Abstract
Purpose
The purpose of this study was to review systematically the literature concerning postoperative management following arthroscopic Bankart repair for traumatic anterior shoulder instability in adolescent and young adult (≤ 25 years) athletes.
Methods
The Pubmed, Medline, EMBASE, EBSCO (CINAHL), and Google Scholar databases were systematically searched according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines to identify all studies reporting postoperative rehabilitation guidelines following arthroscopic Bankart repair in the adolescent and young adult population. The Methodological Index for Nonrandomized Studies instrument and Modified Coleman Methodology Score were used for quality assessment of the included studies. All aspects of rehabilitation were extracted and analyzed, including type/duration of immobilization, range of motion, strength, and return to sport (RTS) criteria.
Results
Screening yielded 17 eligible studies with a total of 675 patients and an average age of 18.3 years. There was considerable variation with regard to reported postoperative rehabilitation guidelines. Of the 17 studies, 15 reported the duration of immobilization; there was a mean of 4 weeks (range, 2-6 weeks). Range of motion and strength restrictions were reported in 15 (88.2%) and 13 (76.4%) studies, respectively. All of the 17 studies included an expected timeframe for RTS, but only 5 of the studies (29.4%) included either subjective or objective criteria to determine safe RTS. Differences in outcomes were unable to be assessed due to large study heterogeneity.
Conclusion
Considerable variation is reported in postoperative rehabilitation guidelines following arthroscopic Bankart repair for traumatic shoulder instability in the adolescent and young adult population. All studies used time-based criteria for determining RTS, but subjective and/or objective criteria were lacking in the majority of studies. The current literature lacks data to generate evidence-based rehabilitation protocols in this young athletic population.
Level of Evidence
Level IV, systematic review of Level II-IV studies.
Traumatic shoulder dislocations are prevalent in adolescents participating in contact or collision sports, and over 90% of these injures are anterior.1,2 Nonsurgical treatment options, including physical therapy, carry a risk of recurrent dislocation between 71% and 92% in an adolescent population.3, 4, 5, 6 To minimize the negative sequelae associated with recurrent instability, including glenohumeral arthritis, arthroscopic repair has been advocated.7, 8, 9, 10, 11 Arthroscopic repair has led to improved patient-reported outcomes, yet high rates of recurrent instability still occur specifically in this at-risk population. In a systematic review by Kasik et al.,12 recurrent instability after arthroscopic repair in adolescents was reported to be 35.9% and 13.8% in contact and collision athletes, respectively. In addition, athletes who underwent arthroscopic repair had a 79.8% rate of return to sport (RTS) to preinjury levels.
Following arthroscopic repair, rehabilitation plays a vital role in promoting tissue healing, protecting the surgical site postoperatively and regaining motion and strength. However, rehabilitation protocols and follow-up reports are inconsistent and are lacking in adolescents and young adults. A rehabilitation guideline for anterior arthroscopic capsulolabral repair of the shoulder was published by the American Society of Shoulder and Elbow Therapists in 2010,13 but it provides only recommendations rather than an evidence-based protocol. Establishing strict guidelines may optimize patient-reported outcomes, minimize recurrent instability and contribute to an athlete’s successful RTS.
The purpose of this study was to review systematically the literature concerning postoperative management following arthroscopic Bankart repair for traumatic anterior shoulder instability in adolescent and young-adult (≤ 25 years) athletes. Our hypothesis was that there is considerable variation in reported postoperative rehabilitation guidelines after arthroscopic Bankart repair in this population.
Methods
Search Strategy and Criteria
The study was exempt from Institutional Review Board approval. It was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.14 A search was conducted on September 28, 2019, of the PubMed, Medline, EMBASE, EBSCO (CINAHL), and Google Scholar databases for clinical studies reporting outcomes following arthroscopic Bankart repair for anterior shoulder instability in an adolescent population. There was no time restriction. The search strategy combined the following terms: adolescent, teenager, young adult, Bankart, joint instability, recurrent dislocation, recurrent shoulder dislocation, shoulder dislocation, and subluxation. A third-year medical student and attending orthopedic surgeon independently screened titles and abstracts for relevant articles. Full texts were reviewed when a decision regarding inclusion or exclusion could not be made on the basis of the title and/or abstract alone. The reference lists of the included studies and recent review articles were also examined to identify any additional relevant studies.
Studies meeting the following criteria were included in the review: (1) clinical studies reporting outcomes after arthroscopic Bankart repairs in adolescent or young adult (≤ 25 years) athletes; (2) studies involving patients with a unidirectional anterior instability pattern following a traumatic shoulder dislocation; and (3) 1-year minimum follow-up. Exclusion criteria were as follows: (1) non-English-language studies; (2) abstract-only publications, reviews articles, technical notes, basic science, case reports, expert opinions, and revision-only case series; (3) studies containing previously published data; and (4) studies in which no age was specified and studies of populations with age ranges that exceeded 25 years (e.g., 14-35 years).
Data Extraction
Data were extracted from included papers by 1 of the investigators and verified by the second investigator. The data retrieved included the following information: title, author, year, location, study design, level of evidence, mean age, age range, sample size, and average length of follow-up. All aspects of rehabilitation were extracted, including type/duration of immobilization, range of motion (ROM), strength, and RTS criteria.
Quality Assessment
The methodological quality and risk of bias of the included studies were evaluated by 2 investigators using the Methodological Index for Non-randomized Studies (MINORS) instrument15 and the Coleman Methodology Score.16 MINORS is a valid instrument designed to assess methodological quality of nonrandomized surgical studies and consists of 12 items, the first 8 being specifically for noncomparative studies. The global ideal score was 16 for noncomparative studies and 24 for comparative studies. The Coleman Methodology Score is a 2-part (A and B), 10-item questionnaire that gives rise to a score between 0 and 100. A higher score represents a study design that avoids the influence of chance, bias and confounding factors. The total number of points correlates with the poor (0-49 points), fair (50-69 points), good (70-84 points), or excellent (85-100 points) quality of the study.17 The Coleman Methodology Score was modified to make it relevant and applicable to our systematic review. There were no disagreements between the 2 reviewers.
Data Analysis
Data abstracted from all included studies were tabulated in Microsoft Excel (2012 version; Microsoft, Redmond, Washington). Descriptive statistics were calculated. Continuous variables were reported as means ± SD (standard deviation). Categorical variables were reported as frequencies with percentages.
Results
Study Characteristics and Patient Demographic Data
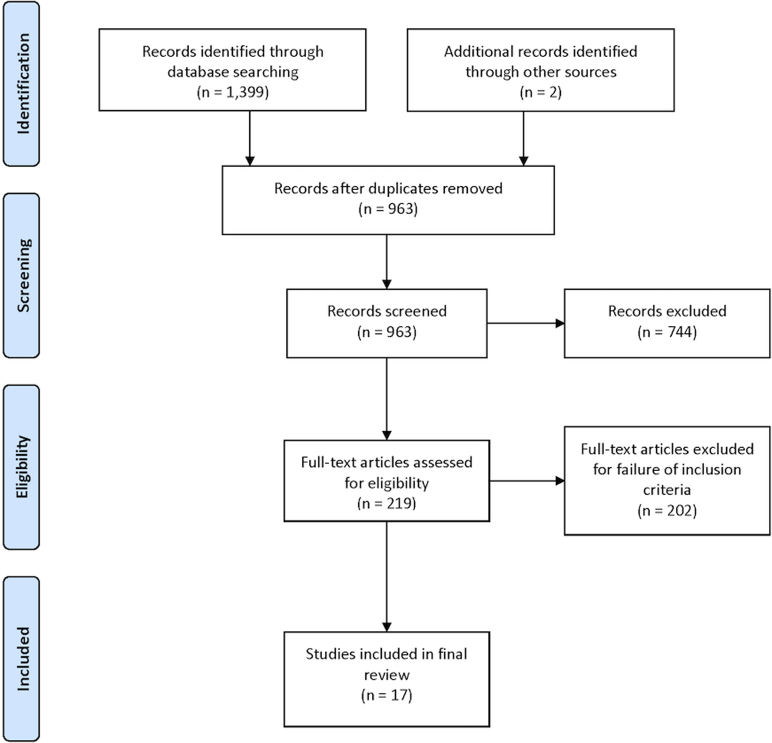
From the 1,399 articles identified in the original search, only 17 studies met the appropriate criteria and were included for final analysis (Fig 1). The characteristics of the selected studies are presented in Table 1. All included articles were published between 1994 and 2019. Of the studies, 10 were conducted in the United States,2,5,18, 19, 20, 21, 22, 23, 24, 25 2 in the United Kingdom,26,27 2 in Italy,6,28 and 1 study each in France,29 Greece/Germany30 and Estonia.31 The articles included in this review involved a total of 675 patients (690 shoulders). The mean sample size in all the studies was 39.7 patients (40.6 shoulders) with a mean age of 18.3 years. The age range of all included studies was 11-25 years. All studies had a 1-year minimum follow-up, and follow-up ranged from 12 months to 120 months.
Fig 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram.
Table 1.
Characteristics of Included Studies
| Study | Year | Location | Mean Age (yrs.) | Sample Size (N) | Mean Follow-up (months) | MINORS Score |
CMS Score |
Level of Evidence |
|---|---|---|---|---|---|---|---|---|
| Arciero et al.5 | 1994 | USA | 20.5 (18-24) | 21 | 32 | 20∗ | 63 | II |
| Castagna et al. 28 | 2012 | Italy | 16 (13-18) | 65 | 63 | 10 | 66 | IV |
| Chapus et al. 29 | 2015 | France | 20.5 (15-25) | 20 | 116.4 | 12 | 73 | IV |
| De Carli et al. 6 | 2019 | Italy | 22.8 (15-25) | 60 | 82.3 | 19∗ | 81 | II |
| DeBerardino et al.19 | 2001 | USA | 20 (17-23) | 49 | 37 | 12 | 71 | IV |
| Dickens et al.18 | 2017 | USA | 20 (18-23) | 50 | 38.4 | 12 | 73 | III |
| Gigis et al. 30 | 2014 | Greece/Germany | 16.7 (15-18) | 38 | 36 | 19∗ | 75 | II |
| Hughes et al.20 | 2018 | USA | 17.7 (15-20) | 20 | 45.6 | 18∗ | 63 | III |
| Jones et al.21 | 2007 | USA | 15.4 (11-18) | 32 | 25.2 | 18∗ | 58 | III |
| Kramer et al.22 | 2019 | USA | 16.03 (13-18) | 36 | 35.6 | 11 | 50 | IV |
| Mazzocca et al.2 | 2005 | USA | 16.6 (13-23) | 18 | 36.6 | 11 | 64 | IV |
| Nixon et al.26 | 2015 | UK | 16.8 (14-18) | 61 | 22 | 9 | 55 | III |
| Owens et al. 23 | 2009 | USA | 20.3 (17-23) | 40 | 140.4 | 11 | 76 | IV |
| Ozturk et al.24 | 2013 | USA | 19.5 (12-24) | 58 | 27 | 11 | 81 | IV |
| Rahu et al.31 | 2018 | Estonia | 21 (16-25) | 16 | 32 | 11 | 72 | IV |
| Saper et al. 25 | 2017 | USA | 16.9 (15-19) | 39 | 75.6 | 11 | 76 | IV |
| Torrance et al.27 | 2018 | UK | 16.3 (14-17) | 67 | 33 | 11 | 73 | IV |
CMS, Coleman Methodology Score; MINORS, Methodological Index for Non-randomized Studies.
Global ideal score is 24 for a comparative study.
Quality Assessment
Most studies were Level IV studies (case series).2,19,22, 23, 24, 25,27, 28, 29,31 There were 4 Level III studies (retrospective group)18,20,21,26 and 3 Level II studies (prospective group).5,6,30 The average MINORS score for the noncomparative studies was 11 (range, 9-12), whereas the average MINORS score for the comparative studies was 18.8 (range, 18-20) (Table 1). The mean modified Coleman score was 68.8 (range, 50-81). Seven studies were ranked as fair,2,5,20, 21, 22,26,28 and 10 studies were ranked as good.6,18,19,23, 24, 25,27,29, 30, 31
Rehabilitation Protocols
There was considerable variation with regard to reported postoperative rehabilitation guidelines. All of the included studies provided information about some type of postoperative shoulder immobilization. The most common duration of immobilization was 4 weeks (8 of 17 studies, 47%).5,6,19,21,23,24,28,31 Sixteen of 17 studies required a period of immobilization; 1 study used a sling for comfort only.26 Of the studies, 6 used a shoulder immobilizer,5,19,21, 22, 23,29 and 7 studies used a sling for immobilization.2,6,18,24,25,28,30 A sling and swathe were given to patients in 2 studies6,24; 3 studies did not specify the type of immobilization utilized.20,27,31
The position of immobilization was listed specifically in 5 studies and varied among them. In 2 studies, the arm was positioned in adduction and internal rotation but used different types of immobilization; Jones et al.21 used a shoulder immobilizer, and De Carli et al.6 used a sling and swathe brace when positioning patients in adduction and internal rotation. One study used a sling with an abduction pillow.25 Another study used a sling in 15° of abduction and 15° of external rotation.28 The final study used a shoulder immobilizer in 30° of external rotation.22
Of the 17 studies, 15 included specific guidelines for postoperative ROM restrictions and duration of restriction (Table 2).2,6,18, 19, 20, 21, 22, 23, 24, 25,27, 28, 29, 30, 31 These restrictions varied between prohibiting all ROM, active-assisted motion, active motion, passive motion, external rotation, abduction, and flexion/extension of the shoulder between 2 and 12 weeks. There was no consensus among these studies about the duration of restriction, type of motion restricted (i.e., active, active-assisted passive) or plane of motion restricted (i.e., abduction, external rotation, etc.) Thirteen studies reported a specific time to initiate muscle strengthening (Table 2).5,6,18, 19, 20, 21, 22, 23, 24, 25,27,28,30 Of the 13 studies, only 5 emphasized strengthening of specific muscle groups, typically the rotator cuff, deltoid and periscapular muscles.21,28 Only 1 of the 13 studies discussed an aggressive strengthening regime for patients involved in more demanding activities.25
Table 2.
ROM Restriction and Duration, Strengthening, Return to Sport
| Study | ROM Restriction | Duration of ROM Restriction | Initiation of Strengthening | Targeted Strengthening | Return to Sport |
|---|---|---|---|---|---|
| Arciero et al.5 | Week 4 | Rotator cuff and scapular muscles | 4 Months | ||
| Castagna et al.28 | Active-assisted and passive shoulder abduction | 4 weeks | Week 8 | Rotator cuff, deltoid and periscapular muscles | 5 Months if return to normal ROM, shoulder muscle strength and endurance |
| Chapus et al.29 | Active-assisted and passive movements | 3 weeks | 3 months | ||
| De Carli et al.6 | Abduction and flexion of the shoulder | 4 weeks | Week 4 | Rotator cuff and scapular muscles | 4 months for noncontact sports |
| 5 months for contact sports | |||||
| DeBerardino et al.19 | Any ROM | 4 weeks | Week 8 | 4 months | |
| Aggressive external rotation | 6 weeks | ||||
| Dickens et al.18 | Any ROM | 12 weeks | Week 12 | 6 months | |
| Gigis et al.30 | Active shoulder movements | 3 weeks | Week 12 | 5 months | |
| Hughes et al.20 | Passive and active-assisted range of motion | 2-4 weeks | Approximately week 6-8 | 6 months | |
| Jones et al.21 | Active and active-assisted ROM | 4 weeks | Week 8 | Rotator cuff, deltoid and periscapular muscles | 4 months |
| Kramer et al.22 | Any ROM | 6 weeks | Week 12 | Dependent on sport-specific training and sport/activity demands | |
| Mazzocca et al.2 | Active assisted ROM | 2 weeks | 6 months, depending on ROM and strength comparison to contralateral shoulder | ||
| Nixon et al.26 | Upon completion of sport-specific rehabilitation | ||||
| Owens et al.23 | Any ROM | 4 weeks | Week 8 | 4 months | |
| Aggressive external rotation | 6 weeks | ||||
| Ozturk et al.24 | Active-assisted ROM | 3 weeks | Week 6 | Rotator cuff, deltoid and scapular muscles | 6 months |
| Active ROM in all planes | 5 weeks | ||||
| Rahu et al.31 | Passive ROM | 4 weeks | 4 months | ||
| Saper et al.25 | Active external rotation, extension, or abduction of the shoulder | 6 weeks | Week 7 | Upon completion of rehabilitation protocol (approximately 7 months) | |
| Torrance et al.27 | Any ROM | 2-4 weeks | Week 2-4 | 3 months |
ROM, range of motion.
The most common criterion used for determination of RTS was time from surgery (Table 2). Of the 17 studies, 12 listed a specific time (range, 3-6 months postoperatively) that they allowed athletes to RTS, and this was the only listed qualification for RTS.5,6,18, 19, 20, 21,23,24,27,29, 30, 31 Four studies modified their time restriction based on return of normal strength, ROM and endurance,28 comparison to the contralateral limb2 or after specific sport training and activity demands.22,26 One study based RTS clearance on completion of a dedicated rehabilitation protocol.25
Discussion
The principal findings of this study showed that no specific rehabilitation guidelines exist following arthroscopic repair for anterior shoulder instability. Significant variability exists regarding immobilization protocol, ROM, strengthening regimen, and RTS. In general, initial protection of the repair was achieved with either a shoulder immobilizer or a sling for 3-6 weeks postoperatively. ROM guidelines were reported in most studies but differed in length of time, motion restriction and plane of motion restriction. Initiation of strengthening was highly variable, occurring between 2 and 12 weeks. Clearance for RTS occurred between 3 and 6 months; some studies implemented specific requirements prior to RTS. Rehabilitation is crucial in preparing athletes involved in contact and collision sports to return back to preinjury levels of sport, but little evidence exists regarding which protocols are superior. In this review, it was difficult to determine the optimal rehabilitation strategies due to the variability in rehabilitation protocols. The heterogeneous population of each study further contributed to the difficulty in establishing a standardized rehabilitation protocol.
There are insufficient data regarding which form of immobilization is superior, and the form relies mostly on the surgeon’s discretion. The 2 primary forms of immobilization after an arthroscopic Bankart repair were either a shoulder immobilizer or a sling for an average of 4 weeks. Length of immobilization is a complex challenge because it requires a balance between protecting the repair by restricting ROM and preventing recurrent instability because of early ROM. Prolonged immobilization can lead to decreased muscle tone and strength, which would be particularly disadvantageous in athletic young adults aiming to return to preinjury levels.32 Similar to the length and type of immobilization, no guidelines regarding position of immobilization have been established. Limited evidence exists in determining whether external rotation results in improved outcomes, especially in young contact athletes. It was initially thought that because external rotation can stress the capsular repair, external rotation should be limited during the early periods of rehabilitation.33
Postoperative ROM restrictions and strengthening are imperative to maintain repair integrity and to promote healing, respectively. Despite a 3-phase protocol released by the American Society of Shoulder and Elbow Therapists,13 no accepted standard of care after an arthroscopic Bankart repair exists. Most studies in our review had a specific period of ROM restriction and strengthening regimen, but studies reporting which rehabilitation protocol are superior is lacking. Some studies have suggested accelerated rehabilitation to be beneficial. In a study by Kim et al.,34 patients in the accelerated rehabilitation group, which entailed immediate ROM and strengthening, were found to regain external rotation faster, return to their previous activity more quickly and experience less pain. However, this study was not limited to a young athletic population. In a separate study geared towards a young athletic population (< 30 years old) and using an accelerated rehabilitation protocol, earlier recovery and good functional outcomes were seen.35 Minimizing stiffness and limiting stress play important roles in determining the optimum length of ROM restriction and the initiation of strengthening in young athletes. These rely mostly on the surgeon’s discretion until further studies regarding ROM restriction and strengthening regimes have been investigated.
Also, a clearly defined time period determining when young athletes should be allowed to RTS has not been established. There is substantial variability among each study for RTS in our review, ranging from 3 to 6 months. Some studies required specific qualifications prior to returning to sports at the designed time period. The lack of consensus may be due to the multifaceted factors that play roles ranging from postoperative healing, return of strength, extent of lesion, and personal desire to reach preinjury level.36, 37, 38 These factors further contribute to the difficulty in defining an evidence-based and standardized timeline, therefore relying heavily upon clinicians’ discretion.
Limitations
The main limitation of this study is the quality of the included studies. The systematic review identified only 17 studies meeting our inclusion criteria, demonstrating the currently limited published evidence in regard to arthroscopic Bankart repair in adolescents and young adults. It is possible that some important studies may have been missed, and there may be numerous unpublished studies on this topic. Also, this review looked solely at the studies published in the English language and, as such, may contribute to a level of publication bias.
Conclusion
There is considerable variation in reported postoperative rehabilitation guidelines following arthroscopic Bankart repair for traumatic shoulder instability in the adolescent and young adult population. All studies used time-based criteria for determining RTS, but subjective and/or objective criteria were lacking in the majority of studies. The current literature lacks data to generate evidence-based rehabilitation protocols in this young athletic population. Although challenging, further studies evaluating the efficacy of various postoperative rehabilitation guidelines are needed.
Footnotes
The authors report the following conflicts of interest or sources of funding: M.G.S. has received consulting fees, education/travel/lodging support, and research support from Arthrex, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Good C.R., MacGillivray J.D. Traumatic shoulder dislocation in the adolescent athlete: advances in surgical treatment. Curr Opin Pediatr. 2005;17:25–29. doi: 10.1097/01.mop.0000147905.92602.bb. [DOI] [PubMed] [Google Scholar]
- 2.Mazzocca A.D., Brown F.M., Jr., Carreira D.S., et al. Arthroscopic anterior shoulder stabilization of collision and contact athletes. Am J Sports Med. 2005;33:52–60. doi: 10.1177/0363546504268037. [DOI] [PubMed] [Google Scholar]
- 3.Wheeler J.H., Ryan J.B., Arciero R.A., Molinari R.N. Arthroscopic versus nonoperative treatment of acute shoulder dislocations in young athletes. Arthroscopy. 1989;5:213–217. doi: 10.1016/0749-8063(89)90174-6. [DOI] [PubMed] [Google Scholar]
- 4.Postacchini F., Gumina S., Cinotti G. Anterior shoulder dislocation in adolescents. J Shoulder Elbow Surg. 2000;9:470–474. doi: 10.1067/mse.2000.108385. [DOI] [PubMed] [Google Scholar]
- 5.Arciero R.A., Wheeler J.H., Ryan J.B., McBride J.T. Arthroscopic Bankart repair versus nonoperative treatment for acute, initial anterior shoulder dislocations. Am J Sports Med. 1994;22:589–594. doi: 10.1177/036354659402200504. [DOI] [PubMed] [Google Scholar]
- 6.De Carli A., Vadala A.P., Lanzetti R., et al. Early surgical treatment of first-time anterior glenohumeral dislocation in a young, active population is superior to conservative management at long-term follow-up. Int Orthop (SICOT) 2019;43:2799–2805. doi: 10.1007/s00264-019-04382-2. [DOI] [PubMed] [Google Scholar]
- 7.Hovelius L., Rahme H. Primary anterior dislocation of the shoulder: Long-term prognosis at the age of 40 years or younger. Knee Surg Sports Traumatol Arthrosc. 2016;24:330–342. doi: 10.1007/s00167-015-3980-2. [DOI] [PubMed] [Google Scholar]
- 8.Randelli P., Ragone V., Carminati S., Cabitza P. Risk factors for recurrence after Bankart repair: A systematic review. Knee Surg Sports Traumatol Arthrosc. 2012;20:2129–2138. doi: 10.1007/s00167-012-2140-1. [DOI] [PubMed] [Google Scholar]
- 9.Robinson C.M., Howes J., Murdoch H., et al. Functional outcome and risk of recurrent instability after primary traumatic anterior shoulder dislocation in young patients. J Bone Joint Surg Am. 2006;88:2326–2336. doi: 10.2106/JBJS.E.01327. [DOI] [PubMed] [Google Scholar]
- 10.Milano G., Grasso A., Russo A., et al. Analysis of risk factors for glenoid bone defect in anterior shoulder instability. Am J Sports Med. 2011;39:1870–1876. doi: 10.1177/0363546511411699. [DOI] [PubMed] [Google Scholar]
- 11.Rugg C.M., Hettrich C.M., Ortiz S., et al. Surgical stabilization for first-time shoulder dislocators: A multicenter analysis. J Shoulder Elbow Surg. 2018;27:674–685. doi: 10.1016/j.jse.2017.10.041. [DOI] [PubMed] [Google Scholar]
- 12.Kasik C.S., Rosen M.R., Saper M.G., Zondervan R.L. High rate of return to sport in adolescent athletes following anterior shoulder stabilisation: A systematic review. J ISAKOS. 2019;4:33–40. doi: 10.1136/jisakos-2018-000224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gaunt B.W., Shaffer M.A., Sauers E.L., et al. The American Society of Shoulder and Elbow Therapists' consensus rehabilitation guideline for arthroscopic anterior capsulolabral repair of the shoulder. J Orthop Sports Phys Ther. 2010;40:155–168. doi: 10.2519/jospt.2010.3186. [DOI] [PubMed] [Google Scholar]
- 14.Moher D., Cook D.J., Eastwood S., et al. Improving the quality of reports of meta-analyses of randomised controlled trials: The QUOROM statement: Quality of Reporting of Meta-analyses. Lancet. 1999;354:1896–1900. doi: 10.1016/s0140-6736(99)04149-5. [DOI] [PubMed] [Google Scholar]
- 15.Slim K., Nini E., Forestier D., et al. Methodological index for non-randomized studies (MINORS): Development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 16.Coleman B.D., Khan K.M., Maffulli N., et al. Victorian Institute of Sport Tendon Study Group. Studies of surgical outcome after patellar tendinopathy: Clinical significance of methodological deficiencies and guidelines for future studies. Scand J Med Sci Sports. 2000;10:2–11. doi: 10.1034/j.1600-0838.2000.010001002.x. [DOI] [PubMed] [Google Scholar]
- 17.Altman D.G., Schulz K.F., Moher D., et al. The revised CONSORT statement for reporting randomized trials: Explanation and elaboration. Ann Intern Med. 2001;134:663–694. doi: 10.7326/0003-4819-134-8-200104170-00012. [DOI] [PubMed] [Google Scholar]
- 18.Dickens J.F., Owens B.D., Cameron K.L., et al. The effect of subcritical bone loss and exposure on recurrent instability after arthroscopic Bankart repair in intercollegiate American football. Am J Sports Med. 2017;45:1769–1775. doi: 10.1177/0363546517704184. [DOI] [PubMed] [Google Scholar]
- 19.DeBerardino T.M., Arciero R.A., Taylor D.C., Uhorchak J.M. Prospective evaluation of arthroscopic stabilization of acute, initial anterior shoulder dislocations in young athletes: Two- to five-year follow-up. Am J Sports Med. 2001;29:586–592. doi: 10.1177/03635465010290051101. [DOI] [PubMed] [Google Scholar]
- 20.Hughes J.L., Bastrom T., Pennock A.T., Edmonds E.W. Arthroscopic Bankart repairs with and without remplissage in recurrent adolescent anterior shoulder instability with Hill-Sachs deformity. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118813981. 2325967118813981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jones K.J., Wiesel B., Ganley T.J., Wells L. Functional outcomes of early arthroscopic Bankart repair in adolescents aged 11 to 18 years. J Pediatr Orthop. 2007;27:209–213. doi: 10.1097/bpo.0b013e31803173d6. [DOI] [PubMed] [Google Scholar]
- 22.Kramer J., Gajudo G., Pandya N.K. Risk of recurrent instability after arthroscopic stabilization for shoulder instability in adolescent patients. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967119868995. 2325967119868995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Owens B.D., Deberardino T.M., Nelson B.J., et al. Long-term follow-up of acute arthroscopic Bankart repair for initial anterior shoulder dislocations in young athletes. Am J Sports Med. 2009;37:669–673. doi: 10.1177/0363546508328416. [DOI] [PubMed] [Google Scholar]
- 24.Ozturk B.Y., Maak T.G., Fabricant P., et al. Return to sports after arthroscopic anterior stabilization in patients aged younger than 25 years. Arthroscopy. 2013;29:1922–1931. doi: 10.1016/j.arthro.2013.09.008. [DOI] [PubMed] [Google Scholar]
- 25.Saper M.G., Milchteim C., Zondervan R.L., et al. Outcomes after arthroscopic Bankart repair in adolescent athletes participating in collision and contact sports. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117697950. 2325967117697950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nixon M.F., Keenan O., Funk L. High recurrence of instability in adolescents playing contact sports after arthroscopic shoulder stabilization. J Pediatr Orthop. 2015;24:173–177. doi: 10.1097/BPB.0000000000000135. [DOI] [PubMed] [Google Scholar]
- 27.Torrance E., Clarke C.J., Monga P., et al. Recurrence after arthroscopic labral repair for traumatic anterior instability in adolescent rugby and contact athletes. Am J Sports Med. 2018;46:2969–2974. doi: 10.1177/0363546518794673. [DOI] [PubMed] [Google Scholar]
- 28.Castagna A., Delle Rose G., Borroni M., et al. Arthroscopic stabilization of the shoulder in adolescent athletes participating in overhead or contact sports. Arthroscopy. 2012;28:309–315. doi: 10.1016/j.arthro.2011.08.302. [DOI] [PubMed] [Google Scholar]
- 29.Chapus V., Rochcongar G., Pineau V., et al. Ten-year follow-up of acute arthroscopic Bankart repair for initial anterior shoulder dislocation in young patients. Orthop Traumatol Surg Res. 2015;101:889–893. doi: 10.1016/j.otsr.2015.09.029. [DOI] [PubMed] [Google Scholar]
- 30.Gigis I., Heikenfeld R., Kapinas A., et al. Arthroscopic versus conservative treatment of first anterior dislocation of the shoulder in adolescents. J Pediatr Orthop. 2014;34:421–425. doi: 10.1097/BPO.0000000000000108. [DOI] [PubMed] [Google Scholar]
- 31.Rahu M., Kartus J.T., Põldoja E., et al. Do articular-sided partial-thickness rotator cuff tears after a first-time traumatic anterior shoulder dislocation in young athletes influence the outcome of surgical stabilization? Orthop J Sports Med. 2018;26 doi: 10.1177/2325967118781311. 2325967118781311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Booth F.W. Physiologic and biochemical effects of immobilization on muscle. Clin Orthop Relat Res. 1987;(219):15–20. [PubMed] [Google Scholar]
- 33.O'Connell P.W., Nuber G.W., Mileski R.A., Lautenschlager E. The contribution of the glenohumeral ligaments to anterior stability of the shoulder joint. Am J Sports Med. 1990;18:579–584. doi: 10.1177/036354659001800604. [DOI] [PubMed] [Google Scholar]
- 34.Kim S.H., Ha K.I., Jung M.W., et al. Accelerated rehabilitation after arthroscopic Bankart repair for selected cases: A prospective randomized clinical study. Arthroscopy. 2003;19:722–731. doi: 10.1016/s0749-8063(03)00397-9. [DOI] [PubMed] [Google Scholar]
- 35.Law B.K.Y., Yung P.S.H., Ho E.P.Y., et al. The surgical outcome of immediate arthroscopic Bankart repair for first-time anterior shoulder dislocation in young active patients. Knee Surg Sports Traumatol Arthrosc. 2008;16:188–193. doi: 10.1007/s00167-007-0453-2. [DOI] [PubMed] [Google Scholar]
- 36.Podlog L., Eklund R.C. Returning to competition after a serious injury: The role of self-determination. J Sports Sci. 2010;28:819–831. doi: 10.1080/02640411003792729. [DOI] [PubMed] [Google Scholar]
- 37.Smith A.M. Psychological impact of injuries in athletes. Sports Med. 1996;22:391–405. doi: 10.2165/00007256-199622060-00006. [DOI] [PubMed] [Google Scholar]
- 38.Tjong V.K., Devitt B.M., Murnaghan M.L., et al. A qualitative investigation of return to sport after arthroscopic Bankart repair: Beyond stability. Am J Sports Med. 2015;43:2005–2011. doi: 10.1177/0363546515590222. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.