To the Editor,
Dermatology practices worldwide are resuming routine clinical activities in the postpandemic era. 1 , 2 Understanding the impact of the COVID‐19 pandemic on inpatient dermatology practices will empower physicians to better prepare for the challenges ahead. 3 , 4 , 5 We aimed to investigate changes in the composition of dermatology wards with respect to inpatient diagnoses and disease characteristics, once the lockdown was lifted in Hubei, the first and worst affected area of COVID‐19 in China.
In this retrospective study, data from 3838 patients admitted between 1 April and 31 May 2019 across seven tertiary hospitals (two hospitals in Wuhan and five hospitals in the other cities of Hubei province) were reviewed and compared to the corresponding period in 2020. We identified a dramatic reduction in the number of admissions (60.79%; 1081 vs. 2747, P < 0.001) compared to 2019, with the highest decline observed in Wuhan (89.58%). Notably, most patients tended to visit nearby hospitals (Fig. 1). However, in 2020, Wuhan hospitals, serving as referral centres for critically ill patients, admitted significantly more patients from surrounding cities (14.47% vs. 26.25%, P = 0.009; Fig. 1) and recorded longer inpatient stays (6.79 vs. 10.00 days, P < 0.001). Compared to 2019, the proportion of patients hospitalized with viral infections, skin tumours and drug eruptions decreased, while admissions for eczema, erythemas and papulosquamous dermatoses increased (Fig. 1). We postulate that the decrease seen in viral infections after the COVID‐19 outbreak was due to the increased use of masks and social distancing measures. The increase in eczema cases was likely from increased use of hand disinfectants. When limited to hospitals in Wuhan, the proportion of admissions due to malignant skin tumours increased significantly (23.22–45.76%). Furthermore, in age‐stratified analysis, the largest proportional declines existed in children aged ≤14 years (71.00%; Table 1).
Figure 1.
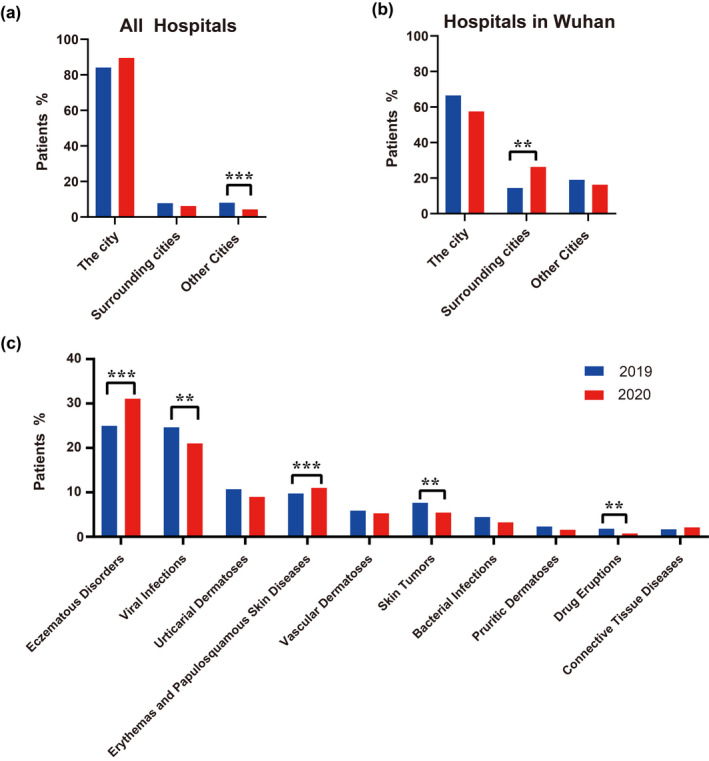
Residential Distribution of Admitted Patients in Dermatology Wards of (A) all hospitals, (B) hospitals in Wuhan and (C) disease spectrum of admitted patients in Dermatology wards during 1 April – 31 May 2020 compared with the corresponding periods in 2019 at Hubei province, China. The city is where the hospital located. Surrounding cities: The neighbouring cities geographically adjacent to the city where the hospital is located. Other cities: The cities geographically not adjacent to the city where the hospital is located.
Table 1.
Clinical characteristics of inpatients in dermatology† between 1 April and 31 May 2020 compared with the corresponding periods in 2019
| 2019 (N = 2757) | 2020 (N = 1081) | P | |
|---|---|---|---|
| Sex, n (%) | |||
| Male | 1323 (47.99) | 542 (50.14) | 0.236 |
| Female | 1434 (52.01) | 539 (49.86) | |
| Age, median (IQR) | 45.00 (25.00, 60.00) | 47.00 (30.00, 60.50) | 0.011 |
| Stratified by age, n (%) | |||
| 0–14 | 369 (13.38) | 107 (9.90) | 0.003 |
| 14–30 | 510 (18.50) | 177 (16.37) | 0.134 |
| 30–40 | 366 (13.28) | 151 (13.97) | 0.564 |
| 40–50 | 413 (14.98) | 178 (16.47) | 0.253 |
| 50–60 | 425 (15.42) | 198 (18.32) | 0.032 |
| >60 | 673 (24.41) | 270 (24.98) | 0.708 |
| Hospital stay, median (IQR) | 7.00 (5.00, 9.91) | 9.00 (6.64, 12.00) | <0.001 |
| Location of hospitals, n (%) | |||
| Hospitals in Wuhan | 858 (31.12) | 80 (7.40) | <0.001 |
| Hospitals in other cites | 1899 (68.88) | 1001 (92.60) | |
| Residential location of patients, n (%) | |||
| The city† | 2320 (84.15) | 968 (89.55) | 0.355 |
| Surrounding cities† | 216 (7.83) | 67 (6.20) | 0.086 |
| Other cities† | 221 (8.02) | 46 (4.26) | <0.001 |
| Disease classification, n (%) | |||
| Eczematous disorders | 689 (24.99) | 336 (31.08) | <0.001 |
| Viral infections | 680 (24.66) | 227 (21.00) | 0.016 |
| Urticarial dermatoses | 295 (10.70) | 97 (8.97) | 0.123 |
| Erythema and Papulosquamous skin diseases | 269 (9.76) | 119 (11.01) | <0.001 |
| Vascular dermatoses | 162 (5.88) | 57 (5.27) | 0.487 |
| Skin tumours | 211 (7.66) | 59 (5.46) | 0.017 |
| Malignant skin tumours | 49 (1.78) | 27 (2.50) | 0.157 |
| Bacterial infections | 123 (4.46) | 35 (3.24) | 0.104 |
| Pruritic dermatoses | 64 (2.32) | 17 (1.57) | 0.170 |
| Drug eruptions | 50 (1.81) | 8 (0.74) | 0.012 |
| Connective tissue diseases | 46 (1.67) | 23 (2.13) | 0.345 |
IQR, interquartile range.
Inpatients in Dermatology: The inpatients come from the wards of dermatology of 7 hospitals including Wuhan Union Hospital, Zhongnan Hospital of Wuhan University, Xiaogan Central Hospital affiliated with Wuhan University of Science and Technology, Huanggang Central Hospital, Xiangyang Hospital Affiliated with Hubei University of Chinese Medicine, Shiyan Renmin Hospital and Shiyan Taihe Hospital. ‡The city is where the hospital located. §Surrounding cities: The neighbouring cities geographically adjacent to the city where the hospital is located. ¶Other cities: The cities geographically not adjacent to the city where the hospital is located.
A 2‐sided P‐value less than 0.05 was considered statistically significant.
In Wuhan Union Hospital, skin tumours (18.54%), eczema (17.22%), erythemas and papulosquamous dermatoses (16.56%) and connective tissue diseases (14.57%) were the most common admission diagnoses between 1 April and 31 June 2020. 47.22% of the patients were admitted to sub‐specialty teams providing high acuity care for complex dermatological disease presentations.
This study had several limitations. (i) misclassification of patients could have occurred if diagnostic categories were applied inconsistently and non‐uniformly across hospitals. (ii) Although this was a multicentre study, it included only seven out of 72 tertiary care hospitals in Hubei; thus, limited samples were represented. (iii) As a retrospective, observational study no conclusions can be drawn about the causal relationship between the impact of the pandemic and the increased proportion of admissions with severe disease presentations.
In conclusion, our study demonstrates a significant impact of the pandemic on the composition and inpatient characteristics of Hubei's dermatology wards postlockdown. 2 Most patients were inclined to postpone their hospital visits and instead sought less specialized care nearby. Citywide lockdowns and public fear of virus spread limited people's movements. During the pandemic, more patients with severe dermatological disease presentations were ultimately hospitalized, and the trend continued postlockdown. These experiences could be replicated in dermatology departments around the world in the postpandemic recovery period, and anticipating these trends can inform decision‐making for clinicians.
Financial disclosures
None.
Funding source
This work was supported by HUST COVID‐19 Rapid Response Call Program (2020kfyXGYJ056) and Hubei Provincial Emergency Science and Technology Program for COVID‐19 (2020FCA037).
Conflicts of interest
Dr. Yamin Zhang, Dr. Jingjing Wen, Dr. Mahin Alamgir, Dr. Jun Xie, Dr. Haixia Jing, Dr. Muping Fang, Dr. Jianxiu Wang, Dr. Meng Zhang, Dr. Zudong Meng, Dr. Liu Yang and Dr. Juan Tao have nothing to disclose.
Acknowledgements
We want to express our deep respect for all the first‐line health care workers for their dedication in the fight against SARS‐CoV‐2 and thank the healthcare workers who participated in this study.
Contributor Information
L. Yang, Email: bengpao82@163.com.
J. Tao, Email: tjhappy@126.com.
References
- 1. Hartnett KP, Kite‐Powell A, DeVies J, Coletta MA, Boehmer TK, Adjemian J et al. Impact of the COVID‐19 pandemic on emergency department visits ‐ United States, January 1, 2019‐May 30, 2020. MMWR Morb Mortal Wkly Rep 2020; 69: 699–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Litchman GH, Rigel DS. The immediate impact of COVID‐19 on US dermatology practices. J Am Acad Dermatol 2020; 83: 685–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Earnshaw CH, Hunter HJA, McMullen E, Griffiths CEM, Warren RB. Reduction in skin cancer diagnosis, and overall cancer referrals, during the COVID‐19 pandemic. Br J Dermatol 2020; 183: 792–794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Arnold JD, Yoon S, Kirkorian AY. The national burden of inpatient dermatology in adults. J Am Acad Dermatol 2019; 80: 425–432. [DOI] [PubMed] [Google Scholar]
- 5. Zhang Y, Wen J, Chen C et al. Challenges and countermeasures in the prevention of nosocomial infections of SARS‐CoV‐2 before resumption of work: implications for the dermatology department. J Am Acad Dermatol 2020; 83: 961–963. [DOI] [PMC free article] [PubMed] [Google Scholar]


