not happen. A final limitation is that only STEMI patients undergoing PPCI are included in the France PCI registry. Therefore, conservatively treated patients were not analyzed. However, patients who were suspected or positive for COVID‐19 also received unrestricted PPCI.
4. DISCUSSION
This is to the best of our knowledge the largest multicenter study to date to report data on pathway delays and in‐hospital outcomes for STEMI patients during the COVID‐19 outbreak. In addition to a significant 12% drop in the number of STEMI patients treated by PPCI in France, the “symptom onset‐FMC” delay in patients who presented directly to the ED almost doubled after the national lockdown.
Reductions in STEMI admissions as a result of the COVID‐19 pandemic have been reported from Austria (25.5%), Italy (26.5%), Spain (40%), and the United States (48%). 9 , 10 , 11 , 12 The centers in the France PCI registry are located in the western part of France, which was less affected than other parts by the COVID‐19 outbreak, which probably explains the smaller reduction in admissions observed in our data.
The decrease in admissions may be related either to a reduction in the incidence of STEMI or to fewer cases arriving at the hospital. A reduced incidence in acute coronary syndromes may be owing to reduced air pollution, less work‐related stress, and less physical activity such as sport during the lockdown. The correlation between urban air pollution and myocardial infarction is controversial. 13 , 14 The rural location of the centers participating in this study and the drop in STEMI immediately after the imposition of lockdown do not support an effect from air quality improvement. Stress may increase the risk of myocardial infarction 15 , 16 but the impact of lockdown on mental or physical stress has been difficult to assess. 17 In a recent French study, the population stress index doubled during the COVID‐19 lockdown, 18 which indicates that overall stress cannot explain the reduction in STEMIs. Reduced physical activity during lockdown might have contributed to a decrease in the incidence of STEMI, but the size of the reduced incidence and the steep fall in cases very soon after lockdown make such an explanation unlikely.
Another potential explanation for our observations is under‐detection of STEMIs in the community during lockdown. Patients may have feared infection at hospitals, postponing STEMI admissions. The trend toward increased symptom onset‐FMC time observed in our study supports a change in patient behavior during the lockdown period. A reluctance of patients to present to hospital has been described for other medical emergencies such as stroke or transient ischemic attack. 19 The tendency toward more presentations with greater hemodynamic instability in the lockdown group in our study may indicate that lower‐risk or mildly symptomatic patients represent the greatest part of the “missing” STEMIs.
We observed the greatest “symptom onset‐FMC" delay in patients presenting directly to emergency departments, which doubled during the lockdown period. A recent Asian small study 20 warned about a significant increase in out‐of‐hospital and door‐to‐device delays for acute STEMI patients during the COVID‐19 period. EMS are generally well equipped to minimize delays in transferring STEMI patients to the cath lab, 3 but during an epidemic, these systems can be overwhelmed. For STEMI patients this would impose a double penalty: patients react later and the transfer time within the EMS is extended. Bespoke pathways in EDs for patients suspected of infection and for other emergencies may improve workflows during an epidemic.
Delayed reperfusion is a powerful predictor of adverse outcomes in STEMI patients. 21 , 22 A recent publication reported mortality rate of 73% in STEMI patients with COVID‐19 in the United States 23 and an Italian survey likewise report significantly higher mortality in patients admitted for myocardial infarction during the COVID‐19 outbreak compared with the same period in 2019. 10 In our cohort, the doubling of mortality in the lockdown group was not statistically significant, but this was possibly because of a modest sample size.
In conclusion, these data from the large multicenter France PCI registry show that the COVID‐19 outbreak in France was associated with a significant decline in STEMI undergoing PPCI and longer transfer times for patients who presented directly to the ED. Mortality doubled but the difference was not statistically significant. With an ongoing second wave of COVID‐19 infections, the reasons for this adverse situation need to be clearer identified in order to target appropriate actions to reduce inefficiencies in care delivery, as well as promote changes in patient awareness and behavior.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
AUTHOR CONTRIBUTIONS
GR, PM, RK, and GM obtained research funding.GR, RH, and PM conceived and designed the study. GR, RH, and PM drafted the manuscript and all authors contributed substantially to its revision. All authors were involved in the execution of the study. GR takes responsibility for the paper as a whole.
Biography
Grégoire Rangé, MD is a cardiologist at Hôpitaux de Chartres, Chartres, France.

Rangé G, Hakim R, Beygui F, et al. Incidence, delays, and outcomes of STEMI during COVID‐19 outbreak: Analysis from the France PCI registry. JACEP Open. 2020;1:1168–1176. 10.1002/emp2.12325
Funding and support: This work was supported by the regional health agency of Normandy, Centre Val de Loire (2015/OSMS/OS/15), and Ministry of Health. The sponsors were not involved in the design, study progression, collection, management, data analyses, or interpretations of the results and had no role in the preparation, review, or approval of the manuscript.
Supervising Editor: Henry E. Wang, MD, MS.
REFERENCES
- 1. Cannon CP, Gibson CM, Lambrew CT, et al. Relationship of symptom‐onset‐to‐balloon time and door‐to‐balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA 2000;283:2941‐2947. [DOI] [PubMed] [Google Scholar]
- 2. Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomized trials. Lancet 2003;361:13–20. [DOI] [PubMed] [Google Scholar]
- 3. Huber K, Gersh BI, Goldstein P, Granger CB, Armstrong PW. The organization, function, and outcomes of ST‐elevation myocardial infarction networks worldwide: current state, unmet needs and future directions. Eur Heart J 2014;35:1526‐1532. [DOI] [PubMed] [Google Scholar]
- 4. Szerlip M, Anwaruddin S, Aronow HD, et al. Considerations for cardiac catheterization laboratory procedures during the COVID‐19 pandemic. Perspectives from the Society for Cardiovascular Angiography and Interventions Emerging Leader Mentorship (SCAI ELM) Members and Graduates. Catheter Cardiovasc Interv 2020;96(3):586‐597.. [DOI] [PubMed] [Google Scholar]
- 5. Chieffo A, Stefanini GG, Price S, et al. EAPCI position statement on invasive management of acute coronary syndromes during the COVID‐19 pandemic. Eurointervention 2020;16:233‐246. [DOI] [PubMed] [Google Scholar]
- 6. Rangé G, Chassaing S, Marcollet P, et al. The CRAC cohort model: A computerized low cost registry of interventional cardiology with daily update and long‐term follow‐up. Rev Epidemiol Sante Publique 2018;66:209‐216. [DOI] [PubMed] [Google Scholar]
- 7. Andreini D, Arbelo E, Barbato E, et al. ESC guidance for the diagnosis and management of CV disease during the COVID‐19 pandemic. Available at https://www.escardio.org/Education/COVID-19-and-Cardiology/ESC-COVID-19-Guidance. Accessed April 22, 2020.
- 8. Ibanez B, James S, Agewall S,et al; ESC Scientific Document Group . 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST‐segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST‐segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2018;39:119‐177. [DOI] [PubMed] [Google Scholar]
- 9. Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJ. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID‐19: the pandemic response causes cardiac collateral damage. Eur Heart J 2020;41(19):1852‐1853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. De Rosa S, Spaccarotella C, Basso C, et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID‐19 era. Eur Heart J 2020;41(22):2083‐2088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rodríguez‐Leor O, Cid‐Álvarez B, Ojeda S, et al. Impact of the COVID‐19 pandemic on interventional cardiology activity in Spain. REC Interv Cardiol 2020;2:82‐89. [Google Scholar]
- 12. Solomon MD, McNulty EJ, Rana JS, et al. The Covid‐19 pandemic and the incidence of acute myocardial infarction. N Engl J Med 2020;383(7):691‐693. [DOI] [PubMed] [Google Scholar]
- 13. Caussin C, Escolano S, Mustafic H, et al. Short‐term exposure to environmental parameters and onset of ST‐elevation myocardial infarction. The CARDIO‐ARSIF registry. Int J Cardiol 2015;183:17‐23. [DOI] [PubMed] [Google Scholar]
- 14. Mustafic H, Jabre P, Caussin C, et al. Main air pollutants and myocardial infarction: a systematic review and meta‐analysis. JAMA 2012;307:713‐721. [DOI] [PubMed] [Google Scholar]
- 15. Gabbay FH, Krantz DS, Kop WJ, et al. Triggers of myocardial ischemia during daily life in patients with coronary artery disease: physical and mental activities, anger and smoking. J Am Coll Cardiol 1996;27:585–592. [DOI] [PubMed] [Google Scholar]
- 16. Manoj MT, Joseph KA, Vijayaraghavan G. Association of depression, anxiety, and stress with myocardial infarction: A case‐control study. J Clin Prev Cardiol 2018;7:86‐92. [Google Scholar]
- 17. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 2020; 395: 912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chan‐Chee C, Leon C, Lasbeur L, et al. The mental health of the French facing the COVID‐19 crisis: prevalence, evolution and determinants of anxiety disorders during the first two weeks of lockdown (COVIPREV study, 23–25 March and 30 March‐1 April, 2020. Bull Epidemiol Hebd 2020;13:260‐269. [Google Scholar]
- 19. Kansagara AP, Goyal MS, Hamilton S, Albers GW. Collateral effect of COVID‐19 on stroke evaluation in the United States. N Engl J Med 2020;383(4):400‐401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tam CCF, Cheung KS, Lam S, et al. Impact of coronavirus disease 2019 (COVID‐19) outbreak on ST‐segment elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes 2020;13:e006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Guerchicoff A, Brener SJ, Maehara A, et al. Impact of delay to reperfusion on reperfusion success, infarct size, and clinical outcomes in patients with ST‐segment elevation myocardial infarction. The INFUSE‐AMI Trial (INFUSE‐Anterior Myocardial Infarction). J Am Coll Cardiol Interv 2014;7:733‐740. [DOI] [PubMed] [Google Scholar]
- 22. De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation 2004;109:1223‐1225. [DOI] [PubMed] [Google Scholar]
- 23. Bangalore S, Sharma A, Slotwiner A. ST‐Segment Elevation in patients with COVID.19 – A case series. N Engl J Med 2020;382(25):2478‐2480. [DOI] [PMC free article] [PubMed] [Google Scholar]


