Abstract
In order to reduce the high infection rate of COVID‐19, individuals began to engage in self‐isolation amid a time of uncertainty and worry. Given that social support can be protective against the negative effects of distress on mental and physical health, the lack of support may negatively impact individuals during their self‐isolation. Thus, the current study examined the role of self‐isolation on feelings of stress, the perception and reception of social support, and mental health problems during the COVID‐19 pandemic. A sample of 405 college students were asked to report on the amount of self‐isolation in which they were engaging, worry about COVID‐19, psychological health, and received and perceived social support. Results indicated that when the length of time in self‐isolation was taken into account, perceived social support buffered the connection between worry about COVID‐19 and psychological health. These results indicate that social support, worry about COVID‐19, and self‐isolation may influence individuals’ psychological health during times of stress.
Keywords: Social Support, COVID‐19, Stress‐Buffering, Worry, Isolation
Resumen
Con el fin de disminuir el alto índice de contagio de la COVID‐19, las personas comenzaron a autoaislarse en medio de un momento de incertidumbre y preocupación. Teniendo en cuenta que el apoyo social puede ser protector contra los efectos negativos del distrés en la salud mental y física, la falta de apoyo puede afectar negativamente a las personas durante su autoaislamiento. Por lo tanto, el presente estudio analizó el papel que desempeña el autoaislamiento en los sentimientos de estrés, la percepción y la recepción de apoyo social y los problemas de salud mental durante la pandemia de la COVID‐19. Se solicitó a una muestra de 405 estudiantes universitarios que informen sobre la cantidad de autoaislamiento que estaban haciendo, las preocupaciones acerca de la COVID‐19, la salud psicológica y el apoyo social recibido y percibido. Los resultados indicaron que cuando se tuvo en cuenta el periodo de tiempo en autoaislamiento, el apoyo social percibido amortiguó la conexión entre la preocupación acerca de la COVID‐19 y la salud psicológica. Estos resultados indican que el apoyo social, la preocupación acerca de la COVID‐19 y el autoaislamiento pueden influir en la salud psicológica de las personas durante momentos de estrés.
摘要
为了降低COVID‐19的高感染率,在不确定的情况下以及充满忧虑的时期,个体开始实行自我隔离。鉴于社会支持可以保护人们免受低落情绪对身心健康的负面影响,缺乏支持可能对个体在自我隔离期间产生负面影响。因此,本研究考察了在COVID‐19大流行期间,自我隔离对压力感、社会支持的感知和接受以及心理健康问题等方面产生的作用。受试样本包括405名大学生,他们被要求报告他们的自我孤立程度、对COVID‐19的担忧程度、心理健康程度、获得的社会支持和感知到的社会支持程度。这些结果表明,在考虑自我隔离时间长度的情况下,社会支持感缓冲了对COVID‐19的忧虑与心理健康这两者之间的联系。本文研究结果表示社会支持、对COVID‐19的忧虑和自我隔离都可能会影响个体在压力时期的心理健康。
On March 11th, the World Health Organization declared the novel coronavirus (COVID‐19) outbreak a pandemic (World Health Organization, 2020). As part of the effort to stem the projected exponential daily increase of infections and “flatten the curve” (i.e., decrease the number of severe cases to a manageable number; Matrajt & Leung, 2020), schools, colleges, and universities closed their doors and sent students home, and numerous states in the United States of America (USA) asked individuals to stay at home, work remotely, social distance, and avoid leaving home unless necessary (CDC, 2019). Additionally, social gatherings were limited to less than 10 people (or fewer in some states and cities as determined by local government officials) and many students turned to virtual meetings, classes, and social media to meet their social needs. As individuals practice social distancing and self‐isolation in an effort to help limit the spread of COVID‐19, they leave the social atmosphere commonly associated with attending university/college/work and may experience higher rates of loneliness, feelings of isolation, and poor psychological health.
Social support has been shown to be a protective factor between the negative effects of distress on mental and physical health (e.g., Cohen & Wills, 1985; Szkody & McKinney, 2019). The COVID‐19 pandemic has been associated with increased in fear and worry (Mertens, Gerritsen, Dujindam, Salemink, & Engelhard, 2020). Although high rates of social support may be protective for mental health problems during a highly stressful life event, such as during the COVID‐19 pandemic, a lack of social support during the pandemic may increase the risk for mental health problems. Research during past pandemics (e.g., HIV/AIDS, H1N1 influenza, SARS, and Ebola) has found that social support was associated with lower rates of mental health problems (e.g., Asante, 2012; Chew et al., 2020). However, with the COVID‐19 pandemic, social distancing and self‐isolation may limit the availability and reception of social support as social boundaries are extended. Thus, the practices designed to “flatten the curve” may result in limiting the spread of the virus, but it may also have negative psychological consequences. The current study examined the roles of social distancing and self‐isolation on feelings of stress or worry about the pandemic, the perception and reception of social support, and mental health problems during the COVID‐19 pandemic.
Negative Effects of Loneliness and Stress‐Buffering Hypothesis
According to the Belonging Hypothesis (Baumeister, 2011) and the Evolutionary Theory of Loneliness (Cacioppo, et al., 2006), humans are social creatures that naturally bond with others to help protect them from environmental factors. In the past, humans relied on each other to help collect food and fight against predators. Individuals who lack social interaction or support may withdraw further and become more vigilant to threats (Cacioppo et al., 2006). Moreover, loneliness, or the perception of isolation or being cut off from others (“Loneliness”, n.d.), has been found to increase the negative appraisal of threats (i.e., individuals may see threats as more dangerous than they would otherwise; Hawkley, Burleson, Bernston, & Cacipppo, 2003; Qualter et al., 2013), which may result in individuals suffering from increased overall stress. College students may experience loneliness, or feeling cut off from others, as they are no longer on college campuses and away from populations of other students or friends. Furthermore, students may also feel cut off from others, as they no longer are able to physically connect with friends as they would have if not socially distancing or self‐isolating. College campuses provide many social interactions for their students such as sports events, in‐person classes, conferences, and more that may no longer be available when students self‐isolate and campuses close resulting in loneliness. Even for those living with roommates or family, feeling cut off from other previously available resources may result in loneliness.
Indeed, loneliness and worry may explain why many major health organizations (e.g., Brooks et al., 2020; Center for Disease Control, 2019) have suggested that individuals continue to connect with others during the COVID‐19 pandemic. Past research has shown an increase in depression, anxiety, suicidality, and more as a result of major natural disasters (Norris, Watson, Hamblen, & Pfefferbaum, 2005). Thus, it stands to reason that the college students in the United States may also experience a similar spike in negative mental and physical health outcomes as a result of the COVID‐19 pandemic. Specifically, COVID‐19‐related worry has been associated with clinical levels of depression, anxiety, and post‐traumatic stress disorder in emerging adult students (Liu, Zhang, Wong, & Hyun, 2020). COVID‐19 has also been associated with disordered eating behaviors as individuals are cut off from support systems and face continued exposure to COVID‐19‐related media and other stressors (Rodgers et al., 2020). The Stress‐Buffering Hypothesis posits that social support plays a protective role against the negative effects of stress (e.g., worry) from negative life events on mental and physical health (Cassel, 1976). Specifically, the more social support or resources that a person has, or perceives to have available, may help the individual to feel more in control of the stressful situation or may lead to more emotional disclosure and processing of the negative event, which then improves associated outcomes (e.g., lower rates of depression or anxiety, better access to health care, etc.). Perceived support in particular has been theorized to help individuals reappraise stressful events (Cohen, Gottlieb, & Underwood, 2000), whereas received support has been theorized to intervene on the impacts of stress by assisting with coping (Bianco & Eklund, 2001; Lakey & Cohen, 2000).
It is important to take this theory into account during the COVID‐19 pandemic, as individuals engaging in efforts to “flatten the curve” through social distancing and self‐isolation may not perceive or have access to social support systems while physically away from their social networks. In response, many institutions in the United States (and across the world) have activated online counseling and telehealth, developed and promoted social media platforms for social connection, and have moved all education online (e.g., Xiao, Zhang, Kong, Li, & Yang, 2020). However, to date, studies examining the perceived availability or reception of social support have mainly been conducted in Eastern and European countries as these were the first impacted by the virus several months before the virus spread to the United States (e.g., Xiao et al., 2020).
Several studies worldwide have examined the impact of loneliness, social support, stress, and mental health problems on non‐US populations. Cao et al. (2020) found that among Chinese college students, living at home with a parent, having a stable family income, and perceiving more social support were associated with lower rates of anxiety and stress associated with COVID‐19. Similarly, a study among college students in Poland found that loneliness significantly increased financial worry and isolation worry (Okruszek, Aniszewska‐Stańczuk, Piejka, Wiśniewska, & Żurek, 2020). Moreover, college students are not the only ones at risk. In a nationwide study in the United States, stay at home orders were positively associated with health anxiety, financial worry, and depression for individuals age 20 to 74 (Tull, Edmonds, Scamaldo, Richmond, Rose, & Gratz, 2020). Additionally, studies have found that higher levels of support are protective against social distancing and self‐isolation and worry during the COVID‐19 pandemic among adults age 20 and older (Banerjee, Burkholder, Sana, & Szirony, 2020; Nelson, Pettitt, Flannery, & Allen, 2020).
Current Study
Given the importance of examining current risk factors for mental health problems among college students in the United States during the COVID‐19 pandemic, the current study examined the roles of social distancing and self‐isolation on social support, worry about the pandemic (i.e., stress), and mental health problems. Additionally, the study utilized the model proposed by the Stress‐Buffering Hypothesis to examine the protective, or deleterious when absent, effects of social support on college student mental health during the pandemic. Furthermore, as perceived and received support have been shown to differentially buffer against stress on mental or physical health concerns through different theorized mechanisms, a model was examined to test the buffering role of both perceived social support and received social support.
Hypothesis 1 stated that days social distancing and in self‐isolation would be positively associated with worry about COVID‐19 and negatively associated with both perceived and received social support for college students and that worry about COVID‐19 would be negatively related to psychological health. Hypothesis 2 stated that, consistent with the Stress‐Buffering Hypothesis, social support would act as a buffer between stress about COVID‐19 and mental health problems (i.e., higher levels of social support would weaken the relationship between stress about COVID‐19 and mental health problems). Lastly, Hypothesis 3 stated that higher days in self‐isolation would reduce the buffering effect of social support.
Method
Procedure
Following Institutional Review Board approval, college attending students were recruited via an online research portal at a large Southern university in the United States. Additionally, participants were recruited online through a snowball sampling method using social media (i.e., a link to the survey was shared online which was then shared to other interested parties). Individuals completed informed consent and survey measures online and students received research credit for psychology classes for completion of the study. All participants were treated in accordance with the APA Code of Ethics.
Participants
Raw data consisted of 423 (M age = 19.77, SD = 2.18; minimum = 18, maximum = 45) individuals who completed the survey; data from 79 individuals were removed due to less than 10% of the survey being completed by these participants. The majority of the sample reported currently staying with their parents (60.8%) or in their own personal home/apartment (29.0%). Consistent with that report, most participants reported that they were staying with at least one other person in their home (95.3%). Thus, the majority of participants (78.5%) reported currently living with a family member, 13.6% reported staying with a friend or roommate, 1% reported staying with their child, 3.2% reported staying with “other,” and 4.7% reported living alone. Additional descriptives of the sample are shown in Table 1. Of the students who completed the survey, 407 received research credit for their psychology class and 16 individuals received no incentive to complete the survey.
Table 1.
Descriptives of the Sample
| Variable | n | % |
|---|---|---|
| Sex at Birth | ||
| Male | 147 | 34.8 |
| Female | 275 | 65.0 |
| Non‐Hispanic Ethnicity | ||
| White | 197 | 46.3 |
| Black or African American | 47 | 11.1 |
| Asian or Asian American | 6 | 1.4 |
| American Indian or Alaska Native | 1 | 0.2 |
| Native Hawaiian or Pacific Islander | 1 | 0.2 |
| Another ethnicity | 1 | 0.2 |
| Hispanic Ethnicity | ||
| White | 122 | 28.8 |
| Black or African American | 23 | 5.4 |
| Asian or Asian American | 2 | 0.5 |
| Another ethnicity | 2 | 0.5 |
| Multiethnic | 22 | 5.2 |
| Education Level | ||
| Did not complete high school | 1 | 0.2 |
| High school degree or GED | 351 | 83.0 |
| Earned a two‐year degree | 36 | 8.5 |
| Earned a four‐year degree | 29 | 6.9 |
| Earned a graduate degree | 6 | 1.4 |
| Household Income | ||
| $0–$34,000 | 53 | 12.5 |
| $35,000–$49,000 | 33 | 7.8 |
| $50,000–$79,999 | 69 | 16.3 |
| $80,000–$99,999 | 42 | 9.9 |
| $100,000 + | 143 | 33.8 |
| Prefer not to answer | 83 | 19.6 |
| Have you social distanced or self‐isolated? | ||
| Yes | 301 | 71.2 |
| No | 122 | 28.8 |
| Reasons for Not Social Distancing or Self‐Isolating | ||
| Work | 113 | 28.5 |
| Care‐taking | 76 | 19.2 |
| Travel | 81 | 20.4 |
| To have fun (e.g., attend parties) | 83 | 20.5 |
| Medical reasons | 26 | 6.6 |
| I don’t think the disease is real | 10 | 2.5 |
| I don’t think the disease is serious | 44 | 11.1 |
| I don’t think I will get the disease | 57 | 14.5 |
| Other | 47 | 17.3 |
Measures
Stress and Self‐Isolation during COVID‐19
Participants were asked to indicate if they were engaging in self‐isolation since March 9th, 2020. Individuals who reported social distancing and/or being in self‐isolation were then asked to indicate when they began social distancing/isolation. Time spent social distancing or in self‐isolation was calculated by determining the amount of days between the time/date indicated and the date they completed the questionnaire to assess for the amount of time practicing these behaviors and examine the association of time isolating on psychological health. Days self‐isolating or social distancing were treated as a continuous variable in the current study. Furthermore, individuals were asked to rate their level of worry about COVID‐19 on a scale from 1 (not at all worried) to 5 (extremely worried). Worry about the pandemic was utilized in the current study as the stressor in the stress‐buffering model examined (i.e., “How worried are you about the Coronavirus?”). Individuals who did not socially distance or self‐ isolate were scored as 0 days in self‐isolation.
Multidimensional Survey of Perceived Social Support (MSPSS)
The MSPSS (Zimet, Dahlem, Zimet, & Farley, 1988) consists of 12 items that measure their perceived availability of support since March 9th (the beginning of the COVID‐19 pandemic in the United States) from friends, family, and someone who is close to the participant (e.g., aunt, uncle, significant other, grandparent, etc.). Items were scored on a 7‐point scale from 1 (very strongly disagree) to 7 (strongly agree). Subscales included friends (e.g., I can count on my friends when things go wrong), mother, and father (e.g., My mother/father really tries to help me). Subscales were totaled and averaged for a total support score (i.e., the ratings of each item were summed to create a total score; Zimet et al, 1988). Internal consistency and construct validity have been demonstrated in previous studies (Zimet et al., 1988), and Cronbach’s alpha was .94 in the current study. The total support score was utilized in the current study to determine participants’ perceived social support during the pandemic.
Inventory of Socially Supportive Behaviors (ISSB)
The ISSB (Barrera, Sandler, & Ramsay, 1981) is a 40‐item inventory that scores how often a particular type of social support was received since March 9th (the beginning of the COVID‐19 pandemic in the United States) including guidance (e.g., Helped you understand why you didn't do something well), emotional support (e.g., Listened to you talk about your private feelings), and tangible support (e.g., Gave you under $25). Participants were asked to respond to the measures differentiated by source of offered support (i.e., mother, father, friend, and someone who is close to the participant [e.g., aunt, uncle, significant other, grandparent, etc.]). Items were scored on a scale from 1 (not at all) to 5 (about every day). Ratings for each item were summed to create a total score for received social support. Internal consistency and good construct validity have been demonstrated in previous studies (Barrera et al., 1981) and Cronbach’s alpha was .97 in the current study. The current study utilized this measure to determine the amount of total received social support as reported by the participant during the pandemic.
WHO Quality of Life Instrument—Short Form (WHOQOL‐BREF)
The WHOQOL‐BREF (WHOQOL Group, 1998) is a 26‐item measure of quality of life across four domains since March 9th (the beginning of the COVID‐19 pandemic in the United States): physical, psychological, social relationships, and environment. Items were scored on a Likert scale from 1 to 5. To score, each subscale is summed, and scores are transformed by multiplying the sum of the subscale by 4, so that the scores are comparable to the full WHOQOL version of the measure. The psychological health scale (e.g., How much do you enjoy life?, How well are you able to concentrate?, How often do you have negative feelings such as blue mood, despair, anxiety, depression?) was utilized in the current study to examine mental health during the pandemic. The Cronbach alpha for the current study was .81.
Data Analysis
Correlations were performed using AMOS 26.0 across all variables to test Hypothesis 1. A single‐path analysis was performed using AMOS 26.0 across all variables to test their direct effects and their interaction effects. Age, ethnicity, biological sex, and amount of days from the date the survey was completed were used as control variables within the model. Specifically, Hypothesis 2 was tested using worry about COVID‐19 × perceived social support and worry about COVID‐19 × received social support interactions to predict psychological health. Hypothesis 3 was tested by adding days in self‐isolation as an additional moderator to predict psychological health (i.e., worry about COVID‐19 × perceived social support × days in self‐isolation and worry about COVID‐19 × received social support × days in isolation). Significant interactions were interpreted with spotlight analysis at ±1 SD.
Results
Descriptives and properties of all scales and variables are shown in Table 2. The distribution of the days self‐isolating/social distancing variable was examined for skewness given that some individuals reported not engaging in these behaviors. A visual examination of the distribution demonstrated no bimodal distribution but a moderate skewness (skewness = .857) well within acceptable limits (Field, 2009). Group differences between individuals who self‐isolated for at least one day versus individuals who did not self‐isolated or social distance were examined using independent t tests as shown in Table 3. Those who self‐isolated/social distanced for at least one day reported significantly more worry, less received support, and worse psychological health in comparison to those who did not self‐isolate or social distance. Correlations between all variables are shown in Table 4. Hypothesis 1 was partially supported by correlations as days in self‐isolation were positively correlated to worry about COVID‐19, and worry about COVID‐19 was negatively associated with psychological health. Contrary to Hypothesis 1, days in isolation were not correlated with perceived social support and were positively correlated with received social support. Direct and interaction effects are shown in Table 5. Direct effects demonstrated that worry about COVID‐19 was associated negatively with psychological health, whereas perceived and received social support were associated positively with psychological health.
Table 2.
Descriptives and Properties of Variables
| M (n) | SD (%) | Range | Cronbach’s α | |
|---|---|---|---|---|
| Worry about COVID‐19 | 2.78 | 0.94 | 1–5 | N/A |
| Not at all worried | (35) | (8.3) | ||
| A little worried | (120) | (28.5) | ||
| Moderately worried | (186) | (44.2) | ||
| Very Worried | (63) | (15.0) | ||
| Extremely Worried | (17) | (4.0) | ||
| Days Social Distancing or in Self‐Isolation | 17.59 | 13.93 | 0–91 | N/A |
| Avoided going to large gatherings of people for fun (e.g., bars, events, movies) | (347) | (85.9) | ||
| Avoided going to large gatherings of people for religious reasons (e.g., church) | (331) | (81.9) | ||
| Avoided flying on a plane | (254) | (62.9) | ||
| Self‐isolated at home | (328) | (81.0) | ||
| Avoided going to appointments unless absolutely necessary | (276) | (68.1) | ||
| Stayed at least 6 feet away from people | (318) | (78.5) | ||
| Avoided public places with small gatherings of people (e.g., coffee shops) | ||||
| Gone to get takeout instead of dining in restaurants | (297) | (73.3) | ||
| Gone grocery shopping during off times/hours | (316) | (78.0) | ||
| Perceived Social Support | 91.05 | 18.83 | 16–112 | .94 |
| Received Social Support | 99.50 | 34.99 | 40–200 | .97 |
| Psychological Health | 14.11 | 3.14 | 4–20 | .81 |
Table 3.
Descriptives and Properties of Variables
| Self‐Isolated/Social Distanced (n = 281) | Did Not Self‐Isolate/Social Distance (n = 126) | t | p | Cohen’s d | |
|---|---|---|---|---|---|
| M (SD) | M (SD) | ||||
| Worry about COVID‐19 | 2.82 (.94) | 2.58 (.86) | 2.487 | .01 | .27 |
| Days Social Distancing/Self‐Isolation | 24.85 (10.49) | 0 (.00) | 29.97 | .00 | 3.20 |
| Perceived Social Support | 91.32 (19.14) | 92.17 (16.80) | −.40 | .69 | .04 |
| Received Social Support | 101.70 (37.10) | 95.05 (29.50) | 1.91 | .05 | .20 |
| Psychological Health | 14.04 (3.16) | 14.43 (3.02) | −1.18 | .24 | .13 |
Table 4.
Correlations
| 1. | 2. | 3. | 4. | 5. | |
|---|---|---|---|---|---|
| 1. Days in Isolation | — | ||||
| 2. Worry about COVID‐19 | .10* | — | |||
| 3. Perceived Social Support | −.02 | .08 | — | ||
| 4. Received Social Support | .11* | .10* | .26* | — | |
| 5. Psychological Health | −.01 | −.15* | .35* | .23* | — |
* indicates p < .05.
Table 5.
Direct Effects on Psychological Health
| Variable | b |
|---|---|
| Worry about COVID‐19 | −.16* |
| Perceived Social Support | .37* |
| Received Social Support | .13* |
| Days in Isolation | .03 |
| Days in Isolation × Worry | .03 |
| Perceived Social Support × Received Social Support | −.11* |
| Worry about COVID‐19 × Perceived Social Support | .02 |
| Days in Isolation × Perceived Social Support | −.15* |
| Worry about COVID‐19 × Received Social Support | .05 |
| Days in Isolation × Received Social Support | .14* |
| Days in Isolation × Worry about COVID‐19 × Perceived Social Support | −.12* |
| Days in Isolation × Worry about COVID‐19 × Received Social Support | −.04 |
* indicates p < .05.
Hypothesis 2, which stated that social support (i.e., perceived and received) would buffer the effect between worry about COVID‐19 and psychological health, was not supported as neither interaction term (i.e., worry about COVID‐19 × perceived social support and worry about COVID‐19 × received social support) were significant. Thus, neither received nor perceived social support successfully buffered against the negative effects of worry about COVID‐19 on psychological health, without taking days self‐isolating/social distancing into account.
However, when days in self‐isolation were added as an additional moderator (i.e., Hypothesis 3 which stated that days in isolation would reduce the buffering effect), a significant 3‐way interaction was found for days in self‐isolation × worry about COVID‐19 × perceived social support only. See Figure 1 for a visual interpretation of the significant 3‐way interaction.
Figure 1.
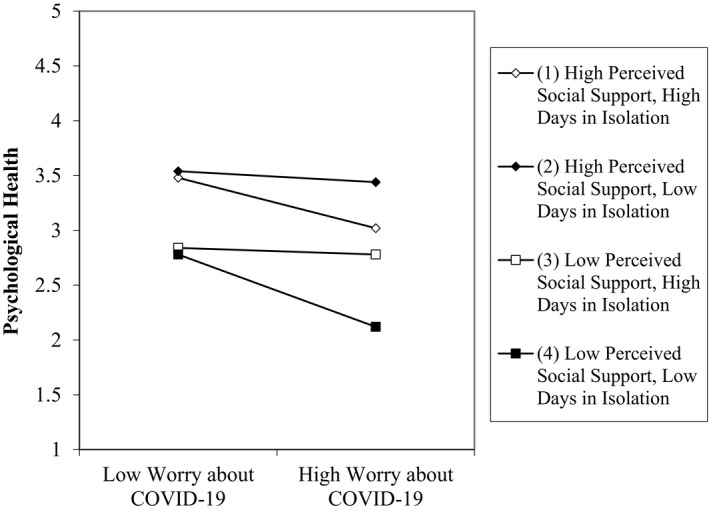
Days in isolation × worry about COVID‐19 × perceived social support interaction.
Demonstrating a clear and consistent main effect, higher levels of perceived social support were always associated with higher psychological health in comparison to individuals who reported lower levels of perceived social support across levels of other variables. The combination of low perceived social support and less time in self‐isolation/social distancing had the most deleterious effects on psychological health. Spending more time self‐isolating/social distancing, when combined with low perceived social support, was associated with slightly better psychological health, indicating that time self‐isolation/social distancing may be protective when social support resources may not be available. However, high perceived support was protective regardless of the time in isolation. The best outcomes on psychological health occurred when time self‐isolating/social distancing was low and perceived support was high, suggesting that individual psychological health was best when individuals both perceived support/resources and were not encumbered by the barriers of self‐isolation/social distancing. Within the 3‐way interaction, an examination of the slope differences of each moderator combination demonstrated significantly different impacts on psychological health (all p < .001) except between the interaction between high perceived social support and high days in self‐isolation vs. low perceived social support and low days in self‐isolation.
Although not hypothesized, the interaction between days in self‐isolation/social distancing and received social support was significant. Specifically, days in self‐isolation/social distancing was associated with decreased psychological health when in combination with less received support suggesting that individuals who were engaging in these behaviors may have had poor psychological outcomes when received support was low.
Discussion
The current study examined the role of self‐isolation on feelings of worry, social support, and psychological health during the COVID‐19 pandemic. As expected, results indicated that individuals who were worried about COVID‐19 reported worse psychological health. Excessive worry is one of the symptoms of anxiety disorders and is often associated with depressive symptoms (Booth & Tekes, 2019). Worrying also reduces mental resources, which makes it hard to retain a positive mindset and can result in negative world view (Stefanopoulou, Hirsch, Hayes, Adlam & Coker, 2014). Similarly, increased social support (either perceived or received), was associated with higher scores of psychological health. This result is supported by previous research, which has suggested that social support can insulate individuals from psychological problems (Szkody & McKinney, 2019).
Contrary to the Stress‐Buffering Hypothesis, social support did not buffer the relationship between worry about COVID‐19 and psychological health (i.e., 2‐way interactions not significant; Cassel, 1976). These results may have occurred because many of the individuals in the study were self‐isolating or social distancing when possible. Although they may have reported receiving and perceiving social support, days in self‐isolation may have altered the impact of that support, or days in self‐isolation may have impacted their reported worry about the pandemic. Indeed, perceived social support served as a buffer between worry about COVID‐19 and psychological health only when days in self‐isolation were lower and worry about COVID‐19 was higher (i.e., the significant 3‐way interaction).
These results are not surprising given that loneliness has been associated with increased worry amid the COVID‐19 pandemic (e.g., Okruszek et al., 2020). Research has also indicated that loneliness often leads to negative psychological health, such as depression, anxiety, and overall worse well‐being (Jaya, Hillmann, Reininger, Gollwitzer, & Lincoln, 2017; Satici, 2019). In the current sample, people with higher perceived social support appeared to be harmed by more days in self‐isolation, but those with lower perceived social support appeared to be benefited, although this inference is speculative given the cross‐sectional nature of the data and potential for confounds. Nonetheless, these results may indicate that the limited availability of normally high perceived support while self‐isolating may be detrimental on psychological health. These individuals with higher perceived social support may feel lonelier during periods of self‐isolation because they miss, and are unable to access, that support system which they perceive they have. Individuals who are unable to (e.g., due to work), or choose not to self‐isolate, may still feel they have a high level of support to fall back on if they experience hardships. These individuals also are potentially experiencing the least amount of life changes since they are not self‐isolating. However, neither of these categories are as negatively impactful as not having a perception of available support.
Conversely, individuals who may not have a higher perception of available social support may use self‐isolation as a way to improve their psychological health on their own, especially when experiencing higher levels of worry about COVID‐19. Additionally, self‐isolation may serve as an avoidance coping mechanism against anxiety‐provoking situations such as being exposed to the virus (e.g., Hofmann & Hay, 2018; Krypotos, Effting, Kindt, & Beckers, 2015). This may be especially true of individuals who may feel they have no one to turn to if they do contract the disease. For example, those who are self‐isolation may not have to view reminders that they have poor social support (e.g., seeing groups of friends at a restaurant), so their depressive symptoms decrease. They also may feel like they are able to regain a sense of control over the situation by self‐isolating, given their lack of social support. On the other hand, individuals who report a lack of support and cannot self‐isolate may feel a loss of control given that they have no one to turn to and are more at risk of catching COVID‐19.
Moreover, these results suggest that the group most at risk for poor psychological health were those experiencing more worry about COVID‐19, had lower perceived social support, but had lower days in self‐isolation. This finding may suggest that these individuals may have increased worry about their lack of self‐isolating behavior, perhaps because they were unable to do so. College students were unable to self‐isolate because their jobs were considered essential, having family members they must care or provide for, or because they did not have the finances to not work, even for a short time. Although most participants reported a household income greater than $50,000, it is plausible that college students want jobs to pay some of their own bills or be otherwise financially independent.
Additionally, it is important to note that for both perceived and received social support, there was a significant interaction between support and days in isolation on psychological health. Specifically, and consistent with previous literature, having higher levels of social support (either perceived or received) was protective against the negative effects of self‐isolation and/or social distancing on psychological health when controlling for worry.
Limitations and Future Directions
Although the current study has many strengths, the limitations must be acknowledged. Given that it was a cross‐sectional design, the current study is unable to determine causation or direction of effects. For example, it may be that individuals with poor mental health before the pandemic may perceive or receive less social support and thus, feel they must isolate or have been isolating more than other populations. Additionally, these individuals may also worry or ruminate about the pandemic more than individuals in good psychological health. Further examination of the longitudinal effects of COVID‐19 is required to fully understand the mechanisms of social support and self‐isolation during the pandemic. In addition, the sample consisted of college students, which limits external validity. Also, more than half (60.8%) of the sample reported they were living with their parents, and the vast majority (96.2%) were living with someone else in the home. Additionally, many individuals reported some reason they were unable to self‐isolate or social distance which may be the result of being an essential worker, having family in the home to care for, or other reasons that were not fully explored in the current study. Thus, the majority of the sample were not entirely self‐isolated, and this may limit the ability of the current study to examine loneliness as a result of self‐isolation (e.g., those following social distancing guidelines may not experience loneliness depending on who they live with). Additionally, the social support measures requested that participants indicate a “special person” who gave them/provided support of some kind. Individuals were not requested to identify the “special person” and thus no distinction could be made between having support from extended kin or a romantic partner within this measure. However, the measure continued to capture the overall view of perceived/received social support.
The current study also did not ask if the days in self‐isolation were consecutive, which may have an influence upon the negative impacts of loneliness. In addition, it is possible that participants already had poor psychological health before COVID‐19, which would limit the ability to determine if self‐isolation and worry about the pandemic had resulted in their poor psychological health. It is also important to note that the study did not examine the specific perception or experience of loneliness while self‐isolating. A fuller measure that encapsulates these experiences may shed light on some of the findings in the study. Lastly, the measure of worry about COVID‐19 consisted of a single item. The item did not ask participants to clarify the source of their worry about the pandemic (e.g., the economy, the future, death/illness, etc.) which may limit interpretations of the findings to generalized worry, versus a more nuanced interpretation of specific COVID‐19‐related worry. Future studies may consider using a fuller measure of worry to assess for reliability and validity. Similarly, the current study asked participants to self‐report social distancing and self‐isolating as of March 9th; future studies may seek to examine how individuals define these behaviors when others are in the home or to examine social distancing and self‐isolating separately.
The current study added to the limited amount of available literature on the impact of COVID‐19 and demonstrated that perceived and received social support, worry about COVID‐19, and self‐isolation may influence individuals’ psychological health. Self‐isolation may be an effective tool to prevent the spread of the COVID‐19 pandemic, but also may negatively impact mental health for certain groups of people. It is important to identify factors, such as the moderators included in the current study, which may help reduce the negative impacts of social isolation, such as virtual social activities. Future studies should also expand the current study to examine how social isolation impacts individuals of different ages and different household sizes. Additionally, as the pandemic has differentially impacted ethnic minority populations (Center for Disease Control, 2020), future research should examine these moderators, and others, among these specific populations. Lastly, the moderator of the source of either perceived or received support may help to illuminate which sources of support suffer the most during socially distancing or self‐isolating. Understanding where support may lag or disappear may help clinicians, parents, and teachers to intervene and fill the support gap for college students during the pandemic.
Conclusion
In conclusion, the results of the current study have several practical implications. For example, the current study suggests that when combined with high levels of social support, isolation may be a protective factor against mental health problems during COVID‐19. Institutions, workplaces, and professors may take this into account and consider providing college students the chance to self‐isolate or socially distance during the pandemic to improve quality of health. Additionally, opportunities to connect with individuals and provide resources may also help to protect college students from poor psychological quality of life.
References
- Asante, K. O. (2012). Social support and the psychological wellbeing of people living with HIV/AIDS in Ghana. African Journal of Psychiatry, 15(5), 340–345. [DOI] [PubMed] [Google Scholar]
- Banerjee, S. , Burkholder, G. , Sana, B. , & Szirony, M. (2020). Social Isolation as a predictor for mortality: Implications for COVID‐19 prognosis. medRxiv, 10.1101/2020.04.15.20066548 [DOI] [Google Scholar]
- Barrera, M. , Sandler, I. N. , & Ramsay, T. B. (1981). Preliminary development of a scale of social support: Studies on college students. American Journal of Community Psychology, 9(4), 435–447. 10.1007/BF00918174 [DOI] [Google Scholar]
- Baumeister, R. F. (2011). Need‐to‐belong theory. In Van Lange P. A. M., Kruglanski A. W. & Higgins E. T. (Eds.), Handbook of theories of social psychology (pp. 121–140). London, UK: Sage Publishing. [Google Scholar]
- Bianco, T. , & Eklund, R. C. (2001). Conceptual considerations for social support research in sport and exercise settings: The case of sport injury. Journal of Sport Exercise Psychology, 23, 85–107. 10.1123/jsep.23.2.85 [DOI] [Google Scholar]
- Booth, R. W. , & Tekes, B. (2019). Individual differences in anxiety and worry, not anxiety disorders, predict weakened executive control: Preliminary evidence. International Journal of Psychology and Psychological Therapy, 19, 337–344. [Google Scholar]
- Brooks, S. K. , Webster, R. K. , Smith, L. E. , Woodland, L. , Wessely, S. , Greenberg, N. & et al. (2020). The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The Lancet, 395, 912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo, J. T. , Hawkley, L. C. , Ernst, J. M. , Burleson, M. , Berntson, G. G. , Nouriani, B. & et al. (2006). Loneliness within a nomological net: An evolutionary perspective. Journal of Research in Personality, 40(6), 1054–1085. [Google Scholar]
- Cao, W. , Fang, Z. , Hou, G. , Han, M. , Xu, X. , Dong, J. et al. (2020). The psychological impact of the COVID‐19 epidemic on college students in China. Psychiatry Research, 287, 112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassel, J. (1976). The contribution of the social environment to the host resistance. American Journal of Epidemiology, 104, 107–123. [DOI] [PubMed] [Google Scholar]
- Center for Disease Control . (2019). Stress and coping. Retrieved from https://www.cdc.gov/coronavirus/2019‐ncov/daily‐life‐coping/managing‐stress‐anxiety.html [Google Scholar]
- Center for Disease Control . (2020). COVID‐19 in racial and ethnic minority groups. Retrieved from https://www.cdc.gov/coronavirus/2019‐ncov/need‐extra‐precautions/racial‐ethnic‐minorities.html [Google Scholar]
- Chew, Q. H. , Wei, K. C. , Vasoo, S. , Chua, H. C. , & Sim, K. (2020). Narrative synthesis of psychological and coping responses towards emerging infectious disease outbreaks in the general population: practical considerations for the COVID‐19 pandemic. Singapore Medical Journal, 61, 350–356. 10.11622/smedj.2020046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, S. , Gottlieb, B. H. , & Underwood, L. G. (2000). Social relationships and health. In Cohen S., Underwood L. G. & Gottlieb B. H. (Eds.), Social support measurement and intervention: A guide for health and social scientists (pp. 3–25). New York, NY: Oxford University Press. [Google Scholar]
- Cohen, S. , & Wills, T. A. (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98(2), 310–357. [PubMed] [Google Scholar]
- Field, A. (2009). Discovering statistics using SPSS:(and sex and drugs and rock'n'roll). Thousand Oaks, CA: Sage. [Google Scholar]
- Hawkley, L. C. , Burleson, M. H. , Berntson, G. G. , & Cacioppo, J. T. (2003). Loneliness in everyday life: Cardiovascular activity, psychosocial context, and health behaviors. Journal of Personality and Social Psychology, 85(1), 105–120. 10.1037/0022-3514.85.1.105 [DOI] [PubMed] [Google Scholar]
- Hofmann, S. G. , & Hay, A. C. (2018). Rethinking avoidance: Toward a balanced approach to avoidance in treating anxiety disorders. Journal of Anxiety Disorders, 55, 14–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaya, E. S. , Hillmann, T. E. , Reininger, K. M. , Gollwitzer, A. , & Lincoln, T. M. (2017). Loneliness and psychotic symptoms: The mediating role of depression. Cognitive Therapy and Research, 41, 106–116. [Google Scholar]
- Krypotos, A. M. , Effting, M. , Kindt, M. , & Beckers, T. (2015). Avoidance learning: A review of theoretical models and recent developments. Frontiers in Behavioral Neuroscience, 9, 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakey, B. , & Cohen, S. (2000). Social support and theory. In Cohen S., Underwood L. G. & Gotlieb B. H. (Eds.), Social support measurement and intervention: A guide for health and social scientists. New York, NY: Oxford University Press. [Google Scholar]
- Liu, C. H. , Zhang, E. , Wong, G. T. F. , & Hyun, S. (2020). Factors associated with depression, anxiety, and PTSD symptomatology during the COVID‐19 pandemic: Clinical implications for US young adult mental health. Psychiatry Research, 290, 113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loneliness . (n.d.). Merriam‐Webster.com dictionary. Retrieved from https://www.merriam‐webster.com/dictionary/loneliness [Google Scholar]
- Matrajt, L. , & Leung, T. (2020). Evaluating the effectiveness of social distancing interventions to delay or flatten the epidemic curve of coronavirus disease. Emerging Infectious Diseases, 26(8), 1740–1748. 10.3201/eid2608.201093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mertens, G. , Gerritsen, L. , Duijndam, S. , Salemink, E. , & Engelhard, I. M. (2020). Fear of the coronavirus (COVID‐19): Predictors in an online study conducted in March 2020. Journal of Anxiety Disorders, 74, 102258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson, B. , Pettitt, A. K. , Flannery, J. , & Allen, N. (2020). Psychological and epidemiological predictors of COVID‐19 concern and health‐related behaviors. Retrieved from https://psyarxiv.com/jftze/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris, F. H. , Watson, P. J. , Hamblen, J. L. , & Pfefferbaum, B. J. (2005). Provider perspectives on disaster mental health services in Oklahoma City. Journal of Aggression, Maltreatment & Trauma, 10(1–2), 649–661. [Google Scholar]
- Okruszek, L. , Aniszewska‐Stańczuk, A. , Piejka, A. , Wiśniewska, M. , & Żurek, K. (2020). Safe but lonely? Loneliness, mental health symptoms and COVID‐19. Retrieved from https://psyarxiv.com/9njps/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qualter, P. , Brown, Sl , Rotenberg, Kj , Vanhalst, J. , Harris, Ra , Goossens, L. et al. (2013). Trajectories of loneliness during childhood and adolescence: Predictors and health outcomes. Journal of Adolescence, 36(6), 1283–1293. [DOI] [PubMed] [Google Scholar]
- Rodgers, R. F. , Lombardo, C. , Cerolini, S. , Franko, D. L. , Omori, M. , Fuller‐Tyszkiewicz, M. et al. (2020). The impact of the COVID‐19 pandemic on eating disorder risk and symptoms. International Journal of Eating Disorders, 53, 1166–1170. 10.1002/eat.23318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satici, S. A. (2019). Facebook addiction and subjective well‐being: A study of the mediating role of shyness and loneliness. International Journal of Mental Health and Addiction, 17, 41–55. [Google Scholar]
- Stefanopoulou, E. , Hirsch, C. R. , Hayes, S. , Adlam, A. , & Coker, S. (2014). Are attentional control resources reduced by worry in Generalized Anxiety Disorder? Journal of Abnormal Psychology, 123, 330–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szkody, E. , & McKinney, C. (2019). Stress‐buffering effects of social support on depressive problems: Perceived vs. received social support and moderation by parental depressive problems. Journal of Child and Family Studies, 28, 2209–2219. 10.1007/s10826-019-01437-1 [DOI] [Google Scholar]
- Tull, M. T. , Edmonds, K. A. , Scamaldo, K. , Richmond, J. R. , Rose, J. P. , & Gratz, K. L. (2020). Psychological outcomes associated with stay‐at‐home orders and the perceived impact of COVID‐19 on daily life. Psychiatry Research, 289, 113098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHOQOL Group (1998). Development of the World Health Organization WHOQOL‐BREF quality of life assessment. Psychological Medicine, 28, 551–558. [DOI] [PubMed] [Google Scholar]
- World Health Organization . (2020). Coronavirus disease (COVID‐2019) situation reports. Retrieved from https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019/situation‐reports [Google Scholar]
- Xiao, H. , Zhang, Y. , Kong, D. , Li, S. , & Yang, N. (2020). Social capital and sleep quality in individuals who self‐isolated for 14 days during the coronavirus disease 2019 (COVID‐19) outbreak in January 2020 in China. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research, 26, e923921‐1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimet, G. D. , Dahlem, N. W. , Zimet, S. G. , & Farley, G. K. (1988). The multidimensional scale of perceived social support. Journal of Personality Assessment, 52(1), 30–41. 10.1207/s15327752jpa5201_2 [DOI] [PubMed] [Google Scholar]


