Abstract
BACKGROUND
Acute stress might increase short-term heart rate variability and blood pressure variability (BPV); however, chronic stress would not alter short-term BPV in animal models.
AIM
To examine the association of psychological stress with long-term BPV in young male humans.
METHODS
We prospectively examined the association of chronic psychological stress with long-term BPV in 1112 healthy military males, averaged 32.2 years from the cardiorespiratory fitness and hospitalization events in armed forces study in Taiwan. Psychological stress was quantitatively evaluated with the Brief Symptom Rating Scale (BSRS-5), from the least symptom of 0 to the most severe of 20, and the five components of anxiety, insomnia, depression, interpersonal sensitivity, and hostility (the severity score in each component from 0 to 4). Long-term BPV was assessed by standard deviation (SD) for systolic and diastolic blood pressure (SBP and DBP), and average real variability (ARV), defined as the average absolute difference between successive measurements of SBP or DBP, across four visits in the study period from 2012 to 2018 (2012-14, 2014-15, 2015-16, and 2016-18).
RESULTS
The results of multivariable linear regressions showed that there were no correlations of the BSRS-5 score with SDSBP, SDDBP, ARVSBP, and ARVDBP after adjusting for all the covariates [β(SE): -0.022 (0.024), -0.023 (0.026), -0.001 (0.018), and 0.001 (0.020), respectively; P > 0.05 for all]. In addition, there were also no correlations between each component of the BSRS score and the long-term BPV indexes.
CONCLUSION
Our findings suggest that chronic psychological stress might not be associated with long-term BPV in military young male humans.
Keywords: Long-term blood pressure variability, Military, Psychological stress, Young males, Brief Symptom Rating Scale, Average real variability
Core Tip: This study investigated the relationship of psychological stress evaluated using the Brief Symptom Rating Scale (BSRS-5) with long-term blood pressure variability (BPV) in 1112 military young male adults across four visits during a 7-year period. We found that there were no correlations of the BSRS-5 score and related components with systolic and diastolic BPV indexes in the fully adjusted model. Although previous studies have demonstrated that there was an association between psychological stress and elevated blood pressure, our study suggested no association of psychological stress and long-term BPV in young male adults.
INTRODUCTION
Psychological stress is related to activation of the sympathetic nervous system and production of norepinephrine and epinephrine from the adrenal glands, leading to elevated blood pressure. Previous studies have shown that psychological stress, particularly chronic stress, may cause the development of hypertension[1]. To our knowledge, psychological stress is subjective and complicated in human beings. An experiment in mice demonstrated that acute stress might result in increased short-term heart rate variability and blood pressure variability (BPV); however, chronic stress would not alter short-term BPV[2]. Whether chronic mental stress is associated with long-term BPV remains unclear in human beings. Therefore, we investigated such association in a military cohort of young male adults.
MATERIALS AND METHODS
Study population
We prospectively examined the association of chronic psychological stress with long-term BPV in 1112 healthy military males aged 18-40 years (32 years on average) from the cardiorespiratory fitness and hospitalization events in armed forces study in Taiwan[3-10]. All participants visited the Hualien Armed Forces General Hospital for a comprehensive health examination including the survey of demographics, anthropometrics, hemodynamics, mental stress, and behaviors and laboratory studies at least at two-year intervals from 2012 to 2018 (2012-14, 2014-15, 2015-16, and 2016-18).
Psychological stress measurements
The chronic psychological stress severity of military males in Taiwan was assessed using the Brief Symptom Rating Scale (BSRS-5) in the past 3 mo. There were five psychological domains included in BSRS-5, i.e., depression (feeling blue), anxiety (feeling tense), interpersonal sensitivity (feeling inferior to others), hostility (feeling easily annoyed or irritated), and insomnia (trouble falling asleep). The scoring scale of each domain is Likert-type, ranging from 0 to 4 in severity: 0, nothing; 1, a little; 2, moderately; 3, quite a bit; 4, extremely[11,12]. The BSRS-5 scores ≤ 5, 6-9, and ≥10 were defined as normal, slight, and great stress, respectively[11]. The test-retest reliability coefficient of the BSRS-5 score was 0.82, and the internal consistency (Cronbach alpha) coefficients ranged from 0.77 to 0.90[12,13].
BPV measurements
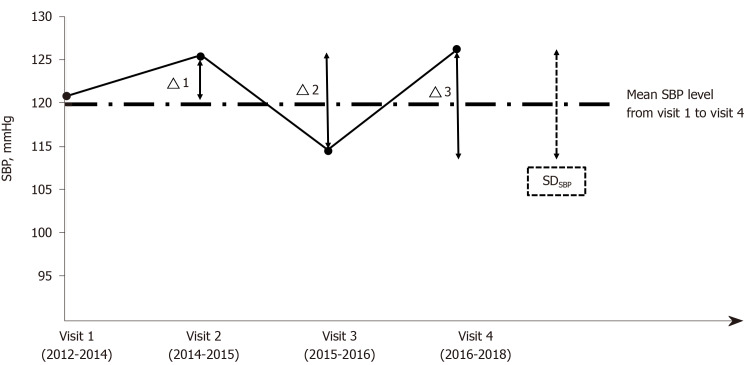
Caffeine or theophylline-containing materials were banned for all participants in a 12-h fast before each hospital visit. Systolic and diastolic blood pressure (SBP and DBP, respectively) was measured with an automated blood pressure monitor (FT-201; Parama-Tech Co. Ltd., Fukuoka, Japan), once over right upper arm of each participant in a sitting position after a rest for 15 min or more at each visit. Long-term BPV was assessed across four visits in the study period by standard deviation (SD) and average real variability (ARV) for SBP and DBP variability. For instance, SD and ARV for SBP variability denoted as SDSBP and ARVSBP are respectively presented by dotted and solid lines in Figure 1. ARV was defined as the average absolute difference between successive measurements of blood pressure, and it takes the order of measurements into account [(|Δ1| + |Δ2| + |Δ3|)/3][14].
Figure 1.
Standard deviation and average real variability for systolic blood pressure variability denoted as SDSBP and ARVSBP respectively presented by dotted and solid lines. Average real variability was defined as the average absolute difference between successive measurements of blood pressure, and it takes the order of measurements into account [(|Δ1| + |Δ2| + |Δ3|)/3]. SBP: Systolic blood pressure; SDSBP: Standard deviation for systolic blood pressure variability.
Statistical analysis
The characteristics of those who had a BSRS-5 score ≤ 5 and BSRS-5 score > 5 are expressed as the mean ± SD for continuous data, and categorical data are expressed as numbers and percentages. In model 1, a multivariable linear regression model adjusted for age, body mass index, baseline SBP and DBP, alcohol intake status, and physical activity (exercise frequency) was used to determine the relationship. The statistic power calculated was 0.85. A value of P < 0.05 was considered significant. SAS statistical software (SAS version 9.4; SAS Institute, Cary, NC, United States) was used for all statistical analyses.
RESULTS
Table 1 shows the baseline profiles of the study participants. The age, body stature, hemodynamic status, and serum lipid profiles were similar between the normal subjects and those with stress. Those who had chronic mental stress were found with a lower level of physical activity and higher prevalence of alcohol drinking. Table 2 shows the results of multivariable linear regressions. In the unadjusted model, there were no correlations between the BSRS score and each component with SD and ARV for SBP and DBP variability, except that interpersonal sensitivity was borderline significantly and negatively correlated with SDSBP [β(SE): -0.010 (0.005), P = 0.07]. After adjusting for the covariates in model 1, the associations of the BSRS score and each component with the long-term BPV indexes did not change a lot and remained insignificant. The correlation between interpersonal sensitivity and SDSBP was just mildly reduced [β(SE): -0.009 (0.005), P = 0.09].
Table 1.
Baseline characteristics of the study cohort (n = 1112)
|
Characteristic
|
BSRS ≤ 5 (n = 983)
|
BSRS > 5 (n = 129)
|
P
value
|
| Age (yr) | 32.21 ± 3.87 | 32.22 ± 4.02 | 0.99 |
| Body mass index (kg/m2) | 25.14 ± 2.93 | 25.18 ± 2.71 | 0.89 |
| SBP (mmHg) | 118.45 ± 13.45 | 117.60 ± 12.98 | 0.49 |
| DBP (mmHg) | 71.58 ± 10.12 | 71.83 ± 9.95 | 0.78 |
| Heart rate (beats per min) | 74.96 ± 10.48 | 75.51 ± 11.54 | 0.58 |
| Fasting plasma glucose (mg/dL) | 94.42 ± 13.17 | 95.09 ± 15.33 | 0.59 |
| Total cholesterol (mg/dL) | 180.27 ± 36.62 | 179.30 ± 34.01 | 0.75 |
| High-density lipoprotein (mg/dL) | 47.97 ± 9.78 | 48.30 ± 11.15 | 0.72 |
| Physical activity | |||
| Never or occasionally | 147 (15.0) | 38 (29.5) | < 0.01 |
| 1-2 times/wk | 365 (37.1) | 62 (48.1) | |
| ≥ 3-5 times/wk | 471 (47.9) | 29 (22.5) | |
| Current drinkers (%) | 441 (44.9) | 76 (58.9) | < 0.01 |
| Current smokers (%) | 376 (38.3) | 55 (42.5) | 0.33 |
Continuous variables are expressed as the mean ± SD, and categorical variables as n (%). BSRS: Brief Symptom Rating Scale; SBP: Systolic blood pressure; DBP: Diastolic blood pressure.
Table 2.
Association of the Brief Symptom Rating Scale score and the components with the long-term blood pressure variability indexes in multivariable liner regressions
|
Unadjusted
|
Model 1
|
|||||
|
|
β(SE)
|
P
value
|
R
2
, %
|
β(SE)
|
P
value
|
R
2
, %
|
| BSRS scores | ||||||
| ARVSBP | -0.005 (0.019) | 0.80 | 0.0 | -0.001 (0.018) | 0.94 | 7.2 |
| ARVDBP | -0.003 (0.020) | 0.88 | 0.0 | 0.001 (0.020) | 0.96 | 7.2 |
| SDSBP | -0.028 (0.025) | 0.26 | 0.1 | -0.022 (0.024) | 0.36 | 7.2 |
| SDDBP | -0.032 (0.027) | 0.23 | 0.1 | -0.023 (0.026) | 0.38 | 7.2 |
| Anxiety | ||||||
| ARVSBP | -0.005 (0.005) | 0.31 | 0.1 | -0.003 (0.005) | 0.51 | 6.2 |
| ARVDBP | -0.003 (0.005) | 0.53 | 0.0 | -0.001 (0.005) | 0.83 | 6.1 |
| SDSBP | -0.009 (0.006) | 0.17 | 0.2 | -0.006 (0.006) | 0.32 | 6.2 |
| SDDBP | -0.007 (0.007) | 0.29 | 0.1 | -0.003 (0.007) | 0.66 | 6.1 |
| Depression | ||||||
| ARVSBP | -0.002 (0.004) | 0.62 | 0.0 | -0.001 (0.004) | 0.71 | 5.6 |
| ARVDBP | 0.000 (0.004) | 0.93 | 0.0 | 0.000 (0.004) | 0.93 | 5.6 |
| SDSBP | -0.007 (0.005) | 0.16 | 0.2 | -0.006 (0.005) | 0.21 | 5.7 |
| SDDBP | -0.005 (0.006) | 0.40 | 0.1 | -0.003 (0.006) | 0.58 | 5.6 |
| Hostility | ||||||
| ARVSBP | 0.002 (0.004) | 0.66 | 0.0 | 0.003 (0.004) | 0.55 | 6.1 |
| ARVDBP | 0.001 (0.005) | 0.88 | 0.0 | 0.001 (0.005) | 0.83 | 6.0 |
| SDSBP | -0.003 (0.006) | 0.54 | 0.0 | -0.002 (0.006) | 0.67 | 6.1 |
| SDDBP | -0.006 (0.006) | 0.31 | 0.1 | -0.005 (0.006) | 0.40 | 6.1 |
| Interpersonal sensitivity | ||||||
| ARVSBP | -0.002 (0.004) | 0.55 | 0.0 | -0.002 (0.004) | 0.60 | 6.1 |
| ARVDBP | -0.001 (0.004) | 0.76 | 0.0 | 0.000 (0.004) | 0.90 | 6.1 |
| SDSBP | -0.010 (0.005) | 0.07 | 0.3 | -0.009 (0.005) | 0.09 | 6.3 |
| SDDBP | -0.008 (0.006) | 0.18 | 0.2 | -0.006 (0.006) | 0.29 | 6.2 |
| Insomnia | ||||||
| ARVSBP | 0.003 (0.004) | 0.49 | 0.0 | 0.003 (0.004) | 0.41 | 3.9 |
| ARVDBP | 0.001 (0.004) | 0.80 | 0.0 | 0.001 (0.004) | 0.74 | 3.8 |
| SDSBP | 0.001 (0.005) | 0.84 | 0.0 | 0.002 (0.005) | 0.72 | 3.8 |
| SDDBP | -0.003 (0.005) | 0.58 | 0.0 | -0.002 (0.005) | 0.71 | 3.8 |
β means standardized regression coefficient; R2 means a measure for model prediction. The covariates adjusted in model 2 include age, systolic and diastolic blood pressure, physical activity, and current alcohol intake. BSRS: Brief Symptom Rating Scale; ARVSBP: Average real variability for systolic blood pressure variability; ARVDBP: Average real variability for diastolic blood pressure variability; SDSBP: Standard deviation for systolic blood pressure variability; SDDBP: Standard deviation for diastolic blood pressure variability.
DISCUSSION
We found that young military male adults with chronic psychological stress had a higher prevalence of alcohol drinking and less physical activity, reflecting that the BSRS score may be reliable for the evaluation of mental stress[15,16]. The principal finding was that there was no association of chronic psychological stress and its pivotal domains with long-term BPV in young military male adults. A prior study in mice has revealed that acute stress but not chronic stress was associated with short-term BPV (within an hour measurement)[2]. In addition, acute stressors on human beings could lead to an elevation of blood pressure levels and the effect persisted for a while[17]. This finding may make short-term BPV less sensitive to stress as compared with heart rate variability in human beings and similarly in the mouse model[2,18]. Notably, this study was the first one providing the evidence for a null association between chronic psychological stress and long-term BPV.
The results from the mouse experiment also demonstrated that acute stress could increase short-term BPV, which was likely due to sympathetic nervous system activation and baroreflex control impairment[2]. On the contrary, chronic stress might reduce short-term BPV due to the coordination of sympathetic activation and physiological response to the vascular alterations in hypertension[19,20]. Our findings also revealed that the BSRS-5 score was inversely correlated to almost all of the long-term BPV indexes in young male adults despite insignificance. This tendency of inverse association might differ by the components of BSRS-5 score, which was in line with anxiety, depression, and interpersonal sensitivity but contradicted to insomnia.
There were some strengths in this study. First, the questionnaire for BSRS-5, physical examinations, and blood pressure measurements were all performed standardly and in a strict manner at the clinic visit. Second, many unmeasured confounders had been controlled at baseline since daily life of the military such as deployment, physical activity, and stress sources were similar across troops. On the contrary, there were several limitations in this study. First, the results were obtained from the male subjects and might be inappropriately applied for the female subjects. Second, the study had a follow-up period for merely 7 years when the prevalence of hypertension remained low, possibly reducing the degree of association between psychological stress and BPV. Third, we used only a single measurement of blood pressure on each visit, which might be susceptible to change by cigarettes, coffee, and indoor temperature. Although the objective environment and the detailed preparations for blood pressure assessment have been regulated, other confounders such as white coat hypertension might be present in some subjects, possibly resulting in a bias. Lastly, there were only four occasions (every two years in interval) for blood pressure measurement, which would cause wide variations of SD and ARV, resulting in reduced associations for psychological stress. The interval of blood pressure measurement had a long time scale (years instead of months). Therefore, it may promote further studies to either confirm or dispute the conclusions.
CONCLUSION
In conclusion, our findings suggest that chronic psychological stress is not associated with long-term BPV in young males. In addition, this study is the first one revealing a null association between each chronic stress component and long-term BPV in human beings. It is necessary to see whether there might be a change for the relationship with long-term BPV in a longer follow-up when the prevalence of hypertension increases with ageing.
ARTICLE HIGHLIGHTS
Research background
An experiment in mice demonstrated that acute stress might result in increased short-term heart rate variability and blood pressure variability (BPV); however, chronic stress would not alter short-term BPV.
Research motivation
Whether chronic mental stress is associated with long-term BPV remains unclear in human beings.
Research objectives
To examine the association of psychological stress with long-term BPV in young male adults.
Research methods
The association between chronic psychological stress and long-term BPV was examined in 1112 healthy military males, averaged 32.2 years in Taiwan. Psychological stress was quantitatively evaluated using the Brief Symptom Rating Scale (BSRS-5), from the least symptom of 0 to the most severe of 20, and the five components of anxiety, insomnia, depression, interpersonal sensitivity, and hostility (the severity score in each component from 0 to 4). Long-term BPV was assessed by standard deviation (SD) for systolic and diastolic blood pressure (SBP and DBP), and average real variability (ARV), defined as the average absolute difference between successive measurements of SBP or DBP, across four visits in the study period from 2012 to 2018 (2012-14, 2014-15, 2015-16, and 2016-18).
Research results
The results of multivariable linear regressions showed that there were no correlations of the BSRS-5 score with SDSBP, SDDBP, ARVSBP, and ARVDBP after adjusting for all the covariates [β(SE): -0.022 (0.024), -0.023 (0.026), -0.001 (0.018), and 0.001 (0.020), respectively; P > 0.05 for all]. In addition, there were also no correlations between each component of the BSRS score and the long-term BPV indexes.
Research conclusions
Our findings suggest that chronic psychological stress might not be associated with long-term BPV in military young males.
Research perspectives
Future studies should focus on the association between chronic mental stress and long-term BPV which is assessed by a smaller interval of blood pressure measurement (i.e., from years to months).
Footnotes
Institutional review board statement: This prospective study was reviewed and approved by the Institutional Review Board of the Mennonite Christian Hospital (No. 16-05-008) in Hualien, Taiwan.
Informed consent statement: Written informed consent was obtained from all participants.
Conflict-of-interest statement: The authors declare that they have no conflicts of interest to disclose.
STROBE statement: The authors have read the STROBE Statement—checklist of items, and the manuscript was prepared and revised according to the STROBE Statement—checklist of items.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: American Heart Association, No. 216027375.
Peer-review started: July 3, 2020
First decision: October 6, 2020
Article in press: November 4, 2020
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dai X S-Editor: Chen XF L-Editor: Wang TQ P-Editor: Li JH
Contributor Information
Yen-Po Lin, Department of Critical Care Medicine, Yonghe Cardinal Tien Hospital, Yonghe 234, Taiwan.
Chia-Hao Fan, Department of Nursing, Hualien Armed Forces General Hospital, Hualien 97144, Taiwan.
Kun-Zhe Tsai, Department of Dentistry, Hualien Armed Forces General Hospital, Hualien 971, Taiwan.
Ko-Hwan Lin, Department of Psychiatry, Hualien Armed Forces General Hospital, Hualien 97144, Taiwan.
Chih-Lu Han, Department of Medicine, Taipei Veterans General Hospital, Taipei 112, Taiwan.
Gen-Min Lin, Department of Medicine, Hualien Armed Forces General Hospital, Hualien 970, Taiwan. farmer507@yahoo.com.tw.
Data sharing statement
As the study materials were obtained from the military in Taiwan, the data were confidential and not allowed to be opened in public. If there are any needs for clarification, the readers can contact Colonel Dr. Gen-Min Lin, the corresponding author, for sharing the data.
References
- 1.Liu MY, Li N, Li WA, Khan H. Association between psychosocial stress and hypertension: a systematic review and meta-analysis. Neurol Res . 2017;39:573–580. doi: 10.1080/01616412.2017.1317904. [DOI] [PubMed] [Google Scholar]
- 2.Farah VM, Joaquim LF, Bernatova I, Morris M. Acute and chronic stress influence blood pressure variability in mice. Physiol Behav . 2004;83:135–142. doi: 10.1016/j.physbeh.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 3.Lin GM, Li YH, Lee CJ, Shiang JC, Lin KH, Chen KW, Chen YJ, Wu CF, Lin BS, Yu YS, Lin F, Su FY, Wang CH. Rationale and design of the cardiorespiratory fitness and hospitalization events in armed forces study in Eastern Taiwan. World J Cardiol . 2016;8:464–471. doi: 10.4330/wjc.v8.i8.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen YJ, Chen KW, Shih YL, Su FY, Lin YP, Meng FC, Lin F, Yu YS, Han CL, Wang CH, Lin JW, Hsieh TY, Li YH, Lin GM. Chronic hepatitis B, nonalcoholic steatohepatitis and physical fitness of military males: CHIEF study. World J Gastroenterol . 2017;23:4587–4594. doi: 10.3748/wjg.v23.i25.4587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tsai KZ, Lin JW, Lin F, Su FY, Li YH, Lin YP, Lin YK, Han CL, Hsieh CB, Lin GM. Association of betel nut chewing with exercise performance in a military male cohort: the CHIEF study. J R Army Med Corps . 2018;164:399–404. doi: 10.1136/jramc-2017-000899. [DOI] [PubMed] [Google Scholar]
- 6.Tsai KZ, Lai SW, Hsieh CJ, Lin CS, Lin YP, Tsai SC, Chung PS, Lin YK, Lin TC, Ho CL, Han CL, Kwon Y, Hsieh CB, Lin GM. Association between mild anemia and physical fitness in a military male cohort: The CHIEF study. Sci Rep . 2019;9:11165. doi: 10.1038/s41598-019-47625-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chao WH, Su FY, Lin F, Yu YS, Lin GM. Association of electrocardiographic left and right ventricular hypertrophy with physical fitness of military males: The CHIEF study. Eur J Sport Sci . 2019;19:1214–1220. doi: 10.1080/17461391.2019.1595741. [DOI] [PubMed] [Google Scholar]
- 8.Liu PY, Lin YK, Chen KW, Tsai KZ, Lin YP, Takimoto E, Lin GM. Association of Liver Transaminase Levels and Long-Term Blood Pressure Variability in Military Young Males: The CHIEF Study. Int J Environ Res Public Health . 2020;17 doi: 10.3390/ijerph17176094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lin GM, Lu HH. A 12-Lead ECG-Based System With Physiological Parameters and Machine Learning to Identify Right Ventricular Hypertrophy in Young Adults. IEEE J Transl Eng Health Med . 2020;8:1900510. doi: 10.1109/JTEHM.2020.2996370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lin GM, Liu K. An Electrocardiographic System With Anthropometrics via Machine Learning to Screen Left Ventricular Hypertrophy among Young Adults. IEEE J Transl Eng Health Med . 2020;8:1800111. doi: 10.1109/JTEHM.2020.2990073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee MB, Liao SC, Lee YJ, Wu CH, Tseng MC, Gau SF, Rau CL. Development and verification of validity and reliability of a short screening instrument to identify psychiatric morbidity. J Formos Med Assoc . 2003;102:687–694. [PubMed] [Google Scholar]
- 12.Chen HC, Wu CH, Lee YJ, Liao SC, Lee MB. Validity of the five-item Brief Symptom Rating Scale among subjects admitted for general health screening. J Formos Med Assoc . 2005;104:824–829. [PubMed] [Google Scholar]
- 13.Lu IC, Yen Jean MC, Lei SM, Cheng HH, Wang JD. BSRS-5 (5-item Brief Symptom Rating Scale) scores affect every aspect of quality of life measured by WHOQOL-BREF in healthy workers. Qual Life Res . 2011;20:1469–1475. doi: 10.1007/s11136-011-9889-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hastie CE, Jeemon P, Coleman H, McCallum L, Patel R, Dawson J, Sloan W, Meredith P, Jones GC, Muir S, Walters M, Dominiczak AF, Morrison D, McInnes GT, Padmanabhan S. Long-term and ultra long-term blood pressure variability during follow-up and mortality in 14,522 patients with hypertension. Hypertension . 2013;62:698–705. doi: 10.1161/HYPERTENSIONAHA.113.01343. [DOI] [PubMed] [Google Scholar]
- 15.Lin KH, Chen YJ, Yang SN, Liu MW, Kao CC, Nagamine M, Vermetten E, Lin GM. Association of Psychological Stress with Physical Fitness in a Military Cohort: The CHIEF Study. Mil Med . 2020;185:e1240–e1246. doi: 10.1093/milmed/usz469. [DOI] [PubMed] [Google Scholar]
- 16.Lin GM, Nagamine M, Yang SN, Tai YM, Lin C, Sato H. Machine Learning Based Suicide Ideation Prediction for Military Personnel. IEEE J Biomed Health Inform . 2020;24:1907–1916. doi: 10.1109/JBHI.2020.2988393. [DOI] [PubMed] [Google Scholar]
- 17.Hjortskov N, Rissén D, Blangsted AK, Fallentin N, Lundberg U, Søgaard K. The effect of mental stress on heart rate variability and blood pressure during computer work. Eur J Appl Physiol . 2004;92:84–89. doi: 10.1007/s00421-004-1055-z. [DOI] [PubMed] [Google Scholar]
- 18.Fredrikson M, Blumenthal JA, Evans DD, Sherwood A, Light KC. Cardiovascular responses in the laboratory and in the natural environment: is blood pressure reactivity to laboratory-induced mental stress related to ambulatory blood pressure during everyday life? J Psychosom Res . 1989;33:753–762. doi: 10.1016/0022-3999(89)90091-3. [DOI] [PubMed] [Google Scholar]
- 19.Grippo AJ, Beltz TG, Johnson AK. Behavioral and cardiovascular changes in the chronic mild stress model of depression. Physiol Behav . 2003;78:703–710. doi: 10.1016/s0031-9384(03)00050-7. [DOI] [PubMed] [Google Scholar]
- 20.Pagani M, Rimoldi O, Pizzinelli P, Furlan R, Crivellaro W, Liberati D, Cerutti S, Malliani A. Assessment of the neural control of the circulation during psychological stress. J Auton Nerv Syst . 1991;35:33–41. doi: 10.1016/0165-1838(91)90036-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
As the study materials were obtained from the military in Taiwan, the data were confidential and not allowed to be opened in public. If there are any needs for clarification, the readers can contact Colonel Dr. Gen-Min Lin, the corresponding author, for sharing the data.