Abstract
An occlusive large bore sheath is a frequently encountered situation in cases of cardiogenic shock (CS) requiring mechanical circulatory support (MCS). Resultant acute limb ischemia could be a catastrophic complication which significantly affects the prognosis of an already sick patient population. A novel, yet simple, technique using the radial artery, instead of the ipsilateral or contralateral common femoral artery (CFA), as a donor vessel of an external bypass which provides antegrade perfusion to a limb with an occlusive large bore sheath is hereby described. Radial access (RA) has been shown to improve mortality in acute coronary syndrome; however, it is sometimes avoided by some operators in CS cases due to the possible appropriate need for MCS. This technique offers a substitution of a second CFA access for a RA in order to provide adequate ipsilateral limb perfusion. Hence, one can start a CS case with a default RA and perform peripheral angiography after diagnostic cardiac catheterization. If the peripheral vasculature is inappropriate for MCS, the patient would have already benefited from the mortality advantage of RA. If obstructive PAD is absent, then an occlusive Impella sheath can be placed in a CFA after antegrade ipsilateral superficial femoral artery (SFA) access is obtained for an external radial to femoral bypass, while the PCI is performed through the Impella sheath according to the single access PCI technique. Finally, the advantages and disadvantages of this new approach are described and compared with each of the traditionally known external and internal femoral bypass techniques.
Keywords: acute, cardiogenic, extremity, ischemia, lower, shock
1. INTRODUCTION
Indwelling large bore sheath femoral access is more frequently encountered in the critical care unit of the modern era due to the continued evolution of effective mechanical circulatory support (MCS) options. Antegrade limb perfusion is often necessary in this very ill patient population since the consequences of acute ischemic limb loss are dramatic. Limb ischemia raises overall morbidity and mortality 1 to a point where the risk benefit ratio of the placement of MCS may become unreasonable without pre‐emptive antegrade perfusion. 2
Multiple methods of antegrade limb perfusion have been described. 2
Ipsilateral femoral external bypass (Figure 1): From the large bore Impella peel‐away sheath side port to the antegrade ipsilateral SFA sheath through external tubing.
Contralateral femoral external bypass (Figure 2): From a contralateral retrograde common femoral artery (CFA) sheath to an antegrade ipsilateral superficial femoral artery (SFA) sheath through external tubing.
Contralateral femoral internal bypass (Figure 3): From a contralateral retrograde 7 French (Fr) CFA sheath to the ipsilateral profunda femoris artery (PFA) through an up‐an‐over internal 4 Fr sheath which is placed through the 7 Fr contralateral sheath.
FIGURE 1.

Ipsilateral femoral external bypass from the side port of the Impella CP peel‐away sheath to the side port of an antegrade superficial femoral artery (SFA) sheath through a male‐to‐male tubing connector
FIGURE 2.

Contralateral femoral external bypass from a contralateral retrograde common femoral artery (CFA) sheath to an antegrade ipsilateral SFA sheath through external tubing with male‐to‐male connector
FIGURE 3.

Contralateral femoral internal bypass from a contralateral retrograde 7 French (Fr) CFA sheath to the ipsilateral profunda femoris artery (PFA) through an up‐an‐over internal 4 Fr sheath which is placed through the 7 Fr contralateral sheath
All three methods use the external iliac artery as a donor vessel for the affected limb perfusion. We hereby describe a clinical case which outlines a novel approach using ipsilateral radial access (RA) as primary inflow for the external bypass circuit (Figure 4). We believe this technique has a more favorable risk/benefit ratio when compared with the femoral or iliac arteries. We then discuss the advantages and disadvantages of each antegrade limb perfusion technique.
FIGURE 4.
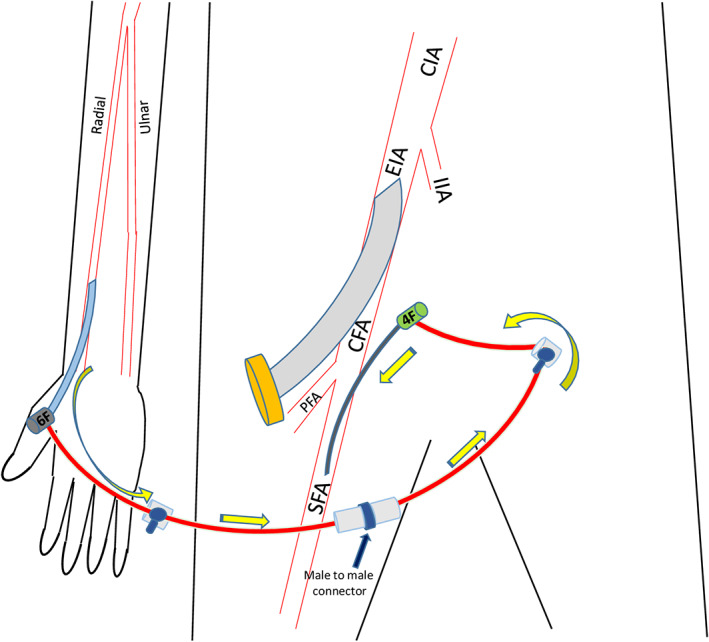
Radial to femoral external bypass technique: From the side port of a radial artery 6 Fr sheath to the side port of antegrade SFA 4 Fr sheath through external tubing with male‐to‐male connector
1.1. Case
A 52‐year‐old male with history of obstructive coronary disease status post multiple percutaneous coronary interventions and ischemic cardiomyopathy presented to the emergency department for gradually worsening severe dyspnea at rest in the last 3 days and severe chest pressure. His examination revealed moderate respiratory distress, hypotension, tachycardia, jugular venous distention, S3 gallop, bilateral rales in lower and mid lung fields, and mottled cool lower extremities with 3+ edema. Electrocardiogram revealed a new complete left bundle branch block which was considered an ST‐elevation myocardial infarction equivalent. The patient was taken emergently to the cardiac catheterization laboratory in cardiogenic shock (CS) and was intubated.
Coronary angiography performed from a right RA revealed multiple patent stents without significant in‐stent restenosis or thrombosis and no recurrent obstructive epicardial disease. Left ventricular filling pressure was severely elevated. Urgent limited transthoracic echocardiography (TTE) revealed severe left ventricular systolic dysfunction (ejection fraction of 10%) with severe left ventricular dilatation and severe global hypokinesis.
Norepinephrine and epinephrine drips were quickly up titrated during the diagnostic case to maintain adequate systemic perfusion. An Impella CP was then emergently implanted from an ultrasound (US) guided right CFA micropuncture access after distal abdominal aortography with bilateral iliac arteriography, performed from the RA, revealed no evidence of obstructive arterial disease. TTE confirmed an adequate inlet position and mechanical support was quickly increased up to a maximum of 3.5 L/min.
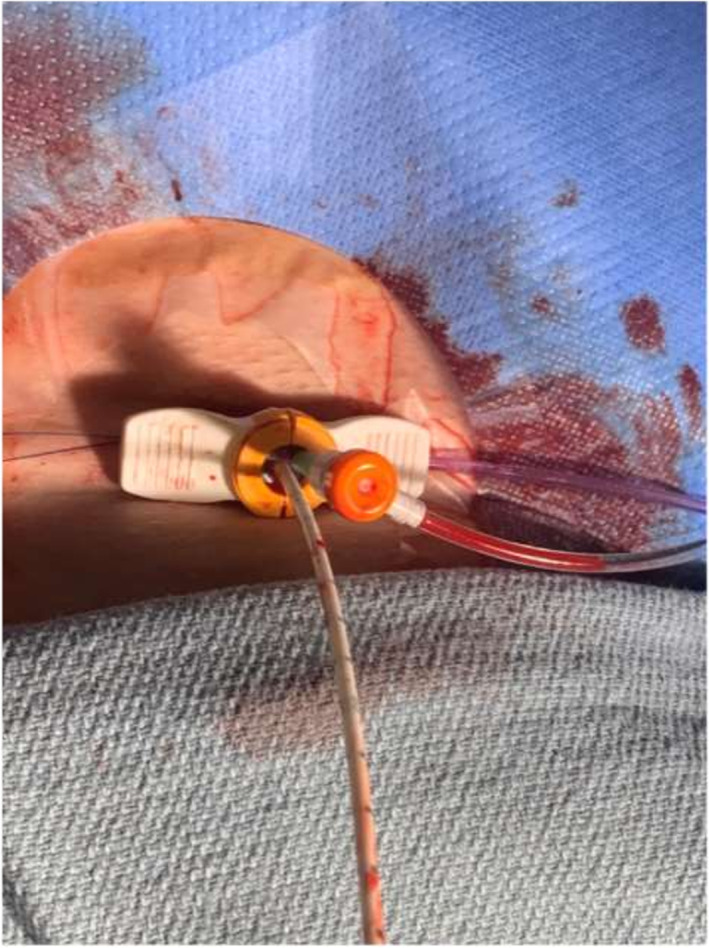
Right CFA angiography performed from the side port of the 14 Fr sheath revealed absent flow below the access site. In order to allow for right lower extremity (LE) perfusion, an antegrade 4 Fr SFA sheath was placed under US guidance using the micropuncture technique.
Since right RA had been obtained for the diagnostic procedure—this access being a default arterial access for cardiac catheterization even for CS cases in our laboratory—and in order to decrease the very high morbidity of this patient, we thought it would be reasonable to avoid a third arterial access (contralateral CFA) by connecting the right RA 6 Fr sheath as a donor vessel to the antegrade right SFA 4 Fr receiver sheath, with a male to male tubing connector (Figures 5 and 6).
FIGURE 5.

Right radial to right superficial femoral external bypass
FIGURE 6.
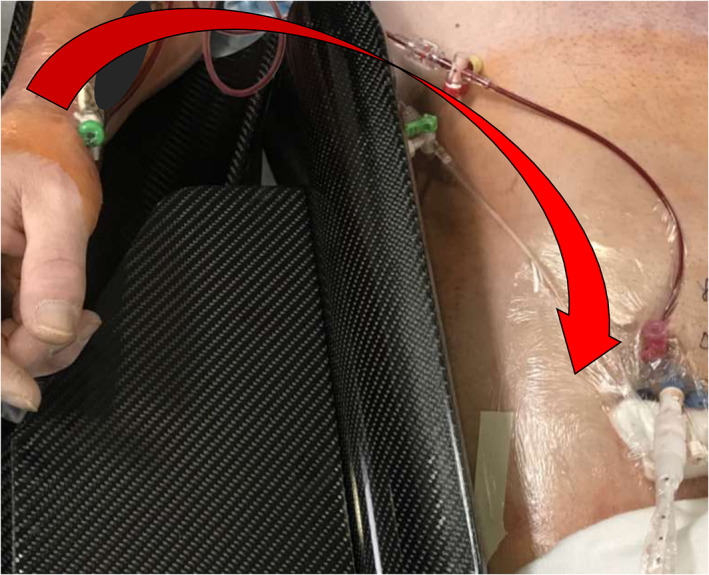
Right radial to right superficial femoral external bypass
To our knowledge, this is the first reported case of an external radial to femoral bypass (RFB) technique for antegrade perfusion of a LE with an indwelling occlusive arterial sheath.
This RFB was effective in maintaining symmetrical LE perfusion throughout the patient's hospital stay while recovering from CS with an occlusive Impella CP sheath. It prevented limb amputation, which by itself, adds a large burden of morbidity and mortality in this already severely ill patient population (Figure 7).
FIGURE 7.

Effective limb perfusion with radial to femoral bypass which prevented an amputation
2. DISCUSSION
Whatever approach is adopted and if the hemodynamics allow, it is generally recommended to be proactive rather than reactive and get an antegrade SFA access before the placement of an indwelling large bore sheath. 3 This also makes antegrade access technically easier.
Table 1 summarizes the downsides of the traditional techniques and the rationale behind the need for this less invasive approach. We hereby discuss the pros and cons of each bypass option:
-
Ipsilateral femoral external bypass:
-
Pros:
No need for additional contralateral access (less morbidity and procedural time)
No need for RA for the diagnostic catheterization and percutaneous coronary intervention (PCI) with the advent of the single access for high risk PCI (SHiP) technique 4 (Figure 8) which allows for faster setup and lower procedural time. This technique consists of placing up to a 7 Fr sheath through the valve of the 14 Fr Impella CP sheath, alongside the Impella catheter, to allow for PCI through a single access instead of a separate arterial access
No compromise of the contralateral LE perfusion
-
-
Cons:
Necessity to keep the Impella peel‐away sheath in place instead of the repositioning sheath which increases thrombosis risk even while on therapeutic anticoagulation
Ipsilateral iliac inflow affected by the 9 Fr Impella catheter even in the absence of obstructive disease
Further limitation of ipsilateral iliac inflow by pseudolesions created by the straightening effect of stiff sheath/catheter combination
-
Contralateral femoral external bypass:
-
Pros:
Ease of the traditional retrograde femoral access (FA) technique
No limitations of contralateral iliac inflow in the absence of obstructive disease
-
Cons:
Added morbidity of a second FA
Limitation of outflow to the contralateral limb which is already compromised by CS: Contralateral limb perfusion already halved by the presence of a CFA sheath, now reduced to ¼ of baseline flow since half of the remaining flow is shunted to the contralateral side
Suboptimal ergonomics
-
-
Contralateral femoral internal bypass:
-
Pros:
-
No external portion of the bypass circuit
Easier setup for the nursing staff
Less potential for infections
-
-
Cons:
More flow limiting to contralateral limb (7 Fr)
Higher potential for catheter thrombosis with sheath in sheath approach even with adequate anticoagulation
Higher risk of iliac artery thrombosis around crossover sheath with serious consequences
Sheath hemostatic valve prone to bleeding with sheath‐in‐sheath approach
Peripheral vascular interventional skills required
Additional catheters, sheaths and wires needed
More radiation
More contrast
Time consuming
Potential for vascular injury with advancement of the up‐and‐over sheath next to the large bore sheath (especially if calcified)
Outflow into ipsilateral PFA: Not a guarantee for adequate perfusion of infrapopliteal vessels
Higher cost
-
TABLE 1.
Major advantages and disadvantages of arterial bypass techniques for maintenance of antegrade perfusion in limbs with occlusive sheaths.
| Advantages | Disadvantages | |||
|---|---|---|---|---|
| Ipsilateral external bypass |
|
|
||
| Contralateral external bypass |
|
|
||
| Contralateral internal bypass |
|
|
|
|
| Radial to femoral external bypass |
|
|
|
|
Abbreviations: CABG, coronary artery bypass grafting; CS, cardiogenic shock; ECPELLA, extra‐corporeal membrane oxygenation plus imPELLA; LE, lower extremity; PAD, peripheral arterial disease; PFA, profunda femoris artery; SHiP, single access in high risk percutaneous coronary interventions; UE, upper extremity; US, ultrasound.
FIGURE 8.
SHiP technique: Single access in High risk Percutaneous coronary interventions. A 6 or 7 Fr sheath is placed through the valve of a 14 Fr Impella CP sheath alongside the Impella CP catheter which allow for PCI and mechanical circulatory support (MCS) to be used through the same access site
On the other hand, the new external RFB technique, offers the following 15 unique advantages in this sick patient population:
It is associated with significantly better clinical outcomes as evidenced in the transcatheter aortic valve replacement (TAVR) population. 5
RA being favorably the default access in a large proportion of catheterization laboratories, there is no substantial benefit in getting an additional FA site for a total of three arterial access sites. This translates into more procedural time, radiation, and morbidity.
If radial was not the primary access, it is less risky in terms of bleeding risk to stick the radial artery rather than the femoral artery of a fully anticoagulated patient.
With the advent and increased adoption of the SHiP technique 4 (Figure 8) in CS patients who are likely going to require maintenance of MCS after the case, instead of using radial as primary PCI access site while the limb is ischemic from the occlusive Impella sheath, the RA can be used to perfuse the ipsilateral LE while PCI is being performed from a single access Impella sheath. This will potentially result in less vascular complications and better outcomes.
There is less infectious risk (especially when compared with closure devices deployed through an indwelling sheath for a few days, as aseptic as the technique can get).
More physiologically continuous circuit from radial to contiguous ipsilateral femoral rather than discontinuous crossover flow.
Upper extremity inflow is often less diseased than iliac inflow. Additionally, a radial sheath has the same size of a femoral donor sheath so it delivers the same amount of flow.
In the setting of shock and vasopressor support, upper extremity ischemia is less frequent than lower extremity ischemia. It seems more logical to spare the less perfused limb from a donor sheath.
It is a simple and more ergonomically friendly setup since RA is closer to the operator than contralateral FA.
It does not compromise the perfusion of the upper limb in the large majority of patients. In contrast, the contralateral LE flow is reduced by 75% with the femoro‐femoral external bypass technique. This does not usually cause significant contralateral limb ischemia in patients without baseline infra‐inguinal arterial disease, however, when combined with shock induced distal vasospasm and baseline non obstructive infra‐popliteal disease (which is frequent in this often diabetic patient population) it can lead to severe distal hypoperfusion.
Consequences of radial artery occlusion are way less significant than contralateral CFA occlusion. The latter severely affects prognosis and requires another endovascular/open surgical procedure.
Sheaths are less prone to kinking at the wrist rather than the groin.
Wrist splints still allow for arm mobility without significant restriction, while moving the legs with an external femoral bypass has more tendency to jeopardize sheath flow.
If the patient requires the addition of peripheral ECMO to Impella (ECpella), the contralateral groin is available for that (with antegrade perfusion from the left radial) rather than used for antegrade perfusion of the ipsilateral limb.
-
The particular advantages over the internal bypass technique include:
RA does not require peripheral vascular interventional skills
It perfuses the SFA and not the PFA
There is no risk of vascular injury around the ipsilateral large bore sheath
Conversely, there are no techniques without downsides. However, most of these disadvantages can be overcome with simple solutions
RA may be challenging in CS patients due to a more thready pulse and spasm at baseline. This can be overcome easily with the use of ultrasound guidance (high frequency probe).
The radial artery is more prone to spasm than the femoral artery, however, topical application of nitroglycerin on the forearm, even in the setting of vasopressor therapy, may help. Other factors that may help include warm blankets around the arm, a higher Ptt goal closer to 80 and a 1 Fr downsize of the receiver sheath.
-
Longer radial sheath dwell times imply two specific risks:
Hand ischemia in cases where the radial artery is dominant, hence the absolute necessity of a noninvasive assessment of palmar arch patency (Allen's or Barbeau 6 tests), prior to the adoption of the RFB strategy. The current Society of Cardiovascular Angiography and Interventions (SCAI) expert consensus statement update on best practices of transradial angiography and interventions, 7 which does not recommend routine hand noninvasive collateral testing as a triage tool for access site selection, does not apply to this situation, since the radial sheath is expected to remain in place for a relatively prolonged duration of time.
Higher probability of radial artery occlusion when compared with occlusion rates after cardiac catheterization or PCI. Hence, a shorter deflation protocol is recommended and a simultaneous transient ulnar compression increases radial artery patency rates. 8
If the patient requires additional coronary arterial grafting, one less potential graft is available for this purpose.
This approach is more susceptible to sheath dislodgement due to the wider range of motion of the upper extremities (especially in confused and agitated CS patients) compared with groin/leg movements in patients on strict bedrest. Strict critical care nursing measures are necessary to limit the range of motion of the upper extremity providing the donor vessel of the external bypass circuit, as well as the other upper extremity to prevent reaching and pulling of the external bypass. This may require transient restraints.
3. CONCLUSION
RFB seems to be a simple, less invasive, fast, and effective method for the maintenance of limb perfusion in patients with CS who require occlusive MCS. It offers all the known advantages of RA when compared with FA while delivering the same flow. Large prospective studies are required to confirm these findings in a similar patient population.
Lichaa H. The “lend a hand” external bypass technique: External radial to femoral bypass for antegrade perfusion of an ischemic limb with occlusive large bore sheath ‐ A novel and favorable approach. Catheter Cardiovasc Interv. 2020;96:E614–E620. 10.1002/ccd.29187
REFERENCES
- 1. Huang M, Ong BH, Hoo AEE, et al. Prognostic factors for survival after extracorporeal membrane oxygenation for cardiogenic shock. ASAIO J. 2020;66(2):141‐145. [DOI] [PubMed] [Google Scholar]
- 2. Kaki A, Alraies MC. Antegrade limb perfusion techniques: occlusive sheath management In: Shroff A, Pinto D, eds. Vascular access, management, and closure best practices. Suite 400, WA: The Society for Cardiovascular Angiography and Interventions (SCAI); 2019:164‐167. [Google Scholar]
- 3. Kaki A, Alraies MC, Kajy M, et al. Large bore occlusive sheath management. Catheter Cardiovasc Interv. 2019. Mar 1;93(4):678‐684. 10.1002/ccd.28101. [DOI] [PubMed] [Google Scholar]
- 4. Wollmuth J, Korngold E, Croce K, Pinto DS. The single‐access for hi‐risk PCI (SHiP) technique. Catheter Cardiovasc Interv. 2020;96(1):114‐116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Junquera L, Urena M, Latib A, et al. Comparison of transfemoral versus transradial secondary access in transcatheter aortic valve replacement. Circ Cardiovasc Interv. 2020;13(3):e008609 10.1161/CIRCINTERVENTIONS.119.008609. [DOI] [PubMed] [Google Scholar]
- 6. Barbeau G. Evaluation of the ulnopalmar arterial arches with pulse oximetry and plethysmography: comparison with the Allen's test in 1010 patients. Am Heart J. 2004;147:489‐493. [DOI] [PubMed] [Google Scholar]
- 7. Shroff AR, Gulati R, Drachman DE, et al. SCAI expert consensus statement update on best practices for transradial angiography and intervention. Catheter Cardiovasc Interv. 2020;95(2):245‐252. [DOI] [PubMed] [Google Scholar]
- 8. Koutouzis MJ, Maniotis CD, Avdikos G, Tsoumeleas A, Andreou C, Kyriakides ZS. Ulnar artery transient compression facilitating radial artery patent hemostasis (ULTRA): a novel technique to reduce radial artery occlusion after transradial coronary catheterization. J Invasive Cardiol. 2016;28(11):451‐454. [PubMed] [Google Scholar]


