Abstract
We report a unique case of a young woman with recurrent immune‐mediated (virus‐negative) lymphocytic fulminant myocarditis during the coronavirus disease 2019 pandemic. At the first endomyocardial biopsy (EMB)‐proven episode, she had concomitant pneumonia, and a temporary biventricular assist device implant was followed by complete and long‐lasting cardiac recovery. Five years later, she was re‐admitted for relapsing cardiogenic shock with a recent history of pneumonia. She was treated with extracorporeal life support with apical venting for left ventricular unloading, and full recovery was achieved. Despite negative seriate nasopharyngeal swabs and EMB during hospitalization, an antibody positivity for severe acute respiratory syndrome coronavirus 2 was discovered after 4 weeks from discharge. This is the first report of an EMB‐proven, immune‐mediated (virus‐negative) recurrence of fulminant myocarditis. We hypothesize that in patients with a predisposing immunogenetic background, autoimmune disease may be triggered or reactivated by major infections, for example, pneumonia, that may act as adjuvants leading to an immune‐mediated hyper‐response.
Keywords: fulminant myocarditis, recurrent myocarditis, virus‐negative lymphocytic myocarditis
Introduction
Fulminant myocarditis (FM) is characterized by sudden onset with haemodynamic compromise requiring immediate inotropic therapy and/or mechanical circulatory support (MCS). 1 , 2 , 3 In FM, endomyocardial biopsy (EMB) is mandatory to achieve certainty in diagnosis and guide aetiology‐directed therapy. 2
Case report
In February 2015, a 40‐year‐old female and mother of two young children presented to the emergency department (ED) complaining of fatigue and chest pain without any relevant clinical history. She had no family history of cardiomyopathy or autoimmune disease. Computed tomography (CT) scan ruled out pulmonary embolism but showed right lung pneumonia. Severe left ventricular (LV) systolic dysfunction [LV ejection fraction (LVEF) < 20%] and unobstructed coronary arteries were detected ( Video S1 , 0:05). Despite inotropic support, the patient needed percutaneous veno‐arterial extracorporeal membrane oxygenation (V‐A ECMO) support. After 48 h with no clinical improvement, the patient was referred to our centre. Through a left mini‐thoracotomy in the fifth intercostal space, the cardiac apex was approached for inflow LV assist device (LVAD) implantation, and a myocardial sample was taken for histological analysis. With the use of a right mini‐thoracotomy in the second intercostal space, a vascular prosthesis was anastomosed to the aorta as outflow line. A right ventricular assist device (RVAD) was implanted using the left femoral vein and the pulmonary artery through a left mini‐thoracotomy in the second intercostal space. A diagnosis of virus‐negative lymphocytic myocarditis was made on the basis of EMB (Figure 1A and 1B ). Serum tested weakly positive for anti‐heart and anti‐intercalated disk autoantibodies. Although the diagnosis consisted of a lymphocytic immune‐mediated (virus‐negative) myocarditis with severe systolic dysfunction, the patient was not put on immunosuppression because of pneumonia. She was progressively weaned from RVAD, which was removed after 6 days. Twenty days later, the LVAD was also removed, as a complete LV recovery was achieved. The patient's stay in the intensive care unit (ICU) was prolonged (37 days) owing to nosocomial pneumonia, acute renal failure needing 14 days of continuous veno‐venous haemodialysis, positive blood cultures for Candida utilis and Enterococcus faecium, and presence of Enterovirus on sputum. LVEF was 50% at discharge (102 days). After the first hospitalization, the patient developed an amiodarone‐related thyroid disease and chronic kidney disease for which she was followed up by the respective specialists. She was put on beta‐blocker therapy with carvedilol and aldosterone antagonist. Her newly developed Stage IV chronic kidney disease with a glomerular filtration rate between 15 and 20 mL/min was treated with additional sodium therapy for persistent hyponatremia. Three years later, after being hospitalized owing to severe hyponatremia, aldosterone antagonist administration was suspended. For the subsequent 5 years, the patient was asymptomatic and was followed up with echocardiograms ( Video S1 , 0:15), ECGs, and blood and troponin tests every 6 months.
Figure 1.
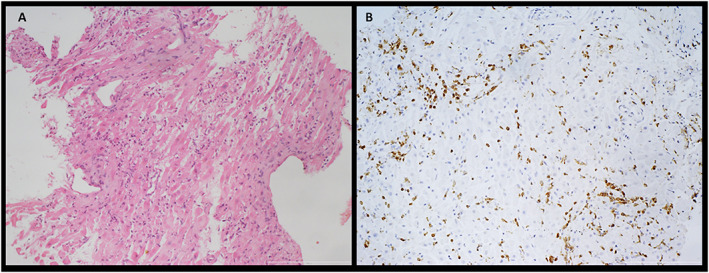
Pathological findings in endomyocardial biopsy (EMB) at first episode. (A) EMB specimen showing extensive myocardial inflammation associated with diffuse myocytes necrosis [hematoxylin and eosin (H&E); scale bar 200 μm]. (B) Strong positivity of immunohistochemistry for T‐lymphocytes (immunostaining anti‐CD3; scale bar 200 μm).
In January 2020, the patient presented several times to the ED complaining of atypical chest pain and fever. ECG was unchanged, and troponin values were repeatedly normal; the echocardiogram also remained consistent ( Video S1 , 0:30). In March, she was re‐admitted to secondary care ED for dyspnoea and palpitations. ECG showed diffuse ST elevation with tombstone morphology; troponin was also markedly increased (peak TnI 83 000 ng/L, normal range 0–34 ng/L) (Figure 2A ). Because she presented during the coronavirus disease 2019 (COVID‐19) outbreak, she underwent a nasopharyngeal swab test for severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), which resulted negative. A bedside echocardiogram showed severe LV dysfunction with healthy coronary arteries ( Video S1 , 0:40). She was then transferred to our institution. On arrival, she developed haemodynamic and electrical instability consisting of an arrhythmic storm and cardiac arrest, requiring emergent femoral–femoral V‐A ECMO. One hour later, following severe haemodynamic instability, we decided to unload the LV by placing an apical venting through the previous left mini‐thoracotomy in the fifth intercostal space; an EMB was again performed at the LV apex. A 4 L/min support was commenced; better organ perfusion was evidenced by lactate reduction and pH improvement. Complex incessant arrhythmias persisted despite i.v. amiodarone, lidocaine, and esmolol administration. The EMB showed a virus‐negative lymphocytic myocarditis (Figure 3A and 3B ). Immunosuppressive therapy with steroids (methylprednisolone, 1 g i.v. bolus OD for the first 3 days, then 100 mg i.v. OD for the first week followed by progressive tapering in the subsequent days) was then immediately started; azathioprine (50 mg per os b.i.d.) was also added. A progressive normalization of ECG and biventricular contractility was observed (Figure 2B ). In the following days, there was a rapid recovery of cardiac function with a decreasing need for mechanical support. VA‐ECMO was removed on the ninth post‐operative day. She was transferred from the ICU on the 13th post‐operative day. Echocardiography at discharge showed mild LV dysfunction (LVEF 48%) ( Video S1 , 1:00). She was discharged home on Day 32, with a maintenance immunosuppressive therapy of oral methylprednisolone and azathioprine. Methylprednisolone was then tapered the following days with a weekly 25% reduction and a target of chronic 5 mg per day. Additionally, she is currently on alternating doses of azathioprine (100 mg per os 1 day and 150 mg the next day). Four weeks after discharge, once the test was introduced in Italy, an immunological assay for SARS‐CoV‐2 IgM and IgG was performed showing a weak positivity for specific antibodies while immunosuppressed.
Figure 2.
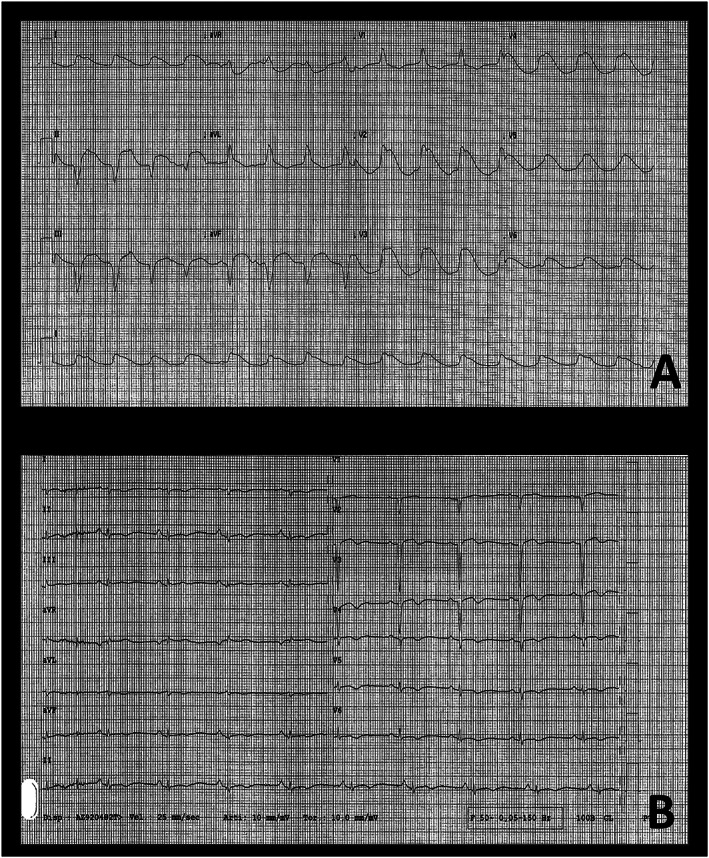
(A) ECG at hospital admission showing a wide QRS complex. (B) ECG at discharge showing a restoration of the sinus rhythm; QRS waves narrowing with diffuse negative T waves; low voltages on all the precordial leads.
Figure 3.
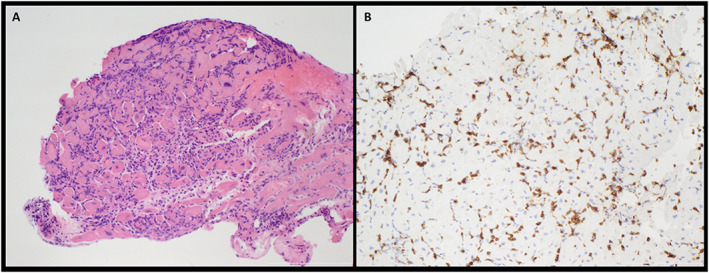
Pathological findings in endomyocardial biopsy (EMB) at recurrent fulminant myocarditis (FM) episode. (A) EMB specimen showing persistent myocardial inflammation associated with diffuse myocytes necrosis [hematoxylin and eosin (H&E); scale bar 200 μm]. (B) Strong positivity of immunohistochemistry for T‐lymphocytes (immunostaining anti‐CD3; scale bar 200 μm).
Discussion
This is the first report to show that lymphocytic virus‐negative FM relapses can be observed in the same patient with a similar presentation severity. Regardless of the MCS used, prompt LV unloading is critical for myocardial recovery; in addition, timely integration of MCS with tailored EMB‐guided immunosuppression was of critical importance in the treatment of our patient. Outcome of lymphocytic FM compared with non‐fulminant disease is controversial, reported as excellent 1 or bad. 2 So far, it is unclear whether the fulminant modality has independent negative prognostic value per se regardless of other known negative predictors such as the histology, giant cell vs. lymphocytic, and the degree of biventricular dysfunction. 2
FM is rare, and fulminant episodes of recurrences have already been reported in literature. 4 , 5 On the basis of serological tests, the aetiology of recurrent myocarditis in cases discussed by Matsue and Yoshimizu et al. is to be considered viral related, missing any EMB in both. In our case, immunohistochemical results of EMBs performed during the acute phase pointed to lymphocytic myocarditis. All serological and molecular tests on the samples obtained were negative for viruses, hence our definition of virus‐negative immune‐mediated lymphocytic myocarditis.
Although this is the first report of recurrent immune‐mediated lymphocytic FM with a fulminant relapse, our specific case keeps in line with the relapsing–remitting course of other autoimmune diseases. 2 In the first episode of FM for our patient, immunosuppression was withheld because of concomitant pneumonia and, after pneumonia resolution, because of the sustained recovery of ventricular function. The long‐lasting asymptomatic state of the patient with preserved biventricular function in the following 5 years confirmed that the first episode was indeed cured. During the strict echocardiographic follow‐up in the time preceding the recurrence, no clinical or instrumental evidence ever suggested the presence of a subclinical myocarditis, justifying the absence of further invasive examinations. The second episode highlights the importance of a timely combined surgical and medical approach; initial high dose i.v. steroids were highly effective in suppressing a life‐threatening arrhythmic storm.
Another interesting feature of this case was the presence of pneumonia as a prodromal event in both FM episodes. We hypothesize that, in patients with a predisposing immunogenetic background, autoimmune disease may be triggered or reactivated by major infections, for example, pneumonia, that may act as adjuvants leading to an immune‐mediated hyper‐response. 2 The patient had a history of pneumonia in the first months of 2020 during the initial spread of the COVID‐19 pandemic in Northern Italy. In the absence of severe symptomatology and the still dormant SARS‐CoV‐2 outbreak, a CT scan was not performed; the patient was discharged home on antibiotic therapy with a community‐acquired pneumonia diagnosis after a chest X‐ray. Nasopharyngeal swabs tests performed during hospitalization were negative, as was EMB‐based analysis of viral activity. It cannot be excluded that an autoimmune inflammatory process was triggered by the pneumonia prodromal episode 2 months prior. Unfortunately, the late introduction (May 2020) of serological assays for SARS‐CoV‐2 in the Italian market delayed our ability to make fully informed decisions regarding the treatment of this patient, who was already undergoing a heavy immunosuppressive regimen with steroid and azathioprine as a relapse maintenance therapy. Regardless, pathology studies up to date have yet to specifically address the myocardium and the burden of myocarditis in COVID‐19 patients, which remain to be established. 6 , 7
Funding
Departmental Strategic Investment (SID) 2020, BIRD205838, University of Padua.
Supporting information
Video S1. Transthoracic‐Echocardiogram 3 days post BiVAD implantation (0:05); Transthoracic‐Echocardiogram at discharge (0:15); Transthoracic‐Echocardiogram 5 years after the first episode (0:30); Transthoracic‐Echocardiogram and Coronary Angiography at admission for recurrent FM (0:40); Transthoracic‐Echocardiogram at discharge (1:00).
Caraffa, R. , Marcolongo, R. , Bottio, T. , Rizzo, S. , Bifulco, O. , Bagozzi, L. , D'Onofrio, A. , Caforio, A. L. P. , Jorgji, V. , Basso, C. , and Gerosa, G. (2021) Recurrent autoimmune myocarditis in a young woman during the coronavirus disease 2019 pandemic. ESC Heart Failure, 8: 756–760. 10.1002/ehf2.13028.
Raphael Caraffa and Renzo Marcolongo equally contributed to this work.
References
- 1. Kociol RD, Cooper LT, Fang JC, Moslehi JJ, Pang PS, Sabe MA, Shah RV, Sims DB, Thiene G, Vardeny O, American Heart Association Heart Failure and Transplantation Committee of the Council on Clinical Cardiology . Recognition and initial management of fulminant myocarditis: a scientific statement from the American Heart Association. Circulation 2020; 141: e69–e92. [DOI] [PubMed] [Google Scholar]
- 2. Caforio AL, Pankuweit S, Arbustini E, Basso C, Gimeno‐Blanes J, Felix SB, Fu M, Heliö T, Heymans S, Jahns R, Klingel K. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J 2013; 34: 2636–2648. [DOI] [PubMed] [Google Scholar]
- 3. Tarzia V, Bortolussi G, Bianco R, Buratto E, Bejko J, Carrozzini M, de Franceschi M, Gregori D, Fichera D, Zanella F, Bottio T, Gerosa G. Extracorporeal life support in cardiogenic shock: impact of acute versus chronic etiology on outcome. J Thorac Cardiovasc Surg 2015; 150: 333–340. [DOI] [PubMed] [Google Scholar]
- 4. Yoshimizu N, Tominaga T, Ito T, Nishida Y, Wada Y, Sohmiya K, Tanaka S, Shibata K, Kanzaki Y, Ukimura A, Morita H, Hoshiga M, Ishizaka N. Repetitive fulminant influenza myocarditis requiring the use of circulatory assist devices. Intern Med 2014; 53: 109–114. [DOI] [PubMed] [Google Scholar]
- 5. Matsue Y, Kumasaka L, Nagahori W, Ohno M, Suzuki M, Matsumura A, Hashimoto Y. A case of fulminant myocarditis with three recurrences and recoveries. Int Heart J 2010; 51: 218–219. [DOI] [PubMed] [Google Scholar]
- 6. Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, Liu S, Zhao P, Liu H, Zhu L, Tai Y, Bai C, Gao T, Song J, Xia P, Dong J, Zhao J, Wang FS. Pathological findings of COVID‐19 associated with acute respiratory distress syndrome. Lancet Respir Med 2020; 8: 420–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Barton LM, Duval EJ, Stroberg E, Ghosh S, Mukhopadhyay S. COVID‐19 autopsies, Oklahoma, USA. Am J Clin Pathol 2020; pii: aqaa062; 153: 725–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video S1. Transthoracic‐Echocardiogram 3 days post BiVAD implantation (0:05); Transthoracic‐Echocardiogram at discharge (0:15); Transthoracic‐Echocardiogram 5 years after the first episode (0:30); Transthoracic‐Echocardiogram and Coronary Angiography at admission for recurrent FM (0:40); Transthoracic‐Echocardiogram at discharge (1:00).


