Abstract
Cancers have always been an intractable problem because of recurrence and drug resistance. In the past few decades, nanoparticles have been explored intensely to diagnose, prevent and treat malignancy due to their good penetrability and better targeting. However, most nanocarriers have poor biodegradation and can be discharged out of the body quickly or cleared by immune cells while failing to obtain effective drug concentration at the specific sites. The emergence of biological membrane encapsulation technology relieves the fast clearance of antitumor drugs and reduces toxicity in vivo. This review will discuss the advantages and disadvantages of several blood cell membrane-coated nanoparticles and further introduce exosome-carried drugs to evidence the promising prospect of biomimetic nanoparticle drug delivery systems.
Keywords: tumor, drug delivery systems, blood cells, biological membranes
Introduction
Recently, the number of people who are suffering from cancer increased rapidly due to environment pollution and unhealthy lifestyle. It has always been an alarming problem for the past several decades around the world. Although the treatment of malignant tumor has developed rapidly, traditional chemotherapy and phototherapy are still the most common methods. However, common chemotherapeutic agents have a few fatal drawbacks in clinical application, such as poor water solubility, low oral bioavailability and serious adverse reactions over therapeutic effect.1 In addition, a series of new problems arise from single or combined therapy, such as recurrence, drug resistance, systemic side effects and so on.
Nontargeted drugs affect the normal cells or organs instead of the disease location. Therefore, the development of suitable carriers that can improve the therapeutic efficacy at specific sites and reduce drug resistance by increasing the accumulation of chemotherapy drugs at the targeted sites to achieve high targeted efficiency and low general toxicity becomes an indispensable need. Under this circumstance, the application of molecular targeted drugs has caught scientists’ attention and they have made a great breakthrough. Recent studies showed that nanoparticles structured smaller than 100 nm in at least one dimension had a tremendous potential as drug carriers due to their small size and unique physicochemical and biological properties that make them an appealing material for biomedical applications.2 Nanoparticle drug delivery systems are widly researched in medical treatment, including a large variety of forms like liposomes, polymer nanoparticles, solid lipid nanoparticles, hybrid nanoparticles, biomimetic nanoparticles, and so on.3 Compared with traditional treatments, nanoscale drug carriers have the advantages of good penetrability, strong targeting, and long-acting time. Nanoparticles are continuously engineered and perform the potential to transform the diagnosis, prevention and treatment of difficult-to-treat diseases such as cancer, Alzheimer’s disease, stroke, and diabetes.4–6 However, the development of functional nanoparticles is still limited by its nature. Liposomes, metal nanoparticles and polymer nanomaterials are the most commonly used nanocarriers. While most liposomes can only carry hydrophilic drugs and be discharged out of the body quickly the latter two have poor biodegradation as a result that they are easily retained in liver and kidney tissues to cause toxic damage, and it is difficult to obtain effective drug concentration at the specific sites.
Under the circumstances, biological drug delivery systems such as albumin, erythrocytes, and platelets with the advantages of nontoxic and immunogenicity, innate biocompatibility, large drug loading, and high targeting have come into being and have been proposed to play an important role in tumor treatment. This article reviews some biocompatible and biodegradable nanoparticles used in cancer administration, which includes not only biological membrane like hemocyte, but also some synthetic polymeric nanoparticles (Table 1), from the best synthetic polymeric nanoparticles PLGA to the combination of nature cell membranes NPs, to achieve a feasible precision medicine for tumor therapeutic applications.
Table 1.
Examples of Nanoparticles and Therapeutic Moieties Loaded by Erythrocyte/Platelet/Leukocyte/Exosome in Various vitro and vivo Tumor Models
| Coated Membranes | Inner Cores | Therapeutic Moieties | Applications | References |
|---|---|---|---|---|
| Erythrocyte | DSPE-PEG | Paclitaxel | Chemotherapy for gastric cancer | 29 |
| CuS | Doxorubicin | Synergistic photo-chemotherapy for melanoma | 30 | |
| - | 1,2‐diaminocyclohexane‐platinum (II) and ICG | Synergistic photo-chemotherapy | 31 | |
| PCEC | IR780 iodide and docetaxel | Photo-chemotherapy for breast cancer | 32 | |
| Platelet | PLGA | MRI contrast agent | Detection of atherosclerosis | 4 |
| PLGA | Bufalin | Chemotherapy for hepatic carcinoma | 23 | |
| PLGA | Docetaxel | Coronary restenosis | 35 | |
| – | Adriamycin | Chemotherapy for lymphoma | 36 | |
| Gold nanorods | - | Photothermal therapy for squamous cell carcinoma | 37 | |
| ZrO2 NPs | Cervical cancer | 38 | ||
| Leukocyte | PLGA | Doxorubicin | Glioma | 40 |
| Silica nanoparticles | Doxorubicin | Breast cancer | 41 | |
| Exosome | Silicon nanoparticles | Doxorubicin | Chemotherapy for hepatocarcinoma, breast cancer, lung metastasis tumor | 45 |
| Copper-cysteamine nanoparticles | – | Photothermal therapy for hepatocarcinoma | 51 | |
| – | Doxorubicin | Chemotherapeutic for osteosarcoma | 52 |
PLGA-based Nanoparticles
Poly (lactic-co-glycolic acid) (PLGA) has been one of the most studied polymeric carriers approved by the FDA for anticancer therapy because of its low systemic toxicity and high biodegradability compared to other polymeric systems.7 As a controlled-release formulation of drugs,8 drug molecules in NPs are slowly released from the pores of the material surface as the PLGA degrades, as a result, the drugs maintain a constant concentration for a long time, prolong the exposure time, and improve the bioavailability.9 What is more, another attractive characteristic of PLGA over other nanoparticles is that PLGA is one of the best characterized biodegradable copolymers because it decomposes into nontoxic lactic acid and glycolic acid and further into H2O and CO2 eliminated from the body with low to no toxicity.10,11 According to all these advantages of PLGA NPs, are extensively used in a variety of fields, for example, PLGA NPs loaded with corresponding therapeutic drugs can cross the blood–brain barrier and reach the central nervous system.12
In addition to the intrinsic properties of PLGA NPs, incorporating targeting ligands, such as small molecules, peptides, antibodies, and aptamers onto their surface make them better with respect to targeting strategy, biocompatibility, and preferential accumulation.10,13 Zheng et al verified co-delivery of sorafenib and metapristone by the LFC131-conjugated (a peptide inhibitor of CXCR4) PLGA NPs showed prolonged circulation and target accumulation at tumor sites, and thus suppressed tumor growth in HCC models.14 Byeon et al developed HA-labeled PLGA NPs (HA-PLGA NPs) incorporating both PTX and FAK siRNA as a two-in one delivery system to increase the efficiency of targeted delivery against tumor-specific receptors and to enhance therapeutic efficacy in drug-resistant ovarian cancer.15
In comparison to monotherapy, anticancer drugs encapsulated in PLGA nanoparticles show good biocompatibility, strong cytotoxicity, significant antitumor activity and minimal systemic toxicity.11,15 Co-encapsulation of two drugs to the tumor via single nanoparticles could better maintain the synergistic drug effect in vivo than the co-administration of two single drugs and drug-carried nanoparticles.16 What is more, as a kind of biodegradable organic polymer, PLGA has good modifiability.
Biofilm Nanoparticles
Cell membrane camouflaged nanoparticles have been exploited as drug-delivery carriers for several decades because of the improvement of the targeting efficiency and retention of carried drugs. Originally, the initial cell membrane-based nanoparticles (CMBNPs) were fabricated from a red blood cell membrane shell and PLGA core through a co-extrusion process, forming a core-shell structure.17 Subsequently, all kinds of cell membranes, such as platelets, albumin, cancer cells, and exosome vesicles, have been exploited as carriers to carry various drugs in different fields.18–21 There were three basic strategies for the development of biomimetic nanoparticles: (1) synthetic NPs modified with targeting ligands that mimic cell surface proteins, (2) cell membrane-coated NPs, and (3) liposomes engineered with cell membrane proteins.22
Though the retention time of drug improves after PEG-modified NPs, the immune response to synthetic materials still concerns researchers, as well as that the most synthetic nanoparticles have poor bioavailability which lead to low accumulation and quick excretion in vivo13. Furthermore, simple surface functionalization methods cannot accurately simulate the complex interfaces that exist in nature, and finally NPs will be recognized as foreign bodies and cannot completely escape subsequent immune response.23 Under this circumstance, scientists turn their interest to natural cells, which are the fundamental units in biosome.24 Cells perform specific and basic tasks through different significant biomacromolecules, which are embedded into cell membranes, a lipid bilayer equipped with a collection of biomacromolecules.25 Cell membranes are able to control the physical interactions between each other, like regulating immune functions, receiving signals, and anchoring binding interactions.25,26 Take erythrocytes as an example, nonnuclear, abundant, long half-life (up to 120 days in blood circulation), all these key advantages made RBC membrane-coated NPs the hottest carrier to deliver various chemotherapeutics.27
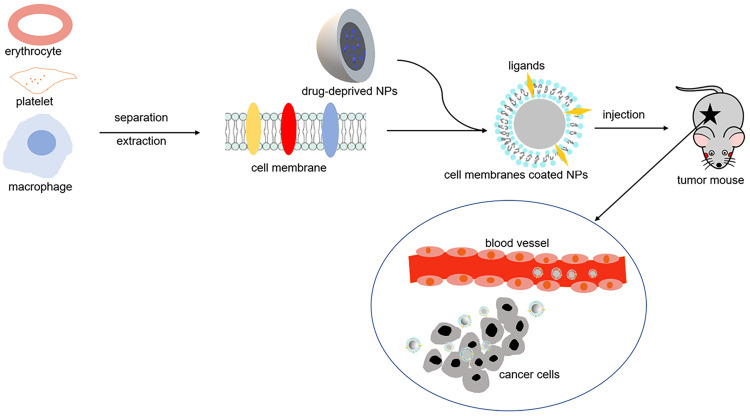
Cell membrane coating retains the complex composition of the entire cell surface on the nanoparticle, bypassing the necessary for complicated chemistry and the identification of individual membrane components. Blood cells are the most used membranes to envelop NPs, (Figure 1), along with a popular new-born carrier, exosomes. On account of the combined advantages of both synthetic nanoparticle cores and natural cell membranes, biofilm nanoparticles have gained increasing attention in precise molecular drug delivery in cancer.3
Figure 1.
Schematic illustration of erythrocyte/platelet/macrophage membrane-coated nanoparticles for tumor therapy in tumor-bearing mice.
Erythrocyte Membranes Coated NPs (RBCNPs)
In the realm of tumor diagnosis and therapy, nanoparticles have revealed promising achievements with high penetration and targeting. But the short drug accumulation time, low dose in tumor tissues, and immune elimination as a foreign body are subsequent problems. Under the circumstance, the blood membrane enveloped nanoparticles emerge.
As the first studied drug coating biological membrane, the research of red blood cells as nanofilms has a long history. Erythrocytes are the most numerous blood cell up to fvie billion per milliliter in human circulation.28 This feature guarantees a huge material bank package for nanodrugs. Furthermore, without nucleus and organelles, mature RBC membranes are advantageous for extraction and purification. The unique double concave discoid shape provides RBCs a larger superficial area to carry other cargoes, such as oxygen and functional proteins. It has been proved that combining associated proteins and other elements membranes enhanced the targeting and penetration capabilities of core anticancer drugs.29 Meanwhile, drug accumulation intensity in tumor is much stronger than that of normal tissues in RBCNPs when contrasted with control groups, and thus showing better inhibition of tumor growth.30
CD47, as the self-marker protein on RBC surfaces, interact with signal-regulatory protein α (SIRPα) expressed by macrophages through sending signal “no eating me”. Finally, RBCNPs also improve the immune-evading capability and effectually avoid uptake by immune cells when compared with bare NPs.31 Last but not least, erythrocytes have a much longer life span for about 120 days in circulation. In comparison to synthetic encapsulation, nanoparticles encapsulated with RBC membranes relatively possess longer circulation and retention time.32
In other words, huge quantity, unique construction, long lifespan, along with escaping the immune system, contribute to the particular superiority of an erythrocyte-coated drug delivery system, which also accounts for the hot extensive research into erythrocytes camouflaged nanoparticles.
Platelet Membranes Coated NPs (PNPs)
As a natural ingredient in blood circulation, platelets are nuclear-free fragments generated by megakaryocytes in bone marrow in adults. Like erythrocytes they are nonnuclear and their small size enables them to be extracted relatively easily. Due to more receptors on the surface, platelets show more complexity and multifactorial functionality. They are able to avoid phagocytic uptake by macrophages. Platelets exist in lots of physiological and pathological processes such as wound healing, inflammatory reaction, thrombosis, and organ transplantation rejection. Studies show that they also play an important role in tumors as a result of the interaction with many receptors in tumor cell membranes,33 for example, platelets participate in tumor metastasis and neovascularization, moreover, tumor cells induce platelet is aggregation which known as TCIPA. Platelets have membrane protein P-selectin to mediate the binding of platelets to CD44 on tumor cells,34 which endows PNPs particular functionality to CD44 high expression tumors.
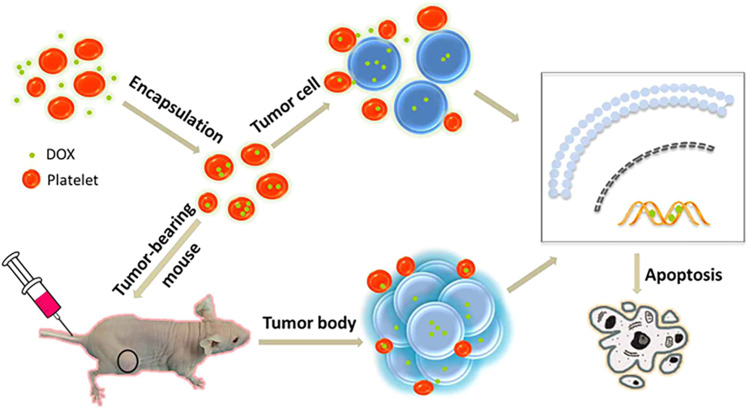
Owing to the advantages of natural affinity to tumor cells, platelet membranes have inspired the design of many functional nanocarriers. In the area of tumor targeted therapy, researchers demonstrated that anticancer drugs could be incorporated into nano-polymeric cores, and these drug-loaded nanoparticles manifested considerable efficacy in tumor mouse models.23 Hu et al adopted a cell membrane cloaking technique to prepare PNPs, whose final size were slightly larger about 15 nm than the bare NPs. And compared to bare NPs and RBCNPs, the platelets coated NPs showed significantly enhanced permeation and retention effect in vivo.35 Coating with natural platelet membrane, PNPs are capable of navigating through circulation and distributing to diseased tissue preferentially rather than healthy position.4 Xu et al used platelets to transport doxorubicin (DOX) to treat lymphoma and they found DOX-loaded with platelets targeted cancer cells well through the phenomenon “TCIPA” (Figure 2), and the growth inhibition of cancer cells was strengthened while the cardiotoxicity of DOX was weakened.36 In addition, Rao et al combined photothermal therapy with tumor cells targeted platelets delivery system, which could subsequently damage the tumor tissues and accumulate the PNPs.37 Compared to uncoated particles, the platelet membrane-cloaked nanoparticles have reduced cellular uptake by macrophage-like cells, thus reducing their clearance and extending the circulation time.35,38 Introducing additional elements onto the outer surface of NPs to add extra functionality via polymer tethers enable anticancer drug to be most absorbed and utilized by targeted tissues, and further improve the common advantages of platelets and traditional synthetic nanoparticles.
Figure 2.
Schematic illustration of the mechanism of enhanced anticancer activity of DOX-platelet through “tumor cell-induced platelet aggregation”.
Note: Reproduced from Xu P, Zuo H, Chen B, et al. Doxorubicin-loaded platelets as a smart drug delivery system: an improved therapy for lymphoma. Sci Rep. 2017;7:42632. Creative Commons License and Disclaimer Available from: http://creativecommons.org/licenses/by/4.0/legalcode .36
All results showed that drug-loaded PNPs gave an efficacious chemotherapeutic treatment and effectively inhibited the growth of carcinoma, presenting the unique self-reinforcing characteristic of this delivery system in the treatment of cancer.
Leukocyte Membranes Coated NPs (LNPs)
Leukocytes (white blood cells), including granulocytes, lymphocytes and monocytes, which belong to the immune system, have larger volumes than RBCs because of their nucleus. Inflammation, which is regulated by WBCs, is closely related to the tumor microenvironment. The leukocytes participated in neovascularization, metastasis and progress of tumor through the interaction with all kinds of cytokines, chemokines and proteins between tumor cells, such as TNF-α, RANKL which is called leukocyte infiltration.39
Macrophages have drawn the most attention among all the leukocytes to be designed as the coats of nanoparticles in recent years.40 Coated with macrophage membranes, NPs own the ability to easily migrate between blood vessels and other extravascular tissues as well as macrophages. Besides, macrophages naturally phagocytose malignant cells and decrease fibrosis. It has been proved that compared to conventional NPs, the macrophage membrane-coated ones (MNPs) can effectively transport anticancer drugs to specific sites and achieve prominent accumulation time with a controlled release effect.41 The WBC membranes also act against opsonization and reticuloendothelial system (RES) clearance which serves as a tumor-homing navigator to enhance tumor accumulation.42 As a biofilm nanoparticle, macrophage derived NPs reveal excellent biocompatibility and immune evasion ability via CD47 embedded in membranes.
However, imperfectly as karyocytes, compared with RBCs and platelets, the extraction and purification of leukocytes are more complex. In addition, the main histocompatibility complex (MHC) molecules expressed on its exterior may lead to incompatibility. Irrespective of its shortcoming, the targeting and regulating ability on tumor and inflammation of WBC make it a promising candidate for the encapsulation of NPs.
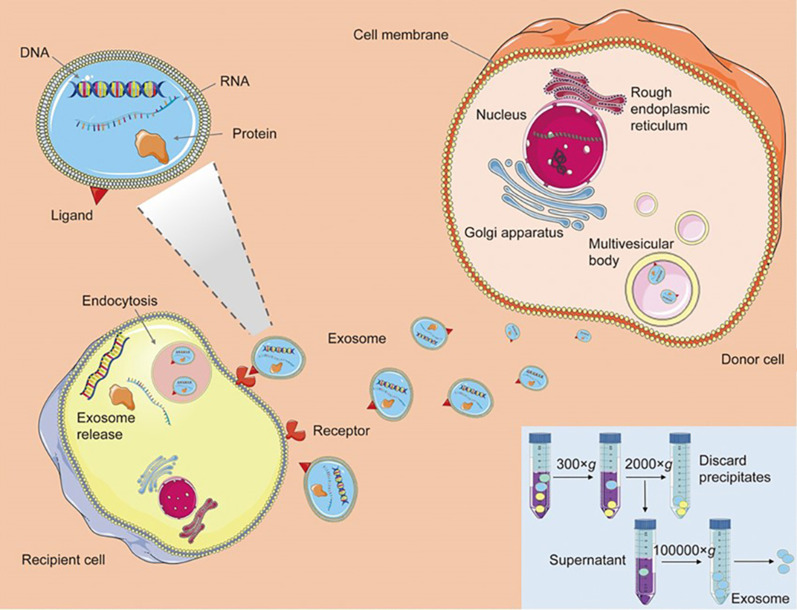
Exosomes Based NPs
Exosomes are nanosized (30–120 nm) membrane vesicles excreted by various types of cells which are acting as a mean of long-distance intercellular communication and biomaterial transfers without cell-to-cell contact.25,43 What cannot be ignored is that exosomes originated from inward budding of membrane of multivesicular bodies and are released from the cells into the extracellular environment with the plasma membrane44 (Figure 3), therefore, a broad kind of cargo on cell membranes of the parent cells are contained in exosomes, including nucleic acids, proteins and enzymes.45 Researchers demonstrate that exosomes are associated with several hallmark features of cancers, including stimulating tumor angiogenesis, rebuilding the stroma to establish the tumor microenvironment, as well as facilitating tumor growth and drug resistance by the means of horizontal transfer of genetic information between cancer cells.46
Figure 3.
Schematic illustration of generation, release and cargo transfer of exosomes.
Note: Reprinted by permission from Springer Nature. Acta Pharmacologica Sinica. Engineering exosomes as refined biological nanoplatforms for drug delivery. Luan X, Sansanaphongpricha K, Myers I, Chen H, Yuan H, Sun D. 2017;38(6):754–763. Copyright © 2017.20
The therapeutic application of exosomes is promising because injected exosomes are effectively entering other cells with minimal immune clearance and repeated injections are well tolerated without substantial side effects.44,47,48 It is worth noting that exosomes are enriched with transmembrane protein and adhesion proteins, and also specific protein receptors, therefore, protein cargoes on exosomes can be transported to and receipted by targeted cells effectively to induce cellular responses, such as the inducing and promoting of neoplasia.49 In addition, exosomes present an excellent capacity to escape the clearance by immune system depending on protein CD47, which is a widely expressed integrin associated transmembrane protein that functions in part to protect cells from phagocytosis.50 Inspired from these advantages, exosomes are engineered as effective vehicles for therapeutics. Huang et al found that in photodynamic therapy, the soluble nanodrugs were able to enter exosomes secreted by tumor cells, and supposed that exosomes could be used to deliver drugs to target pancreatic cells.51
Of particular concern, additional characters of exosomes in delivering functional cargos to diseased cells also favor their use as drug deliveries. The lipid and protein composition and other natural constituents of exosomes play a role in enhanced bioavailability and in minimizing adverse reactions, suggesting that biocompatibility is guaranteed and systemic toxicity does not need to be taken into consideration when compared with artificial chemical delivery vehicles. By comparison with free chemotherapeutics, the exosome-loaded ones can kill tumor cells more effectively and show low cytotoxicity in myocardial cells and other healthy tissues.52 Once nanoparticle-loaded exosomes are generated, they will be preferentially captured by the same cell line. Therefore, specific exosome-based transports are preferentially transferred to typical cell types but not to others.53
While as a distinct type of nanocarrier, already carrying numerous proteins and nucleic acids by their nature, exosomes relatively fail to achieve high loading capacity.43 Moreover, the successful modification, purification and analytical procedures require more exploration.20,54 In general, exosomes are extracellular membrane-derived vesicles derived from most cell types, which can be engineered to deliver diverse therapeutic payloads as worthwhile nanocarriers.
Conclusion
With the advantages of harmless degradation products, synthetic PLGA NPs have been functionalized with targeted peptides or other functional groups to increase the capacity of targeting delivery of anticancer drugs to tumors. And co-delivery of multiple drugs in a single nanocarrier shows a better synergistic drug effect and lower side effects than simple combined administration, thus the recurrence and drug resistance rates drop considerably.
However, there are still a few drawbacks limiting synthetic NPs to meet clinical expectation used on patients. As a drug delivery system, nanoparticles are transported to their target tissues via blood environment, thus the compatibility of engineered NPs with blood constituents must be taken into consideration with extreme care. Scientists found that PLGA NPs could result in the damage and premature elimination of erythrocytes because they accelerate the clearance of blood cells in the way of the alteration of cells’ functionality, mechanical properties and integrity.6 Blood cell membrane-coated nanoparticles have the capability to overcome these problems like immune elimination. Both in vitro and vivo, cell membrane-coated NPs have significantly enhanced the retention of drugs and retained cytotoxicity toward carcinoma. In fact, natural biofilm-based nanoparticles are equipped with the capability to unite advantages of both synthetic nanocarriers and cell-mediated drug delivery. They possess low immunogenicity which is able to avoid the rapid clearance and low toxicity to effectively spare healthy cells when compared with non-natural vehicles. Biofilm nanoparticles display prolonged circulation and preferential targeting to disease tissues which enhance tumor-targeting property of chemotherapeutics to malignant tumors. Although the development of nanomedicine has been studied for a long time, few clinical applications are available. The request of efficient and safety materials to deliver drugs and the potential additional risk on human health are challenges demanding prompt solution.
In conclusion, with the rapid development of encapsulation skills, bionanoparticles that combine the unique functionalities of natural biomaterials, such as cell membranes or membrane vesicles have recently increased considerable attention as effective drug delivery platforms.
Acknowledgments
This work was supported by the Jiangsu Social Development Project (Project No. BE 2018711), Southeast University Project (Project No. 2018yy-jccx003), the Key Medical Projects of Jiangsu Province (BL2014078), the Key Department of Jiangsu Province (2016–2020).
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Li S, Li X, Ding J, Han L, Guo X. Anti-tumor efficacy of folate modified PLGA-based nanoparticles for the co-delivery of drugs in ovarian cancer. Drug Des Devel Ther. 2019;13:1271–1280. doi: 10.2147/DDDT.S195493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilczewska AZ, Niemirowicz K, Markiewicz KH, Car H. Nanoparticles as drug delivery systems. Pharmacol Rep. 2012;64(5):1020–1037. [DOI] [PubMed] [Google Scholar]
- 3.Jin K, Luo Z, Zhang B, Pang Z. Biomimetic nanoparticles for inflammation targeting. Acta Pharm Sin B. 2018;8(1):23–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wei X, Ying M, Dehaini D, et al. Nanoparticle functionalization with platelet membrane enables multifactored biological targeting and detection of atherosclerosis. ACS Nano. 2018;12(1):109–116. doi: 10.1021/acsnano.7b07720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rong X, Ji Y, Zhu X, et al. Neuroprotective effect of insulin-loaded chitosan nanoparticles/PLGA-PEG-PLGA hydrogel on diabetic retinopathy in rats. Int J Nanomedicine. 2019;14:45–55. doi: 10.2147/IJN.S184574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de la Harpe KM, Kondiah PPD, Choonara YE, Marimuthu T, Du Toit LC, Pillay V. The hemocompatibility of nanoparticles: a review of cell-nanoparticle interactions and hemostasis. Cells. 2019;8(10):1209. doi: 10.3390/cells8101209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Surendran SP, Moon MJ, Park R, Jeong YY. Bioactive nanoparticles for cancer immunotherapy. Int J Mol Sci. 2018;19:12. doi: 10.3390/ijms19123877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhong Y, Su T, Shi Q, et al. Co-administration of iRGD enhances tumor-targeted delivery and anti-tumor effects of paclitaxel-loaded PLGA nanoparticles for colorectal cancer treatment. Int J Nanomedicine. 2019;14:8543–8560. doi: 10.2147/IJN.S219820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Duan T, Xu Z, Sun F, et al. HPA aptamer functionalized paclitaxel-loaded PLGA nanoparticles for enhanced anticancer therapy through targeted effects and microenvironment modulation. Biomed Pharmacother. 2019;117:109121. doi: 10.1016/j.biopha.2019.109121 [DOI] [PubMed] [Google Scholar]
- 10.Rezvantalab S, Drude NI, Moraveji MK, et al. PLGA-based nanoparticles in cancer treatment. Front Pharmacol. 2018;9:1260. doi: 10.3389/fphar.2018.01260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gao J, Liu J, Xie F, Lu Y, Yin C, Shen X. Co-delivery of docetaxel and salinomycin to target both breast cancer cells and stem cells by PLGA/TPGS nanoparticles. Int J Nanomedicine. 2019;14:9199–9216. doi: 10.2147/IJN.S230376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rigon L, Salvalaio M, Pederzoli F, et al. Targeting brain disease in MPSII: preclinical evaluation of IDS-loaded PLGA nanoparticles. Int J Mol Sci. 2019;20:8. doi: 10.3390/ijms20082014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Luk BT, Zhang L. Cell membrane-camouflaged nanoparticles for drug delivery. J Control Release. 2015;220(Pt B):600–607. doi: 10.1016/j.jconrel.2015.07.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zheng N, Liu W, Li B, et al. Co-delivery of sorafenib and metapristone encapsulated by CXCR4-targeted PLGA-PEG nanoparticles overcomes hepatocellular carcinoma resistance to sorafenib. J Exp Clin Cancer Res. 2019;38(1):232. doi: 10.1186/s13046-019-1216-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Byeon Y, Lee JW, Choi WS, et al. CD44-targeting PLGA nanoparticles incorporating paclitaxel and FAK siRNA overcome chemoresistance in epithelial ovarian cancer. Cancer Res. 2018;78(21):6247–6256. [DOI] [PubMed] [Google Scholar]
- 16.Dai W, Wang X, Song G, et al. Combination antitumor therapy with targeted dual-nanomedicines. Adv Drug Deliv Rev. 2017;115:23–45. doi: 10.1016/j.addr.2017.03.001 [DOI] [PubMed] [Google Scholar]
- 17.Li R, He Y, Zhang S, Qin J, Wang J. Cell membrane-based nanoparticles: a new biomimetic platform for tumor diagnosis and treatment. Acta Pharm Sin B. 2018;8(1):14–22. doi: 10.1016/j.apsb.2017.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.An FF, Zhang XH. Strategies for preparing albumin-based nanoparticles for multifunctional bioimaging and drug delivery. Theranostics. 2017;7(15):3667–3689. doi: 10.7150/thno.19365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kroll AV, Fang RH, Zhang L. Biointerfacing and applications of cell membrane-coated nanoparticles. Bioconjug Chem. 2017;28(1):23–32. doi: 10.1021/acs.bioconjchem.6b00569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Luan X, Sansanaphongpricha K, Myers I, Chen H, Yuan H, Sun D. Engineering exosomes as refined biological nanoplatforms for drug delivery. Acta Pharmacol Sin. 2017;38(6):754–763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li SP, Lin ZX, Jiang XY, Yu XY. Exosomal cargo-loading and synthetic exosome-mimics as potential therapeutic tools. Acta Pharmacol Sin. 2018;39(4):542–551. doi: 10.1038/aps.2017.178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khodabandehlou K, Masehi-Lano JJ, Poon C, Wang J, Chung EJ. Targeting cell adhesion molecules with nanoparticles using in vivo and flow-based in vitro models of atherosclerosis. Exp Biol Med (Maywood). 2017;242(8):799–812. doi: 10.1177/1535370217693116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang H, Wu J, Williams GR, et al. Platelet-membrane-biomimetic nanoparticles for targeted antitumor drug delivery. J Nanobiotechnology. 2019;17(1):60. doi: 10.1186/s12951-019-0494-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de la Torre P, Pérez-Lorenzo MJ, Alcázar-Garrido Á, Flores AI. Cell-based nanoparticles delivery systems for targeted cancer therapy: lessons from anti-angiogenesis treatments. Molecules. 2020;25:3. doi: 10.3390/molecules25030715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fang RH, Jiang Y, Fang JC, Zhang L. Cell membrane-derived nanomaterials for biomedical applications. Biomaterials. 2017;128:69–83. doi: 10.1016/j.biomaterials.2017.02.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wu M, Le W, Mei T, et al. Cell membrane camouflaged nanoparticles: a new biomimetic platform for cancer photothermal therapy. Int J Nanomedicine. 2019;14:4431–4448. doi: 10.2147/IJN.S200284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xia Q, Zhang Y, Li Z, Hou X, Feng N. Red blood cell membrane-camouflaged nanoparticles: a novel drug delivery system for antitumor application. Acta Pharm Sin B. 2019;9(4):675–689. doi: 10.1016/j.apsb.2019.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sun Y, Su J, Liu G, et al. Advances of blood cell-based drug delivery systems. Eur J Pharm Sci. 2017;96:115–128. doi: 10.1016/j.ejps.2016.07.021 [DOI] [PubMed] [Google Scholar]
- 29.Chen H, Sha H, Zhang L, et al. Lipid insertion enables targeted functionalization of paclitaxel-loaded erythrocyte membrane nanosystem by tumor-penetrating bispecific recombinant protein. Int J Nanomedicine. 2018;13:5347–5359. doi: 10.2147/IJN.S165109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang D, Dong H, Li M, et al. Erythrocyte-cancer hybrid membrane camouflaged hollow copper sulfide nanoparticles for prolonged circulation life and homotypic-targeting photothermal/chemotherapy of melanoma. ACS Nano. 2018;12(6):5241–5252. doi: 10.1021/acsnano.7b08355 [DOI] [PubMed] [Google Scholar]
- 31.Liu W, Ruan M, Wang Y, et al. Light-triggered biomimetic nanoerythrocyte for tumor-targeted lung metastatic combination therapy of malignant melanoma. Small. 2018;14(38):e1801754. doi: 10.1002/smll.201801754 [DOI] [PubMed] [Google Scholar]
- 32.Yang Q, Xiao Y, Yin Y, Li G, Peng J. Erythrocyte membrane-camouflaged IR780 and DTX coloading polymeric nanoparticles for imaging-guided cancer photo-chemo combination therapy. Mol Pharm. 2019;16(7):3208–3220. doi: 10.1021/acs.molpharmaceut.9b00413 [DOI] [PubMed] [Google Scholar]
- 33.Lavergne M, Janus-Bell E, Schaff M, Gachet C, Mangin PH. Platelet integrins in tumor metastasis: do they represent a therapeutic target? Cancers (Basel). 2017;9:10. doi: 10.3390/cancers9100133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhai Y, Su J, Ran W, et al. Preparation and application of cell membrane-camouflaged nanoparticles for cancer therapy. Theranostics. 2017;7(10):2575–2592. doi: 10.7150/thno.20118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hu CM, Fang RH, Wang KC, et al. Nanoparticle biointerfacing by platelet membrane cloaking. Nature. 2015;526(7571):118–121. doi: 10.1038/nature15373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xu P, Zuo H, Chen B, et al. Doxorubicin-loaded platelets as a smart drug delivery system: an improved therapy for lymphoma. Sci Rep. 2017;7:42632. doi: 10.1038/srep42632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rao L, Bu LL, Ma L, et al. Platelet-facilitated photothermal therapy of head and neck squamous cell carcinoma. Angew Chem Int Ed Engl. 2018;57(4):986–991. doi: 10.1002/anie.201709457 [DOI] [PubMed] [Google Scholar]
- 38.Shang Y, Wang Q, Li J, et al. Platelet-membrane-camouflaged zirconia nanoparticles inhibit the invasion and metastasis of hela cells. Front Chem. 2020;8:377. doi: 10.3389/fchem.2020.00377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Deng G, Sun Z, Li S, et al. Cell-membrane immunotherapy based on natural killer cell membrane coated nanoparticles for the effective inhibition of primary and abscopal tumor growth. ACS Nano. 2018;12(12):12096–12108. doi: 10.1021/acsnano.8b05292 [DOI] [PubMed] [Google Scholar]
- 40.Pang L, Qin J, Han L, et al. Exploiting macrophages as targeted carrier to guide nanoparticles into glioma. Oncotarget. 2016;7(24):37081–37091. doi: 10.18632/oncotarget.9464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xuan M, Shao J, Dai L, He Q, Li J. Macrophage cell membrane camouflaged mesoporous silica nanocapsules for in vivo cancer therapy. Adv Healthc Mater. 2015;4(11):1645–1652. doi: 10.1002/adhm.201500129 [DOI] [PubMed] [Google Scholar]
- 42.Zhang Y, Cai K, Li C, et al. Macrophage-membrane-coated nanoparticles for tumor-targeted chemotherapy. Nano Lett. 2018;18(3):1908–1915. doi: 10.1021/acs.nanolett.7b05263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Batrakova EV, Kim MS. Using exosomes, naturally-equipped nanocarriers, for drug delivery. J Control Release. 2015;219:396–405. doi: 10.1016/j.jconrel.2015.07.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kalluri R, LeBleu VS. The biology, function, and biomedical applications of exosomes. Science. 2020;367:6478. doi: 10.1126/science.aau6977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yong T, Zhang X, Bie N, et al. Tumor exosome-based nanoparticles are efficient drug carriers for chemotherapy. Nat Commun. 2019;10(1):3838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jia Y, Chen Y, Wang Q, et al. Exosome: emerging biomarker in breast cancer. Oncotarget. 2017;8(25):41717–41733. doi: 10.18632/oncotarget.16684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fitts CA, Ji N, Li Y, Tan C. Exploiting exosomes in cancer liquid biopsies and drug delivery. Adv Healthc Mater. 2019;8(6):e1801268. doi: 10.1002/adhm.201801268 [DOI] [PubMed] [Google Scholar]
- 48.Liao W, Du Y, Zhang C, et al. Exosomes: the next generation of endogenous nanomaterials for advanced drug delivery and therapy. Acta Biomater. 2019;86:1–14. doi: 10.1016/j.actbio.2018.12.045 [DOI] [PubMed] [Google Scholar]
- 49.Shao H, Im H, Castro CM, Breakefield X, Weissleder R, Lee H. New technologies for analysis of extracellular vesicles. Chem Rev. 2018;118(4):1917–1950. doi: 10.1021/acs.chemrev.7b00534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kamerkar S, LeBleu VS, Sugimoto H, et al. Exosomes facilitate therapeutic targeting of oncogenic KRAS in pancreatic cancer. Nature. 2017;546(7659):498–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Huang X, Wan F, Ma L, et al. Investigation of copper-cysteamine nanoparticles as a new photosensitizer for anti-hepatocellular carcinoma. Cancer Biol Ther. 2019;20(6):812–825. doi: 10.1080/15384047.2018.1564568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wei H, Chen J, Wang S, et al. A nanodrug consisting of doxorubicin and exosome derived from mesenchymal stem cells for osteosarcoma treatment in vitro. Int J Nanomedicine. 2019;14:8603–8610. doi: 10.2147/IJN.S218988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sancho-Albero M, Navascués N, Mendoza G, et al. Exosome origin determines cell targeting and the transfer of therapeutic nanoparticles towards target cells. J Nanobiotechnology. 2019;17(1):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Morishita M, Takahashi Y, Matsumoto A, Nishikawa M, Takakura Y. Exosome-based tumor antigens-adjuvant co-delivery utilizing genetically engineered tumor cell-derived exosomes with immunostimulatory CpG DNA. Biomaterials. 2016;111:55–65. doi: 10.1016/j.biomaterials.2016.09.031 [DOI] [PubMed] [Google Scholar]