Abstract
Background
This survey of centers caring for patients receiving home parenteral nutrition (HPN) was conducted to assess the impact of the coronavirus disease 2019 (COVID‐19) crisis on the management of these patients regarding provision of care, monitoring, regular follow‐up, and any changes to service infrastructure.
Methods
A survey was devised and publically published on the Research Electronic Data Capture database management system, with individual centers responding to a public link.
Results
A total of 78 adult and pediatric centers worldwide contributed to the survey, representing ≥3500 patients’ experiences. Centers reported infrastructure maintenance for Parenteral Nutrition (PN) bag deliveries to patients (60, 76.92%) or delivery of ancillary items (57, 73.08%), home delivery and HPN administration (65, 83.33%), and home care nurse shortages (25, 32.05%). Routine follow‐up of HPN patients changed to either all telemed or mixed with emergency clinic review (70, 89.74%). In 26 centers (33.33%), HPN for newly discharged patients with benign conditions was reduced or stopped. Based on clinical history, the centers reported psychological distress for patients (52, 66.67%), with anxiety, worry, concern, and apprehension reported most frequently (37 of 52, 71.15%) but also fear (10 of 52, 19.23%), depression (5 of 52, 9.62%), and issues related to isolation/confinement (12 of 52, 23.08%).
Conclusions
The COVID‐19 pandemic was reported by clinicians to have had a far‐reaching adverse impact on patients receiving HPN, especially their safety in terms of provision of personal protective equipment, PN bags, available nursing staff, and psychological well‐being. Healthcare systems responded to the challenge and presented new ways of working.
Keywords: coronavirus disease 2019, chronic intestinal failure, home parenteral nutrition, parenteral nutrition
Clinical Relevancy Statement
This article describes a unique survey on the impact of the coronavirus disease 2019 pandemic on the management of patients with chronic intestinal failure who are receiving home parenteral nutrition (HPN). Provision of bags and materials, regular monitoring, initiation of HPN for new patients, and the psychological behavior of patients were affected. The HPN teams reacted by developping new ways of working.
Introduction
Since December 2019 when the first cases of coronavirus disease 2019 (COVID‐19), caused by severe acute respiratory syndrome coronavirus 2, were reported 1 , 2 and subsequently developed into a pandemic, clinicians across the world have been struggling to effectively treat this infection. It has been characterized by asymptomatic carriage or low‐grade symptoms for the majority of those affected, with a minority developing low‐oxygen saturations followed by rapid deterioration into a severe acute respiratory syndrome. 3 The typical risk factors appear to be older age; multiple comorbidities, including diabetes, hypertension, and respiratory disease; and ethnicity. 4 , 5
Intestinal failure (IF) is a relatively rare condition in which the gut is unable to support life. 6 Treatment is by a central venous catheter (CVC) to provide the nutrients in the form of parenteral nutrition (PN). There are 3 main types of IF following abdominal surgery 6 , 7 :
Patients receiving home PN (HPN) are at risk of complications associated with IF, including catheter‐associated bloodstream infections (CRBSIs) and loss of CV access from venous thromboembolic phenomena. 6 , 8 , 9 Patients, therefore, require meticulous care of their CVC, with ready access to gloves and disinfectants to prevent infections. The lowest CRBSI infection rates are observed in patients who are nursed in some series. 10 Prevention of infection with COVID‐19 is thought to be reduced through mask usage 11 given the risk of airborne viral infections, 12 and masks should therefore be available for all carers, whether home care nurses or relatives. The ready availability of monitoring through biochemical assessments, clinic appointments, pertinent radiological investigations, and access to fully staffed teams are important strategies to protect these vulnerable patients, as recommended by the European Society for Clinical Nutrition and Metabolism (ESPEN). 6 , 13 , 14
Patients with IF share similar key characteristics with patients who are most at risk for COVID‐19. As a population, they are at risk of malnutrition and have comorbidities and, as a population, are getting older: 20%–36% of patients receiving HPN were aged >65–69 years, 10 with ≤20% having multiple comorbidities. 10 It is not unsurprising, therefore, that recommendations to prevent infection in patients with IF have suggested this can be achieved through isolating patients at risk 15 , . 16
It was for these reasons that we wanted to survey clinicians who were caring for patients receiving HPN to determine how our caring for patients receiving HPN has changed and if patients/carers/nurses experienced deficiencies of care during the pandemic, whether in supply chain or in the way that we care for patients.
Methods
Study data were collected and managed by using Research Electronic Data Capture (REDCap) tools hosted by the University of Oxford, Medical Sciences Division. 17 , 18 The survey questionnaire was sent as a public link, provided on the ESPEN website and in the ESPEN newsletter, to 122 centers on the ESPEN chronic IF database. 6 The survey was open from May 1, 2020, to June 10, 2020. The only identifier recorded was the name of the institution and the country location. REDCap is a secure, web‐based software platform designed to support data capture for research studies, providing (1) an intuitive interface for validated data capture; (2) audit trails for tracking data manipulation and export procedures; (3) automated export procedures for seamless data downloads to common statistical packages; and (4) procedures for data integration and interoperability with external sources. The results were analyzed by using Excel (Microsoft; Redmond, Washington, USA).
When respondents were unsure of whether they had any patients infected with COVID‐19, all subsequent data surrounding rates of presentation symptoms, administration of PN, and inpatient management were included in the “not infected” responses.
Definitions and Areas Questioned
The study was divided into 15 sections:
-
Demographics
Name of the center, country of origin, number of patients receiving HPN (ranges), and proportion of benign or malignant disease process
-
COVID‐19 infection
Awareness of COVID‐19 infection in their patients; whether receiving HPN affected escalation of care; and ability to follow patients on their journey with infection
-
In those hospitalized with COVID‐19, awareness of whether patients contracted COVID‐19
Community vs hospital acquired
Presenting symptomatology for COVID‐19
-
Care organization for HPN patients
Programmed hospitalization (investigations and treatment) and emergency admission (HPN complications)
-
PN administration for patients infected with COVID‐19
Self‐care, nurse, or relative/carer
Reduced access to home care nursing
-
Shortage of infrastructure
HPN administration, bag supply, and ancillaries
HPN administration refers to underlying work that goes into caring for HPN patients
-
Shortage of personal protective equipment (PPE)
Masks, gloves, and disinfectant
Masks were for carers/nurses administering PN
-
Clinical reviews during the pandemic and changes to ways of working
Clinics, biochemistry, and other investigations (echo, radiological, and endoscopic)
Psychological impact on patients was subjectively assessed by the clinicians. The questionnaire allows free‐text responses.
-
New patients discharged home who are receiving HPN; was there a change in proportions discharged?
Benign and malignant
Results
Location of Survey Respondents
A total of 78 centers from around the world contributed to the survey, representing ≥3500 patient experiences from both adult and pediatric centers, with ≥8 pediatric centers caring for <10 patients in 4 of 8 (50%), 10–30 patients in 3 of 8 (37.5%), and 30–50 patients in 1 of 8 (12.5%). Continents represented include Asia (2 centers), Australia (6 centers), North America (3 centers), South America (4 centers), and Europe (63 centers). Within Europe, the countries with the highest COVID‐19 infection rates (UK, Italy, Spain, Germany, and France) accounted for 66.67% of all the European centers, representing ≥1780 patients.
HPN Center Demographics
All of these centers accounted for a wide spread of HPN population density. Figure 1 shows the range of numbers of patients receiving HPN represented as the number and percentage of centers that have patients receiving HPN. A total 34.61% (27 of 78) had >50 patients receiving HPN. Seventy‐five percent of the patients cared for by responding centers had IF because of benign conditions and 25% were due to malignant conditions.
Figure 1.
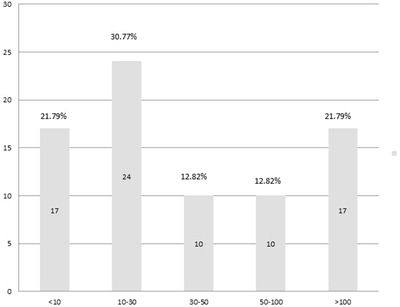
Histogram of the number of patients per center.
Implications of the Pandemic on Service Provision
Changes in home care infrastructure
The proportion of centers experiencing a reduction in home care provision was greatest for ancillaries (dressing packs, giving sets, and other consumables) in which 17 (21.79%) had a reduction in service: 14 (17.95%) had a <50% reduction; 1 (1.28%) had a >50% reduction; 2 (2.56%) were completely reduced; 57 (73.08%) had no reduction; and 4 (5.13%) were unsure. Similarly, 16 (20.51%) had reduced service for the provision of PN bags: 13 (16.67%) had a <50% reduction; 2 (2.56%) had a >50% reduction; 1 was completely reduced (1.28%); 60 (76.92%) had no reduction; and 2 (2.56%) were unsure. Lastly, HPN administration was reduced in 12 (15.38%) centers: 10 had a <50% reduction (12.82%); 2 had a >50% reduction (2.56%); 0 were completely reduced; 65 (83.33%) were maintained; and 1 (1.28) was unsure. In contrast, for HPN nurse availability: 25 (32.05%) had a shortage of HPN nurses; 45 (53.85%) had no shortage; and 11 (14.10%) were unsure if there had been a shortage.
PPE provision was reported for masks, and 24 (30.77%) centers had a reduction in provision: 14 (17.95%) had a <50% reduction; 8 (10.26) had a >50% reduction; 2 were completely reduced (2.56%); 39 (50.00%) were maintained; and 15 (19.23%) were unsure. For gloves, 15 (19.20%) centers were reduced: 11 (14.10%) had a <50% reduction; 3 (3.85) had a >50% reduction; 1 (1.28%) was all reduced; 53 (67.95%) were maintained; and 10 (12.82%) were unsure. Lastly, disinfectant to clean the CVCs in 21 centers (26.92%) was reduced: 13 (16.67%) had a <50% reduction; 6 (7.69%) had a >50% reduction; 2 (2.56%) were all reduced; 47 (60.26%) were maintained; and 10 (12.82%) were unsure.
Changes in hospital infrastructure
A total of 58 (74.36%) centers reduced their routine work caring for patients receiving HPN: 7 (8.97%) had a <50% reduction; 17 (21.79%) had a >50% reduction; 34 (43.59%) were all reduced; 15 (19.23%) were maintained; and 5 (6.41%) were unsure. In contrast, emergency availability for HPN patients continued, with only 7 (8.98%) having a reduction in emergency work: 3 (3.85) were <50% reduced; 4 of 78 (5.13%) were >50% reduced; and 71 of 78 (91.03%) were maintained.
Seventy (89.74%) centers changed to either all telemed or a mixture of telemed and emergency clinic review, as can be seen in Table 1. In addition, the frequency of biochemistry testing was reduced or stopped in 50 (64.11%) centers, and routine or nonurgent radiological tests were reduced or stopped in 71.79%.
Table 1.
Changes in the Proportion of Centers (n, %) in the Setup of Clinics and Biochemistry and Radiological Investigations
| Clinics | Biochemistry | Investigations | ||||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | n | % | |||
| Face‐to‐face only | 1 | 1.28 | Maintained routine testing | 28 | 35.90 | Maintained routine testing | 4 | 5.13 |
| Postponed | 4 | 5.13 | Reduced testing | 47 | 60.26 | Reduced testing | 18 | 23.08 |
| Telemed only | 41 | 52.56 | Stopped testing | 3 | 3.85 | Emergency testing only | 50 | 64.10 |
| DC to GP | 3 | 3.85 | Stopped testing | 6 | 7.69 | |||
| Mixture of above | 29 | 37.18 | No review if done | 0 | 0.00 | |||
DC, discharge; GP, general practioner.
Lastly, it was important to assess the impact the COVID‐19 pandemic had on planned discharges and whether there was a difference for benign or malignant conditions. Indeed, both conditions fared similarly, with a reduction or cessation of discharged patients receiving HPN for benign conditions occurring in 33.33% of centers and in 29.48% of centers for malignant conditions.
Despite the risk that the COVID‐19 pandemic could have had on the infrastructure of HPN delivery (production, delivery, and administration), although there was a reduction observed, the majority of centers reported favorable outcomes regarding sustainability within the system.
Impact of the Pandemic on the Psychological Well‐Being of Patients
The majority of centers (52, 66.67%) reported opinions about the psychological impact of the pandemic on patients receiving HPN. Looking at the frequency of free‐text responses, certain themes appeared and are reported as a proportion of those who responded that the pandemic did have an impact on the psychology of their patients: 71.15% reported words or phrases that encompassed anxiety, worry, concern, and apprehension; 19.23% reported fear; 9.62% reported depression; stress was reported in 7.69%; and 23.08% reported negative thoughts or feelings surrounding isolation or confinement caused by the pandemic.
COVID‐19 Infection
Although 53 (67.95%) centers did not report any cases of patients receiving HPN who were infected with COVID‐19, 7 (8.97%) centers were unsure of the number of patients but might have had patients infected. In 18 (23.08%) centers, they reported 37 patients known to have swab‐positive or computed tomography scan positive changes consistent with COVID‐19, for whom 28 were thought to be community acquired and 7 hospital acquired; 2 were unknown.
Figure 2 shows a flow diagram of outcomes of those patients receiving HPN who were infected with COVID‐19. Over 10% of patients infected and admitted (14.81% [4 of 28]) required ventilatory support in the form of noninvasive ventilation or intubation. Because IF is not routinely reported as a normal risk comorbidity for COVID‐19 infection, we asked whether receiving HPN was used to determine escalation limits: 19 (24.36%) reported HPN contributed to decision‐making regarding escalation to therapy for patients infected; 36 (46.15%) reported it was not considered as a comorbidity to affect escalation plans; 23 (29.49%) were unsure if it did or not.
Figure 2.
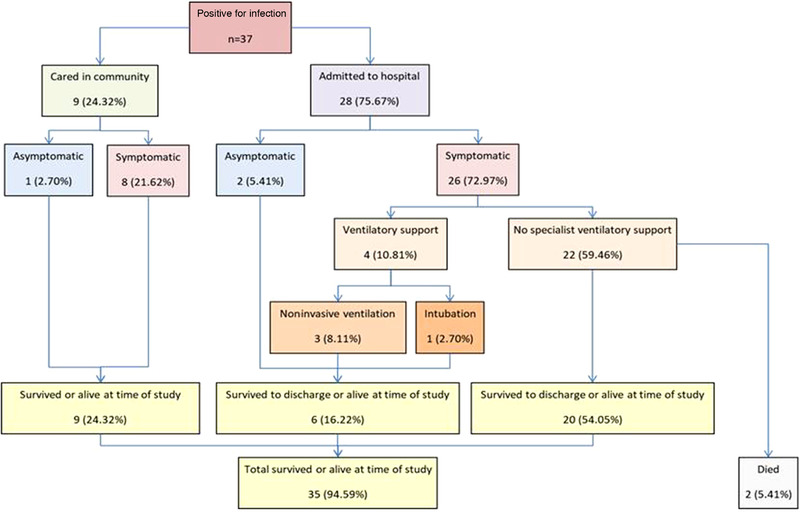
Flow diagram of the outcomes of patients receiving home parenteral nutrition who are infected with COVID‐19. Percentages as a proportion of those infected with COVID‐19. COVID‐19, coronavirus disease 2019.
Symptoms of COVID‐19 displayed in these patients who were admitted were thought to be as follows: digestive symptoms (5 of 37 [13.51%]); hydroelectrolyte problems (5 of 37 [13.51%]); malnutrition (0 of 37); neurological (1 of 37 [2.70%]); pulmonary symptoms (16 of 37 [43.24%]); pyrexia (22 of 37 [59.46%]); and none of the above (1 of 37 [2.70%]).
We found that of those patients who had COVID‐19 infection, 18 of 37 (48.65%) self‐administered PN, 17 of 37 (45.95%) were nursed, and 4 of 37 (10.81%) had family or a relative provide it; 2 patients did a mixture of self‐administration and family‐member administration.
Discussion and Conclusion
This survey has shown that from centers across the world, the COVID‐19 pandemic has affected the infrastructure surrounding care for patients receiving HPN. For the majority of centers, the provision of nursing care, PPE, and administration of HPN has remained unaffected. In addition, routine follow‐up of patients receiving HPN has changed from being face‐to‐face to using telemedicine, with an associated reduction in routine monitoring of biochemistry and radiological procedures. The ability to discharge home new patients receiving HPN was restricted for both benign and malignant conditions and to a similar degree. The opinion of the clinicians within each center was that the pandemic was having a negative impact on their patients’ psychology in terms of feelings of anxiety, fear, depression, and thoughts surrounding isolation or confinement.
The dilemma for health authorities is the balance between general infection‐control measures that PPE affords vs protecting a valuable resource for healthcare professionals, and this has caused some to recommend not wearing masks. 19 However, the use of mask protection suggests they are helpful in protecting the wearer and preventing community spread, 20 with a marked reduction of ∼90% in virus transmission. 21 It is worrying to note that in this survey, nursing teams caring for patients receiving HPN were not able to access appropriate masks in 30.77% of centers. The lack of other PPE for appropriate CVC care puts patients at risk of CRBSIs. 8 Unfortunately, this survey was not able to assess the impact of the loss of access to appropriate PPE or nursing support available on complications associated with IF, such as CRBSI, but this information may become available in later studies.
Small‐scale telemedicine was already being practiced for select patients to reduce the distance traveled to HPN centers. 22 , 23 In a state of emergency, this has been rolled out widely, in which 89.74% of centers changed to all or a mixture of face‐to‐face work for emergencies and telemedicine and using technological platforms, with an associated reduction in routine work in favor of keeping emergency work available. Although 83% of healthcare professionals were inexperienced at using telemedicine in one study from Spain, 96% thought it was an adequate method of carrying out healthcare and useful for medical follow‐up of patients with chronic diseases who may come from a geographically dispersed area and who needed routine administration such as prescription provision, 24 which characterizes patients receiving HPN. Reluctance to commence telemedicine is thought to be due to 3 main barriers: clinician willingness, reimbursement, and healthcare organization. 25 The reimbursement is often the area that is needed to reassure healthcare providers that it is cost‐effective to change. The further changes observed in monitoring with a reduction or cessation of biochemistry in 64.11% of centers and radiology in 30.77% of centers, coupled with the reduction in elective work, remain to be seen in the delayed impact this will have on patient outcomes, although the small‐scale pilot studies found better outcomes for those selected patients. 22 , 23
Where patients do gain access to medical services, only 20% of COVID‐19 infections are thought to require admission. 26 The presentation of symptoms fits with commonly observed patterns of pyrexia as the main symptom; 1 , 2 , 4 however, some studies have suggested gastrointestinal symptoms may account for 2%–40% of cases. 1 , 2 , 4 We noted similar observations to those reported in early series in which noninvasive ventilation rates of 13%–24% and invasive mechanical ventilation of 4%–5% 1 , 2 were higher than observed here, in which 8.11% had noninvasive ventilation and 2.70% were intubated. We observed a 5.41% mortality rate for patients receiving HPN compared with 11%–15% in early series. 1 , 2 A follow‐up survey will be performed within the next few months, as the present survey was not really designed to detect complications potentially related to COVID‐19 infection.
The rise of psychological morbidity for patients receiving HPN in the face of an ongoing pandemic is worrying. Although it was a subjective evaluation by the clinicians, it is of interest that 71.15% of centers reported words or phrases that encompassed anxiety, worry, concern, and apprehension; 19.23% reported fear; 9.62% reported depression; 7.69% reported stress; and 23.08% reported negative thoughts or feelings surrounding isolation or confinement caused by the pandemic. This compares with a study of 1210 Chinese residents that found 53% suggested the pandemic caused moderate to severe psychological distress, and they reported a number of different psychological symptoms: depression (17%), anxiety (29%), and stress (8%) 27 . Interestingly, the authors also reported better outcomes for those with specific up‐to‐date information (such as local infection rates) and messages of precautionary measures (eg, hand hygiene or mask wearing).
The COVID‐19 pandemic was reported to have had a far‐reaching adverse impact on patients receiving HPN, especially their safety in terms of the provision of PPE, PN bags, available nursing staff, and psychological well‐being. Healthcare systems responded to the challenge and presented new ways of working.
Statement of AuthorshipA. Van Gossum, L. Pironi, F. Joly, S. Lal, and P. Allan equally contibuted to the conception and the design of the survey; P. Allan contributed to the acquisition and analysis of the data; P. Allan drafted the manuscript; and A. Van Gossum, L. Pironi, F. Joly, S. Lal, and P. Allan contibuted to the interpretation of the data. All authors critically revised the manuscript, agree to be fully accountable for ensuring the intergrity and accuracy of the work, and read and approve the final manuscript as submitted.
Conflicts of interest
L. Pironi is on the advisatory board for Baxter and Takeda, provides scientific communication for Fresenius Kabi, and is a consultant for B Braun. All other authors have no conflicts of interest to disclose.
Acknowledgments
P. Allan would like to thank Prof Paul Klenerman for assistance in setting up the REDCap database. The research was supported by the National Institute for Health Research (NIHR) Oxford Biomedical Research Centre. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. We would like to thank the following contributing centers: Rigshospitalet, Belfast Trust, Addenbrooke's Hospital Cambridge, University Hospital Coventry, Salford Royal Hospital NHS Foundation Trust, Radboud University Nijmegen Medical Centre, Centre Hospitalier Universitaire de Nice, Azienda Ospedaliera Universitaria Città della Salute e della Scienza, Norfolk & Norwich University Hospital, Raffaele DIMICCOLI Hospital Barletta, Children's Hospital Affiliate of Vilnius University Hospital, Santaros Kliniko, Hospital Universitario Miguel Servet de Zaragoza, University Hospital Leuven, Department of Woman and Child's Health University Hospital of Padova, Gaslini Institute for Child Health IRCCS G. Gaslini, Hospital General Universitario Gregorio Maranon, Erasme, Hospital Universitari Arnau de Vilanova, Centre for Postgraduate Medical Education Warsaw, Military Hospital Budapest, Hospital Universitari Bellvitge, Queensland Children's Hospital, Royal Prince Alfred Hospital Sydney, Children`s Clinical University Hospital, ASST Grande Ospedale Metropolitano Niguarda, Orlandi Bussolengo, Hospital Universitario Ramón y Cajal, Royal London Hospital, Beaujon Hospital, Cleveland Clinic, Hospital das Clínicas of São Paulo University School of Medicine, Hospital Regional Universitario De Málaga, Nicolaus Copernicus Hospital Gdansk, University Hospital Inselspital Bern, University Hospital of Wales, St Orsola Hospital University of Bologna, Rabin Medical Center, IRCCS INRCA – Ancona, Glasgow Royal Infirmary, Schneider's Children Medical Center, Hospital 12 de Octubre, Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo, Institut de Cancerologie de l'Ouest, Chu de Rennes, University Hospital of North Norway, Stanley Dudrick Hospital Skawina, Azienda Policlinico Umberto I Rome, University Hospital Center of Limoges, Hospital Clínico San Carlos, Erasmus MC Sophia Children's Hospital, SOLCA Guayaquil, Ramazzini, Kralovske Vinohrady University Hospital, University Hospital, Southampton NHS Foundation Trust, Hospital Virgen del Camino, Christchurch, 12 de Octubre Universitary Hospital, Starship Children's Hospital, Asklepios Klinik St. Georg Hamburg, Inselspital Bern, Odense University Hospital, Helsinki University Hospital, Laiko General Hospital of Athens, Fiona Stanley Hospital, Sahlgrenska University Hospital, Hull University Hospitals Trust, SPSK 4 Lublin Medical University of Lublin, Auckland District Health Board, Hospital de Navarra, AUSl di Parma, Nottingham University Hospital, Hospital Universitario Fundación Favaloro, LK Horn, Oxford University Hospitals NHS Foundation Trust, Clinique Saint‐Yves, Hospices Civils de Lyon, Toronto General Hospital, and Mayo Clinic
[Correction added on 28 January 2021, after first online publication: The affiliation of the author Loris Pironi was revised.]
References
- 1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497‐506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507‐513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID‐19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054‐1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zhang JJ, Dong X, Cao YY, et al. Clinical characteristics of 140 patients infected with SARS‐CoV‐2 in Wuhan, China. Allergy. 2020;75(7):1730‐1741. [DOI] [PubMed] [Google Scholar]
- 5. Khunti K, Singh AK, Pareek M, Hanif W. Is ethnicity linked to incidence or outcomes of covid‐19? BMJ. 2020;369:m1548. [DOI] [PubMed] [Google Scholar]
- 6. Pironi L, Arends J, Bozzetti F, et al. ESPEN guidelines on chronic intestinal failure in adults. Clin Nutr. 2016;35(2):247‐307. [DOI] [PubMed] [Google Scholar]
- 7. Lal S, Teubner A, Shaffer JL. Review article: intestinal failure. Aliment Pharmacol Ther. 2006;24(1):19‐31. [DOI] [PubMed] [Google Scholar]
- 8. Allan P, Lal S. Intestinal failure: a review. F1000Res. 2018;7:85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Allan PJ, Lal S. Metabolic bone diseases in intestinal failure. J Hum Nutr Diet. 2020;33(3):423‐430. [DOI] [PubMed] [Google Scholar]
- 10. Bond A, Soop M, Taylor M, et al. Home parenteral nutrition and the older adult: Experience from a national intestinal failure unit. Clin Nutr. 2020;39(5):1418‐1422. [DOI] [PubMed] [Google Scholar]
- 11. Leung CC, Lam TH, Cheng KK. Mass masking in the COVID‐19 epidemic: people need guidance. Lancet. 2020;395(10228):945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Long Y, Hu T, Liu L, et al. Effectiveness of N95 respirators versus surgical masks against influenza: A systematic review and meta‐analysis. J Evid Based Med. 2020;13(2):93‐101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lal S, Van Gossum A, Joly F, et al. Considerations for the management of home parenteral nutrition during the SARS‐CoV‐2 pandemic: A position paper from the Home Artificial Nutrition and Chronic Intestinal Failure Special Interest Group of ESPEN. Clin Nutr. 2020;39(7):1988‐1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pironi L, Boeykens K, Bozzetti F, et al. ESPEN guideline on home parenteral nutrition. Clin Nutr. 2020;39(6):1645‐1666. [DOI] [PubMed] [Google Scholar]
- 15. An P, Ji M, Ren H, et al. Prevention of COVID‐19 in patients with inflammatory bowel disease in Wuhan, China. Lancet Gastroenterol Hepatol. 2020;5(6):525‐527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kennedy NA, Jones GR, Lamb CA, et al. British Society of Gastroenterology guidance for management of inflammatory bowel disease during the COVID‐19 pandemic. Gut. 2020;69(6):984‐990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377‐381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Feng S, Shen C, Xia N, Song W, Fan M, Cowling BJ. Rational use of face masks in the COVID‐19 pandemic. Lancet Respir Med. 2020;8(5):434‐436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Liu X, Zhang S. COVID‐19: Face masks and human‐to‐human transmission. Influenza Other Respir Viruses. 2020;14(4):472‐473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ma QX, Shan H, Zhang HL, Li GM, Yang RM, Chen JM. Potential utilities of mask‐wearing and instant hand hygiene for fighting SARS‐CoV‐2. J Med Virol.9, 2020;10.1002/jmv.25805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Saqui O, Chang A, McGonigle S, et al. Telehealth videoconferencing: improving home parenteral nutrition patient care to rural areas of Ontario, Canada. JPEN J Parenter Enteral Nutr. 2007;31(3):234‐239. [DOI] [PubMed] [Google Scholar]
- 23. Cloutier A, Bond A, Taylor MI, et al. Successful implementation of remote video consultations for patients receiving home parenteral nutrition in a national UK Centre. Frontline Gastroenterol. 2020;11(4):280‐284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jimenez‐Rodriguez D, Santillan Garcia A, Montoro Robles J, et al. Increase in Video Consultations During the COVID‐19 Pandemic: Healthcare Professionals' Perceptions about Their Implementation and Adequate Management. Int J Environ Res Public Health. 2020;17(14). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID‐19). J Telemed Telecare. 2020;26(5):309‐313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Media Statement: Knowing the risks for COVID‐19 [press release]. WHO Indonesia website: World Health Organisation, 8 March 2020 2020. [Google Scholar]
- 27. Wang C, Pan R, Wan X, et al. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID‐19) Epidemic among the General Population in China. Int J Environ Res Public Health. 2020;17(5). [DOI] [PMC free article] [PubMed] [Google Scholar]


