Abstract
Background:
Relaxation, biofeedback, and cognitive behavioral therapy are evidence-based behavioral therapies for migraine. Despite such efficacy, research shows that only about half of patients initiate behavioral therapy recommended by their headache specialists.
Objective:
Motivational interviewing (MI) is a widely used method to help patients explore and overcome ambivalence to enact positive life changes. We tested the hypothesis that telephone-based MI would improve initiation, scheduling, and attending behavioral therapy for migraine.
Methods:
Single-blind randomized controlled trial comparing telephone-based MI to treatment as usual (TAU). Participants were recruited during their appointments with headache specialists at two sites of a New York City medical center. Inclusion criteria: ages 16 to 80, migraine diagnosis by UCNS certified headache specialist, and referral for behavioral therapy for prevention in the appointment of recruitment. Exclusion criteria: having done behavioral therapy for migraine in the past year. Participants in the MI group received up to 5 MI calls. TAU participants were called after 3 months for general follow-up data. The pre-specified primary outcome was scheduling a behavioral therapy appointment, and secondary outcomes were initiating and attending a behavioral therapy appointment.
Results:
76 patients were enrolled and randomized (MI=36, TAU=40). At baseline, the mean number of headache days was 12.0±9.0. Self-reported anxiety was present for 36/52 (69.2%) and depression for 30/52 (57.7%). Follow up assessments were completed for 77.6% (59/76, MI= 32, TAU=27). The mean number of MI calls per participant was 2.69±1.56 [0 to 5]. There was a greater likelihood of those in the MI group to initiating an appointment (22/32, 68.8% vs. 11/27, 40.7%, p=0.0309). There were no differences in appointment scheduling or attendance. Reasons stated for not initiating behavioral therapy were lack of time, lack of insurance/funding, prioritizing other treatments, and travel plans.
Conclusions:
Brief telephone based MI may improve rates of initiation of behavioral therapy for migraine, but other barriers appear to lessen the impact on scheduling and attending behavioral therapy appointments.
Keywords: progressive muscle relaxation, cognitive behavioral therapy, biofeedback, adherence, behavioral therapy
Introduction:
There are safe and well tolerated level A evidence-based migraine preventive treatments such as biofeedback, cognitive behavioral therapy (CBT) and relaxation. 1 These therapies have long lasting benefits. 2 However, there are challenges to getting patients to utilize these recommended treatments. 3 Previously, we conducted a study (N=234) which found that only 56% of those referred by a headache specialist for behavioral therapy for migraine prevention initiated scheduling an appointment for the behavioral therapy. 4 Time was cited as the most common barrier to initiating behavioral therapy. 4
Many patients with chronic pain referred for behavioral treatment are not prepared to engage in behavioral treatment. 5,6 A need for research focused on engaging patients in ways to overcome barriers to initiating behavioral treatment that has been proven to reduce opioid use has been identified as a priority. 7 Finding ways to engage more patients in these non-pharmacologic effective interventions also proven to decrease medication overuse is particularly urgent given the current opioid crisis in the United States. 8
Motivational interviewing (MI) is an ideal intervention to study in a migraine patient population because MI is “a person-centered counseling style for addressing the common problem of ambivalence about change.” 9 In MI, the counselor tries to help the client become the advocate for change through four central principles:(1) express empathy; (2) develop discrepancy between the undesirable behaviors and client values that are inconsistent with those behaviors; (3) roll with resistance rather than confronting it directly; and, (4) support self-efficacy. MI techniques include eliciting and reinforcing change talk, listening reflectively, affirming, and summarizing. MI counselors also use decisional balance procedures to help clients explore and weigh the pros and cons of change. MI is the most successfully disseminated evidence-based practice for substance abuse, with over 80 randomized clinical trials (RCTs) supporting its efficacy, 10 and long-term benefits (>1 year), 11 and small studies show its potential benefit in chronic pain conditions. 12
While MI was originally developed as a counselling style to be delivered in-person, there have been many telephone based MI studies. 13 One study found that a brief telephone intervention for as little as 15 minutes on two occasions was effective in motivating participants to attend psychotherapy after MI. 14 In the case of headache medic ine, one pilot study assessing whether telephone-based MI was helpful in adolescents with chronic headache and medication overuse, found that headache frequency improved after participants received up to four calls. 15
We sought to examine brief, non-clinician delivered, telephone-based MI and its effect compared to treatment as usual (TAU) on rates of initiating, scheduling and attending a first behavioral therapy session after specialist referral for behavioral therapy for migraine. We hypothesized that telephone-based MI would lead to greater initiating, scheduling and attending behavioral therapy for migraine.
Methods:
We conducted a two-arm randomized parallel controlled trial examining the impact of telephone based MI on initiating, scheduling, and attending an appointment for Level A evidence based behavioral headache treatments recommended by a headache specialist. This was a single blinded study where patients were blinded to the full study purpose and to allocations. Participants were told that the broad purpose of the study was to assess what they think about their headache care. They were not debriefed after the study.
Specifically, participants were informed the study involved a survey and follow-up calls about their headache treatment. Using 1:1 block randomization with blocks of 4 to 6, half were randomized to the MI arm (up to 5 MI calls) and the other half were randomized to the treatment as usual (TAU) group, which received a phone call after three months to determine whether they pursued behavioral therapy and to qualitatively assess potential reasons for their decision.
Participants and Recruitment
The study took place at two sites within one medical center in New York City. Three headache fellowship trained and United Council of Neurologic Subspecialty (UCNS) Certified headache specialists at the same urban medical center took part in the study. Two headache specialists referred out to either a health psychologist or psychologist who had a special focus on behavioral treatment for headache, while the third referred to a psychiatric nurse practitioner in the same office who was trained in the three evidence-based modalities (CBT, progressive muscle relaxation (PMR) and biofeedback). For purposes of this study, a referral for behavioral therapy was defined by a note in the patient’s chart or indication by the headache specialist on the study questionnaire that a referral was made/counseling conducted to see a healthcare provider for behavioral therapy for migraine.
Participants were recruited consecutively for visits between 6/4/18 and 8/20/18. If interested, written informed consent was obtained. Following this, patients were asked to complete a questionnaire on RedCap 16 on a tablet or paper when needed in the office. The survey included questions about demographics, headache history and disability [the Migraine Disability Assessment Screen (MIDAS)], a full self-reported medical history, and prior healthcare utilization. No compensation was provided for participation in the study.
Inclusion criteria were: patients 18 years and older diagnosed with migraine by the headache specialist based on the International Classification of Headache Disorders Criteria (ICHD)-3 beta 17 who were referred for behavioral therapy for migraine during the migraine visit.
Exclusion criteria were not having a phone number, and participating in behavioral therapy for migraine currently or anytime in the past year. MI is an opportunity for health promotion when patients are not motivated but might be amenable to an intervention as it can be a pre-treatment intervention to motivate people to attend counseling. People who are already seeking treatment would be considered motivated in the stages of change model, and thus in the “preparation” or “action” stage which is the desired outcome in successful MI interventions. 18
Once participants met full study criteria, they were randomized using a block randomization unconcealed list consulted by the study team. The block randomization list was created by a statistician unrelated to the study team.
Measures
Baseline Measures
The Migraine Disability Assessment (MIDAS) 19 is a validated 5 item questionnaire that has internal consistency and test-retest reliability and was developed to assess headache-related disability with the goal of improving migraine care. Questions ask about prior activity limitations over the past 3 months. Examples include “On how many days in the last 3 months did you miss family, social or leisure activities because of your headaches?” and “On how many days in the last 3 months did you miss work or school because of your headaches?”
The Patient Health Questionnaire (PHQ-8) is an eight-item validated depression scale used as a diagnostic tool and to determine the severity of depressive symptoms In the past 2 weeks. 20 Questions are rated on a likert scale from 0 to 3, “not at all; several days; more than half the days; nearly every day.” Example questions include: “Little interest or pleasure in doing things” and “feeling tired or having little energy.”
The Generalized Anxiety Disorder 7 (GAD-7) is a validated, reliable 7 item questionnaire used to screen for the presence of general anxiety disorder and to measure anxiety symptom severity over the past 2 weeks. 21 Example questions include “feeling nervous, anxious, or on edge” and “becoming easily annoyed and irritable” which are rated on a likert scale from 0 to 3: “not at all; several days; more than half the days; nearly every day.”
Quantitative Assessments During the Telephone Calls
Initially, when designing the study, we had one pre-specified primary outcome: scheduling the behavioral therapy appointment. Later, after we began the phone calls for this pilot feasibility/acceptability study, we realized that some participants were initiating but not scheduling, others were making the appointment but then not attending the appointment while others were attending the appointment. Thus, we felt that it would be better to divide the outcome based on the 3 stages (initiation, scheduling, and attending the appointment). This is in line with MI strategies for pain management which includes three phases: enhancing, strengthening and maintaining behavioral changes. 22 Thus, during the call, patients were asked 1) whether they initiated making (enhancing), scheduled (strengthening) and/or attended behavioral migraine therapy appointments and 2) reasons for taking part or not initiating behavioral migraine therapy. In this study, we defined initiating as “inquiring about,” scheduling as “making” and attending as “showing up for” an appointment for Level A evidence based behavioral headache treatments.
Participants were also asked the following: “Do you plan on continuing the behavioral therapy” (yes/no), “How important is managing migraine/headache to you?” (0 to10 scale); “How confident are you that you can effectively manage your migraine/headache?” (0 to10 scale); “How confident are you that doing behavioral therapy will help effectively manage your migraine/headache?” (0 to10 scale). These questions were asked to briefly assess importance and confidence rulers.
To those in the TAU group, a structured follow-up telephone assessment was administered approximately three to four months after the headache appointment. Patients were asked whether they initiated making, scheduling, and/or attending behavioral migraine therapy appointments. They were also asked the following: “Do you plan on continuing the behavioral therapy” (yes/no), “How important is managing migraine/headache to you?” (0 to10 scale); “How confident are you that you can effectively manage your migraine/headache?” (0 to10 scale); “How confident are you that doing behavioral therapy will help effectively manage your migraine/headache?” (0 to10 scale).
As above, scheduling a behavioral therapy appointment was our primary outcome. Secondary outcomes were whether patients initiated and attended the behavioral therapy appointments. A priori, we had planned to also assess and compare the number of behavioral sessions attended. However, given the low proportion of participants attending any appointments, we were unable to complete this secondary aim examining adherence amongst those in treatment. Other measures in this study were (1) the four likert scale questions above and (2) qualitative data about the MI calls as described below.
Qualitative Data Obtained During the Telephone Calls
All participants were asked during the calls: “What do you think is the most important reason you [made an appointment with a behavioral provider OR did not make an appointment with a behavioral provider]?” Study members documented responses from all of the phone calls in RedCap 23 in real-time for later thematic analyses.
In order to not contaminate the MI group from the TAU group, different individuals generally made the MI versus the TAU calls.
Intervention
Motivational Interviewing Training
Prior research suggests that the level of training background does not influence the success of MI 24 and that undergraduate students can be trained to successfully deliver MI. 25 In order to test the feasibility of non-professionals delivering brief telephone delivered MI for migraine for more rapid and cost efficient dissemination in the future, undergraduate students were trained to deliver MI in this study. They participated in a full day MI training conducted by a Motivation Interviewing Network of Trainers (MINT) trainer. 26 Then, over approximately six weeks, they received one on one training with a MI instructor from the Health Education and Training Institute (HETI). 27 During this time, they completed three individual MI training calls whereby their MI calls were audio-recorded and coded by their individual MI instructor from HETI. Feedback was given verbally via coaching with three half-hour phone coaching sessions with an experienced MI coder and coach from HETI, where they received in depth analysis and guidance to discuss the specifics of each audio-recorded call, and via ratings using the Motivational Interviewing Treatment Integrity Code (MITI 4.2.1). These methods of coaching and practice feedback i.e. the rating scale have been shown to enhance post-training proficiency.28
MI Phone Intervention
MI was not developed to be a fully “manualized” technique. Prior research has shown that studies that did not use a manual reported higher effect scores than those that used one. The MI trained undergraduate students were instructed to attempt to complete up to 5 MI calls in the three months following the initial headache appointment with the behavioral therapy referral. 29 MI calls were recommended to occur for at least 15 minutes per call and they were to be spaced apart with about two weeks in between each call. The length of time per call was instructed as guidance only as there is little evidence on the minimum length of time needed to have an effective intervention. 30
An example of an open-ended MI call might be, “What can you tell me about your physician’s recommendation for you to see a therapist?” A closed ended question (non-MI) question might be, “Did your physician recommend that you see a therapist?” Another example might be, “What thoughts went through your head when your physician recommended you see a therapist for management of your migraine? A closed ended question (non-MI) might be, “Did you think about seeing a therapist for migraine management after your physician made that recommendation?”
Analyses:
Quantitative:
Descriptive statistics including means and standard deviations were calculated. The distribution of variables was evaluated for normality using the Shapiro-Wilk’s Test for Placebo. The primary outcome (scheduling an appointment) was evaluated using chi-square tests as were the secondary outcomes of initiating and scheduling. The other secondary outcomes of the managing/confidence questions wats evaluated using two sample, two-tailed t-tests. The sample size was large enough and the deviations from normality moderate enough to support the use of t-tests.
Statistical significance was defined at p< 0.05. R version 3.5.1 was used for all statistical analyses.
This was a pilot study which like other pilot studies of MI did not have a power calculation. 31,32 As indicated by Kraemer and colleagues, 33 our pilot sample size was based on the pragmatics of recruitment and the requisites for examining feasibility. A prior study conducted by our team that took place over a similar recruitment period found that out of 234 eligible patients, about 30% (69/234) were referred for behavioral therapy. Accounting for about 10 to15% dropout, our recruitment goal was 75 to 80 in this pilot study. Thus, we ended enrollment when we reached our target goal (76 patients).
Qualitative:
The final secondary outcome, qualitative MI call data, was evaluated using general thematic analysis. General thematic analysis was used to analyze the reasons that patients who were referred to behavioral therapy adhered or did not adhere to the recommendation to schedule an appointment with a provider. AG and GS individually created a list of codes that emerged from responses to each question. Multiple patients received more than one code. The individual code lists were compared and combined to establish a universal code. AG and GS each used the universal code to assign codes to the respondent data, and then reconciled the coding. Discrepancies were resolved by study member MTM. The authors AG, GS and MTM carefully evaluated the codes to achieve agreement on themes. 34
The study was approved by the NYU Institutional Review Board. Written informed consent was obtained from all study subjects. In addition, it was registered on clinicaltrials.gov [NCT03799211].
Results:
Three UCNS Certified Headache Specialists participated in the study which was conducted over an 11 week time period from June 4, 2018 to August 20, 2018. As seen in Figure 1, 307 patients with headache were seen by these three providers during the recruitment period. Of the 76 patients who met study criteria and were randomized, 36 were assigned MI and 40 were assigned the TAU arm. We utilized a per protocol analysis including only those participants who completed the three month assessment in the TAU group and those who had completed at least one MI call in the active group. Two patients could not be reached for at least one MI call, and two others asked to leave the study during the first MI call before any data was obtained; thus, n=32 were analyzed in the MI group. Similarly, 13 patients from the TAU group could not be reached for their 3-month follow-up call and thus the TAU analysis included n=27 participants.
Figure 1.
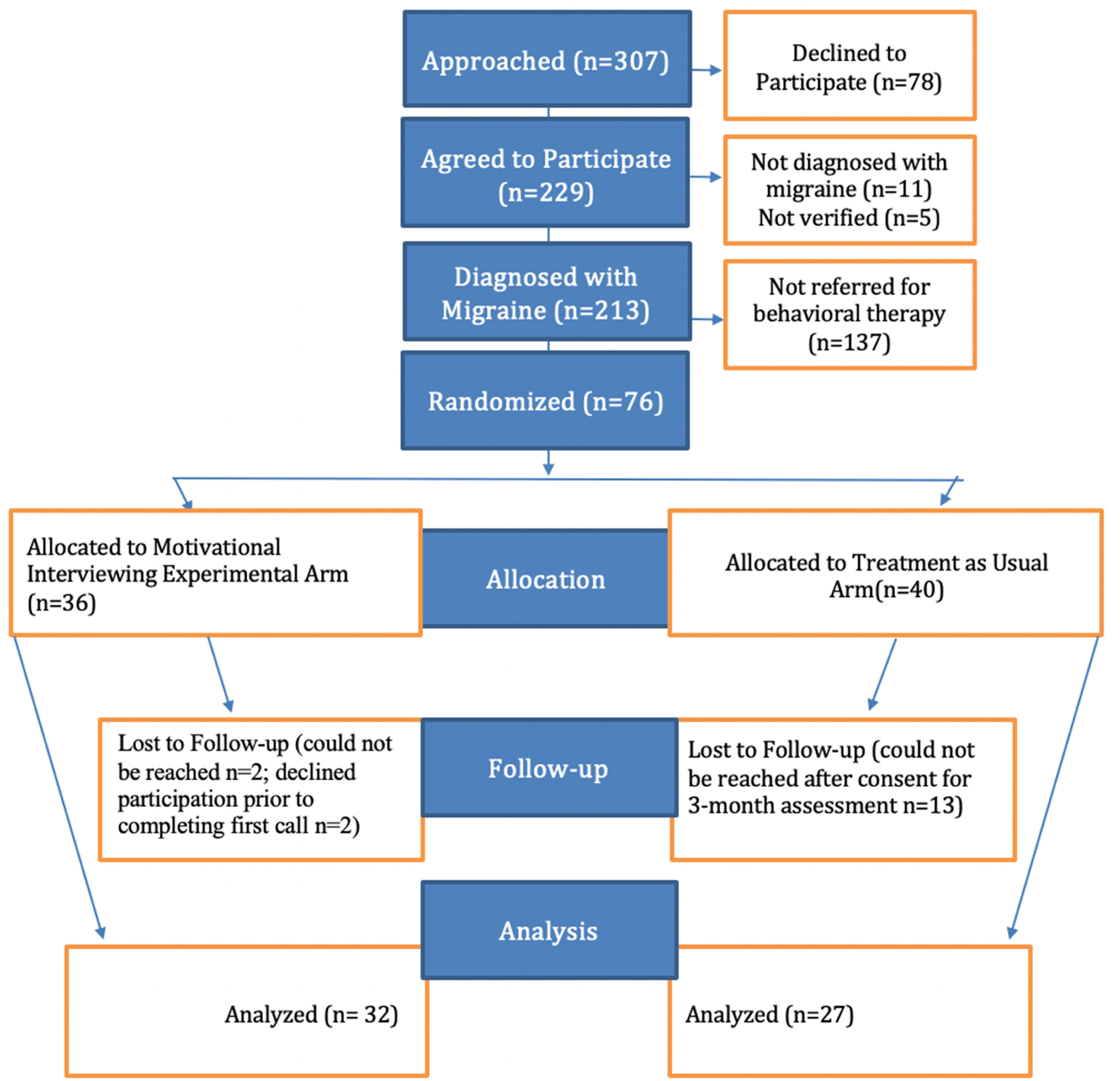
Schematic of Experimental Design
As seen in more detail in Table 1, subjects were predominantly female, Caucasian and highly educated, with a mean age of 39±12 years. All participants had health insurance and almost all had prescription drug coverage. The majority of participants scored moderate or higher on the PHQ-8 for depression and on the GAD-7 for anxiety. Headache days, pain intensity, age, depression, anxiety and MIDAS scores were not normally distributed. Median number of headache days/month was: 10 [IQR: 5 – 15]. The majority (70.9% or 44/62) patients were in the moderate to severely disabled disability categories as measured by the MIDAS.
Table 1:
Participant Demographics, Headache Characteristics and Prior Healthcare Utilization
| Participant Information | Intervention Arm (n=36) |
Control Arm (n=40) |
p-value |
Total Participants (n=76) |
|---|---|---|---|---|
| Sex | 0.184 | |||
| Female | 32 (89%) | 39 (98%) | 71 (93%) | |
| Male | 4 (11%) | 1 (3%) | 5 (7%) | |
| Age | 0.428 | |||
| Current Age (Mean, SD, Range) | 40.4 ± 12.3 (18–66) | 38.1 ± 12.1 (19–68) | 39.2 ± 12.2 (18–68) | |
| Race | 0.283 | |||
| White | 26 (72%) | 33 (83%) | 59 (78%) | |
| All others | 10 (28%) | 7 (18%) | 17 (22%) | |
| Ethnicity | 0.328 | |||
| Hispanic or Latino | 6 (17%) | 4 (10%) | 10 (13%) | |
| Not Hispanic or Latino | 27 (75%) | 35 (88%) | 62 (82%) | |
| Years of Formal Education | 0.462 | |||
| Less than Four Years of College | 3 (8%) | 6 (15%) | 9 (12%) | |
| Bachelor’s Degree | 17 (47%) | 14 (35%) | 31 (41%) | |
| Graduate study or Advanced Degree | 10 (28%) | 13 (33%) | 23 (30%) | |
| Annual Income | 0.662 | |||
| Under $25,000 | 3 (8%) | 4 (10%) | 7 (9%) | |
| $25,000 - $50,000 | 4 (11%) | 4 (10%) | 8 (11%) | |
| $50,000 - $75,000 | 4 (11%) | 8 (20%) | 12 (16%) | |
| $75,000 – 100,000 | 4 (11%) | 6 (15%) | 10 (13%) | |
| $100,000 - $150,000 | 4 (11%) | 7 (18%) | 11 (14%) | |
| $150,000 - $200,000 | 3 (8%) | 4 (10%) | 7 (9%) | |
| Over $200,000 | 7 (19%) | 2 (5%) | 9 (12%) | |
| Refused/Unknown | 7 (19%) | 5 (13%) | 12 (16%) | |
| Health Insurance | ||||
| has medical coverage | 35 (97%) | 38 (95%) | 0.619 | 73 (96%) |
| no medical coverage | 1 (3%) | 2 (5%) | 3 (4%) | |
| has drug/prescription coverage | 33 (92%) | 38 (95%) | 0.564 | 71 (93%) |
| no drug/prescription coverage | 1 (3%) | 0 (0%) | 1 (1%) | |
| Self-Reported Prior History of Having had the Following Psychiatric Conditions* | ||||
| Depression | 14 (39%) | 16 (40%) | 0.921 | 30 (39%) |
| Anxiety | 13 (36%) | 23 (58%) | 0.062 | 36 (47%) |
| Post-traumatic Stress Disorder (PTSD) | 1 (3%) | 3 (8%) | 0.617 | 4 (5%) |
| Bipolar Disorder | 1 (3%) | 1 (3%) | 0.94 | 2 (3%) |
| Obsessive Compulsive Disorder (OCD) | 1 (3%) | 0 (0%) | 0.474 | 1 (1%) |
| Attention Deficit Hyperactivity Disorder (ADHD) | 3 (8%) | 4 (10%) | 0.802 | 7 (9%) |
| Insomnia | 3 (8%) | 5 (13%) | 0.715 | 8 (11%) |
| Schizophrenia | 1 (3%) | 0 (0%) | 0.474 | 1 (1%) |
| Self Report of Ever Being Diagnosed with Overlapping Pain Conditions* | ||||
| Irritable Bowel Syndrome (IBS) | 7 (19%) | 10 (25%) | 0.562 | 17 (22%) |
| Temporomandibular Disorder | 1 (3%) | 0 (0%) | 0.474 | 1 (1%) |
| Fibromyalgia | 2 (6%) | 2 (5%) | 0.914 | 4 (5%) |
| Endometriosis | 1 (3%) | 1 (3%) | 0.94 | 2 (3%) |
| Chronic Low Back Pain | 3 (8%) | 2 (5%) | 0.663 | 5 (7%) |
| Other | 2 (6%) | 5 (13%) | 0.435 | 7 (9%) |
| Baseline Headache Characteristics | ||||
| Number of Headache Days in the last month | n=36 | n=40 | 0.275 | n=76 |
| Mean ± SD (min-max), median [IQR] |
13.2 ± 9 (2–31), 12 [6 – 16.75] |
11 ± 8.9 (0–30) 8 [4 – 15] |
12 ± 9 (0–31) 10 [5 – 15] |
|
| Pain intensity (0–10 scale) | n=36 | n=39 | 0.031 | n=75 |
| Mean ± SD (min-max), median [IQR] |
6.7 ± 2 (3–10), 7 [5 – 8] |
5.6 ± 2 (0–9) 6 [4 – 7] |
6.1 ± 2.1 (0–10) 6 [5 – 8] |
|
| MIDAS (Sum of the first 5 questions) | n=30 | n=32 | 0.246 | n=62 |
| Mean ± SD (min-max), median [IQR] |
38.9 ± 55.5 (0–280), 18 [8.5 – 46] |
25.8 ± 29.3 (0–133) 15.5 [8.25 – 31] |
32.2 ± 44.1 (0–280) 17.5 [8.75 – 33.75] |
|
| Grade | ||||
| 1 0–5 | 5 (14%) | 6 (15%) | 0.995 | 11 (14%) |
| 2 6–10 | 3 (8%) | 4 (10%) | 7 (9%) | |
| 3 11–20 | 8 (22%) | 9 (23%) | 17 (22%) | |
| 4 21+ | 13 (36%) | 14 (35%) | 27 (36%) | |
| Psychiatric Screens | ||||
| PHQ-8 | n=35 | n=39 | 0.111 | n=74 |
| Mean ± SD (min-max) median [IQR] |
15.2 ± 4.8 (8–24) 15 [11–17] |
13.6 ± 3.4 (9–22) 13 [11.25–15] |
14.4 ± 4.2 (8–24) 14 [11–17] |
|
| GAD-7 | n=36 | n=40 | 0.934 | n=76 |
| Mean ± SD (min-max) median [IQR] |
12.7 ± 4.6 (7–21) 12.5 [8–16.25] |
11.8 ± 3.6 (7–19) 12 [9–14.5] |
12.2 ± 4.1 (7–21) 12 [8.5–15] |
|
The percentages reported for these questions may not add up to 100 as participants were able to select multiple responses.
As shown in Table 2, the vast majority of patients had previously been evaluated and/or treated by neurologists for headaches (66/75; 88.0%) and most had also seen their primary care physician for headaches (55/75; 73.3%). About one fifth (15/76; 19.7%) had previously participated in any behavioral therapy (CBT, biofeedback and/or PMR) prior to one year of enrollment into the study. Of those who had not done any of these evidence based behavioral therapies, about one quarter (15/59; 25.4%) reported having previously received a recommendation to try behavioral therapy for the treatment of headache.
Table 2:
Healthcare Utilization
| MI arm | TAU arm | All | |
|---|---|---|---|
| Headache Healthcare Utilization | |||
| Previously seen for evaluation and/or treatment of headaches* | |||
| Neurologist | 31/35 (88.6%) | 35/40 (87.5%) | 66/75 (88.0%) |
| Eye doctor (Ophthalmologist) | 14/35 (40.0%) | 8/40 (20.0%) | 22/75 (29.3%) |
| Dentist | 7/35 (20.0%) | 5/40 (12.5%) | 12/75 (16.0%) |
| Emergency Room/Urgent Care Physician | 7/35 (20.0%) | 9/40 (22.5%) | 16/75 (21.3%) |
| Primary Care Physician (Pediatrician/Family Medicine) | 25/35 (71.4%) | 30/40 (75.0%) | 55/75 (73.3%) |
| Ear Nose and Throat Physician (otolaryngologist) | 5/35 (14.3%) | 6/40 (15.0%) | 11/75 (14.7%) |
| Chiropractor | 4/35 (11.4%) | 9/40 (22.5%) | 13/75 (17.3%) |
| Acupuncturist | 7/35 (20.0%) | 14/40 (35.0%) | 21/75 (28.0%) |
| Psychologist | 5/35 (14.3%) | 8/40 (20.0%) | 13/75 (17.3%) |
| Physical Therapist | 7/35 (20.0%) | 5/40 (12.5%) | 12/75 (16.0%) |
| Psychiatrist | 6/35 (17.1%) | 6/40 (15.0%) | 12/75 (16.0%) |
| Had previously done any behavioral therapy for migraine | 9/36 (25%) | 6/40 (15%) | 15/76 (19.7%) |
| Had previously done any of the following specific forms of behavioral therapy: | |||
| Cognitive Behavioral Therapy | |||
| 1 visit | 2/8 (25.0%) | 0/2 (0.0%) | 2/10 (20.0%) |
| 2–5 visits | 2/8 (25.0%) | 0/2 (0.0%) | 2/10 (20.0%) |
| 6–10 visits | 1/8 (12.5%) | 0/2 (0.0%) | 1/10 (10.0%) |
| 10+ visits | 3/8 (37.5%) | 2/2 (100%) | 5/10 (50.0%) |
| Biofeedback | |||
| 1 visit | 0/2 (0.0%) | 0/3 (0.0%) | 0/5 (0.0%) |
| 2–5 visits | 1/2 (50.0%) | 2/3 (66.7%) | 3/5 (60.0%) |
| 6–10 visits | 0/2 (0.0%) | 1/3 (33.3%) | 1/5 (20.0%) |
| 10+ visits | 1/2 (50.0%) | 0/3 (0.0%) | 1/5 (20.0%) |
| Progressive Muscle Relaxation | |||
| 1 visit | 0/4 (0.0%) | 0/1 (0.0%) | 0/5 (0.0%) |
| 2–5 visits | 1/4 (25.0%) | 0/1 (0.0%) | 1/5 (20.0%) |
| 6–10 visits | 2/4 (50.0%) | 0/1 (0.0%) | 2/5 (40.0%) |
| 10+ visits | 1/4 (25.0%) | 1/1 (100%) | 2/5 (40.0%) |
| Has not previously done behavioral therapy but someone previously recommended behavioral therapy (cognitive behavioral, biofeedback or progressive muscle relaxation) for treatment of headache. | 6/25 (24.0%) | 9/34 (26.5%) | 15/59 (25.4%) |
| Specific Recommendations: | |||
| Cognitive Behavioral Therapy | 1/6 (16.7%) | 1/9 (11.1%) | 2/15(13.3%) |
| Biofeedback | 1/6 (16/7%) | 2/9 (22.2%) | 3/15 (20.0%) |
| All 3 | 1/6 (16.7%) | 3/9 (33.3%) | 4/15 (26.7%) |
| Unspecified | 3/6 (50.0%) | 2/9 (22.2%) | 5/15 (33.3%) |
| Online | 0/6 (0.0%) | 1/9 (11.1%) | 1/15 (6.7%) |
| Reasons for not trying it?* | |||
| Did not have enough information about treatment | 0/6 (0.0%) | 0/8 (0.0%) | 0/14 (0.0%) |
| Did not think they worked | 1/6 (16.7%) | 1/8 (12.5%) | 2/14 (14.3%) |
| Did not have time | 4/6 (66.7%) | 5/8 (62.5%) | 9/14 (64.3%) |
| Not covered by insurance | 1/6 (16.7%) | 2/8 (25.0%) | 3/14 (21.4%) |
| Covered by insurance, but co-pay/deductible was too high | 1/6 (16.7%) | 0/8 (0.0%) | 1/14 (7.1%) |
| Other | 0/6 (0.0%) | 3/8 (37.5%) | 3/14 (21.4%) |
| Has previously done other psychotherapy (Not cognitive behavioral, biofeedback or progressive muscle relaxation therapies) for headaches? | 2/36 (5.6%) | 5/40 (12.5%) | 7/76 (9.2%) |
| Has previously done psychotherapy (Not cognitive behavioral, biofeedback or progressive muscle relaxation therapies) not for headaches? | 9/35 (25.7%) | 16/39 (41.0%) | 25/74 (33.8%) |
| Other non-pharmacologic therapies tried* | |||
| Acupuncture | 12/20 (60.0%) | 17/28 (60.7%) | 29/48 (60.4%) |
| Meditation | 12/20 (60.0%) | 19/28 (67.9%) | 31/48(64.6%) |
| Yoga | 13/20 (65.0%) | 8/28 (28.6%) | 21/48 (43.8%) |
| Tai Chi | 1/20 (5.0%) | 1/28 (3.6%) | 2/48 (4.2%) |
| Chiropractic Manipulation | 8/20 (40%) | 12/28 (42.9%) | 20/48 (41.7%) |
| Other | 3/20 (15.0%) | 3/28 (10.7%) | 6/48 (12.5%) |
The percentages given for the questions about previously seen healthcare providers, reasons for not trying the behavioral treatment, and previous nonpharmacologic headache treatments may add up to greater than 100% as individual participants had the ability to select multiple answer choices in these questionnaire categories.
Patients received an average number of 2.69±1.56 [0 to 5] MI calls. The average time spent on each MI call was 12.10±5.13[4 to 28] minutes.
Preliminary Efficacy Data
Overall across groups, only 18/59 (30.5%) participants scheduled and 13/59 (22.0%) attended at least one appointment by 3 months after their referral to behavioral therapy. Our pilot study results revealed that those in the MI groups were more likely to initiate making an appointment (Table 3, 22/32 (68.8%) vs. 11/27 (40.7%), chi-square=4.7, p=0.031, OR=3.20, OR 95%CI: 1.10 to 9.34) but there was no difference between groups in scheduling (p= 0.204) or attending the appointment (p=0.974).
Table 3:
Appointment Statistics
| MI arm N=32* | TAU arm N=27 | Significance | ||
|---|---|---|---|---|
| Initiated Behavioral Therapy Appointment | 22/32 (68.8%) | 11/27 (40.7%) | .031 | |
| Scheduled an appointment with provider for behavioral therapy | 12/32 (37.5%) | 6/27 (22.2%) | .204 | |
| Attended the behavioral therapy appointment | 7/32 (21.9%) | 6/27 (22.2%) | .974 | |
| Plan on continuing the behavioral therapy (yes) | 5/32 (15.6%) | 4/27 (14.8%) | .931 | |
| How important is managing migraine/headache to you? (0–10 scale)** | First Call: 9.16 +/− 1.27, [6–10], 10.00 |
Last Call: 9.22+/− 1.18, [6–10], 10.00 |
9.19+/− 1.30, [6–10], 10.00 |
.944 |
| How confident are you that you can effectively manage your migraine/headache? (0–10 scale)** | First Call: 6.26 +/− 2.27, [0–10],7.00 |
Last Call: 6.62+/− 2.50, [0–10], 7.50 |
6.59+/− 2.26, [0–10], 7.00 |
.576 |
| How confident are you that doing behavioral therapy will help you effectively manage your migraine/headache? (0–10 scale)** | First Call: 4.83+/− 2.47, [0–10], 5.00 |
Last Call: 5.04+/− 1.95, [0–9], 5.00 |
5.35+/− 2.59, [0–10], 6.00 |
.441 |
2 MI pts were never reached by phone and 2 withdrew on the first follow-up call before the questions were asked.
p-values for these last 3 questions represent two sample, two-tailed t-tests comparing responses given in the first and last MI calls. The remainder of the p-values represent two sample, two-tailed t-tests comparing the MI and TAU groups.
As shown in Table 3, there was no difference on a 0 to 10 scale in patients’ importance or confidence in their migraines pre and post the MI calls. For example, there was no change in the level of importance of managing migraine for patients in the first call compared to the last call [9.16±1.27 versus 9.22±1.18, p=0.8531]. The responses to the questions regarding importance/confidence in managing the headaches were not normally distributed.
As seen in Table 4, themes in the MI group for why patients scheduled behavioral therapy were: Previous Treatments Have Been Unpleasant/Ineffective, Positive Attitudes Towards Behavioral Therapy, and Recommended by Doctor. Themes in the TAU group for why patients scheduled behavioral therapy were: Seeking Improvement in Headaches/QOL, Seeking Nonpharmacologic Treatment Options, Recommended by Doctor, Accessibility. Themes for why those in the MI group did not schedule behavioral therapy were: Time as a Barrier, Cost as a Barrier, Does Not Think Behavioral Therapy Will Work, Difficulty Accessing or Initiating appointments, No Reason to do Behavioral Therapy, and Considering or Using Other Treatment Options. Themes for why those in the TAU group did not schedule behavioral therapy were: Time as a Barrier, Cost as a Barrier, Does Not Think Behavioral Therapy Will Work, Difficulty Accessing or Initiating appointments, Satisfied with Current Treatment, and Prioritizing Other Things.
Table 4:
Qualitative Taxonomy of Themes and Codes of Reasons Why Patients Made/Did Not Make Behavioral Therapy Appointment
| THEMES | CODES | THEMES | CODES | ||
|---|---|---|---|---|---|
| Reasons for Making the Appointment MI Group | Previous Treatments Have Been Unpleasant/Ineffective | Want to try something new b/c previous treatments have been ineffective: 4 Meds are too expensive/unpleasant: 2 Seeking HA relief: 6 Pregnant and cannot take drugs: 1 |
Reasons for Making the Appointment Control Group |
Seeking Improvement in Headaches/ QOL |
Seeking headache relief: 3 Headaches are affecting QOL: 1 |
| Behavioral Therapy Positives | Interested in non-pharm options: 3 Wanted to try something new/different:1 Maximize their control over migraines by doing multiple things: 2 Interested in mind-body connection: 1 Interesting: 1 |
Seeking Nonpharmacologic Treatment Options | Seeking non-pharmacologic options: 1 | ||
| Recommended by Doctor | Following doctor’s orders: 3 | Recommended by Doctor | Following/trust doctor’s orders: 2 | ||
| Accessibility | Easily found provider/ who took insurance: 1 | ||||
| Reasons for Not Making the Appointment MI Group | Time as a Barrier | Travel plans/on Vacation: 8 Patient does not have time to travel to the provider: 1 Providers lack flexible hours/patient assumes they would: 5 Mechanism to make an appt is inconvenient/difficult: 3 Didn’t have time to initiate/look into making an appt: 6 Lacks time to do BT because of work/other engagements: 9 Surgery/hospitalization: 2 |
Reasons for Not Making the Appointment Control Group | Time as a Barrier | No time to schedule/initiate an appointment: 5 Doesn’t have time due to work/other engagements: 4 Travel plans/vacation: 2 |
| Cost as a Barrier | No insurance/limited coverage/expensive/cannot afford: 10 | Cost as a Barrier | Cannot afford/insurance: 4 | ||
| Does Not Think Behavioral Therapy Will Work | Not enough accessible information on BT: 4 Does not think BT is suitable for their specific migraine triggers: 3 Doesn’t think BT would measure up to medication effects: 1 Unsure of efficacy of behavioral therapy as a result of the perceived infrequency of the appointments (once week rather than daily): 1 Previous experience with BT/something similar was not effective: 4 |
Does Not Think Behavioral Therapy Will Work | Did not have effective past experience w/ BT: 1 | ||
| No Reason to Do Behavioral Therapy | Headaches are not that serious: 8 Prioritizing other non-HA health concerns: 4 Confident w/ current plan: 11 Physician didn’t emphasize enough: 2 |
Satisfied with Current Treatment | Confident w/ current treatment plan: 5 | ||
| Considering or Using Other Treatment Options | Prioritizing medications for HA first: 4 Prioritizing other non-pharm HA treatments:2 Concerned different treatments would conflict, would not know which one is actually working: 2 Weighing treatment options before committing to BT: 1 |
Prioritizing Other Things | Prioritizing other non-pharm: 2 Prioritizing other health concerns: 2 |
||
| Difficulty Accessing or Initiating Appointments | Unable to find provider nearby: 1 Mental state prevented making BT appointment: 2 In the process of making an appointment: 2 Unhappy with provider/in process of finding a new one: 2 Lost paper w/ providers: 4 |
Difficulty Accessing or Initiating appointments | Providers are hard to reach/haven’t heard back: 4 |
BT=Behavioral Therapy
No adverse events were noted in this trial.
Discussion:
In this pilot study assessing telephone based motivational interviewing as a potential approach to improve rates of initiating, scheduling and attending appointments for behavioral therapy for migraine, we found the following: (1) In total across both groups, only 31% participants scheduled and only 22% attended at least one appointment following headache specialist referral to behavioral therapy. While there was no difference between MI and TAU in the percentage of patients scheduling or attending behavioral therapy appointments for migraine, there was a difference between the MI and TAU groups in initiating behavioral therapy for migraine. (2) The qualitative feedback provided demonstrated that there are other factors that appear to limit patients’ scheduling and attending such appointments.
Previously, telephone interventions were found to provide a novel method and to be of low cost and an appropriate tool for use in healthcare settings. 35 However, we experienced some difficulty in reaching patients by phone. We only successfully completed a mean of 2.7 out of 5 calls. However, as research shows, telephone interventions improve access to various populations in the healthcare system who may not be able to access effective interventions for their mental illness symptoms. 36 Several studies have demonstrated that psychological therapies delivered by telephone were as effective as face-to-face treatment,37 therapeutic alliance was comparable, and participants were satisfied with this model of delivery. 38 MI sessions as short as 15 minutes in length, performed as pre-treatment, improved attendance for mental health treatment and thus an increased uptake of mental health interventions. 30
As in these prior studies, our results indicate that our low cost intervention consisting of non -clinician telephone based MI in which patients did engage with callers for a mean duration of 12 minutes improves rates of initiation of inquiry about setting up the behavioral therapy. However, MI did not change the rate in which the patients in the MI arm actually scheduled or attended their behavioral therapy appointments relative to the TAU arm. This is interesting because a systematic review of 72 clinical trials spanning a range of conditions showed a small to medium effect size in improving health outcomes but failed to support the theory that increased client change talk would predict behavior change. 29 There was also a more recent systematic review of 14 clinical trials examining MI as a pre-treatment to enhance attendance for treatment of mental health issues. 30 They also conducted subgroup analyses to investigate differences among individuals seeking treatment for the mental health issues and those who were not seeking treatment for the mental health issues. In five of the fourteen studies, there was minimal or no influence of MI as a pre-treatment. They also found that individuals not seeking treatment benefitted the most from MI. Interestingly, in two of the studies, MI pre-treatment did facilitate an increase in informal help seeking from parents and significant others. 39
Patients may want to engage in behavioral therapy but for reasons presented in this study (and similar previously published reasons) [see several of the recent reviews on this topic 40,41], there are too many other barriers, oftentimes external factors, preventing them from doing so. 3 Factors such as time and cost were themes across both the MI and TAU groups and likely account for the discrepancy between initiating behavioral therapy in the MI group and attending the session. Cost is also a likely factor explaining the discrepancy in rates in which patients initiated inquiry about behavioral therapy in our prior study (~56%) and in the control arm of the current study (~41%). 42 In our prior study on initiation rates for migraine behavioral therapy, which showed that 56% of people initiated making an appointment, a behavioral therapy clinical trial was being offered around the same time in the same city, thus providing some migraine patients the opportunity to receive some cognitive therapy for free. However, at the time of enrollment in this study, enrollment in that study was closed, potentially increasing cost as a barrier.
In addition, even though patients were referred for behavioral therapy, some responses support some participants may not have felt the need to engage in it. While they were seeing a headache specialist and were referred for behavioral therapy at the visit, we had themes including no reason to do behavioral therapy and satisfied with the current plan.
Strengths
This was a low cost intervention with non-professionals trained in MI. The study took place in two different types of headache specialist offices (one academic/faculty group practice and one private practice). Further, the study included a detailed description of baseline demographic and clinical characteristics. These included patient age, race, income, insurance coverage along with pre-existing medical conditions and prior experience with behavioral therapy and non-pharmacological therapies. The study was also a single-blind study, so that no participant knowledge of the use of MI would skew the results.
Despite the following limitations, the study provides a thorough look into the barriers patients are confronted with when recommended behavioral therapy, as well as their initial perceptions of the therapy. This information can be used to better suit the presentation and organization of behavioral treatment to make patients more open to consider level A, evidence-based non-pharmacological modalities of treatment.
Limitations
Our study had several limitations. Generalizability may be limited as the study took place within one healthcare system in a large metropolitan city where many behavioral therapists for migraine are out of pocket providers. Replication across other settings is needed. This was a pilot study which like other pilot studies of MI did not have a power calculation. 31,32 We anticipated having a higher referral rate for behavioral therapy as only 30% of the overall study population were referred for behavioral therapy. However, the study period coincided with the release of a new class of migraine specific preventative medicine to the market. Many patients may have made an appointment with the headache specialist with the specific intention of inquiring about or obtaining the new medication. Thus, we had a small sample size. With our nonsignificant findings, we may have type 2 error; if the sample size had been larger we might have had more significant findings. In addition, we might have had different findings-more than 22% of people referred for behavioral therapy actually attending an initial session of behavioral therapy for migraine, if the study had been conducted in different geographic regions where behavioral therapy is less costly. This is because patients in the study often stated that treatment expenses and lack of insurance coverage deterred them from making behavioral therapy appointments.
In addition, our study was limited in that we only assessed the use of MI in migraine for the initiation, scheduling and making an appointment for migraine behavioral therapy. As this was a pragmatic study and we wished to minimize patient burden, we limited the questions asked and did not assess for stages of change or self-efficacy using in-depth validated psychometric scales; we only assessed for importance and confidence rulers. Furthermore, as noted in the literature, MI may be used for a variety of purposes, including but not limited to (1) stopping or preventing an unhealthy behavior (2) promoting healthy behavior for a specific problem (3) behavior change in specific settings. We did not assess MI in other contexts for which it might be useful in the migraine patient population. In addition, we only used telephone-based MI. MI has been delivered in-person 43 and now there are efforts to also deliver it via smartphones. 44 However, one advantage of telephone based MI over in-person MI is that it may enable some participants with higher barriers to in-person appointments to initially engage-using in person MI only reaches those already willing and able come in for a psychological intervention.
In terms of treatment fidelity, the MI was conducted by undergraduate students who were not as experienced as some MI counselors in other studies. However, part of the reason for the popularity of MI is that it can be used by people without advanced degrees. These non professionals were able to pass rigorous, standardized training and certification procedures. While the undergraduates went through rigorous training so that they could perform MI, and did practice sessions with the trained coaches, we did not monitor treatment fidelity throughout the study.
Finally, while this was a randomized controlled study, future studies should use a stricter design with the randomization allocation fully blinded.
Future Research
In a prior study assessing telephone-based MI for medication overuse headache, more calls in the intervention group were associated with having fewer headache days at follow-up. 15 Also, prior research demonstrated that the addition of individual MI pretreatment (one in-person and 3 telephone based sessions) to group CBT for a heterogeneous group of anxiety disorders led to significantly better outcomes than for CBT without MI. 45 However, in this pilot study, we did not examine headache outcomes comparing MI as a prelude to behavioral therapy versus just the behavioral therapy. This would be appropriate for larger scaled studies in future research. However, before such studies are conducted, it will likely be necessary to try to lessen some of the barriers identified in participating in behavioral therapy. Our results further support the need to find novel ways to engage and retain patients with migraine in behavioral interventions, as there are barriers even to initial telephone based motivational interviewing that exist. After some of the other barriers to obtaining behavioral therapy are overcome, future work might also examine the effect of MI telephone calls on lessening the drop outs from migraine behavioral therapy. Finally, there may be subpopulations within the migraine population who might benefit the most from MI before behavioral therapy. For example, in the pre-treatment of MI before CBT study in GAD, the effects of adding an MI pretreatment to CBT on worry reduction appeared to be greatest for individuals with high worry severity at baseline. 46 Another study showed that those with higher levels of baseline anxiety had better results with MI 47 however, a meta-analysis showed that MI is effective for people with high levels of distress and for people with low levels of distress. 24 The meta-analysis also showed that older participants had greater benefit from MI. 24 Thus, future studies might assess whether certain migraine subpopulations might be targeted for motivational interviewing based interventions.
Conclusion:
MI may help to improve rates of initiation of behavioral therapy for migraine but other barriers appear to lessen the impact in scheduling and attending the behavioral therapy appointments. Future work should target ways to lessen individual patient barriers to participation in behavioral interventions for migraine alongside MI strategies.
Study Funding:
Funding for the study was provided by a grant obtained from the International Headache Academy which covered the cost of the motivational interviewing training/coaching/coding. Dr. Minen is a recipient of a K23 AT009706 from the National Center for Complementary and Integrative Health which allows provides salary support to conduct research.
Footnotes
Mia Minen, MD, MPH-Dr. Minen has received funding from the NCCIH for salary support. She has also received funds for travel to meetings of the American Academy of Neurology Guidelines Development, Dissemination and Implementation Subcommittee, of which she is a member, and funds for travel to the American Headache Society’s meetings because she is an AHS General Board member. She is also Co-Section Head of the Headache Section of Pain Medicine and is an Associate Editor of the journal Headache.
Gabriella Sahyoun-no disclosures
Ariana Gopal-no disclosures
Valeriya Levitan, MD-no disclosures
Elizabeth Pirraglia, MA-no disclosures
Naomi M. Simon, MD. MSc
Audrey Halpern, MD-has pharmaceutical speaking disclosures unrelated to the topic.
This paper is not under consideration with any other journal.
References
- 1.Campbell J, Penzien D, Wall E. Evidence-based guidelines for migraine headache: Behavioral and physical treatments. 2000.
- 2.Andrasik F, Blanchard EB, Neff DF, Rodichok LD. Biofeedback and relaxation training for chronic headache: A controlled comparison of booster treatments and regular contacts for long-term maintenance. J Consult Clin Psychol 1984;52(4):609–615. doi: 10.1016/0304-3959(85)90211-8. [DOI] [PubMed] [Google Scholar]
- 3.Matsuzawa Y, Lee YSC, Fraser F, et al. Barriers to behavioral treatment adherence for headache: An examination of attitudes, beliefs, and psychiatric factors. Headache 2019;59(1):19–31. doi: 10.1111/head.13429 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Minen MT, Azarchi S, Sobolev R, et al. Factors related to migraine patients’ decisions to initiate behavioral migraine treatment following a headache specialist’s recommendation: A prospective observational study. Pain Med 2018;19(11):2274–2282. doi: 10.1093/pm/pny028 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jensen MP, Nielson WR, Turner JA, Romano JM, Hill ML. Changes in readiness to self-manage pain are associated with improvement in multidisciplinary pain treatment and pain coping. Pain. 2004;111(1–2):84–95. doi: 10.1016/j.pain.2004.06.003 [doi]. [DOI] [PubMed] [Google Scholar]
- 6.Kerns RD, Habib S. A critical review of the pain readiness to change model. J Pain. 2004;5(7):357–367. doi: S1526-5900(04)00877-6 [pii]. [DOI] [PubMed] [Google Scholar]
- 7.Wilson M, Roll JM, Corbett C, Barbosa-Leiker C. Empowering patients with persistent pain using an internet-based self-management program. Pain Manag Nurs 2015;16(4):503–514. doi: 10.1016/j.pmn.2014.09.009 [doi]. [DOI] [PubMed] [Google Scholar]
- 8.National Institutes of Health. HEAL initiative research plan. U.S. Department of Health and Human Services Web site. https://www.nih.gov/research-training/medical-research-initiatives/heal-initiative/heal-initiative-research-plan. Updated 2019.
- 9.Miller W, Rollnick S. Motivational interviewing: Helping people change. 3rd ed. New York: Guilford Press; 2013. [Google Scholar]
- 10.Hall K, Staiger PK, Simpson A, Best D, Lubman DI. After 30 years of dissemination, have we achieved sustained practice change in motivational interviewing? Addiction. 2016;111(7):1144–1150. doi: 10.1111/add.13014 [doi]. [DOI] [PubMed] [Google Scholar]
- 11.Lundahl B, Burke BL. The effectiveness and applicability of motivational interviewing: A practice-friendly review of four meta-analyses. J Clin Psychol 2009;65(11):1232–1245. doi: 10.1002/jclp.20638 [doi]. [DOI] [PubMed] [Google Scholar]
- 12.Alperstein D, Sharpe L. The efficacy of motivational interviewing in adults with chronic pain: A meta-analysis and systematic review. J Pain. 2016;17(4):393–403. doi: 10.1016/j.jpain.2015.10.021 [doi]. [DOI] [PubMed] [Google Scholar]
- 13.Gaume J, Magill M, Longabaugh R, Bertholet N, Gmel G, Deappen JB. Influence of counselor characteristics and behaviors on the efficacy of a brief motivational intervention for heavy drinking in young men-a randomized controlled trial. Alcoholism: Clinical and Experimental Research. 2014;38(7):2138–2147. [DOI] [PubMed] [Google Scholar]
- 14.Zanjani F, Miller B, Turiano N, Ross J, Oslin D. Effectivness of telephone-based referral care management, a brief intervention to improve psychiatric treatment engagement. Psychiatric Services. 2008;59(7). [DOI] [PubMed] [Google Scholar]
- 15.Stevens J, Hayes J, Pakalnis A. A randomized trial of telephone-based motivational interviewing for adolescent chronic headache with medication overuse. Cephalalgia 2014;34(6):446–454. doi: 10.1177/0333102413515336 [doi]. [DOI] [PubMed] [Google Scholar]
- 16.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition (beta version). Cephalalgia 2013;33(9):629–808. doi: 10.1177/0333102413485658 [doi]. [DOI] [PubMed] [Google Scholar]
- 18.Lawrence P, Fulbrook P, Somerset S, Schulz P. Motivational interviewing to enhance treatment attendance in mental health settings: A systematic review and meta-analysis. J Psychiatr Ment Health Nurs 2017;24(9–10):699–718. doi: 10.1111/jpm.12420 [doi]. [DOI] [PubMed] [Google Scholar]
- 19.Stewart WF, Lipton RB, Dowson AJ, Sawyer J. Development and testing of the migraine disability assessment (MIDAS) questionnaire to assess headache-related disability. Neurology. 2001;56(6 Suppl 1):S20–8. [DOI] [PubMed] [Google Scholar]
- 20.Kroenkea K, Strine TW, Spitzer RL, Williams JBW, Berry JT, Mokhada AH. The PHQ-8 as a measure of current depression in the general population. Journal of affective disorders. 2009;114(1–3):163–173. [DOI] [PubMed] [Google Scholar]
- 21.Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med 2006;166(10):1092–1097. doi: 166/10/1092 [pii]. [DOI] [PubMed] [Google Scholar]
- 22.Jensen MP. Enhancing motivation to change in pain treatment In: Turk DC, Gatchel RJ, eds. Psychological approaches to pain management, second edition: A practitioner’s handbook. 2nd ed. New York: Guilford Pr; 2002:71–93. [Google Scholar]
- 23.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lundahl BW, Kunz C, Brownell C, Tollefson D, Burke BL. Analysis of motivational interviewing: Twenty-five years of empirical studies. research on social work practice. 2010;20(2):137–160. Research on Social Work Practice. 2010;20(2):137–160. [Google Scholar]
- 25.Yung A, Crane T, Loescher L, Younger A, Bingham L, Thomson C. A novel model to support lifestyle interventions in cancer survivors: Undergraduate students and multimodal software platform. Society for Behavioral Medicine Annual Meeting. 2017.
- 26.MINT. Motivational interview training. 2018.
- 27.Health Education and Training Institute. MITI coding services. Health Education and Training Institute Web site. https://www.hetimaine.org/. Updated 2019.
- 28.Miller WR, Yahne CE, Moyers TB, Martinez J, Pirritano M. A randomized trial of methods to help clinicians learn motivational interviewing. J Consult Clin Psychol 2004;72(6):1050–1062. doi: 2004-21587-015 [pii]. [DOI] [PubMed] [Google Scholar]
- 29.Hettema J, Steele J, Miller WR. Motivational interviewing. Annual Review of Clinical Psychology. 2005;1(1):91–111. [DOI] [PubMed] [Google Scholar]
- 30.Lawrence P, Fulbrook P, Somerset S, Schulz P. Motivational interviewing to enhance treatment attendance in mental health settings: A systematic review and meta-analysis. J Psychiatr Ment Health Nurs 2017;24(9–10):699–718. doi: 10.1111/jpm.12420 [doi]. [DOI] [PubMed] [Google Scholar]
- 31.Syzdek MR, Green JD, Lindgren BR. Pilot trial of gender-based motivational interviewing for increasing mental health service use in college men. Psychotherapy. 2016;53(1):124–129. [DOI] [PubMed] [Google Scholar]
- 32.Buckner JD, Schmidt NB. A randomized pilot study of motivation enhancement therapy to increase utilization of cognitive–behavioral therapy for social anxiety. Behaviour research and therapy. 2009;47(8):710–715. [DOI] [PubMed] [Google Scholar]
- 33.Leon AC, Davis LL, Kraemer HC. The role and interpretation of pilot studies in clinical research. J Psychiatr Res 2011;45(5):626–629. doi: 10.1016/j.jpsychires.2010.10.008 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Miller FA, Alvarado K. Incorporating documents into qualitative nursing research. J Nurs Scholarsh 2005;37(4):348–353. [DOI] [PubMed] [Google Scholar]
- 35.Kaplan WA. Can the ubiquitous power of mobile phones be used to improve health outcomes in developing countries? Global Health. 2006;2:9-8603-2-9. doi: 1744-8603-2-9 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kazdin AE, Rabbitt SM. Novel models for delivering mental health services and reducing the burdens of mental illness. Clinical Psychological Science. 2013;1:170–191. [Google Scholar]
- 37.Mohr DC, Vella L, Hart S, Heckman T, Simon G. The effect of Telephone-Administered psychotherapy on symptoms of depression and attrition: A Meta-Analysis. Clinical Psychology. 2008;15(3):243–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jenkins-Guarnieri MA, Pruitt LD, Luxton DD, Johnson K. Patient perceptions of telemental health: Systematic review of direct comparisons to in-person psychotherapeutic treatments. Telemed J E Health. 2015;21(8):252–260. [DOI] [PubMed] [Google Scholar]
- 39.Syzdek MR, Addis ME, Green JD, Whorley MR, Berger J. A pilot trial of gender-based motivational interviewing for help-seeking and internalizing symptoms in men. Psychosocial Men and Masculinity. 2014;15(1):90–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gewirtz A, Minen M. Adherence to behavioral therapy for migraine: Knowledge to date, mechanisms for assessing adherence, and methods for improving adherence. Curr Pain Headache Rep 2019;23(1):3-019-0739-3. doi: 10.1007/s11916-019-0739-3 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Matsuzawa Y, Lee YSC, Fraser F, et al. Barriers to behavioral treatment adherence for headache: An examination of attitudes, beliefs, and psychiatric factors. Headache 2019;59(1):19–31. doi: 10.1111/head.13429 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Minen M, Azarchi S, Sobolev R, et al. Factors related to migraine patients’ decisions to initiate behavioral migraine treatment following a headache specialist’s recommendation: A prospective observational study. Pain Medicine. 2018;19(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Smedslund G, Berg RC, Hammerstrøm KT, et al. Motivational interviewing for substance abuse. Cochrane Database Syst Rev 2011;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stieger M, Nißen M, Rüegger D, Kowatsch T, Flückiger C, Allemand M. PEACH, a smartphone- and conversational agent-based coaching intervention for intentional personality change: Study protocol of a randomized, wait-list controlled trial. BMC Psychology. 2018;6(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Westra HA, Dozois DJA. Preparing clients for cognitive behavioral therapy: A randomized pilot study of motivational interviewing for anxiety. Cognitive Therapy and Research. 2006;30:481–498. [Google Scholar]
- 46.Westra HA, Arkowitz H, Dozois DJA. Adding a motivational interviewing pretreatment to cognitive behavioral therapy for generalized anxiety disorder: A preliminary randomized controlled trial. J Anxiety Disord 2009;23(8):1106–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Arkowitz H, Westra HA, Miller WR, Rollnick S. Motivational interviewing in the treatment of psychological problems. New York: Guilford; 2018. [Google Scholar]


