Abstract
Background
The coronavirus brought the world’s leaders to the center of the media stage, where they not only managed the COVID-19 pandemic but also communicated it to the public. The means they used to communicate the global pandemic reveal their strategies and the narratives they chose to create in their nation’s social consciousness. In Israel, the crisis broke out after three election cycles, such that the government in charge of the crisis was an interim government under the leadership of Prime Minister Benjamin Netanyahu, who was operating under three criminal indictments. This study sought to examine the ways in which Prime Minister Netanyahu and two senior Israel Ministry of Health officials—Director General Moshe Bar Siman Tov and Prof. Sigal Sadetsky, Head of Public Health Services—communicated information about the health crisis in Israel during what has been termed the first wave and the beginning of the second wave.
Methods and Sample
The research adopted qualitative methods (discourse, content and thematic analysis) to analyze the communication strategies and compare them to health and risk communication. Triangulated data collection from different data sources was used to increase the credibility and validity of the results. The research sample comprised the following sources from March 3 through June 21, 2020: transcripts of 19 press conferences and 12 press interviews, 95 emergency regulations signed by Prime Minister Netanyahu, and 52 articles in major Israeli newspapers.
Results
Netanyahu and the Health Ministry Director General used an apocalyptic narrative to communicate COVID-19 to the public. The main strategies used in constructing this narrative were intimidation, lack of information transparency, giving the public conflicting instructions contrary to the health and risk communicating approach, and using a health crisis to promote political intentions and actions.
Conclusion
Communicating health crises to the public, particularly ongoing crises like COVID-19, requires that leaders implement the health and risk communication approach and create a cooperative narrative that does not rely on a strategy of intimidation, but rather on empathy and on fact-based and transparent information.
Keywords: COVID-19, health and risk communication, Prime Minister Netanyahu, Israeli public, qualitative research
Introduction
On January 30, 2020, the World Health Organization (WHO) declared the coronavirus outbreak to be a Public Health Emergency of International Concern (PHEIC).1 Since then, the rapidly evolving 2019 coronavirus disease (COVID-19) pandemic has been placing an overwhelming burden on health systems, motivating authorities to respond with effective and appropriate interventions, policies and messages.2
The literature discussing health and risk communication and media during crises points to the importance of transparency in conveying information to the public.3,4 According to the literature, when the public finds itself living under conditions of uncertainty, it wants the leaders to provide updated information. In addition, people seek useful information that explains what they should do to protect themselves and their surroundings. Such information should be clear despite its complexity. Conflicting messages from authorities motivate the public to continue searching for information from unofficial sources.5
In addition, public trust in authorities and leaders is crucial, particularly during a crisis that requires public cooperation. Public confidence can only be built and established when leaders demonstrate caring and empathy, dedication, commitment and equity.6,7 Trust and credibility become eroded when experts disagree, when risk management organizations are not coordinated, when no one listens and there is no dialogue and public participation, and when no one seems willing to acknowledge risks or disclose information in a timely manner.8,9
Reviews of public health emergency responses indicate that health leaders require the following leadership skills: competence in public health science; decisiveness along with flexibility; ability to maintain situational awareness and provide situational assessment; ability to coordinate diverse participants across very different disciplines; communication skills; and the ability to inspire trust.10
According to Agnes Binagwaho,
This pandemic highlights the need for leaders to be educated on implementation science principles to be able to make evidence-based decisions through a multi-sectoral, integrated response, with consideration for contextual factors that affect implementation.11
Yet such skills are not routinely taught in public health curricula, leading to a discrepancy between the textbooks and what happens in the field.12,13
Furthermore, despite the importance of and need for risk communication expertise, all over the world funding for professional communication staff is low. According to Laurie Garrett,
If governments, agencies, and health organizations want people at risk of infection to respond to COVID-19 with an appropriate level of alertness, to cooperate with health authorities, and to act with compassion and humanity, they must be willing to fund their messengers.14
COVID-19 has created health, political and global challenges. The pandemic forced world leaders to cope with uncertainty and in many cases generated crises and tremendous losses for health, welfare and economic systems. As Laurie Garrett stated,
Stock markets worldwide are showing record-breaking plummets, global supply and production systems are in danger of collapse, and in some places panic has gone viral—even where the virus, itself, has not.14
The economic consequences may go beyond the unemployment brought on by the closures.15–18 Indeed, the uncertainty regarding health may be translated into uncertainty in the insurance world.19
Because the pandemic broke out during the internet revolution and the social network era, in many countries public relations about the virus generated a new social language and a new propaganda campaign. During the crisis, leaders communicated information and messages to the public via press conferences and social media platforms such as YouTube, Facebook and Twitter that circumvented journalists. Eight out of nine (88.9%) G7 world leaders have verified and active Twitter accounts, with a total following of 85.7 million users. Out of 203 viral tweets about COVID-19, 166 (82.8%) were classified as “informative,” with 48 of these (28.6%) providing weblinks to government-based sources, while 19 (9.4%) were “morale-boosting” and 14 (6.9%) were “political.” The numbers of followers and the viral tweets were not strictly related.20
In their efforts to manage the crisis, not only did world leaders take center stage, they also communicated their messages to the entire world,21 causing them to compete with each other over which leader made the most educated decisions and enlisted public cooperation. According to Jill Rutter, senior fellow at the London-based Institute for Government,
The main questions for these leaders is, can they convey a clear message and give people the reassurance they need while admitting this is an incredibly fast-moving, difficult world of real unknowns?22
Every world leader had a different relationship with the traditional media, and each one of them adopted a different strategy in communicating information about the pandemic to the public.22 US President Donald Trump first denied that the pandemic existed. After that, he sent the public erratic messages and engaged in complex relations with the traditional media, accusing them of distorting his words. Despite his highly charged relations with the media, his press conferences became the focus of American television and print news, which Donna Ladkin claims are ”dominated by one man: Donald Trump.”23 The US news covered every word Trump said, even though he disregarded the important issues of morbidity monitoring and field testing and “forgot that more people are now dying of COVID-19-related complications every day than of cancer or heart disease.”23
Criticism was also directed at UK Prime Minister Boris Johnson for his inconsistent messages to the public. In contrast, German Chancellor Angela Merkel was praised by the media for being transparent with the public and transmitting messaged anchored in facts. So was New Zealand’s Prime Minister Jacinda Ardern, who chose a strategy of public inclusion. Former New Zealand Prime Minister Helen Clark observed that Ardern “doesn’t preach at them; she’s standing with them.” Ardern outlined the dilemmas and challenges and instituted a policy of welfare and empathy during the crisis. For example, she announced 20% salary cuts for herself and the ministers in her government.24
Government willingness to be led by expertise and efforts to mobilize the population and facilitate coping are key leadership practices that serve to build the trust in leadership needed for the transformative collective action demanded by a pandemic.25 Alastair Campbell wrote in The Independent: ‘Ardern is surely one of, if not the, standout leaders of this crisis’.26 A study that compared male-led and female-led countries during the COVID-19 pandemic found that half of all countries and 63% of female-led countries launched coordinated information campaigns before their first confirmed case of COVID-19. Among the rest, time to implementation was one week shorter on average in countries with women leaders.27
Beyond the implications of COVID-19 for national and global economies, the crisis exposed deep social conflicts in many countries. For example, during the crisis the United States also had to deal with the murder of George Floyd and the ensuing political and ethnic divide.28 Indeed, COVID-19 prompted a major question about leadership in times of crisis: how to achieve a balance between important public health issues and the preservation of individual liberty? The virus cares little about whether nations are democratic or authoritarian. Nevertheless, democratic governments already used the virus to launch an onslaught on freedoms, while regimes that were authoritarian to begin with used the pandemic to grab even more power. For example, the governments of Poland and Hungary managed to turn the crisis into an opportunity to install their regimes even more solidly and to harm their political rivals.29 Hungarian Prime Minister Viktor Orban used the pandemic as an excuse to cancel all elections and remain in power indefinitely. He invoked broad powers to limit air travel and individual movements. Yet these restrictions have no expiration date, nor was there any parliamentary review of his actions. Orban stated:
We are fighting a two-front war. One front is called migration, and the other one belongs to the coronavirus. There is a logical connection between the two, as both spread with movement.30
Serbian President Aleksandar Vucic pushed for similar extreme measures and relied on heavily armed police patrols to enforce his edicts. He too undermined parliamentary oversight of his actions and assumed the right to rule by decree.30
Israel’s management of the COVID-19 crisis differs from that of other countries because Israel was in the midst of a deep constitutional crisis that affected its management of the pandemic. During the period under examination in this study, the COVID-19 situation in Israel was being managed by an interim prime minister operating under three criminal indictments, after three election cycles in which no clear victor emerged.31 The pandemic generated a multidimensional crisis in Israel by endangering public health, undermining economic and social resilience, challenging effective governance and even providing a cover for processes that could potentially harm democratic values.32
This study sought to examine the ways in which Prime Minister Netanyahu and two senior Israel Ministry of Health officials—Director General Moshe Bar Siman Tov and Prof. Sigal Sadetsky, Head of Public Health Services—communicated information about the health crisis in Israel during what has been termed the first wave and the beginning of the second wave. The study’s objective was to use the health and risk communication approach to examine how Israeli leaders managed health and risk communication and discourse about COVID-19 and communicated the guidelines to the public.
Materials and Methods
Research Framework
This study employed qualitative research methods to analyze the communicative strategies adopted by Israeli officials to manage the COVID-19 crisis. Data triangulation methods33–35 were used to increase the credibility and validity of the results. Data were collected from different sources: press conferences and press interviews, legislation, and newspaper articles that dealt with the COVID-19 guidelines in Israel. All the data sources were analyzed simultaneously36,37 to integrate the perspectives used to communicate the health risks of COVID-19 to the Israeli public.
Discourse analysis, content analysis and thematic analysis were used to analyze the communication strategies, while comparing them to the health and risk communication approach. Through discourse analysis38–40 we established that speech is not a direct representation of human experience, but rather an explicit linguistic tool constructed and shaped by numerous social and ideological influences. The method capitalizes on critical inquiry into language and how it is used to uncover the societal influences underlying behavior and thoughts. We applied discourse analysis to the language and strategies adopted to communicate the COVID-19 health crisis in Israel, particularly by the speakers at press conferences (see the Analysis section for the protocol used for discourse-based discourse).
Content analysis41 was used to analyze the ways in which the COVID-19 guidelines were communicated to the Israeli public according to the health and risk communication approach. Thematic analysis42 of the texts of all spokespersons was used to develop the main themes in the analysis.
Research Sample
The research sample included the following sources: transcripts of press conferences and press interviews on Israel’s three major television channels (Channel 12, Channel 13 and Kan 11) with the key figures who managed the COVID-19 crisis during what was termed the first wave and the beginning of the second wave; emergency regulations signed by Prime Minister Benjamin Netanyahu; and articles in two major Israeli newspapers (Haaretz, including its economic magazines, and YNET) during the COVID-19 crisis that covered instructions to the public. The sampling method was direct sampling43 of all the materials from March 3, 2020 to June 21, 2020, a period that encompassed the pre-closure and closure periods, the exit strategy and the COVID-19 routine, and the beginning of the discourse on the second wave.
The press conferences of Prime Minister Benjamin Netanyahu, Health Ministry Director General Moshe Bar Siman Tov and Head of the Health Ministry’s Public Health Services Prof. Sigal Sadetsky underwent discourse analysis. In addition, we analyzed the comments of Health Minister Yaakov Litzman, who was absent most of the time and not actively involved in managing and communicating COVID-19 information to the public.
The research sample included instructions issued to the public as well as 95 emergency regulations signed by Prime Minister Netanyahu during the COVID-19 crisis in Israel.44 Sampling of press articles about COVID-19 yielded 126 relevant articles, 52 of which focused on communicating instructions and information to the public. Sampling was based on key search words (eg, instructions to the public, quarantine, closure, tests, emergency regulations, masks, social distancing, essential workers, purple badge standard, information transmission, public transparency and more). Table 1 describes the sample in detail.
Table 1.
Research Sample
| Press Conferences: N=19 | Prime Minister Benjamin Netanyahu Participated in 19 Press Conferences, Health Minister Yaakov Litzman in 6 Press Conferences, Health Ministry Director General Moshe Bar Siman Tov in 7 Press Conferences, and Head of Health Ministry Public Health Services Prof. Sigal Sadetsky in 2 Press Conferences. |
| Interviews in the Media – Individual appearances on news broadcasts on one of Israel’s three main television channels (Channel 12, Channel 13 and KAN): N=12 (Channel 12: N=6; Channel 13: N=2; KAN: N=4) | Health Ministry Director General Moshe Bar Siman Tov: N=11 (Channel 12: N=5; Channel 13: N=2; KAN: N=4) |
| Head of Health Ministry’s Public Health Services Prof. Sigal Sadetsky: N=1 (Channel 12: N=1) | |
| Emergency Regulations | N=95 |
| Articles in the Press: N=52 | YNET: N=19; Globes: N=6; Haaretz: N=13; Calcalist: N=5; The Marker: N=9 |
Analysis
The research findings were analyzed using the discourse analysis language-dominant view of language,38–40 content analysis41 and thematic analysis.42 In the first stage, we transcribed all the press conferences and press interviews. In the second stage, we constructed a research question protocol based on content analysis patterns and on the health and risk communication approach3,4 to content and means of conveying information, as described below:
What type of language (terms, words) do the policymakers use to convey the information to the public?
What communication strategies do they use to communicate the information (eg, intimidation/empathy/identification)?
What hidden benefit do the spokespersons gain from using a particular strategy?
What is the social and political context in which the messages are communicated?
What are the main issues/topics emerging from the instructions?
Do the spokespersons communicate the information to the public using scientific language (eg, references to uncertainty)?
Are the guidelines structured, coherent and based on the health and risk communication approach from the literature?
How do the spokespersons appeal to the values and conventions of their audience?
Do the spokespersons appeal to different sub-groups in the population or do they direct their message at a specific audience?
In the third stage we analyzed the materials according to the protocol questions. We considered each text of each spokesperson separately. The fourth stage entailed integrative content analysis41 and thematic analysis42 of the texts spoken by all the spokespersons. In the fifth stage we constructed two discourse axes. The first axis—the pandemic axis—contained the spokespersons’ strategies in conveying information. This axis was parallel to the second axis—the political axis. These axes are described in detail in the Results section. In the sixth stage, we analyzed press articles that covered public guidelines and emergency regulations based on the above protocol questionnaire and specifically questions 5–9. We then constructed two additional discourse axes as described in detail in the Results section: communicating information to the public (third axis) and the parallel axis of recommendations for conveying information according to the health and risk communication approach (fourth axis).
Validity and Reliability
This research is based upon qualitative research methods and data triangulation. We examined a variety of texts to analyze the communications strategies in order to facilitate broader and fuller understanding.33 The data were collected and processed simultaneously so as to generate integrated perspectives and ways of understanding how the information was conveyed to the public.36 This data triangulation increases the validity and reliability of the research and enhances the interpretation of the findings.37
Throughout the course of the study, we stored all relevant information, from transcribing the press conferences to screening the press articles and analyzing the findings through arriving at the final results and conclusions.45 Each researcher analyzed the sample texts separately based on the aforementioned research protocol. After that, the researchers discussed the analysis using the inter-rater reliability method to arrive at consensus.46
Results
National Emergency Narrative: Pandemic in a Political Context
Netanyahu adopted a centralist approach in managing and communicating the crisis. During the period of this research, he gave prime time televised press conferences almost every day to announce additional guidelines and restrictions dictated by COVID-19, without giving journalists any opportunity to ask questions. The two senior Ministry of Health officials mentioned above—Moshe Bar Siman Tov and Prof. Sigal Sadetsky—were with him at these press conferences, while Health Minister Litzman, who belongs to the ultra-Orthodox stream of Judaism, was absent from most of them. Analysis of the press conferences and interviews reveals that Netanyahu generated a national emergency narrative for his listeners and the entire Israeli public.
Netanyahu’s target audience can be divided into two: The first group comprises the general public, whom Netanyahu and the senior Ministry of Health officials attempted to convince that this is a time of emergency so they must listen and conform to the stringent guidelines. During the first wave, these measures included closing schools, higher education institutions and workplaces, a general public closure, and passing a law giving the prime minister broad powers during the crisis without approval or supervision from the Knesset (Israeli parliament).47 The second targeted group consisted of Netanyahu’s political rivals, whom Netanyahu attempted to convince that they must join forces to cope with the national emergency brought on by COVID-19.
It is important to note that at the time this research was conducted, the COVID-19 crisis in Israel was being managed by an interim government led by an interim prime minister operating under three criminal indictments, after three election cycles in which no clear victor emerged. In effect, Israel’s parliament had stopped functioning normally. Netanyahu’s declared objective was to form a unity government with the Blue-White party led by Benny Gantz, former Chief of the General Staff of the Israel Defense Forces. Such a unity government would enable Netanyahu to remain in office as Israel’s prime minister.
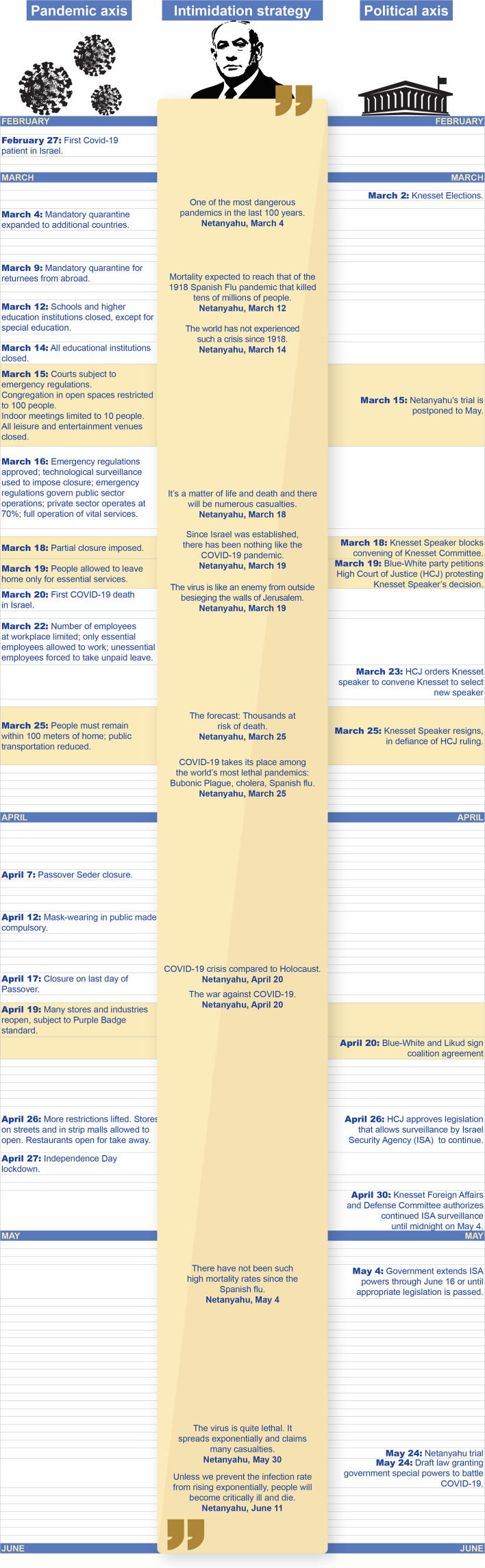
Our analysis shows that to construct this national emergency narrative for these two target audiences and to link political and health concerns, Netanyahu adopted three strategies: 1) a strategy of intimidation; 2) a public relations strategy to reinforce his image as a leader working for the good of the public and thus to attract his political rival, who would identify with these intentions; 3) a strategy of generating symbiosis between health and political concerns by embedding calls for a unity government in press conferences dedicated to the COVID-19 pandemic. Analysis of the emergency guideline timetable and the political timetable points to parallels between the health and political axes (see Figure 1). In the following sections we describe these three strategies in detail.
Figure 1.
Infographic depicting emergency guidelines timetable and political timetable.
First Strategy: Use of Intimidation
Analysis of the press conferences shows that intimidation48–50 was the primary strategy used by Prime Minister Netanyahu and the Ministry of Health Director General to convey the guidelines about the COVID-19 pandemic to the public. To this end, the spokespersons made use of military language51 to link the health crisis to a state of war. Moreover, the spokespersons predicted high morbidity and mortality rates and created algorithms and images to link the pandemic to other health or social catastrophes throughout human history. The thematic analysis of each of these strategies is detailed below.
Use of Military Language
In the press conferences and interviews the spokespersons used military language51 to communicate the guidelines to the public. Figure 2 shows the integration between military language and the language of COVID-19.
Figure 2.
Infographic depicting frequency of words used by the spokespersons in the press conferences and interviews.
For example, Netanyahu declared the current situation to be a state of war.
This time we identified the danger in time. We made important decisions, such as closing the nation’s borders, and we harnessed all the nation’s systems to the war on corona. (Netanyahu, April 4, 2020)
According to Netanyahu, the coronavirus is an “external enemy” that must be battled or destroyed.
… after dealing with the outer wrapping by tightening and closing off external access to the country, we must now change the routine of life … to cope with the crisis caused by a virus that seeks to attack us from the outside. (Netanyahu, March 11, 2020)
Hence, Netanyahu declared that the entire Israeli public must change its daily routine and adopt an emergency routine.
We have reached a historic moment of emergency, a national emergency, an international emergency … now is the time for an emergency government for a limited period, so that together we can fight to save the lives of thousands of citizens. (Netanyahu, March 12, 2020)
According to Netanyahu, the public should also enlist in the all-out war against the COVID-19: “Every one of you is a soldier in the battle against corona” (Netanyahu, March 19, 2020). After declaring that “in essence, this war is a civilian war,” Netanyahu went on to tell his listeners about the enemy they are fighting: a dangerous, evasive, unpredictable and invisible enemy that must be ambushed and attacked using all possible means.
We are now at war with an invisible enemy, we are at battle. Our enemy is an invisible virus. To defeat it, and we can defeat it … we must find it, just as in any war you must find the enemy. (Netanyahu, March 14, 2020)
Predicting High Morbidity and Mortality Rates
At the onset of the first wave, Netanyahu and Health Ministry Director General Bar Siman Tov cited high morbidity (“many thousands”) and mortality (“tens of thousands”) rates. Note that as of the writing of this paper, these rates have not been reached. On November 21, 2020 the death toll in Israel was 2,754, mostly older people or those with preexisting conditions.52–54
… according to our scenarios many thousands of Israeli citizens may die from the disease … We will try to distribute the patients, flatten the curve … many people will still die and even more will get sick. (Bar Siman Tov, March 18, 2020)
In predicting the morbidity and mortality rates in Israel, Netanyahu said:
In two weeks, we are liable to find ourselves with thousands of patients, many of whom are at risk of dying. (Netanyahu, March 25, 2020)
Netanyahu spoke about the rising contagion rate in terms of an exponential geometric progression, despite the scientific controversy surrounding this notion.
We must remember one thing: the virus is very lethal. Without protective measures, it will spread exponentially and will claim many casualties. (Netanyahu, May 30, 2020)
Analogies and Comparisons to Other Health and Social Catastrophes Throughout Human History
Analogy to the Spanish Flu Pandemic
From the outset of the crisis, Netanyahu compared the COVID-19 pandemic to the Spanish flu pandemic. The Spanish flu pandemic began in February 1918 and continued through April 1920, infecting 500 million people, about a third of the world’s population at the time, in four successive waves. The death toll is typically estimated to have been somewhere between 17 million and 50 million, making it one of the deadliest pandemics in human history.55 The Spanish flu mainly affected people between the ages of 20 and 40, differentiating it from other pandemics in which most of those who died were elderly and those with preexisting conditions. Unlike the Spanish flu, the COVID-19 pandemic is ongoing, and its morbidity and mortality rates differ. As of November 21, 2020, COVID-19 is still spreading across the globe, with more than 57.3 million cases and 1,368,000 deaths.56 Another difference is that COVID-19 has a more deleterious impact on the older population and those with suppressed immune systems, while the Spanish flu affected mainly younger people. Despite these vast differences, Netanyahu chose to compare these two pandemics.56
The most recent pandemic that resembled what is going on now is the Spanish flu pandemic that raged through the world in 1918 … Tens of millions of people died during that pandemic …. (Netanyahu, March 12, 2020)
There has not been such extensive mortality from a pandemic for a hundred years, since the 1918 Spanish flu pandemic, which by the way lasted three years, with a disastrous second wave. (Netanyahu, May 4, 2020)
COVID-19 Pandemic is Threatening to Destroy the State of Israel
Netanyahu used analogies to historical pandemics to demonstrate the extent of the catastrophe, one that is not only threatening people’s health but also threatening to bring about the destruction of the State of Israel.
Citizens of Israel, the coronavirus is taking its place among other deadly pandemics that have ravaged humanity: the Bubonic Plague, cholera, the Spanish flu at the outset of the 20th century. When these pandemics raged, we did not have a state. (Netanyahu, March 25, 2020)
Analogy to the Holocaust
Prime Minister Netanyahu also compared the epidemiological crisis caused by COVID-19 to the Holocaust. The Holocaust, also known as the Shoah, was the genocide of European Jews during World War II. Between 1941 and 1945, Nazi Germany and its collaborators systematically murdered some six million Jews, around two-thirds of Europe’s Jewish population. Netanyahu’s reference to the COVID-19 pandemic and to the Holocaust in the same speech—his keynote address at Yad Vashem, Israel’s official memorial to the victims of the Holocaust, on Holocaust Remembrance Day—created an analogy to extermination and destruction in the consciousness of many Israelis. Indeed, in the consciousness of the Jewish people the Holocaust is the most traumatic and formative event in modern history. Here is an excerpt from Netanyahu’s Holocaust Remembrance Day speech:
I heard Ka-Tsetnik and other survivors say, you will never be able to understand what we went through there. They were right … nothing resembles the Holocaust. This is also true regarding the global corona crisis … the greatest challenge to humanity since World War II. (Netanyahu, April 20, 2020)
Second Strategy: Public Relations in Managing the Pandemic
From the first attempts at dealing with the pandemic, Netanyahu frequently mentioned Israel’s successful management of the crisis. During all the press conferences, Netanyahu and Health Ministry General Director Bar Siman Tov claimed that Israel’s management of the COVID-19 crisis was superior to that of other countries.
The morbidity rate in Israel relative to the size of the population is one of the lowest in the Organization for Economic Co-operation and Development (OECD), as is the morbidity rate among those who are infected. (Netanyahu, April 18, 2020)
… Israel’s achievements in the battle against corona serve as a model for many countries. The world looks at us with admiration. (Netanyahu, May 4, 2020)
Our analysis shows that Netanyahu related to Israel’s success in managing the COVID-19 crisis as his personal success and that of a handful of people working with him. Both Netanyahu and Director General Bar Siman Tov made prevalent use of the first person “I” in describing COVID-19 management efforts. The word “I” appeared 667 times in the analyzed texts (see Figure 2). This association between the state and the first person “I” appears throughout the discourse used to communicate the pandemic.
… there have been very steep increases … the virus is not surrendering … I can say that thanks to the timely decisions we made and to the cooperation from you, the citizens of Israel, we have prevented the spread of the pandemic … (Netanyahu, June 11, 2020)
Third Strategy: Creating Symbiosis Between Health and Political Matters by Interweaving Political Calls for a Unity Government into Press Conferences About the COVID-19 Pandemic
Our analysis shows that during all the press conferences Netanyahu created an interface between health and political matters. The narratives used in these press conferences were similar in structure: At the beginning of the speech Netanyahu’s remarks referred to the COVID-19 health crisis. After that, he made a political appeal to his political rivals to “shoulder the burden” and establish a national emergency government. The press conferences and interviews dealing with the COVID-19 pandemic included about 11 political mentions (see Figure 1 showing the synchronization between the health and political axes).
I want to thank those on the other side of the political divide … They understand that we are facing a historic emergency … I call for establishing such a government right now, tonight, a national emergency government …. (Netanyahu, March 12, 2020)
We must establish a unity government; we must form a national emergency government. I say to the Blue-White party members, shoulder the burden, we will bear the burden together, we will lead together, and together we will save our people and our nation. (Netanyahu, March 19, 2020)
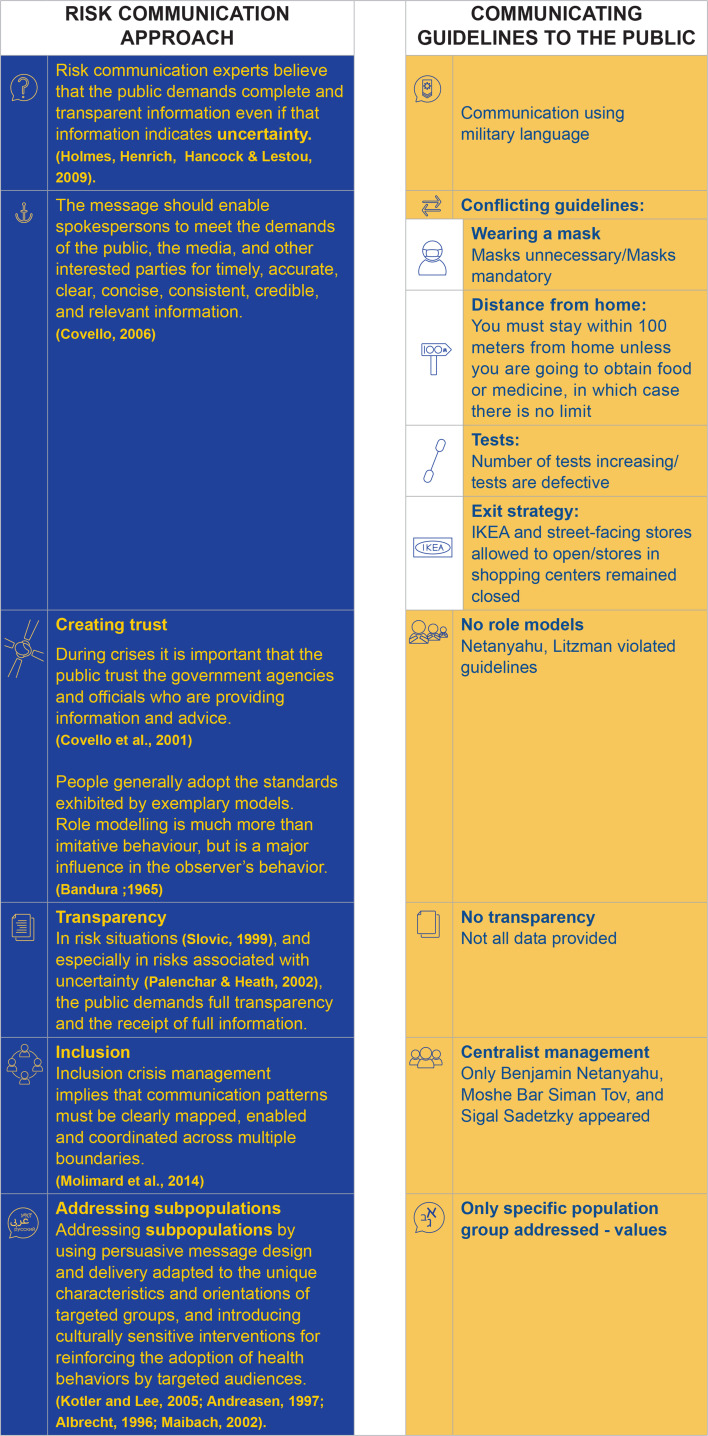
Public Guidelines from the Risk Communication Approach Perspective
Several major issues emerged from the textual analysis of the public guidelines. In the following sections, first we outline these issues: conflicting guidelines, use of certain language, lack of transparency in publicized information, lack of role models, references to the values of the Jewish population and not of other Israeli population groups such as the Arab population, and cautious references to sub-groups in the population with high infection rates. In Figure 3 we compare the method used in communicating these guidelines to the risk communication approach.
Figure 3.
Infographic comparing the method used in communicating the COVID-19 guidelines in Israel and the risk communication approach.
Issues and How They are Conveyed to the Public
Contradictory Instructions
Throughout the COVID-19 crisis, the public received contradictory instructions that constantly changed and were not accompanied by detailed explanations based on scientific consensus.
Wearing Masks
At first Netanyahu claimed there was no need to wear a mask in public.
I want you to see what it means to put a scarf or a tissue on your face. Look, here’s what happens if someone sneezes. The disease is transmitted, these are saliva droplets … You don’t need masks, this is sufficient …. (Netanyahu, March 11, 2020)
I ask you to maintain good hygiene, including using tissues. Masks are not the main thing. This is the main thing, to avoid sneezing, to prevent any contact with your face by using a tissue. (Netanyahu, March 12, 2020)
After some time went by, wearing a mask in public became compulsory (see timetable in Figure 1), and fines were imposed on those who did not conform to the regulations. While this change in the guidelines was not supported by any unequivocal scientific evidence, Netanyahu began advocating wearing a mask in public.
Citizens of Israel, we ask that you all wear masks in public. If you do not have a mask, use a scarf or any other face covering to reduce spreading the virus to others. (Netanyahu, April 1, 2020)
Wearing masks in public is compulsory and in fact this may be the most important means. (Bar Siman Tov, April 24, 2020)
Testing
At the beginning of the crisis, both the Health Ministry’s Director General and the Head of Public Health Services claimed they do not believe in testing and prefer the use of quarantine and closure.
Even if we do widespread laboratory testing, we will not be able to locate everyone and will not be able to stop the morbidity because we know that … people can be infected without experiencing any symptoms at all. (Sadetsky, March 14, 2020)
Later they claimed that even though they “do not believe in testing” they will extend testing in Israel.
Tests are a very important tool, but they are not a means of treating the situation. The solution to this pandemic is not testing but rather quarantine …. (Sadetsky, March 18, 2020)
After public criticism indicating that testing should target medical teams and serve the Health Ministry in assessing morbidity in Israel,57,58 it became apparent that the Ministry’s epidemiological testing system was not functioning and that there was a grave shortage of serological tests. Thus, the reason for so little testing was not only professional but also reflected overall mishandling of the situation.
No laboratory can handle 10,000 tests per day. We are working on it … they are trying to help us increase the number of tests in Israel. (Bar Siman Tov, April 7, 2020)
We have to cope with a worldwide shortage, the things we need are in short supply across the globe, whether it’s swabs or the new word, reagents, that everyone’s talking about. (Bar Siman Tov, April 3, 2020)
Distance from Home
After a general closure was declared, people were restricted to remain within a certain distance of their homes. On the one hand, they were permitted to go out to shop for food, medicine and the like, while on the other hand the instruction was to remain within 100 meters of home (a distance that did not enable many people to go out shopping).
Stay within 100 meters of home and leave only for a short period of time. According to the regulations, you can enter the public space for the following reasons only: going to work; obtaining food, medicines, essential items and essential services; obtaining medical services.59
Exit Strategy
On April 18, 2020 when a decision was reached to end the total closure, it became apparent that there was no formulated exit strategy. Some places of business were granted permission to open under the “purple badge” standard60 while others were not, while the reasons remained unclear. For example, the government allowed the IKEA chain store to open on April 23 but prohibited other stores and shopping centers from opening. In addition, government offices issued conflicting and unclear instructions regarding the purple badge standard, leading many business owners to deliberate whether or not they were allowed to open their businesses.61–66
Conveying Uncertainty as Certainty
The spokespersons chose to present their positions from a position of certainty despite the uncertainty and scientific controversies surrounding how to cope with COVID-19. When the crisis first began, the spokespersons acknowledged the uncertainty entailed in their decision-making.
We are in the midst of a serious, complex, unfolding and dynamic event marked by a high degree of uncertainty. But within this uncertainty, we are persisting in following a consistent strategy that we are upgrading as the event unfolds. (Sadetsky, March 18, 2020)
Yet the spokespersons later abandoned this language of uncertainty, which is the primary language of scientific discourse, and shifted to the language of certainty that marks military discourse (see Figure 2).
Lack of Transparency in Conveying Information
During the entire crisis, the general public, the government ministers and even those working in the Ministry of Health did not have access to essential information about COVID-19. Only those in charge of the crisis along with a few select organizations had access to the raw data collected by the Health Ministry. Morbidity and mortality rates segmented according to socio-demographic factors, including pre-existing conditions, were not publicized to the general public.67
Social organizations came out against the Health Ministry, claiming that coping with the coronavirus requires transparency. Note that in many countries, including those that were winning the battle to eradicate the virus (such as South Korea, Singapore and Taiwan), the principle of transparency served as a guiding light to policymakers. Maintaining maximum transparency is essential to generate the trust needed to ensure that citizens cooperate with government regulations.68,69
Lack of a Role Model
During the crisis it became apparent that public leaders were not strictly conforming to the guidelines they issued to the public, thus serving as negative role models. For example, before Health Minister Litzman and his wife were diagnosed with the coronavirus,70 the minister was seen praying in the Beit Yisrael synagogue in Jerusalem, located on the street where he lives, and in the home of the Gur Hassid. This behavior was contrary to Ministry of Health guidelines prohibiting people from congregating during prayers, even in open spaces, and contrary to instructions issued by religious and ultra-Orthodox leaders stating that every individual should pray alone at home.71,72
In another example, the government decided upon a total closure on the eve of the Passover holiday, and the prime minister announced that people should celebrate the holiday only with immediate family members living in the same house. The Israeli public listened and obeyed these guidelines. Yet Prime Minister Benjamin Netanyahu and President Rivlin chose to disobey these directives by hosting their children, who do not live in the same house with them, for the Passover Seder.73
Appealing to the Values of the Jewish Population
In their remarks, the crisis leaders headed by Netanyahu appealed to the values of Jewish society and used Israel’s holidays to demonstrate the importance of the people’s spirit in the victory over external enemies who sought to destroy them.
The month of Nissan that begins tonight, the month of spring marking the exodus from Egypt, reminds us that our people faced grave dangers. This gives us strength; it gives us hope. We survived Pharaoh … we will survive corona as well. (Netanyahu, March 25, 2020)
Strict adherence to the commandments of the Passover offering, matzah and bitter herbs, to social distancing, hygiene and masks, these are our Passover offerings, our matzah and bitter herbs, they are very bitter (laughs) but should be strictly obeyed. (Netanyahu. April 18, 2020)
When directly appealing to Arab society in his press conferences, Netanyahu used the words “non-Jews,” “non-Jewish ethnic groups,” “religious groups” and “certain groups.” Thus, even though the Christian holiday of Easter coincided with Passover, the prime minister disregarded it. In appealing to the Muslims during the month of Ramadan, Netanyahu called upon them to obey the guidelines “like the Jews did” during Passover.
What I just said is also applicable to the holidays of non-Jewish groups. We extend holiday greetings to everyone, but we also expect them to conform to the same lifesaving regulations. (Netanyahu, March 30, 2020)
With respect to the holidays of non-Jewish groups, celebrations should be within the nuclear family living in the same house. (Netanyahu. April 1, 2020)
Cautious Appeal to Orthodox and Ultra-Orthodox Sub-Groups
Infection and morbidity rates in the Orthodox and ultra-Orthodox localities were high. Yet the prime minister chose to address all sub-groups in the population similarly by issuing a warning rather than explicitly referring to the high morbidity rates in these religious communities.
Certain groups are demonstrably disregarding and even belittling the clear guidelines we issued. Not everyone. Most people are obedient, ultra-Orthodox and secular people, Jews and non-Jews. (Netanyahu, March 30, 2020)
How the Guidelines Were Conveyed to the Public vs the Risk Communication Approach
According to the risk communication approach, care must be taken to provide absolute transparency in conveying information, including conveying any existing uncertainties. In addition, announcements of public guidelines should reveal the rationale upon which they are based, and the information should be useful, coherent and anchored in facts. To establish public trust, the leadership should serve as a reliable role model and should appeal to various sub-groups in the population. The instructions to the public outlined above did not meet these criteria. Figure 3 compares the axis of communicating guidelines to the public to the axis outlining the risk communication approach, which is backed up by excerpts from the professional literature.
Discussion
The coronavirus brought the leaders of the world to the center of the media stage. Most of them chose not only to manage the COVID-19 pandemic but also to communicate it to the public. The way these leaders communicated the global pandemic revealed the narrative and strategies they chose to create in the social consciousness of their countries. In Israel the COVID-19 crisis broke out after three election cycles, such that the government in charge of the crisis was an interim government under the leadership of Netanyahu, who was operating under three criminal indictments. This study sought to examine the ways in which Prime Minister Netanyahu and two senior Ministry of Health officials—the Director General and the Head of the Public Health Services—communicated information about the COVID-19 health crisis in Israel during what has been termed the first wave and the beginning of the second wave.
Analysis of the findings shows that Netanyahu and the Health Ministry Director General used primarily an apocalyptic narrative to communicate with the public. The main strategy in constructing this narrative was one of intimidation. The leading character in this drama is the coronavirus, an external enemy seeking to wreak destruction upon the nation, while the citizens are the soldiers in the army battling the pandemic.
In research conducted during March 2020, we examined the public’s perceptions and viewpoints during the COVID-19 crisis. The results show that 43% of the respondents believe that the main strategy adopted by those leading the crisis is a strategy of intimidation.31,74 In his press conferences, Netanyahu used analogies to major historical pandemics such as the Spanish flu and the Bubonic Plague. Historical pandemics as depicted in all types of artistic forms throughout history (literature, painting, sculpture and the like) symbolize a sense of vulnerability in the face of uncertainty and death, as well as the arbitrary nature of death itself.75 Similar to the narrative during the Spanish flu pandemic and the Bubonic Plague, the narrative that arose during the current pandemic is marked by characters thought to spread disease, usually members of disempowered communities. Indeed, at times of crisis, blame, stigmatization, fears and anxieties (whether realistic or exaggerated) all swirl through the public consciousness.76
The analogies and images taken from apocalyptic historical narratives were intended to arouse a sense of fear and anxiety in the public so as to motivate people to take action in the form of obeying the guidelines during the COVID-19 crisis. At press conferences and during media interviews, Netanyahu and the Health Ministry Director General cited high morbidity and mortality figures that never were relevant for Israel. The Health Ministry’s use of high predicted morbidity and mortality rates during media campaigns is not unusual, as can be seen from previous epidemiological crises. For example, Dew (1999) described how during the 1997 measles outbreak in New Zealand, the Ministry of Health ran a newspaper and television advertisement campaign that used emotional appeals and statistics to shape a “quantification rhetoric,” which, according to Petersen and Lupton,77 “tends to suggest the figures used are not subject to doubt or uncertainty.”
During this media campaign
the viewer was subjected to images of cemeteries and crucifixes passing across the screen, followed by a pulsating brain. Slowly, an outline of a young boy emerged with the message “don’t join the dots.”
These intimidating predictions were exacerbated by the fact that the 1997 outbreak in New Zealand turned out to be minor. The actual number of measles cases reported was 1,200, and not a single child died.
According to Karanikolos and McKee,78 there is a real risk that political scientists and economists will publish analyses that try to attribute morbidity and mortality to policy and politics without understanding the serious and highly political limitations on data about COVID-19 infections and attributable mortality. Issues such as testing policies change over time, and regional variations in practices can further complicate mortality monitoring.
Authorities use the strategy of intimidation because some policymakers believe that during a crisis the public is in a state of panic and hysteria.79 Another example can be seen in the public response to the appearance of four Ebola cases in the US and to the different strategies implemented by various authorities regarding the precautionary measures that needed to be taken in what was perceived as national panic.80,81 Maryn McKenna82 called this response Ebolanoia.
Even if there is public panic, the use of intimidation without empowering individual self-efficacy contradicts the theory of intimidation use in the literature. The Extended Parallel Process Model (EPPM)83 attempts to predict how individuals will react when confronted with fear-inducing stimuli. In order for fear-based policies to be effective, policymakers must induce a moderate level of fear alongside a higher level of self-efficacy and response efficacy. When the public feels that the level of fear is higher than the level of efficacy, the message is ineffective.
As the research findings show, constructing an emergency narrative also served Netanyahu’s covert political intentions. At the outset of the COVID-19 crisis, Netanyahu was unable to form a government in Israel. To obtain the 61 seats required to form a government, he needed the rival Blue-White party to join the coalition. The crisis brought on by the coronavirus, which Netanyahu continually stressed in his press conferences, managed to lure his political rivals into a government under his leadership.
Pulejo and Querubín18 claim that especially before elections, political interests mingle with professional interests. Elections can directly affect the decision-making process and the measures leaders choose to take during an epidemic crisis. According to Pulejo and Querubín, incumbents running for re-election tend to avoid measures more likely to have a negative economic impact by implementing less stringent restrictions as the date of the election draws closer.
In contrast to such leaders, Netanyahu was in a situation of needing to form a government after elections in Israel. Hence, one of his two target audiences consisted of his political competitors. To get them to join his government, he chose to intensify the health crisis. At his press conferences, economic issues were dwarfed to highlight the state of emergency. According to McKee et al,84 many populist leaders in countries such as the United States, Brazil, Russia, India, and the United Kingdom tended to use COVID-19 to advance their political needs. This was not the first time that Netanyahu introduced foreign considerations during a crisis and used a health crisis to cover up other intentions. One such example can be seen during the disaster brought on by a forest fire in the Carmel Mountains in northern Israel.85 The fire burned for four days, becoming the biggest fire in Israel’s history. Netanyahu employed cover-up risk communication during the crisis. He refrained from discussing the causes that allowed the crisis to materialize in order to evade guilt and personal responsibility. Similarly, in discussing Trump’s conduct during the COVID-19 crisis, Donna Ladkin notes that the media focus on the leader creates bias and diverts attention away from the failures of the healthcare systems and the stakeholders.23
The findings of this study reveal that the the spokespersons made widespread use of the first person “I” and adopted centralist communication of the crisis in Israel. Together with the two senior Ministry of Health officials, Netanyahu managed and communicated the crisis without consulting any other experts who might challenge their conceptualization. This centralist management was the topic of public and media criticism.58,86 The research literature shows that centralist management can lead to what is known as “groupthink,”87 a term that describes how in-group pressures lead to deterioration in decision-making and failure to appraise alternative courses of action as a result of striving for unanimity. Janis87 found that it is precisely group cohesiveness and mutual blind trust that can undermine group decisions. This is because this groupthink leads to the exertion of sufficient peer pressure or fear of being seen as different from the group to encourage members to suppress dissenting opinions and then rationalize adopting the group’s opinions as their own.
Dissent plays an important role in decision-making. It sets the stage for revealing and combining unique pieces of information and insights.88,89 Moreover, dissent promotes careful consideration of a diverse collection of possible courses of action in the context of strategic decision-making.90,91 Groups or organizations that stifle dissent in their decision-making fail to consider alternatives and consequences and as a consequence end up producing fiascos. Leaders or senior management who use centralist management tend to avoid information or opinions different from their own and guide the organization to disregard such opinions in the decision-making process.88,89,92,93
Over the years, empirical studies found that the variables that exert the greatest impact on organizations’ effective decision-making are those that address substantial disputes and conflicts.92,93 Coordination of multiple responses in a public health crisis necessitates a strong and effective organizational leadership model.94 The overall public response to the crisis is dependent on the leader’s ability to mobilize and operate the health system.95 During the COVID-19 crisis, countries whose political leaders were able to coordinate between different key sectors and involve the various branches of government, the public and scientific experts in the decision-making process while at the same time providing social and economic support to their citizens and containing various conflicts were able to deal more effectively with COVID-19.96–98
Crisis management by a leader, particularly if that leader employs the centralist method, requires the leader to serve as a positive role model. The findings of this study indicate that Netanyahu and the other key figures leading the crisis did not strictly comply with the guidelines they imposed on the public, thus serving as negative role models. One of the most influential variables in public cooperation is public trust. Public trust in government institutions and leaders is considered essential in any country that seeks to impose its sovereignty on the people and to maintain order. If citizens do not believe in the government’s authority, the appeal of the state as well as its political, economic and social stability are liable to be harmed.99,100
The findings of the current study indicate that the way in which the guidelines were conveyed to the Israeli public were contrary to the health and risk communication approach, which advocates transparency and data anchored in fact. Transparent communication reduces negative emotions and increases the sense of respect toward the organization or institution managing the risk.101 There was no transparency in communicating information about the specific profiles of people who became infected with and died from COVID-19. Moreover, the protocols of government discussions on COVID-19 will remain classified for the next 30 years and will not be available to the public.102 Contrary to this form of management, other world leaders did provide transparent information to the public during COVID-19. At the outset of the crisis, German Chancellor Angela Merkel diligently presented all data at her disposal, and the prime minister of New Zealand informed the public of the rationale behind the decision-making.103 Indeed, she was praised for using diverse rather than selective information and for presenting it transparently to the public. She holds a degree in communications and used Facebook live chats to reach out to her constituency in an informal yet informative way. Her “we’re all in this together” attitude earned her the trust and support of her people, making it possible to enforce a Level 4 national closure.24
In addition to the lack of information transparency, the Israeli public was also given conflicting instructions on various issues. One example pertains to wearing masks. Another is the need for testing those who have no symptoms but were exposed to a confirmed coronavirus patient. As the findings show, at the beginning of the COVID-19 crisis, the spokespersons stated there was no need to wear masks. They later changed their tune, required the public to wear masks outside and imposed fines on those who did not comply. The literature points to uncertainty regarding the effectiveness of wearing masks. Some say that wearing a mask can lead to false confidence.104–106 The uncertainty at the beginning of the crisis regarding how the coronavirus is transmitted (by droplets or airborne) also contributed to the debate regarding the applicability of masks and the degree to which they protect against contagion.107
The risk communication literature indicates that in situations of uncertainty, policymakers do not always provide full information and instead use scientific knowledge to frame uncertainty in terms of absolute certainty.108,109 Vos and van Asselt108 called this “the uncertainty paradox,” referring to situations in which uncertainty is acknowledged (as with the masks), while the role of science is framed as providing certainty.110 Sandman and Lanard109 emphasize the need to “proclaim uncertainty” and advise authorities to share tentative information if that is all they have.
In addition to failing to communicate uncertainty, during the press conferences and interviews the spokespersons did not provide any rationale for the guidelines. For example, why was IKEA allowed to open while shopping centers remained closed? Or why did people need to remain within 100 meters of their homes? In contrast, on its coronavirus website, the government of Singapore111 posted an attractive and accessible campaign explaining the rationale behind the instructions to the public as well as the scientific basis for wearing masks.112 According to the literature on risk communication, the effectiveness of crisis management depends on a leader’s ability to clearly and accurately formulate a response based on accurate information.3 Risk communication with the general public is critical to ensure an efficient and rational response to a crisis.113 When instructions are not backed up by scientific facts, it is difficult for the public to accept them. Moreover, the public can develop lack of trust when one sector is more successful than another in influencing the decision-makers. The findings of this study indicate that Netanyahu incorporated values directed at the Jewish population in his speeches in order to persuade his audience and build trust, while choosing to disregard other population groups such as the Arabs. This exclusive appeal to the Jewish population may have given the rest of the population the feeling that they are not taken into consideration in decision-making. Furthermore, in press conferences Netanyahu avoided direct references to the increased morbidity in the ultra-Orthodox sector. This cautious approach is in line with the risk communication literature that advocates not referring to at-risk groups in an offensive manner so as not to reinforce stigmas or generate guilt. Sometimes during a health crisis, the authorities are afraid that at-risk populations will reject relevant information out of fear of being stigmatized by the media and society.114 Furthermore, this lack of attention to different groups and varying risk levels can lead to the perception that politics are what determine attitudes and policies. This is exemplified by the decision to place the country under a complete closure rather than to employ differential measures based upon morbidity figures.
The limitations of this research are related to the ongoing nature of the COVID-19 crisis. The research findings refer only to the time period in which the research was conducted. Nevertheless, the findings reveal the way in which the leaders chose to communicate the crisis as well as the influence of politics on health. Future research should examine how the ways in which information is conveyed to the public affect issues of public trust and public response to present and future guidelines.
Conclusion
Communicating crises to the public, particularly ongoing crises like COVID-19, requires that leaders implement the health and risk communication approach and create a cooperative narrative that does not rely on a strategy of intimidation, but rather on empathy. Such a narrative should provide fact-based and transparent information regarding uncertainty. Leaders who have managed to win public trust during the COVID-19 crisis are those that advocated strategies of participatory public communication and science-based guidelines.
Abbreviations
COVID-19, coronavirus disease 2019; OECD, Organization for Economic Cooperation and Development; PHEIC, Public Health Emergency of International Concern; WHO, World Health Organization.
Ethics Approval
Because the study was based on public knowledge and not on human subjects, it was exempt from human subjects’ ethics approval by the Ethics Committee of The Faculty of Social Welfare and Health Sciences at the University of Haifa.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.WHO Director-General. Statement on the Second Meeting of the International Health Regulations (2005) Emergency Committee Regarding the Outbreak of Novel Coronavirus (2019-Ncov). Geneva, Switzerland: WHO; 2020. [Google Scholar]
- 2.Betsch C, Wieler LH, Habersaat K; group C. Monitoring behavioural insights related to COVID-19. Lancet. 2020;395(10232):1255–1256. doi: 10.1016/S0140-6736(20)30729-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bennett P, Calman K, Curtis S, Fischbacher-Smith D. Risk Communication and Public Health. Second ed. Oxford: Oxford University Press; 2010. [Google Scholar]
- 4.Gesser-Edelsburg A, Shir-Raz Y. Risk Communication and Infectious Diseases in an Age of Digital Media. London and New York: Routledge; 2016. [Google Scholar]
- 5.Sellnow DD, Sellnow TL. The IDEA model for effective instructional risk and crisis communication by emergency managers and other key spokespersons. J Emerg Manag. 2019;17(1):67–78. doi: 10.5055/jem.2019.0399 [DOI] [PubMed] [Google Scholar]
- 6.Slovic P. Trust, emotion, sex, politics, and science: surveying the risk‐assessment battlefield. Risk Anal. 1999;19(4):689–701. doi: 10.1111/j.1539-6924.1999.tb00439.x [DOI] [PubMed] [Google Scholar]
- 7.Thomas CW. Maintaining and restoring public trust in government agencies and their employees. Adm Soc. 1998;30(2):166–193. doi: 10.1177/0095399798302003 [DOI] [Google Scholar]
- 8.Chess C, Salomone KL, Hance BJ, Saville A. Results of a national symposium on risk communication: next steps for government agencies. Risk Anal. 1995;15(2):115–125. doi: 10.1111/j.1539-6924.1995.tb00306.x [DOI] [Google Scholar]
- 9.Covello VT, McCallum DB, Pavlova M. Principles and guidelines for improving risk communication In: Covello VT, McCallum DB, Pavlova MT, editors. Effective Risk Communication. Contemporary Issues in Risk Analysis. Vol. 4 Boston, MA: Springer; 1989. [Google Scholar]
- 10.Deitchman S. Enhancing crisis leadership in public health emergencies. Disaster Med Public Health Prep. 2013;7(5):534–540. doi: 10.1017/dmp.2013.81 [DOI] [PubMed] [Google Scholar]
- 11.Binagwaho A. We need compassionate leadership management based on evidence to defeat COVID-19. Int J Health Policy Manag. 2020;9(10):413–414. doi: 10.34172/ijhpm.2020.73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gesser-Edelsburg A, Mordini E, James JJ, Greco D, Green MS. Risk communication recommendations and implementation during emerging infectious diseases: a case study of the 2009 H1N1 influenza pandemic. Disaster Med Public Health Prep. 2014;8(2):158–169. doi: 10.1017/dmp.2014.27 [DOI] [PubMed] [Google Scholar]
- 13.Gesser-Edelsburg A, Stolero N, Mordini E, Billingsley M, James JJ, Green MS. Emerging infectious disease (EID) communication during the 2009 H1N1 influenza outbreak: literature review (2009–2013) of the methodology used for EID communication analysis. Disaster Med Public Health Prep. 2015;9(2):199–206. doi: 10.1017/dmp.2014.126 [DOI] [PubMed] [Google Scholar]
- 14.Garrett L. COVID-19: the medium is the message. Lancet. 2020;395(10228):942–943. doi: 10.1016/S0140-6736(20)30600-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parker K, Menasce Horowitz J, Browm A About half of lower-income Americans report household job or wage loss due to COVID-19. Pew Research Center; 2020. Available from: https://www.pewsocialtrends.org/2020/04/21/about-half-of-lower-income-americans-report-household-job-or-wage-loss-due-to-covid-19/. Accessed November20, 2020. [Google Scholar]
- 16.Galasso V. Covid: not a great equaliser. Covid Econ. 2020;(19):241–255. [Google Scholar]
- 17.Greer SL, King EJ, da Fonseca EM, Peralta-Santos A. The comparative politics of COVID-19: the need to understand government responses. Glob Public Health. 2020;15(9):1413–1416. doi: 10.1080/17441692.2020.1783340 [DOI] [PubMed] [Google Scholar]
- 18.Pulejo M, Querubín P Electoral concerns reduce restrictive measures during the COVID-19 pandemic. National Bureau of Economic Research Working Paper Series; 2020. Available from: http://www.nber.org/papers/w27498. Accessed December5, 2020. [DOI] [PMC free article] [PubMed]
- 19.Vuong Q-H, Ho T-M, Nguyen H-K, Vuong -T-T. Healthcare consumers’ sensitivity to costs: a reflection on behavioural economics from an emerging market. Palgrave Commun. 2018;4(1):70. doi: 10.1057/s41599-018-0127-3 [DOI] [Google Scholar]
- 20.Rufai SR, Bunce C. World leaders’ usage of Twitter in response to the COVID-19 pandemic: a content analysis. J Public Health (Oxf). 2020;42(3):510–516. doi: 10.1093/pubmed/fdaa049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kingsley P. Some European Nations Ease Pandemic Rules, but Move Warily. The New York Times; 2020. [Google Scholar]
- 22.Specia M. Sugarcoating and Brutal Honesty: How Leaders are Handling Coronavirus Crisis. The New York Times; 2020. [Google Scholar]
- 23.Ladkin D. What Donald Trump’s response to COVID-19 teaches us: it’s time for our romance with leaders to end. Leadership. 2020;16(3):273–278. doi: 10.1177/1742715020929134 [DOI] [Google Scholar]
- 24.Watson VB Five coronavirus success stories: different, but the same. Security Nexus: Daniel K Inouye Asia-Pacific Center for Security Studies; 2020. Available from: https://apcss.org/wp-content/uploads/2020/06/SecurityNexus_Watson_FIVE_CORONAVIRUS_SUCCESS_STORIES-C.pdf. Accessed September2, 2020.
- 25.Wilson S. Pandemic leadership: lessons from New Zealand’s approach to COVID-19. Leadership. 2020;16(3):279–293. doi: 10.1177/1742715020929151 [DOI] [Google Scholar]
- 26.Cambell A. Jacinda Ardern’s coronavirus plan is working because, unlike others, she’s behaving like a true leader. Independent. 2020. [Google Scholar]
- 27.Aldrich AS, Lotito NJ. Pandemic performance: women leaders in the Covid-19 crisis. Politics Gend. 2020;1–9. doi: 10.1017/S1743923X20000549 [DOI] [Google Scholar]
- 28.Oriola TB, Knight WA. COVID-19, George Floyd and human security. Afri Security. 2020;13(2):111–115. doi: 10.1080/19392206.2020.1783760 [DOI] [Google Scholar]
- 29.Erlanger S. Poland and Hungary Use Coronavirus to Punish Opposition. The New York Times; 2020. [Google Scholar]
- 30.Kolhatkar S. Can Democracy Survive the Coronavirus? NewsClick; 2020. [Google Scholar]
- 31.Gesser-Edelsburg A, Cohen R, Hijazi R, Abed Elhadi SN. Analysis of public perception of the Israeli government’s early emergency instructions regarding COVID-19: online survey study. J Med Internet Res. 2020;22(5):e19370. doi: 10.2196/19370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dekel U. The System-Wide Campaign to Battle the Corona Crisis in Israel. The Institute for National Security Studies; 2020. [Google Scholar]
- 33.Denzin NK. Triangulation 2.0. J Mix Methods Res. 2012;6(2):80–88. [Google Scholar]
- 34.Wagner KD, Davidson PJ, Pollini RA, Strathdee SA, Washburn R, Palinkas LA. Reconciling incongruous qualitative and quantitative findings in mixed methods research: exemplars from research with drug using populations. Int J Drug Policy. 2012;23(1):54–61. doi: 10.1016/j.drugpo.2011.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carter N, Bryant-Lukosius D, DiCenso A, Blythe J, Neville AJ. The use of triangulation in qualitative research. Oncol Nurs Forum. 2014;41(5):545–547. doi: 10.1188/14.Onf.545-547 [DOI] [PubMed] [Google Scholar]
- 36.Yeh CJ, Inman AG. Qualitative data analysis and interpretation in counseling psychology: strategies for best practices. Couns Psychol. 2007;35(3):369–403. doi: 10.1177/0011000006292596 [DOI] [Google Scholar]
- 37.Curtin M, Fossey E. Appraising the trustworthiness of qualitative studies: guidelines for occupational therapists. Aust Occup Ther J. 2007;54(2):88–94. doi: 10.1111/j.1440-1630.2007.00661.x [DOI] [Google Scholar]
- 38.Boutain DM. Critical language and discourse study: their transformative relevance for critical nursing inquiry. ANS Adv Nurs Sci. 1999;21(3):1–8. doi: 10.1097/00012272-199903000-00004 [DOI] [PubMed] [Google Scholar]
- 39.Parker I. Discourse Dynamics: Critical Analysis for Social and Individual Psychology. Florence, KY, US: Taylor & Frances/Routledge; 1992. [Google Scholar]
- 40.Thorne S. Data analysis in qualitative research. Evid Based Nurs. 2000;3(3):68–70. doi: 10.1136/ebn.3.3.68 [DOI] [Google Scholar]
- 41.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- 42.Vaismoradi M, Jones J, Turunen H, Snelgrove S. Theme development in qualitative content analysis and thematic analysis. J Nurs Educ Pract. 2016;6(5):100–110. doi: 10.5430/jnep.v6n5p100 [DOI] [Google Scholar]
- 43.Morse JM. Sampling in grounded theory In: Bryant A, Charmaz K, editors. The SAGE Handbook of Grounded Theory. Thousand Oaks, CA: Sage; 2007:229–244. [Google Scholar]
- 44.Nevo. Corona regulations; 2020. Available from: https://www.nevo.co.il/general/CoronaUpdates.aspx. Accessed September7, 2020.
- 45.Huberman AM, Miles MB. Data management and analysis methods In: Denzin NK, Lincoln YS, editors. Handbook of Qualitative Research. Thousand Oaks, CA, US: Sage Publications, Inc; 1994:428–444. [Google Scholar]
- 46.Lombard M, Snyder-Duch J, Bracken CC. Content analysis in mass communication: assessment and reporting of intercoder reliability. Hum Commun Res. 2002;28(4):587–604. doi: 10.1111/j.1468-2958.2002.tb00826.x [DOI] [Google Scholar]
- 47.Israel Ministry of Justice. Memorandum of the General Security Service Accreditation Law to Assist in the National Effort to Reduce the Spread of the New Corona Virus (Temporary Order). 2020. May19, 2020.
- 48.Kaliner E, Moran-Gilad J, Grotto I, et al. Silent reintroduction of wild-type poliovirus to Israel, 2013 – risk communication challenges in an argumentative atmosphere. Eurosurveillance. 2014;19(7):20703. [DOI] [PubMed] [Google Scholar]
- 49.Williams DE, Olaniran BA. Expanding the crisis planning function: introducing elements of risk communication to crisis communication practice. Public Relat Rev. 1998;24(3):387–400. doi: 10.1016/S0363-8111(99)80147-7 [DOI] [Google Scholar]
- 50.Visschers VHM, Wiedemann PM, Gutscher H, et al. Affect-inducing risk communication: current knowledge and future directions. J Risk Res. 2012;15(3):257–271. doi: 10.1080/13669877.2011.634521 [DOI] [Google Scholar]
- 51.Dochinoiu E. Stylistic aspects in the English military language. Revista Academiei Fortelor Terestre. 2009;14(2):71–78. [Google Scholar]
- 52.Ben-Israel I, Lancet D. Corona data analysis: “Leap? The ‘new’ patients are not contagious”. YNET. 2020. [Google Scholar]
- 53.Friedmann D. There is no one to fight in the atmosphere of hysteria. YNET. 2020. [Google Scholar]
- 54.Lancet D. A second outbreak? 8 important questions for the Ministry of Health. YNET. 2020. [Google Scholar]
- 55.Rosenwald MS History’s deadliest pandemics, from ancient Rome to modern America. The Washington Post; 2020.
- 56.WHO. WHO Coronavirus disease (COVID-19) dashboard; 2020. Available from: https://covid19.who.int/?gclid=Cj0KCQiAkuP9BRCkARIsAKGLE8USyaKh-Mnusm3_p83n_I-_ixF5DqGD-qKOSIroA4vFjerudhOHChIaAilDEALw_wcB. Accessed November21, 2020.
- 57.Arlosoroff M. This is not how we fight the pandemic: the failure of corona tests will cost us NIS 90 billion. TheMarker. 2020. [Google Scholar]
- 58.Efrati I. Factors involved in managing the corona crisis: sadetsky torpedoed critical initiatives and hid information. Haaretz. 2020. [Google Scholar]
- 59.Israel Ministry of Health. Emergency regulations restricting activity have been approved in order to reduce the spread of the coronavirus in Israel [press release]. March25, 2020 Available from: https://www.gov.il/he/departments/news/25032020_01. Accessed September 3, 2020.
- 60.Israel Ministry of Foreign Affairs. Joint Prime Minister’s Office, Health Ministry and Finance Ministry Press Release [press release]. 2020. Available from: https://mfa.gov.il/MFA/InnovativeIsrael/Economy/Pages/Joint-Prime-Minister-s-Office-Health-Ministry-and-Finance-Ministry-Press-Release-19-April-2020.aspx. Accessed November 21, 2020.
- 61.Peleg B. Business owners in Tel Aviv claim that the purple label regulations are not understood. This week they received 646 reports. Haaretz. 2020. [Google Scholar]
- 62.Dovrat-Meseritz A. Every store owner should hire a legal advisor today who will tell him what is allowed and what is not. TheMarker. 2020. [Google Scholar]
- 63.Eichner I, Freidson Y. The opening of IKEA has caused a stir in the government and the market: “Disgrace and discrimination”. YNET. 2020. [Google Scholar]
- 64.Kadosh N. What is behind the decision that allowed the opening of the IKEA chain? Calcalist. 2020. [Google Scholar]
- 65.Levi L, Dovrat-Meseritz A. The extent of IKEA owners’ contributions to Gur hasidic storks has been revealed; and what does that have to do with Ayelet Shaked? TheMarker. 2020. [Google Scholar]
- 66.Somfalvi A. “It does not make sense to open IKEA and leave the malls behind”. YNET. 2020. [Google Scholar]
- 67.Efrati I. Essential information about the corona is not available to the public, ministers and even Ministry of Health officials. Haaertz. 2020. [Google Scholar]
- 68.Dvash R, Zomer G. Survey: Transparency in the Corona Crisis - Summary of Public Attitudes. The Movment for Freedom of Information; 2020. [Google Scholar]
- 69.Schneider T. Request from the Corona Committee: hold a discussion on information transparency. Globes. 2020. [Google Scholar]
- 70.Rabinowitz A. Health Minister Litzman was diagnosed with corona. Haaretz. 2020. [Google Scholar]
- 71.Haeertz Health. Worshipers in Jerusalem: Litzman prayed indoors in violation of emergency regulations. Haaretz. 2020. [Google Scholar]
- 72.Nachshoni K, Mandelbaum E. On Litzman Street, contrary to instructions: praying in a synagogue. YNET. 2020. [Google Scholar]
- 73.Linder R. “Do not bring the son home”: Netanyahu, Rivlin and Litzman present - this is not how the Corona is defeated. TheMarker. 2020. [Google Scholar]
- 74.Rabad A. Research: the public majority trust Bar Siman Tov, less on Litzman. YNET. 2020. [Google Scholar]
- 75.Cunningham A. Epidemics, pandemics, and the doomsday scenario. Hist Speaking. 2008;9(7):29–31. doi: 10.1353/hsp.2008.0035 [DOI] [Google Scholar]
- 76.Wald P. Contagious: Cultures, Carriers, and the Outbreak Narrative. Durham: Duke University Press; 2008. [Google Scholar]
- 77.Petersen A, Lupton D. The New Public Health: Health and Self in the Age of Risk. St Leonards: Allen & Unwin; 1996. [Google Scholar]
- 78.Karanikolos M, McKee M How comparable is Covid-19 mortality across countries? COVID-19 cross-country analysis; 2020. Available from: https://analysis.covid19healthsystem.org/index.php/2020/06/04/how-comparable-is-covid-19-mortality-across-countries/. Accessed November20, 2020.
- 79.Sandman P Ebola in the U.S. (so far): the public health establishment and the quarantine debate. The Peter M. Sandman Risk Communication Website; 2014. Available from: http://www.psandman.com/col/Ebola-4.htm. Accessed May14, 2016.
- 80.Gonsalves G, Staley P. Panic, paranoia, and public health - The AIDS epidemic’s lessons for ebola. N Engl J Med. 2014;371(25):2348–2349. [DOI] [PubMed] [Google Scholar]
- 81.Viebeck E Health officials struggle to control the media narrative about Ebola. The Hill; 2014. Available from: http://thehill.com/policy/healthcare/220458-feds-struggle-to-control-the-media-narrative-about-ebola. Accessed September4, 2020. [Google Scholar]
- 82.Mckenna M. Ebolanoia: the only thing we have to fear is Ebola fear itself. Wired; 2014. Available from: http://www.wired.com/2014/10/ebolanoia/. Accessed September4, 2020. [Google Scholar]
- 83.Witte K. Fear control and danger control: a test of the extended parallel process model (EPPM). Commun Monogr. 1994;61(2):113–134. doi: 10.1080/03637759409376328 [DOI] [Google Scholar]
- 84.McKee M, Gugushvili A, Koltai J, Stuckler D. Are populist leaders creating the conditions for the spread of COVID-19?; Comment on “A scoping review of populist radical right parties’ influence on welfare policy and its implications for population health in Europe. Int J Health Policy Manag. 2020. doi: 10.34172/ijhpm.2020.124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gesser-Edelsburg A, Zemach M. From a fiasco to the Supertanker grand finale: Israeli Prime Minister Netanyahu’s crisis communication during the Carmel disaster. J Risk Res. 2012;15(8):967–989. doi: 10.1080/13669877.2012.686052 [DOI] [Google Scholar]
- 86.Arlosoroff M. Netanyahu’s megalomania will kill us all. TheMarker. 2020. [Google Scholar]
- 87.Janis IL. Groupthink: Psychological Studies of Policy Decisions and Fiascos. Boston: Houghton Mifflin; 1982. [Google Scholar]
- 88.Hoever IJ, van Knippenberg D, van Ginkel WP, Barkema HG. Fostering team creativity: perspective taking as key to unlocking diversity’s potential. J Appl Psychol. 2012;97(5):982–996. doi: 10.1037/a0029159 [DOI] [PubMed] [Google Scholar]
- 89.van Knippenberg D, De Dreu CKW, Homan AC. Work group diversity and group performance: an integrative model and research agenda. J Appl Psychol. 2004;89(6):1008–1022. doi: 10.1037/0021-9010.89.6.1008 [DOI] [PubMed] [Google Scholar]
- 90.Bantel KA, Jackson SE. Top management and innovations in banking: does the composition of the top team make a difference? Strat Manag J. 1989;10(S1):107–124. doi: 10.1002/smj.4250100709 [DOI] [Google Scholar]
- 91.Glick WH, Miller CC, Huber GP. The impact of diversity on organizational performance In: Glick WH, editor. Organizational Change and Redesign: Ideas and Insights for Improving Performance. New York, NY: Oxford University Press; 1993:176–214. [Google Scholar]
- 92.De Dreu CKW, West MA. Minority dissent and team innovation: the importance of participation in decision making. J Appl Psychol. 2001;86(6):1191–1201. doi: 10.1037/0021-9010.86.6.1191 [DOI] [PubMed] [Google Scholar]
- 93.Garner JT, Ragland JP. Tabling, discussing, and giving in: dissent in workgroups. Group Dyn Theory Res Pract. 2019;23(1):57–74. doi: 10.1037/gdn0000098 [DOI] [Google Scholar]
- 94.Boin A, Lagadec P. Preparing for the future: critical challenges in crisis management. J Contingencies Crisis Manag. 2000;8(4):185–191. doi: 10.1111/1468-5973.00138 [DOI] [Google Scholar]
- 95.Lawton L. Public health and crisis leadership in the 21st century. Perspect Public Health. 2013;133(3):144–145. doi: 10.1177/1757913913488469 [DOI] [PubMed] [Google Scholar]
- 96.Purkayastha S, Salvatore M, Mukherjee B. Are women leaders significantly better at controlling the contagion during the COVID-19 pandemic? J Health Soc Sci. 2020;5(2):231–240. [PMC free article] [PubMed] [Google Scholar]
- 97.Wilson S Three reasons why Jacinda Ardern’s coronavirus response has been a masterclass in crisis leadership. The Conversation; 2020. Available from: https://theconversation.com/three-reasons-why-jacinda-arderns-coronavirus-response-has-been-a-masterclass-in-crisis-leadership-135541. Accessed November20, 2020.
- 98.You J. Lessons from South Korea’s Covid-19 policy response. Am Rev Public Admin. 2020;50(6–7):801–808. doi: 10.1177/0275074020943708 [DOI] [Google Scholar]
- 99.Bensman J. The aesthetics and politics of footnoting. Int J Polit Cult Soc. 1988;1(3):443–470. doi: 10.1007/BF01385430 [DOI] [Google Scholar]
- 100.Meyer S, Ward P, Coveney J, Rogers W. Trust in the health system: an analysis and extension of the social theories of Giddens and Luhmann. Health Sociol Rev. 2008;17(2):177–186. doi: 10.5172/hesr.451.17.2.177 [DOI] [Google Scholar]
- 101.Lofstedt RE. How can we make food risk communication better: where are we and where are we going? J Risk Res. 2006;9(8):869–890. doi: 10.1080/13669870601065585 [DOI] [Google Scholar]
- 102.Ashcknasy B. Petition against the Ministry of Health: the management of information regarding the Corona virus is “amateur”. TheMarker. 2020. [Google Scholar]
- 103.Fillion S. The Science Behind Women Leaders’ Success in Fighting Covid-19. Forbes; 2020. [Google Scholar]
- 104.Ashkenazi S. Scientists Against Government Guidelines: There is No Medical Reason for the Aggravation of the Subject of Masks. Globes; 2020. [Google Scholar]
- 105.Filut A. Board of the Association of Public Health Physicians: the charge to wear a mask may harm the eradication of the corona. Calcalist. 2020. [Google Scholar]
- 106.MacIntyre CR, Chughtai AA. Facemasks for the prevention of infection in healthcare and community settings. BMJ. 2015;350:h694. doi: 10.1136/bmj.h694 [DOI] [PubMed] [Google Scholar]
- 107.WHO. Modes of Transmission of Virus Causing COVID-19: Implications for IPC Precaution Recommendations. Scientific Brief. Geneva: World Health Organization; 2020. [Google Scholar]
- 108.van Asselt MBA, Vos E. Wrestling with uncertain risks: EU regulation of GMOs and the uncertainty paradox. J Risk Res. 2008;11(1):281–300. doi: 10.1080/13669870801990806 [DOI] [Google Scholar]
- 109.van Asselt MBA, Vos E, Rooijackers B. Science, knowledge and uncertainty in EU risk regulation In: Everson M, Vos E, editors. Uncertain Risks Regulated. Oxon, OX: Routledge-Cavendish; 2009:359–388. [Google Scholar]
- 110.Fox T The role of uncertainty intolerance in european risk governance. Paper presented at: Risk Research Symposium; King’s College London; 2009. [Google Scholar]
- 111.Government of Singapore. COVID-19 (Coronavirus Disease 2019). gov.sg; 2020. Available from: https://www.gov.sg/features/covid-19. Accessed September4, 2020.
- 112.Government of Singapore. The science behind why masks help prevent COVID-19 spread. gov.sg; 2020. Available from: https://www.gov.sg/article/the-science-behind-why-masks-help-prevent-covid-19-spread. Accessed September4, 2020.
- 113.Thurston GD, Chi Chen L. Risk communication in the aftermath of the World Trade Center disaster. Am J Ind Med. 2002;42(6):543–544. doi: 10.1002/ajim.10163 [DOI] [PubMed] [Google Scholar]
- 114.Guttman N, Salmon CT. Guilt, fear, stigma and knowledge gaps: ethical issues in public health communication interventions. Bioethics. 2004;18(6):531–552. doi: 10.1111/j.1467-8519.2004.00415.x [DOI] [PubMed] [Google Scholar]