Abstract
Purpose
The purpose of this study was to compare alignment measured on standard anteroposterior (AP) radiographs versus full-length weight-bearing radiographs.
Methods
Patients were prospectively enrolled from June 2019 to August 2019 from a single orthopedic surgeon’s practice if they were ≥ 18 years of age, obtained both AP and full-length alignment radiographs and were capable of full weight-bearing with appropriate positioning. Patients were excluded if they were < 18 years of age, had previous knee arthroplasty, previous knee or hip osteotomy, were unable to bear full weight on both limbs, and if the patient’s body habitus precluded appropriate visualization of necessary landmarks on the radiographs. Tibiofemoral angles were measured on AP radiographs using 2 techniques (AP angles 1 and 2). Linear regression and paired t tests were used to compare measurements. The minimal clinically important difference was defined as < 2°.
Results
There were 120 patients (62 males, 58 females) with an average age of 45 ± 17 years who were enrolled. There were positive correlations between average alignment on full-length weight-bearing and AP radiographs for AP angle 1 (r = 0.72) and AP angle 2 (r = 0.76) measurement techniques (P < .001). There was a significant difference in mean alignment between full-length weight-bearing and AP measurements (AP angle 1: 2.5° difference; AP angle 2: 4.4° difference; P < .001). Frequency distributions for the minimal clinically important difference between true mechanical alignment and AP views demonstrated that 46.7% of patients had ≥ 2° difference for AP angle 1, and 78.3% of patients had ≥ 2° difference for AP angle 2.
Conclusion
The average absolute difference in alignment measured between standard AP radiograph and full-length weight-bearing radiograph views was significant, with 46.7% to 78.3% of patients having a greater than 2° absolute difference between these 2 views. In cases where precise objective alignment measurement is necessary, full-length weight-bearing radiographs are recommended over standard AP radiographs for presurgical planning so as to reduce potential error in over- or underestimation of the true mechanical alignment.
Study Design
Prospective case-comparison; Level of evidence, 1.
Proper assessment of limb alignment has important implications for the treatment of many orthopedic pathologies. Treatments that are dependent on limb alignment include knee arthroplasty,1 use of unloader bracing,2 ligament repair and reconstruction,3 meniscal repairs,4 cartilage procedures,5 and knee osteotomy procedures.6 In particular, surgeries that aim to change knee alignment, such as proximal tibial osteotomy6,7 and distal femoral osteotomy,8 rely on a precise assessment of limb alignment, not only for preoperative planning but also as a postoperative measurement tool to determine whether the alignment-correction procedure was successful.1,7
Several methods for measurement of limb alignment in the coronal plane have been described in the literature. Standard anteroposterior (AP) weight-bearing knee and the anteroposterior full-length weight-bearing views are the most common radiographs used for these measurements. Furthermore, multiple AP radiographic measurements have been described as potential techniques to predict the true mechanical axis, without the potential downsides of obtaining full-length weight-bearing radiographs, which include risk of added radiation exposure, additional technical training for technicians, increased time required to obtain the images, and overall greater cost.9, 10, 11, 12, 13 Two of these methods (referred to in the present study as AP angle 1 and AP angle 2) aim to use the center point of the tibial and femoral diaphyses to predict anatomic alignment at the knee, without the need to visualize the hip or ankle joints.9,11 Given the potential mechanical axis deviation from the femoral diaphysis proximally and the potential deviation from the tibial diaphysis distally, both of which are not seen on standard AP radiographs, it is acknowledged by many that AP radiograph measurements (with or without corrective algorithms) are not satisfactory proxies for mechanical alignment measured on full-length weight-bearing radiographs.9 As such, the current literature contains contradictory findings regarding the accuracy of measurements taken from standard AP radiographs when compared to those taken on full-length weight-bearing radiographs.9, 10, 11,14,15 Therefore, the purpose of this study was to compare limb alignment measured on standard AP radiographs versus full-length weight-bearing radiographs. The null hypothesis was that there would be no difference in average limb alignment as measured on AP radiographs versus full-length weight-bearing radiographs.
Methods
Study Design
Prior to patient enrollment, the study protocol was approved by an external institutional review board (IntegReview #072419). Patients were prospectively enrolled from June 2019 to August 2019 from a single orthopedic surgeon’s practice (R.F.L.). Inclusion criteria included patients who were ≥ 18 years of age, obtained both AP and full-length alignment radiographs at their initial or preoperative appointments and were capable of full weight bearing with the knees fully extended and weight equally distributed between both limbs. Patients were excluded if they were < 18 years of age, had undergone previous knee arthroplasty or previous knee or hip osteotomy, were unable to bear full weight on both limbs, or if the patient body habitus precluded appropriate visualization of necessary landmarks on the radiographs. Overall lower-limb alignment was calculated via patient’s mechanical axis on full-length weight-bearing radiographs, which is considered the gold standard for true limb alignment.16 All radiograph measurement techniques were then completed by 2 independent raters (N.R.G., R.S.D.) on each standard AP radiograph.9,11
Radiographic Evaluation
Full-length weight-bearing radiographs were obtained using 3 to 4 individual images on a 43.2 cm x 43.2 cm vertical digital detector. The radiograph beam was centered at the knee at a distance of 182.9 cm. The beam was angled independently for each shot from the hip to the ankle, with distortion corrected by processing algorithms.
The standard AP radiographs were obtained on a 43.2 cm x 43.2 cm cassette at the midcoronal plane of the knee. The radiograph beam was centered at the knee at a distance of 110 cm, with the patients having the posterior aspect of their knees in contact with the vertical cassette. The beam was parallel to the floor, and the machine's settings were 80 kVp at 3.2-8 mAs, based on patient size. All subjects were asked to stand without footwear, and the tibial tubercles faced forward. Both limbs were radiographed simultaneously, with weight equally balanced between both limbs, and the knees were fully extended.
Measurement Techniques
On full-length alignment radiographs, alignment was measured using the hip-knee-ankle angle described by Moreland et al.16 Using digital radiograph imaging software (IMPAX, Agfa Healthcare, Mortsel, Belgium), a line was created that passed from the center of the femoral head through the midpoint of the weight-bearing surface of the tibial plateau. A second line was created that passed from the midpoint of the weight-bearing surface of the tibia through the center of the tibiotalar joint. The angle of intersection between these 2 lines at the knee was recorded as the hip-knee-ankle angle.16
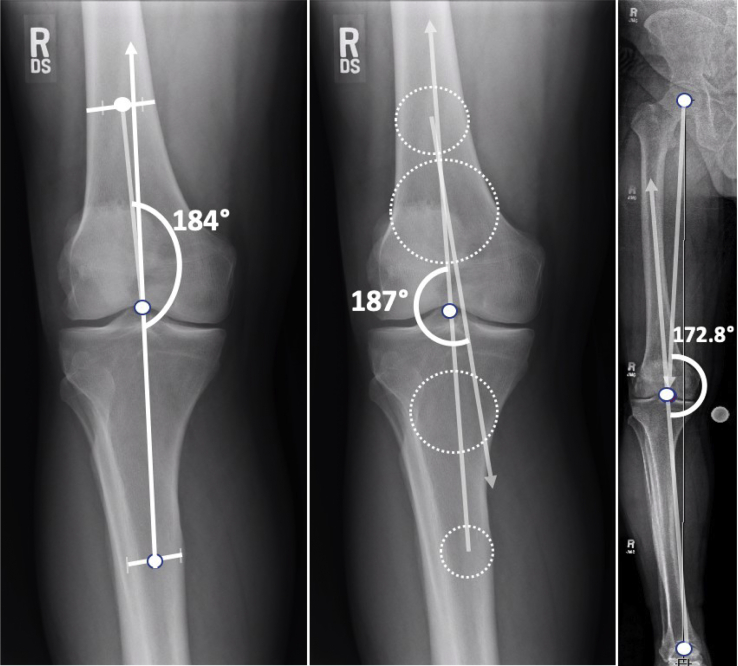
On standard AP radiographs, 2 different measurements were used to calculate the tibiofemoral angle at the knee, both of which have been frequently implemented in other studies and have been described as proxies for mechanical alignment on full-length weight-bearing films.9,10,11,14,15,17, 18, 19, 20, 21, 22 The first tibiofemoral angle measurement technique (AP angle 1) used the midpoint of the weight-bearing surface of the tibia as the apex and 2 points located midway between medial and lateral cortices, a femoral diaphyseal point 10 cm above the tibial eminences and a tibial diaphyseal point 10 cm below the tibial eminences.11 The angle at the joint was recorded as AP angle 1. The second tibiofemoral angle measurement technique (AP angle 2) used 2 pairs of circles set between the medial and lateral cortices of both the femur and the tibia, centered at 5 cm and 10 cm from the joint line. A line passing through the center point of both femoral circles was extended through the joint, intersecting a second line passing through the center point of both tibial circles.9 The angle created at this intersection was recorded as AP angle 2. Angles were recorded in degrees with respect to neutral alignment at 180°. Angles measuring < 180° represented varus alignment and angles measuring > 180° represented valgus alignment (Fig 1).
Fig 1.
Limb alignment measured on standard AP compared to full-length weight-bearing radiographs. Assessment using the tibiofemoral angle 1 (AP angle 1) technique (left) demonstrates limb alignment of 184° (4° valgus); the AP angle 2 technique (middle) demonstrates limb alignment of 187° (7 ° valgus); the mechanical axis on full-length weight-bearing radiograph (right) demonstrates alignment of 172.8° (7.2° varus). Compared to the full-length weight-bearing view, the AP angle 1 an AP angle 2 techniques demonstrate a discrepancy of 11.2° and 14.2°, respectively.
Statistical Analyses
Descriptive statistics were reported for all included patients. Inter- and intrarater agreement was assessed for radiographic measurements with a 2-way random effects model to calculate the intraclass correlation coefficient (ICC). The ICC values were interpreted as follows: ICC < 0.40, poor agreement; 0.4 < ICC < 0.75, fair to good agreement; ICC > 0.75, excellent agreement.23,24 Based on previous data reported by Bito et al., the minimal clinically important difference (MCID) was defined as < 2°, which represents the difference between full-length weight-bearing and standard AP measurement techniques that is not clinically significant.25 As a result, frequency distributions were calculated for subanalysis of the MCID for limb alignment measurements on AP weightbearing views ≥ 2°.
Sample size was determined via an a priori power analysis. The standard deviation of limb alignment was taken from Zampogna et al.,9 who reported a mean difference of 2.85° for full-length weight-bearing mechanical axis compared to standard AP views. Using this standard deviation and based on the assumption of 2-tailed testing with an alpha level of 0.05, 120 patients were a sufficient number to achieve at least 80% statistical power. Linear regression was used to assess the correlation between the full-length weight-bearing mechanical axis and standard AP measurement techniques (AP angle 1 and AP angle 2). Additionally, a paired t test was used to compare the mean difference between measurements taken on full-length weight-bearing and AP angle 1 and AP angle 2 from standard AP radiographs. All data were analyzed by SPSS Statistics (version 22, IBM, Armonk, NY, U.S.A.), with an alpha level set at P < .05 for statistical significance.
Results
There were 120 patients (62 males, 58 females) with an average age of 45 ± 17 years who met the inclusion criteria during the prospective enrollment period. Inter-rater reliabilities for radiograph measurements of mechanical axis on full-length weight-bearing radiographs, AP angle 1 and AP angle 2 were 0.99, 0.91 and 0.88, respectively, which is considered excellent reliability.23,24 Intrarater reliabilities were also considered excellent for radiographic measurements on full-length weight-bearing, AP angle 1 and AP angle 2 views, which were 0.99, 0.98 and 0.95, respectively. The average limb alignment for all patients according to full-length weight-bearing mechanical axis measurement was 178.2° ± 3.8°. When evaluating overall lower limb alignment across the 3 measurement techniques, the average alignment was genu varum (< 180°) according to full-length weight-bearing measurement technique, whereas the same patients displayed genu valgum (> 180°) alignment when using AP angle 2 as a proxy (Table 1).
Table 1.
Patient Demographics and Average Limb Alignment Values According to Full-Length Weight-Bearing and Anteroposterior Weight-Bearing Knee Radiographs
| Demographic | Mean ± SD |
|---|---|
| Age, years | 45 ± 17 |
| Body mass index, kg/m2 | 26.5 ± 5.1 |
| Gender | 62M, 58F |
| Radiograph technique | |
| Full-length weight-bearing, mechanical axis | 178.2 ± 3.8 |
| AP angle 1 | 180.0 ± 3.6 |
| AP angle 2 | 182.6 ± 4.0 |
NOTE. N = 120. Angles were recorded in degrees with respect to neutral alignment at 180°. AP angle 1 and AP angle 2 were the two tibiofemoral angle measurement techniques used on standard AP radiographs.
AP, anteroposterior; F, females; M, males.
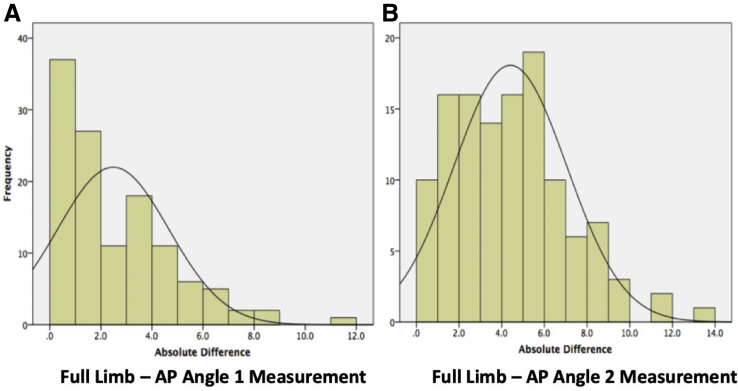
There were significant positive correlations between the average full-length weight-bearing alignment and average AP alignment for the AP angle 1 (r = 0.72) and AP angle 2 (r = 0.76) measurement techniques (P < .001) (Fig 2). When evaluating the mean differences in limb alignment between the full-length weight-bearing and standard AP views, there was a significant difference of 2.5° for limb alignment angle for the AP angle 1 view and a significant difference of 4.4° for limb alignment angle for the AP angle 2 view (P < .001). This indicates that the AP angle 1 measurement technique was more accurate than the AP angle 2. When evaluating frequency distributions for the MCID in limb alignment between full-length weight-bearing and standard AP views, 46.7% (n = 45) of patients had ≥ 2° difference (range, 3˚-12°) from true mechanical alignment for AP angle 1 measurements and 78.3% (n = 78) of patients had ≥ 2° difference (range, 3˚-14°) from true mechanical alignment for AP angle 2 measurements (Table 2) (Fig 2).
Fig 2.
Frequency distributions of differences between full-length weight-bearing (FLWB) and anteroposterior weightbearing (AP) knee radiographs (N = 120). (A) Absolute differences in mechanical alignment between FLWB and tibiofemoral angle measurement 1 (AP angle 1). (B) Absolute differences between FLWB compared to tibiofemoral angle measurement 2 (AP angle 2).
Table 2.
Frequencies of Absolute Differences in Limb Alignment Between Full-Length Weight-Bearing and Anteroposterior Weight-Bearing Knee Radiographs
| Alignment Difference | AP angle 1 N (%) |
AP angle 2 N (%) |
|---|---|---|
| < 1° | 37 (31%) | 10 (8%) |
| 1 ≤ n < 2 | 27 (23%) | 16 (13%) |
| 2 ≤ n < 3 | 11 (9%) | 16 (13%) |
| 3 ≤ n < 4 | 18 (15%) | 14 (12%) |
| 4 ≤ n < 5 | 11 (9%) | 16 (13%) |
| 5 ≤ n < 6 | 6 (5%) | 19 (16%) |
| 6 ≤ n < 7 | 5 (4%) | 10 (8%) |
| 7 ≤ n < 8 | 2 (2%) | 6 (5%) |
| 8 ≤ n < 9 | 2 (2%) | 7 (6%) |
| 9 ≤ n <1 0 | 0 (0%) | 3 (3%) |
| ≥ 10° | 1 (1%) | 3 (3%) |
NOTE. N = 120. AP angle 1 and AP angle 2 are tibiofemoral angle-measurement techniques 1 (lines) and 2 (circles). AP, anteroposterior.
Discussion
The most important finding of this study was that there was a significant difference between the average measurement of lower limb alignment on standard AP and full-length weight-bearing radiographs, with 46.7%-78.3% of standard AP measurements falling outside the MCID of 2° when compared to full-length measurements. Although both measurement techniques on standard AP radiographs were positively correlated with full-length weight-bearing radiographs (AP angle 1 explained 72% of variance, and AP angle 2 explained 76% of variance), they both also had a significant mean difference from full-length weight-bearing measurements (2.5° for AP angle 1 and 4.4° for AP angle 2; P < .001). Therefore, when evaluating a patient’s limb alignment prior to potential surgical intervention, it is recommended that full-length weight-bearing radiographs be obtained to allow for increased accuracy in determining true limb alignment.
The results of the current study indicate a high correlation between standard AP views and full-length limb alignment views (r = 0.72 and r = 0.76); however, there was a significant difference between AP and full-length views (P < .05), indicating the potential for inaccuracies when using standard AP radiographs to predict true limb alignment. Furthermore, 46.7% of AP angle 1 measurements and 78.3% of AP angle 2 measurements were ≥ 2° different from the full-length weight-bearing radiograph measurements, with measurements deviating by as much as 12°. Because of these findings, clinicians ought to avoid calculating limb alignment on AP radiographs in cases where precise alignment measurement is necessary, and instead use the gold standard full-length weight-bearing radiographs. These conclusions are different from those reported by Colebatch et al.,10 who reported that there was no significant difference in means between measurements taken on full-length weight-bearing and standard AP radiographs. The difference in findings may be related to the smaller sample size of 40 patients or to the small number of patients included with alignment > 2° from neutral on full-length weight-bearing radiographs.
The AP angle 1 technique is the most common AP measurement technique used in the clinical setting, and in the current study it demonstrated increased accuracy in predicting true alignment compared to the AP angle 2 measurement technique. In contrast, Zampogna et al. concluded that the AP angle 2 was a more accurate predictor of true alignment.9 This difference may be related to the previous study’s inclusion exclusively of knees with varus malalignment, whereas the current study included consecutive patients, regardless of alignment. Additionally, the aforementioned study included only 36 patients, which may be underpowered compared to the current study’s enrollment of 120 patients.
It is a common clinical trend to use the standard AP radiograph to assess lower-limb alignment.17,26,27 One recent study reported a lower risk of progression of osteoarthritis following meniscal root tears treated with meniscectomy in the setting of neutral limb alignment.28 Based on the standard AP radiographic views used for assessing alignment in the aforementioned study, 1 of the major critiques of their analysis was that the assessment of limb alignment was potentially inaccurate.28,29 Some may advocate for the addition of 5°-7° of varus angulation to anatomic alignment assessed on AP radiographs to account for offset at the hip in order to more closely reflect full-length weight-bearing measurements. However, the range of difference between full-length weight-bearing and AP measurements in the present study informs us that this method in many patients would add either too much varus angulation or insufficient varus angulation to a patient’s true mechanical alignment. A recent study evaluated 1,480 consecutive patients with hip-knee-shaft angles ranging from 2.5°-9°, confirming the insufficiency of the aforementioned correction to AP measurements in many cases.30 Thus, despite the high correlation between AP and full-length radiographs, there is great potential for misinterpretation of true mechanical alignment when using measurements on standard AP radiographs as proxies.
In the case of an osteotomy, it is critical to plan and implement the appropriate degree of alignment correction. Coronal plane measurements calculated on plain radiographs preoperatively must, therefore, be sufficiently accurate in order to achieve the target weight-bearing axis line. Given the significant average difference in alignment measured on standard AP views compared to full-length weight-bearing radiographs consistent with previous studies9,17 and the proportion of measurements found on AP views to be ≥ 2° from true limb alignment, it is recommended that surgeons obtain full-length weight-bearing radiographs to evaluate appropriate candidacy for an osteotomy procedure and for accurate preoperative planning. In addition to perioperative measurements, accurate assessment of knee alignment can have prognostic value. Recent literature has demonstrated that varus knee malalignment identified on full-length weight-bearing radiographs is significantly related to factors associated with worse outcomes, including medial meniscal extrusion and accelerated progression of osteoarthritis following meniscal root tears.31, 32, 33, 34 Furthermore, there is increased risk of progression of lateral compartment osteoarthritis in the setting of valgus knee malalignment.35 Based on the differences in measurements found when using AP versus full-length weight-bearing views, it is recommended that caution be exercised when attempting to use standard AP radiographs to extrapolate a prognosis for pathologies dependent on knee alignment, such as a known meniscal root tear or early osteoarthritis.
Limitations
There were limitations to the current study. The hip-knee-shaft angle was not included, which accounts for offset at the hip; however, the difference in alignment due to offset at the hip is addressed when evaluating the difference between alignment on AP radiographs and the hip-knee-ankle angle on full-length weight-bearing radiographs. Furthermore, the sample population was from a single surgeon’s practice using the same radiographic protocol, which may limit the external validity of the results. However, this allowed for better comparisons in a homogeneous sample and for increased accuracy of obtaining true AP and full-length weight-bearing views. Additionally, the equipment used for obtaining full-length weight-bearing radiographs requires an expensive machine with automated features that reduce the time required to obtain a full-length image, and this may, therefore, limit the generalizability to smaller institutions with more limited resources.
Conclusion
The average absolute difference in alignment measured between standard AP radiographs and full-length weight-bearing radiograph views was significant, with 46.7%-78.3% of patients having a greater than 2° absolute difference between these 2 views. In cases where precise objective alignment measurement is necessary, full-length weight-bearing radiographs are recommended over standard AP radiographs for presurgical planning so as to reduce potential error in over- or underestimation of the true mechanical alignment.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: R.F.L reports grants and personal fees from Arthrex, Ossur and Smith & Nephew and grants from Linvatec outside the submitted work; is on the editorial or governing board of American Journal of Sports Medicine and Knee Surgery, Sports Traumatology, Arthroscopy, and Journal of Experimental Orthopaedics; is a board or committee member of the American Orthopaedic Society for Sports Medicine and the International Society of Arthroscopy, Knee Surgery, Orthopaedic Sports Medicine. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Kumar N., Yadav C., Raj R., Anand S. How to interpret postoperative x-rays after total knee arthroplasty. Orthop Surg. 2014;6:179–186. doi: 10.1111/os.12123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hart H.F., Collins N.J., Ackland D.C., et al. Immediate effects of a brace on gait biomechanics for predominant lateral knee osteoarthritis and valgus malalignment after anterior cruciate ligament reconstruction. Am J Sports Med. 2015;44:865–873. doi: 10.1177/0363546515624677. [DOI] [PubMed] [Google Scholar]
- 3.Kane P.W., Cinque M.E., Moatshe G., et al. Fibular collateral ligament: Varus stress radiographic analysis using 3 different clinical techniques. Orthop J Sport Med. 2018;6:1–6. doi: 10.1177/2325967118770170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jiang E.X., Abouljoud M.M., Everhart J.S., et al. Clinical factors associated with successful meniscal root repairs: A systematic review. Knee. 2019;26:285–291. doi: 10.1016/j.knee.2019.01.005. [DOI] [PubMed] [Google Scholar]
- 5.Dean C.S., Chahla J., Serra Cruz R., LaPrade R.F. Fresh osteochondral allograft transplantation for treatment of articular cartilage defects of the knee. Arthrosc Tech. 2016;5:e157–e161. doi: 10.1016/j.eats.2015.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chahla J., Dean C.S., Mitchell J.J., et al. Medial opening wedge proximal tibial osteotomy. Arthrosc Tech. 2016;5:e919–e928. doi: 10.1016/j.eats.2016.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dean C.S., Chahla J., Moulton S.G., et al. Anterolateral biplanar proximal tibial opening-wedge osteotomy. Arthrosc Tech. 2016;5:e531–e540. doi: 10.1016/j.eats.2016.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mitchell J.J., Dean C.S., Chahla J., et al. Varus-producing lateral distal femoral opening-wedge osteotomy. Arthrosc Tech. 2016;5:e799–e807. doi: 10.1016/j.eats.2016.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zampogna B., Vasta S., Amendola A., et al. Assessing lower limb alignment: Comparison of standard knee X-ray vs long leg view. Iowa Orthop J. 2015;35:49–54. [PMC free article] [PubMed] [Google Scholar]
- 10.Colebatch A.N., Hart D.J., Zhai G., et al. Effective measurement of knee alignment using AP knee radiographs. Knee. 2009;16:42–45. doi: 10.1016/j.knee.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 11.Hinman R.S., May R.L., Crossley K.M. Is there an alternative to the full-leg radiograph for determining knee joint alignment in osteoarthritis? Arthritis Care Res. 2006;55:306–313. doi: 10.1002/art.21836. [DOI] [PubMed] [Google Scholar]
- 12.Hart D., Wall B. NRPB W-Series Rep; 2002. Radiation exposure of the UK population from medical and dental X-ray examinations.http://www.hpa.org.uk/web/HPAweb&HPAwebStandard/HPAweb_C/1247816602523 March:41. [Google Scholar]
- 13.Brouwer R.W., Jakma T.S.C., Bierma-Zeinstra S.M.A., et al. The whole leg radiograph: Standing versus supine for determining axial alignment. Acta Orthop Scand. 2003;74:565–568. doi: 10.1080/00016470310017965. [DOI] [PubMed] [Google Scholar]
- 14.Sheehy L., Felson D., Zhang Y., et al. Does measurment of the anatomic axis consistently predict hip-knee-ankle angle for knee alignment studies in osteoarthritis? Osteoarthr Cartil. 2012;19:58–64. doi: 10.1016/j.joca.2010.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Felson D., Cooke D., Niu J., et al. Can anatomic alignment measured from a knee radiograph subsititute for mechanical alignment from full limb films? Osteoarthr Cartil. 2009;23:1448–1452. doi: 10.1016/j.joca.2009.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moreland J.R., Bassett L.W., Hanker G.J. Radiographic axial analysis of the lower of the extremity. J Bone Jt Surg. 2009;69:745–749. [PubMed] [Google Scholar]
- 17.van Raaij T.M., Brouwer R.W., Reijman M., et al. Conventional knee films hamper accurate knee alignment determination in patients with varus osteoarthritis of the knee. Knee. 2009;16:109–111. doi: 10.1016/j.knee.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 18.Chang C.B., Choi J.Y., Koh I.J., et al. What should be considered in using standard knee radiographs to estimate mechanical alignment of the knee? Osteoarthr Cartil. 2010;18:530–538. doi: 10.1016/j.joca.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 19.Kraus V.B., Vail T.P., Worrell T., McDaniel G. A comparative assessment of alignment angle of the knee by radiographic and physical examination methods. Arthritis Rheum. 2005;52:1730–1735. doi: 10.1002/art.21100. [DOI] [PubMed] [Google Scholar]
- 20.Navali A.M., Bahari L.A.S., Nazari B. A comparative assessment of alternatives to the full-leg radiograph for determining knee joint alignment. Sport Med Arthrosc Rehabil Ther Technol. 2012;4:1. doi: 10.1186/1758-2555-4-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Issa S.N., Dunlop D., Chang A., et al. Full-limb and knee radiography assessments of varus-valgus alignment and their relationship to osteoarthritis disease features by magnetic resonance imaging. Arthritis Care Res. 2007;57:398–406. doi: 10.1002/art.22618. [DOI] [PubMed] [Google Scholar]
- 22.Clement N.D., MacDonald D., Burgess A.G., Howie C.R. Articular surface mounted navigated total knee arthroplasty improves the reliability of component alignment. Knee Surg Sport Traumatol Arthrosc. 2018;26:1471–1477. doi: 10.1007/s00167-017-4433-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fleiss J.L., Chilton N.W., Park M.H. Inter- and intra-examiner variability in scoring supragingival plaque: II. Statistical analysis. Pharmacol Ther Dent. 1980;5:5–9. [PubMed] [Google Scholar]
- 24.Cicchetti D.V. Guidelines , criteria , and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1993;6:284–290. [Google Scholar]
- 25.Bito H., Takeuchi R., Kumagai K., et al. A predictive factor for acquiring an ideal lower limb realignment after opening-wedge high tibial osteotomy. Knee Surgery, Sport Traumatol Arthrosc. 2009;17:382–389. doi: 10.1007/s00167-008-0706-8. [DOI] [PubMed] [Google Scholar]
- 26.Schiraldi M., Bonzanini G., Chirillo D., de Tullio V. Mechanical and kinematic alignment in total knee arthroplasty. Ann Transl Med. 2016;4:1–5. doi: 10.21037/atm.2016.03.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hall M., Bennell K.L., Beavers D.P., et al. Does frontal knee kinematics predict treatment outcomes? Exploratory analyses from the Intensive Diet and Exercise for Arthritis (IDEA) trial. Gait Posture. 2018;63:139–144. doi: 10.1016/j.gaitpost.2018.04.045. [DOI] [PubMed] [Google Scholar]
- 28.Lee B.S., Bin S Il, Kim J.M., et al. Partial meniscectomy for degenerative medial meniscal root tears shows favorable outcomes in well-aligned, nonarthritic knees. Am J Sports Med. 2019;47:606–611. doi: 10.1177/0363546518819225. [DOI] [PubMed] [Google Scholar]
- 29.Chahla J., LaPrade R.F., Krych A.J., et al. Partial meniscectomy for degenerative medial meniscal root tears shows favorable outcomes in well-aligned, nonarthritic knees. Am J Sports Med. 2019;47:606–611. doi: 10.1177/0363546518819225. [DOI] [PubMed] [Google Scholar]
- 30.Lampart M., Behrend H., Moser L.B., Hirschmann M.T. Due to great variability fixed HKS angle for alignment of the distal cut leads to a significant error in coronal TKA orientation. Knee Surg Sport Traumatol Arthrosc. 2019;27:1434–1441. doi: 10.1007/s00167-018-5041-0. [DOI] [PubMed] [Google Scholar]
- 31.Goto N., Okazaki K., Akiyama T., et al. Alignment factors affecting the medial meniscus extrusion increases the risk of osteoarthritis development. Knee Surgery, Sport Traumatol Arthrosc. 2019;27:2617–2623. doi: 10.1007/s00167-018-5286-7. [DOI] [PubMed] [Google Scholar]
- 32.Crema M.D., Roemer F.W., Felson D.T., et al. Factors associated with meniscal extrusion in knees with or at risk for osteoarthritis: The Multicenter Osteoarthritis study. Radiology. 2012;264:494–503. doi: 10.1148/radiol.12110986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Antony B., Driban J.B., Price L.L., et al. The relationship between meniscal pathology and osteoarthritis depends on the type of meniscal damage visible on magnetic resonance images: Data from the Osteoarthritis Initiative. Osteoarthr Cartil. 2017;25:76–84. doi: 10.1016/j.joca.2016.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Teichtahl A.J., Cicuttini F.M., Abram F., et al. Meniscal extrusion and bone marrow lesions are associated with incident and progressive knee osteoarthritis. Osteoarthr Cartil. 2017;25:1076–1083. doi: 10.1016/j.joca.2017.02.792. [DOI] [PubMed] [Google Scholar]
- 35.Chahla J., Mitchell J.J., Liechti D.J., et al. Opening- and closing-wedge distal femoral osteotomy: A systematic review of outcomes for isolated lateral compartment osteoarthritis. Orthop J Sport Med. 2016;4:1–8. doi: 10.1177/2325967116649901. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.