Abstract
Objectives
The study aimed at identifying the commonly used non-prescribed antibiotics (NPAs) and the main health conditions leading to the practices of self-medication with antibiotics (SMAs) in Maputo city, Mozambique.
Design
Cross-sectional qualitative study based on individual and group interviews.
Setting
The study was conducted in nine pharmacies of three socioeconomic areas of Maputo city, from October 2018 to March 2019.
Participants
The study included 32 pharmacy clients and 17 pharmacists. The pharmacy clients included men 10 (31%) and women 22 (69%) ranging from 19 to 67 years while the pharmacists included men 6 (35,3%) and women 11 (64,7%) with ages ranging from 24 to 47 years.
Findings
The majority of the pharmacy clients 30 (93.75%) admitted frequent use of NPAs, 15 (88.2%) out of the 17 pharmacists admitted dispensing NPAs. While the majority of the participants (16) mentioned the use of amoxicillin, also known as ‘two colours medicine’, 14 mentioned the use of cotrimoxazole and seven mentioned amoxicillin with clavulanic acid. Two to five participants also used tetracycline, ciprofloxacin, azithromycin, doxycycline, erythromycin, metronidazole and phenoxymethylpenicillin. The above mentioned NPAs were used to treat self-perceived sore throat, fever, pain, cough, vaginal discharge, eye problems, the common influenza, urinary infections, respiratory tract infections, wounds and toothaches.
Conclusions
Antibiotics are perceived as essential medical resources to manage health and illnesses. While taking an active role in their health-disease process, participants commonly used amoxicillin, ‘two colours’, cotrimoxazole and amoxicillin with clavulanic acid to manage their health and that of their families. In this sense, the practices of SMAs were perceived as part of the self-care process and not necessarily as misuse of antibiotics. A wideunderstanding of health-seeking beliefs and behaviours regarding the utilisation of antibiotics is needed to inform public health experts, health policymakers and other stake-holders in designing and implementing public health education and health promotion programsat all levels in Mozambique.
Keywords: public health, qualitative research, health & safety, substance misuse, anthropology, pharmacology
Strengths and limitations of this study.
The first study reporting the commonly used non-prescribed antibiotics in Mozambique.
Enlarged views, narratives and perspectives from pharmacy clients requesting and pharmacists dispensing non-prescribed antibiotics.
Recruiting outside the pharmacies after the immediate purchase of non-prescribed antibiotics meant selection bias was reduced.
The qualitative approach provided an in-depth view of the phenomenon of the utilisation of non-prescribed antibiotics and self-medication with antibiotics as prescription-only medicines.
The focus group discussions were limited to the pharmacy clients, focus group discussion with pharmacists would have given a group perspective from the dispensers’ point of view.
Introduction
Medicines are considered the core of the illness treatment and care process for both health professionals and patients. As suggested by Geest and Whyte, medicines are ‘things’ with ‘charm’ in every part of the world and culture.1 As medicines and ‘things’, since their discovery, antibiotics are one of the most successful medical resources significantly contributing to the control of infectious diseases causing human morbidity and mortality.2
The clinical and social value of antibiotics for the health system responses to illness and the associated increase in life expectancy suggests why antibiotics are one of the most commercialised, prescribed and used drugs in the world.3–7 However, the excessive and inappropriate use of antibiotics is considered a public health concern due to its association with the problem of antibiotic resistance (AR), a fraction of a major global threat—antimicrobial resistance (AMR). AR is rising to dangerously high levels in all parts of the world.
While global trends on antibiotic use estimate that antibiotics are overused in all regions,8 the excwssive use of antibiotics in agriculture, veterinary and human health is driving the development and spread of AMR globally. This accounts for more than two million infections and at least 23 000 deaths annually in the USA9 and 25 000 deaths in Europe.10 11 It is estimated that by 2050 about 10 million people will die due to AMR complications. The low-income and middle-income countries (LMICs) are more affected due to insufficient infection prevention control measures and the increased burden of infectious diseases.3 12 13
While selfmedication is considered a component of self-care, self medication with antibiotics (SMASs) potentially jeopardises patients’ health contributing to AR (cited reference 3, 14). On the one hand, individuals’ practices of self-medication undermine global efforts to reduce antibiotic consumption, rationalise their use and contain AR. 3 14 On the other hand, the non-prescription sale of antibiotics has increased, especially within LMICs, where control and law enforcement capabilities are limited, faulty or non-existent. For instance, 23% of the increase in the global retail sales volume of antibiotics was attributed to India, where regulations to control over-the-counter sales of antibiotics are poorly enforced.9 In sub-Saharan Africa, the proliferation of pharmacies and the non-prescription sales of antibiotics have been reported in countries such as the Democratic Republic of Congo, Malawi, Mozambique, Namibia, Tanzania and Zambia.15–17
Mozambique is producing increasingly more research on the utilisation of antibiotics at both, hopsital level by health care workers and at individuals and community level. Evidence from a sociologic approach to understand the practice of SMAs among community members showed how the practices of SMAsare common and recurrent, being part of everyday practical reasoning, and, perceived as one of the readily available therapeutic options for self-care.18 Another research reported poor knowledge about antibiotics showed that non-prescribed antibiotics (NPAs) were purchased from pharmacies, despite this being legally prohibited.17
This study is part of a broader research project using the same qualitative methodology to explore the practices of SMAs in Maputo city. Our previous articles regarding the patterns of SMAs, the factors influencing and the pharmacist’s dispensing practices in Maputo city. These articles evidence the different ways in which the public access NPAs, the factorts influencing these practices, and, also the dispensing practices of pharmacists.16 19(please add reference: “Antibiotics heal all diseases”; factors influencing the pratices of self-medication with antibiotics in Maputo City, MozambiqueDOI : 10.1007/s10389-020-01416-7JOPH-D-20-00960R1) As a follow-up, in this article, we report the commonly used NPA and the main health conditions leading to the practices of SMA.
Despite the increasing evidence confirming the utilisation of NPAs in Mozambique, there is still little20 evidence regarding which antibiotics are commonly used. Therefore, identifying the frequently used NPAs seems relevant to enrich the understanding of the practices of SMAs in Mozambique and expand the existing evidence base. Such evidence will inform local policy-makers, healthcare providers and health promoters and provide the foundation for locally tailored interventions to promote the rational use of antibiotics at health care system, individual and community levels.
Research question
What are the commonly used NPAs and the main health conditions leading to the practices of SMAs among pharmacy clients in Maputo city?
Objective
This study aimed at identifying the commonly used NPAs and the main health conditions leading to the practice of SMAs in Maputo city.
Methods
This study is part of a larger research project aimed at exploring the practices of SMAs and the NPA dispensing practices in Maputo city, Mozambique. The same methodology was applied to collect and analyse data from the same participants to inform and respond to the four main objectives of the research namely: the patterns and factors of SMAs, the pharmacists’ practices of non-prescribed antibiotic dispensing and the commonly used NPAs. The results are presented according to four objectives of the primary research, in this article we address the fourth and final objective of the comprehensive study.
Study design, setting and participants
This study is a cross-sectional qualitative study based on in-depth interviews and focus group discussions (FGD) facilitated by the first author. Participants were recruited from three socioeconomic areas (high, middle and low) of the KaMphumo Municipality district within Maputo city according to the National Institute of Statistics of Mozambique.21 The data gathering occurred from October 2018 to March 2019 in nine private pharmacies from three economic areas.
Only private pharmacies were included as the public pharmacies are run by state-related organisations that strictly enforce the prescription-only dispensing of antibiotics. The private pharmacies in Maputo city are owned by individuals who are licensed to dispense and whose pharmacies are registered within the Ministry of Health (MoH). Despite the legislation governing prescription-only medicines (POMs), publicly known enforcement and accountability mechanisms regarding the pharmacies’'s activities, including the dispensing of medicines are scarce to non-existent.
The study participants included the pharmacy clients and the pharmacists. The pharmacists consisted in all professionally trained persons holding either a college degree and or a first degree in pharmaceutical sciences working in the pharmacies. All participants resided in Maputo city and were Portuguese speaking, the official language of Mozambique. While the inclusion of pharmacy clients was motivated by the need to describe the practices of SMA and identify commonly used antibiotics, the inclusion of pharmacists was considered to enrich the data by capturing the perspectives of the dispensers.
Sampling and recruitment strategies
Pharmacies
According to the National Direction of Pharmacy at the MoH, as of September 2018, 451 private pharmacies were registered countrywide. Of these, 150 (33%) were based in Maputo city, which includes the KaMphumo district municipality, where the study was conducted. The registered private pharmacies in the study area were categorised according to the socioeconomic status (high, middle and low) of their location in the city. After using the Excel random number function, three pharmacies were randomly selected from each socio-economic area (n=9).
Pharmacists
A modified snowball sampling technique was used to recruit pharmacists. The first three pharmacists from each socioeconomic area were recruited by telephone based on the information provided by the National Direction of Pharmacy. We then asked each pharmacist to identify at least two other pharmacists working at pharmacies in the KaMphumo district municipality. We contacted 18 pharmacists in total, 17 of whom agreed to participate and were enrolled provided they were not the owners of the pharmacies and not a member of the pharmacy board. This was to ensure that pharmacy participants were working directly with the public, dispensing various pharmaceutical products including antibiotics.
Pharmacy clients
By using a purposeful sampling strategy, the researcher approached pharmacy clients on their exit from the pharmacy. All clients who purchased any medicine between 8:00 and 18:00 hours during the study period and could not provide a valid prescription were cordially invited to show their medication purchases. If the purchased medicine was an antibiotic in the form of tablets, capsules, pills, drops, cream/ointment or syrup, the clients were invited to participate. Clients less than 18 years old and those purchasing antibiotics on behalf of someone else were excluded.
Study tools and data collection
The interview guide for the pharmacists was developed after an extensive literature review of similar studies. Primary data were collected using face-to-face in-depth interviews with open-ended questions. The interview guide was based on the objectives of the study. It consisted of demographic information, questions regarding dispensing practices, reasons, perceptions of pharmacists regarding customers behaviours towards antibiotic use, compliance with the law and guidelines dispensing. The interview guide included a definition of SMA, which was defined as the circumstances wherein the customer requests, purchases and administers an antibiotic without prescription, to themselves or a child.
Two FGD sessions were planned for the pharmacists, but only 2 of the 17 pharmacists agreed to participate in the FGD; therefore, this technique was excluded. Eleven pharmacists were simultaneously employed at public and private pharmacies (performing day and night shifts) and were consequently interviewed at their respective public health facility placements in private rooms. The remaining six interviews of pharmacists working exclusively for private pharmacies occurred in a private room arranged by the researcher (on agreement with the participant).
Overall, 84 clients were approached, of which 44 with valid prescriptions were excluded. From the remaining 40 participants without prescriptions, eight declined to participate, reducing the number to 32. Twenty participants gave consent to participate in individual interviews and 12 to participate in the FGD only. Followed by in-depth interviews, two FGDs with six participants each, were performed. The individual interview guide consisted of demographic characteristics (age, gender, education level and profession), knowledge and behaviours towards of antibiotics use, behaviours towards antibiotics, patterns of SMA, the commonly used antibiotics and the health problems leading to SMA. Definition of antibiotics, self-medication, AR, information about the risks of SMA, was given to the participant at the end of the interview. To ensure a variety of participants and information, the participants of the FGD were different from the individual interviews.
The pharmacy clients participating in the FGD received a small amount (MTN500 00=US$10) to compensate them for transport and call/message expenses relating to logistical arrangements. FGD took place in a public municipality garden in the city centre, in the mornings (a less popular time). A week before the data collection, the first author hosted a 2-day workshop for research assistants to discuss and clarify the objectives of the study and the interview guides. After the first two interviews with each category of participants (clients and pharmacists), the leading researcher held a further 2-hour discussion with research assistants to revise the interview guides, thus ensuing the clarity, length, quality and appropriateness of the interview guides for the subsequent interviews.
Patient and public involvement
This qualitative research was based on face-to-face interviews and group discussions. Before the interviews, participants were informed of the study’s approval by the National Bioethics Committee of Mozambique and authorisation by the National Department of Pharmacy at the MoH of Mozambique.
Through an informed consent process, participants consented, in writing, to participate in the study and for interviews to be audio recorded. In addition to safeguarding personal and professional information, participants were informed that the results of the research would be deidentified and aggregated. Additionally, participants were informed that findings would be disseminated through publications in academic peer-review journals, and verbal presentation of the results to the MoH and the National Direction of Pharmacy.
Data management and analysis
The interviews were audio recorded in Portuguese, transcribed verbatim and translated into English. To check the accuracy of the translation, one randomly selected record was translated and then back-translated by a bi-lingual researcher. The transcripts were coded and thematically analysed. The first author read the transcripts for familiarity and made analytical notes to inform the coding stage. Two coders coded data; the coding tree included the main questions, the answers of participants, and the extracted themes and subthemes.
Results
The results are presented according to the themes that emanated from the analysis process namely: (1) perceived need to self-manage illness and expectations when using NPAs; (2) time spent seeking healthcare and past successful experiences with antibiotics; (3) the antibiotics used for self-medication and (4) the main health conditions leading to SMAs.
Demographics of participants
Participants who purchased NPAs included men 10 (31%) and women 22 (69%) ranging in age from 19 to 67 years. The clients’ average age was 35 years. Three levels of education were identified: primary (1st–7th graders), secondary (8th–12th graders) and tertiary (university level). The pharmacists included men 11 (64,7%) and women six (35,3%), with ages ranging from 24 to 47 years. The pharmacists’ mean age was 36 years. More than half of the pharmacists, 10 (58,8%) had between 5 and 15 years of professional experience, and the remaining 7 (41,2%) had between 2 and 4 years of professional experience. Table 1. presents the demographic characteristics of all included participants.
Table 1.
Demographic characteristics of participants
| Pharmacy clients | |||||
| Variables | Characteristics | No (%) | Variables | Characteristics | No (%) |
| Age | 19–20 | 3 (9.4) | Gender | Male | 10 (31.3) |
| 21–30 | 10 (31.3) | Female | 22 (68.8) | ||
| 31–40 | 9 (28.1) | Education level | Primary | 7 (21.8) | |
| 41–50 | 6 (18.8) | Secondary | 16 (50) | ||
| 51–67 | 4 (12.5) | Tertiary | 9 (28.1) | ||
| Pharmacists | |||||
| Age | 24–34 | 4 (23.5) | Gender | Male | 11 (64.7) |
| 35–44 | 10 (58.8) | Female | 6 (35.3) | ||
| 45–47 | 3 (17.6) | Professional experience | 5–15 years | 10 (58.8) | |
| 1–4 years | 7 (41.2) | ||||
Self-treatment, self-management of illness and expectations when using NPA
Almost all participants emphasised the need to assuming responsibility for their health, as well as the right to seek cure and treatment for self-identified health problems.
One participant indicated:
I just bought cotrisha (cotrimoxazole), I have to make sure I treat my cough (Pharmacy client, 12).
Medicines, including antibiotics without prescription, were seen by participantsas ‘goods’; as essential resources willingly consumed for self-treatment and well-being:
These are goods! They (medicines) are essential after all they help to combat some pathologies that the immune system cannot itself, we take and use them willing to get rid of illness and go on with life (Pharmacy client, 1).
Participant’s concerns regarding the use of NPAs were assessed through two questions: do you have any concerns and fears regarding your self-medication attitude? What are your fears when you use these medicines? The majority of participants reported not having any problems using NPAs. While some FGD participants expressed some degree of anxiety when using NPAs, they did not experience any regret for the practice, believing the need for treatment outweighed the risk of a possible adverse outcome.
Two participants remembered experiencing problems, such as diarrhoea and skin allergies after taking amoxicillin and cotrimoxazole tablets;
Medicines they help, but sometimes depends on your body… I once took cotrimoxazole and got pimples and dark itching skin…but the cough disappeared (Pharmacy clients, FGD 2).
We take them (the antibiotics) to became well, I got diarrhoea after taking these famous two-colour tablets (amoxicillin), the pharmacists said I should not take with any milk products (Pharmacy clients, FGD 1).
Time spent seeking healthcare and past successful experiences with antibiotics
The time spent to be assited by a physician or health care worker, at the health care facilities plays an essential role in the practices of SMAs. Participants complained about the long waiting time for consultation at healthcare facilities Time is perceived as a precious resource; spending many hours or the whole day at the clinic wastes this resource, especially when symptoms are mild, and there are other available treatment pathways such as pharmacies.
Most of the times you get to the public hospital to find out that the nurse or doctor is late, you wait forever to be assisted, and when assisted you get the prescription, but they have a shortage of drugs. You should go buy it outside, in private pharmacies (Pharmacy client, 17).
Many participants reported knowing about antibiotics from their own or a relative’s successful experience with antibiotics. These experiences informed their health-seeking strategy decisions in the event of a new sickness, or the reappearance of symptoms:
I got the prescription before when I had to seek medical appointment! This time I have the same difficulties swallowing, but they are almost finishing so I need more of these tablets (Pharmacy client, 1).
I know these big white tablets (amoxicillin with Clavulanic acid). I went to a doctor before, months ago (Pharmacy client, 2).
Pharmacists, in turn, confirmed that clients use physicians’ prescriptions and medical information from past experiences to construct their own understanding and guide their practices:
Patients seeks medical help at the hospital or clinic. Once, then twice, the doctor or nurse prescribes the same antibiotic; for any pain amoxicillin, for any cough cotrimoxazole, so people get confidence in certain antibiotics (Pharmacist, 8).
The commonly used NPAs
Participants were asked to describe, or indicate on the interviewer’s list, the antibiotics (other than the ones purchased) they previously used without prescription. Figure 1. shows the participants’s commonly used antibiotics.
Figure 1.
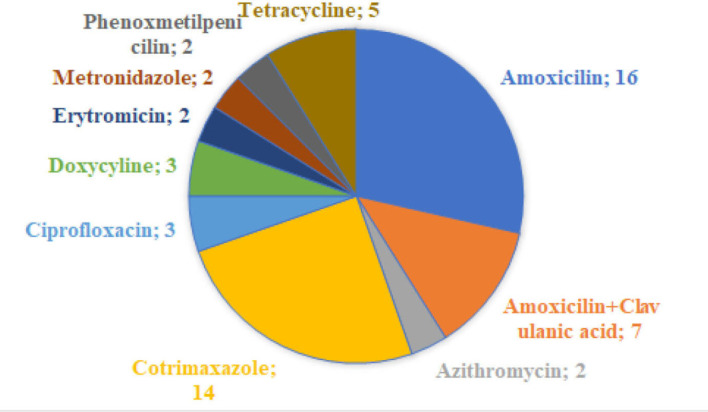
The commonly used non-prescribed antibiotics.
Overall, 30 (93.75%) out of 32 pharmacy clients acknowledged using a variety of antibiotics, such as amoxicillin, cotrimoxazole, ciprofloxacin, azithromycin, metronidazole, amoxicillin with acid clavulanic, tetracycline, doxycycline and erythromycin. As the quotes below indicate:
I used azithromycin and (…) I used the cotrisha (cotrimoxazole) (…) I used metrosha (metronidazole) (Pharmacy client, 10).
I already used erythromycin once to my child…and I already used cotrimoxazole and azithromycin, yes. (Pharmacy client, 3).
‘I asked the pharmacist to give me ‘two colours’(amoxicillin) to treat inside wounds (Pharmacy client, 2).
The results show that amoxicillin and cotrimoxazole were the most purchased antibiotics, with participants requesting the simple amoxicillin, or the one combined with clavulanic acid to treat various health conditions. This was endorsed by pharmacy clients in both individual and group interviews:
I think amoxicillin, the two colours. I use a lot even for the family, yes amoxicillin and the other white one for cough, cotrisha (cotrimoxazole). (Pharmacy client, 9). PLEASE NOTE THAT THIS IS A QUOTATION LIKE THE NEXT PARAGRAPH ITS SHOULD COME IN
What I see, we use a lot of that amoxicillin, I see many people, using the ‘two colours’, and now there is a better one with clavulanic…white big ones, expensive but also good. the other participants agreed. (Pharmacy clients, FGD 1).
In this study, 15 (88.2%) out of 17 pharmacists admitted dispensing NPAs and confirmed that the most commonly dispensed and purchased antibiotics were amoxicillin 500 mg, popularly known as ‘two colours’ (presented in half yellow and half red colours), followed by cotrimoxazole and amoxicillin with clavulanic acid;
Amoxicillin, cotrimoxazole, oh yes! The most wanted, they request much more amoxicillin in capsules with two colours (Pharmacist, 8).
Ooh, cotrimoxazole! Yeah, a lot, many HIV positive patients use cotrimoxazole as a prophylactic…we do sell that and the combined amoxicillin. (Pharmacist, 11).
Sexually transmitted infections (STI) has contributed to the increased demand for some antibiotics that were previously only known by the physicians and pharmacists. Pharmacists reported that clients increasingly request these antibiotics for the self-treatment of STIs.
Interestingly I see some changes, some clients do not want the common ‘two colours’ they now use a lot azytro (azithromycin), doxycycline, for complaints of urinary tract infection, sore throat and other complaints of sexual diseases…yeah (Pharmacist, 17).
From the pharmacists’ point of view, the clients are ‘learning’ about antibiotics through past experiences with physician’s prescriptions:
Not so long ago it was…let me say ‘fancy’ to prescribe amoxicillin with clavulanic acid…but now I see prescriptions of azithromycin, ciprofloxacin…then the patients are currently learning and purchasing as well, laughs (Pharmacist, 16).
The pharmacists recognised the growing practices of SMAs, with clients requesting more of the recent and broad-spectrum antibiotics. However, they noted with concern that antibiotics are wrongly administered with most clients requesting antibiotics in smaller quantities than prescribed for a 3-day course or 5-day course.
For example, he may request cotrimoxazole and take just ten tablets for two to three days, or amoxicillin and take for three days, they are doing it wrong either. (Pharmacist, 2).
Illnesses leading to the practices of SMAs
All the participants expressed their intention to recover from disease as quickly as possible. Sore throat, fever, cough, vaginal discharge, eye problems, the common influenza, urinary infection, respiratory tract problems, wounds and toothaches, were mentioned as the illnesses leading to the practices of SMAs.
I have to get rid of the pain when going to the toilet; then I bought these medicines (doxycycline and cotrimoxazole vaginal cream) and the cream to apply (Pharmacy client, 21).
Pharmacists confirmed that most clients purchased antibiotics for self-diagnosed health problems such as colds, influenza, cough, sore throat, respiratory tract problems, vaginal discharge, eye problems, fever and pain, dental pain and urinary infections.
People buy amoxicillin for flu, cotrimoxazole for cough, they want tetracycline and chloramphenicol for eyes, many complaints, many antibiotic drugs. (Pharmacists, 3).
Some complaints of cough with mucus and difficulty breathing, some young ladies buy amoxicillin with cotrimoxazole and metronidazole for vaginal discharge. (Pharmacists, 8).
Discussion
Through identifying the commonly used NPAs and illustrating the main health conditions associated in the urban area of Maputo city, this study has revealed how the practices of SMAs are undeniable and the dispensing practices are fragile. To date, research investigating the commonly used NPAs in Mozambique is non-existent. Thus, the findings presented in this study will add value to efforts to generate evidence on this topic.
In Mozambique, policies regarding medicines circulation, distribution, regulation and prescription are embedded in the Drug Law number 12/2017. Antimicrobials in general and antibiotics, in particular, are considered POMs in the same law. The findings reiterate the concerning practices of dispensing NPAs. Despite the established penalties for the non-compliant pharmacists and pharmacies, to date, no substantial penalties were publicly applied to pharmacies dispensing POMs.19 This may explain why we found no records of pharmacies that have been penalised for dispensing NPAs. The study findings reiterate the existent and concerning practices of the utilisation of antibiotics to treat self-diagnosed illnesses while highlights the easy accessibility of a variety of antibiotics at private pharmacies in Maputo city, Mozambique. The accessibility of NPAs in the study setting is in line with results reported in other studies,3 14 16 17 22–25 where patients had no difficulties or significant barriers accessing and using NPAs.
Self-medication and self-treatment
In this study, 30 out of 32 pharmacy clients admitted using NPA to manage their health problems. On the other hand, despite admitting dispensing NPAs to their clients, pharmacists noted with concern that the practices of SMAs are frequent and growing, with patients misusing antibiotics, requesting antibiotics in suboptimal and subtherapeutic quantities that do not allow them to complete at least the recommended five doses. Analogous results reported that costumers justified their suboptimal antibiotic dosages requests with financial constraints.26–28
Since events of sickness are likely to happen, participants expressed their entitlement to health. The health-seeking behaviour of participants is determined by their explanatory models of health and their medical rationalities.29 30 The practices of SMAs were regarded as a right of self-care where self-treatment is needed. However, what participants may not understand is that using NPAs exposes them to a variety of health risks, increasing the costs of healthcare services and the burden of resistant infections within the population. Moreover, participants were also not aware that by dispensing the requested NPAs, the pharmacists were acting against the dispensing protocols and the medicines law that states antibiotics are POMs.
Notwithstanding the participants’ concerns with their health and the desire to quickly recover from disease, the results show that the participants may not understand the clinical aetiology of the disease rather, they intend curing or alleviating the disease symptoms. Mainous et al. suggested that most individuals practising SMAs did not look to kill or inhibit the growth of bacteria, but only to ameliorate and recover from the sickness stage.31 Yet, according to Minayo et al. the population’s health disease vision is based on their real conditions of existence; or what the author calls ‘popular aetiology’ and they act based on these premises.32
Geest and Whyte stated that medicines are historically a significant part of the tradition of human health, of the process of healthcare-seeking, and the healthcare system for both, healthcare providers and patients.1 The behaviour of seeking antibiotics to alleviate disease is linked not only to the accessibility of the antibioticsbut also to the social constructions of health and disease process, healthcare workers and healthcare services. Rodrigues points to the responsibility individuals assume for their health, and to the everyday reasoning practices that are linked to the practices of SMAs.18 Therefore, providing patients with full and correct information about antibiotics, about the burden of AR, and the disadvantages of using NPAs alongside other health promotion measures could contribute to raise awareness. These actions would lead to health-seeking behaviours based on informed decisions that may discourage the practices of SMAs.
The study results show how patients learn quickly and use the medical knowledge they acquire when in contact with physicians and other healthcare workers. Patients use experiences (their own and others) of antibiotics, past sickness events and the health knowledge they acquire to construct health-seeking beliefs, attitudes and behaviours that determine their health responses to subsequent sickness events. The use of experience with antibiotics to inform subsequent health-seeking responses was also reported in another study.14
The time spent at healthcare facilities, especially at public health care facilities, was regarded by both pharmacists and clients as a barrier to accessing healthcare services. Participants, thus, used other care pathways and strategies, such as requesting advice from pharmacists and or purchasing medicines directly from the pharmacies.16 The need to seek treatment while saving time has a significant influence on the beliefs and practices of SMAs. Healthcare providers need to think carefully about strategies to reduce the waiting time at healthcare facilities, thus enabling access to public health facilities and oversight of antibiotic use. Simultaneously, providing pertinent user-friendly information regarding the appropriate use of antibiotics within the pharmacies would be critical to the success of strategies for influencing behaviour change related to antibiotic utilisation and containing AR. Contextually adapted approaches that better understand and address the practices of SMAs among the general public are critical.
Although some participants could define SMAs and were aware of some of the risks of the practice, they were not aware of the public health implications of the practices of SMAs. The younger participants referred to the antibiotics by their correct commercial names. However, older participants, and some participants from the low socioeconomic area pharmacies, referred to antibiotics by colour, shape and brand. For example, amoxicillin was referred to as ‘two colour’ due to its presentation in red-yellow capsules. Amoxicillin with clavulanic acid was referred to as the ‘big white tablets’. While tetracycline was referred to as ‘rounded pink and big tablets’, phenoxymethylpenicillin was referred to as ‘phenox’. Cotrimoxazole was referred by the Indian brand name ‘cotrisha’ and metronidazole as ‘metrosha’. The participant’s characterisation of the antibiotics mentioned above is concordant with the antibiotics available in the local pharmaceutical market.
Additionally, a recent study by Cambaco et al in a semirural setting of Mozambique, reported conceptualisation of antibiotics in participants’ terms, the association of antibiotics with specific colours, shapes and health conditions.33 The results show that individuals construct their representations of medicines and generate their terms to define antibiotics. In the current situation, where most individuals have insufficient and inadequate knowledge regarding antibiotics in this setting,17 this has a huge public health implicatiom. These social construtions and the social reproduction of this knowledge within the population may increase the beliefs and the confidence in antibiotics and consequently the widespread of the practices of SMAs. Thus, intensive educational interventions are needed to provide more and accurate knowledge that promotes the need to use antibiotics wisely emphasizing the individual and the public health implications y.
In this sense, medicines are not merely regarded as chemicals but as social goods1 34 that shapes how patients perceive the health disease process, the medication and how patients behave while seeking care. Therefore, clients and patient’s perspectives on medicines and particularly on antibiotics, need to be situated within their personal and group health narratives.1 34 Moreover, it is believed that individuals with appropriate information and knowledge are more likely to take informed decisions and adopt acceptable practices.35 36 These types of information and knowledge ought to be on-going and contextually adjusted and addressed by all stakeholders to improve antibiotic stewardship and conservancy.
The commonly used NPAs
The narratives of the participants, concerning the commonly used antibiotics, show that amoxicillin, cotrimoxazole and amoxicillin with clavulanic acid were the most used antibiotics. We found different results in a study in Nigeria, where ampicillin/cloxacillin, metronidazole, cotrimoxazole, ciprofloxacin and amoxicillin were the most used antibiotics.37
However, studies reporting massive utilisation of non-prescribed amoxicillin, cotrimoxazole and amoxicillin with clavulanic were found in Guatemala,38 39 Zambia40 and Ethiopia.41 This shows the different preferences of antibiotics by the public in other settings. Antibiotic choices and the trending use may be linked to the circulation and availability of these drugs in each location, as the processes of production, importation and distribution of pharmaceutical products vary across countries.42
The utilisation of other antibiotics less prescribed by physicians and more potent antibiotics such as azithromycin, doxycycline and ciprofloxacin were also noticed. This was regarded by pharmacists as a changing trend in the utilisation of antibiotics, especially within the middle and high socioeconomic area pharmacy clients. Comparable results were reported in studies from India, where the tendency to request less common and more potent antibiotics was frequent.10 43
This trending change may be due to the occurrence of bacterial resistance of the penicillin class of which amoxicillin is part. However, this study’s results did not intended to be a confirmation of the emergence of resistant bacteria for the previously used antibiotic classes. However, the tendency to use more potent and less prescribed NPAs, suggests patients quickly learn from prescribers, become soon informed and use the medical information on their own. Therefore, awareness -raising while prescribing would play a role to discourage patients from using the medical information in the next sickness eventswhile discouraging the use of NPAs.
Concerning the diseases and health complaints leading to the practices of SMAs, the results point to common cold, influenza, cough, sore throat, viral respiratory tract problems, vaginal discharge, eye problems, fever, pain, dental pain and urinary tract problems as the most reported health conditions. Advances in medicine have proven that antibiotics are not effective to treat non-bacterial diseases and viral infections. When a bacterial infection is present, specific antibiotics are needed to treat particular infections. Thus, only qualified healthcare professionals are entitled to determine which antibiotic should be used for which bacterial infection after a clinical assessment of the patient. This is a universal clinical protocol and guideline that protects patients in the use of antibiotics, promotes wise utilisation and improves health safety.44–46 Nevertheless, the literature is rich with evidence of practices of SMAs to self-treat, self-diagnosed health conditions that do not necessarily require antibiotic treatment.16 18 24 25 33 47–56 If the patients and pharmacy clients are exposed to this information at all levels, in parallel with other awareness-raising actions, people would be more likely to make informed decisions and avoid self-diagnosis and self-treatment with NPAs. Moreover, the public ability to rapidly learn and recall health information represents an opportunity that should be grasped by pharmacists’, physicians and health promoters to disseminate the correct information about the rational use of antibiotics.
Limitations of the study
This study may serve as exploratory evidence for understanding individual and community expectations, perceptions and uses of antibiotics. Despite the use of the qualitative approach and the in-depth interviews conducted with the dispensers (pharmacists) and the users (pharmacy clients), this study has some limitations. One example is the fact that some participants had to recall the name of antibiotics they have used in the past, which may have the potential of recall bias. Moreover, the tools could be improved if FGD with pharmacists could be performed. These would be useful to capture the opinions of pharmacists in a group and compare with personal views. Additionally, the participants included are not representative of all pharmacies in Maputo city. The study recommends a more extensive comprehensive qualitative and quantitative study of this phenomenon to better inform the public, health authorities and policy-makers.
Conclusion
The findings of this study highlighted the common use of non-prescribed antibiotics to manage individuals and families’ health. Participants freely requested, and pharmacists willingly dispensed antibiotics without valid prescriptions. While using antibiotics to treat self peceived diseases, most of them that do not necessarily need antibiotic treatment, participants incured in the wrong choice of antibioticdosage and duration of the treatment. Nevertheless, participants perceive the practices of SMAs as self-care rather than misuse of antibiotics. Participants’ use of pharmacies as the first point of care and their perception of antibiotics as powerful medicines and easily available medical resources, together with the suboptimal dispensing practices of pharmacists, largely influences the growing practices of SMAs among the studied participants.
While there is a need for broader assessment and understanding of health-seeking beliefs and behaviours regarding the utilisation of medicines in general and antibiotics in particular, contextually adjusted and multifaceted interventions are needed to involve public health stakeholders, individuals, communities and the pharmacists in awareness-raising programmes for antibiotic stewardship and conservancy at all levels in Mozambique.
Supplementary Material
Acknowledgments
ISCISA, NORHED Project and the University of KwaZulu-Natal are acknowledged for the incentive and provision of resources towards this study. The UKZN College of Health Sciences - School of Nursing and Public Health, is acknowledged for the provision of research methodology as well as manuscript writing workshops. The manuscript reviewers are acknowledged for their insightful comments.
Footnotes
Contributors: NFT is the principal investigator, and the main contributor to the manuscript who conceptualised and prepared the draft proposal of the study under the supervision of LEM and VPS. Both LEM and VPS assisted in all stages of the research process and with the manuscript revision and redaction. NFT, LEM and VPS contributed to the reviewed draft version of the manuscript and approved the final version.
Funding: The study was partially funded by a grant received at ISCISA (Higher Institute for Health Sciences) from the NORHED Project (Norway Higher Education and Development) and by College of Health Sciences, the University of KwaZulu Natal as scholarship awarded to the first author.
Disclaimer: The authors declare that the sponsors did not influence the study.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication: Not required.
Ethics approval: The Humanities approved this study, and Social Sciences Ethical Committee (HSREC) from the University of KwaZulu Natal, Durban, South Africa and by the National Bioethics Committee for Health (CNBS) form the Ministry of Health, Mozambique.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available on reasonable request. The raw data for this study were attained in the Portuguese language; the datasets were transcribed and translated to English. The datasets analysed for this paper will be accessed from the corresponding author on reasonable request.
References
- 1.Geest Svander, Whyte SR. The charm of medicines: metaphors and metonyms. Med Anthropol Q 1989;3:345–67. 10.1525/maq.1989.3.4.02a00030 [DOI] [Google Scholar]
- 2.Aminov RI. A brief history of the antibiotic era: lessons learned and challenges for the future. Front Microbiol 2010;1:134. 10.3389/fmicb.2010.00134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Auta A, Hadi MA, Oga E, et al. Global access to antibiotics without prescription in community pharmacies: a systematic review and meta-analysis. J Infect 2019;78:8–18. 10.1016/j.jinf.2018.07.001 [DOI] [PubMed] [Google Scholar]
- 4.Napolitano F, Izzo MT, Di Giuseppe G, et al. Public knowledge, attitudes, and experience regarding the use of antibiotics in Italy. PLoS One 2013;8:e84177. 10.1371/journal.pone.0084177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO The evolving threat of antimicrobial resistance: options for action. Geneva: World Health Organization, 2012. [Google Scholar]
- 6.WHO Critically important antimicrobials for human medicine. 3rd Rev., 2012. [Google Scholar]
- 7.WHO Antimicrobial resistance: global report on surveillance, 2014. [Google Scholar]
- 8.Hollis A, Ahmed Z. Preserving antibiotics, rationally. N Engl J Med 2013;369:2474–6. 10.1056/NEJMp1311479 [DOI] [PubMed] [Google Scholar]
- 9.Laxminarayan R, Matsoso P, Pant S, et al. Access to effective antimicrobials: a worldwide challenge. Lancet 2016;387:168–75. 10.1016/S0140-6736(15)00474-2 [DOI] [PubMed] [Google Scholar]
- 10.Kotwani A, Holloway K. Trends in antibiotic use among outpatients in New Delhi, India. BMC Infect Dis 2011;11:99. 10.1186/1471-2334-11-99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morgan DJ, Okeke IN, Laxminarayan R, et al. Non-prescription antimicrobial use worldwide: a systematic review. Lancet Infect Dis 2011;11:692–701. 10.1016/S1473-3099(11)70054-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aryee A, Price N. Antimicrobial stewardship - can we afford to do without it? Br J Clin Pharmacol 2015;79:173–81. 10.1111/bcp.12417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mueller T, Östergren P-O. The correlation between regulatory conditions and antibiotic consumption within the who European region. Health Policy 2016;120:882–9. 10.1016/j.healthpol.2016.07.004 [DOI] [PubMed] [Google Scholar]
- 14.Alhomoud F, Aljamea Z, Basalelah L. ‘Antibiotics kill things very quickly’- consumers’ perspectives on non-prescribed antibiotic use in Saudi Arabia. BMC Public Health 2018;18:1177. 10.1186/s12889-018-6088-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mshana SE, Matee M, Rweyemamu M. Antimicrobial resistance in human and animal pathogens in Zambia, Democratic Republic of Congo, Mozambique and Tanzania: an urgent need of a sustainable surveillance system. Ann Clin Microbiol Antimicrob 2013;12:28. 10.1186/1476-0711-12-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Torres NF, Solomon VP, Middleton LE. Patterns of self-medication with antibiotics in Maputo City: a qualitative study. Antimicrob Resist Infect Control 2019;8:161. 10.1186/s13756-019-0618-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mate I, Come CE, Gonçalves MP, Elizabeth, Maria P, et al. Knowledge, attitudes and practices regarding antibiotic use in Maputo City, Mozambique. PLoS One 2019;14:e0221452. 10.1371/journal.pone.0221452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rodrigues CF. Self-medication with antibiotics in Maputo, Mozambique: practices, rationales and relationships. Palgrave Communications 2020;6:1–12. [Google Scholar]
- 19.Torres N, Solomon V, Middleton L. Pharmacists’ practices for non-prescribed antibiotic dispensing in Mozambique. Pharm Pract 2020;18:1965. 10.18549/PharmPract.2020.3.1965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.“Antibiotics heal all diseases”; factors influencing the pratices of self-medication with antibiotics in Maputo City, MozambiqueDOI : 10.1007/s10389-020-01416-7JOPH-D-20-00960R1
- 21.Instituto Nacional de Estatística (INE) IV Recenseamento Geral da População e Habitação 2017: Resultados Definitivos - Moçambique, Abril, 2019. [Google Scholar]
- 22.Jamhour A, El-Kheir A, Salameh P, et al. Antibiotic knowledge and self-medication practices in a developing country: a cross-sectional study. Am J Infect Control 2017;45:384–8. 10.1016/j.ajic.2016.11.026 [DOI] [PubMed] [Google Scholar]
- 23.Yates TD, Davis ME, Taylor YJ, et al. Not a magic pill: a qualitative exploration of provider perspectives on antibiotic prescribing in the outpatient setting. BMC Fam Pract 2018;19:96. 10.1186/s12875-018-0788-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ekambi E, Penda N, Mpondo M. Knowledge, practices and attitudes on antibiotics use in Cameroon: self-medication and prescription survey among children, adolescents and adults in private pharmacies, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grigoryan L, Germanos G, Zoorob R, et al. Use of antibiotics without a prescription in the U.S. population: a scoping review. Ann Intern Med 2019;171:257–63. 10.7326/M19-0505 [DOI] [PubMed] [Google Scholar]
- 26.Awad AI, Eltayeb IB. Self-Medication practices with antibiotics and antimalarials among Sudanese undergraduate university students. Ann Pharmacother 2007;41:1249–55. 10.1345/aph.1K068 [DOI] [PubMed] [Google Scholar]
- 27.Senadheera GP, Sri Ranganathan S, Gunawardane NS, et al. Practice of self-medication with antibiotics in the Colombo district, Sri Lanka. Ceylon Med J 2017;62:70. 10.4038/cmj.v62i1.8439 [DOI] [PubMed] [Google Scholar]
- 28.Ali AS, Ahmed J, Ali AS, et al. Practices of self-medication with antibiotics among nursing students of Institute of nursing, Dow University of health sciences, Karachi, Pakistan. J Pak Med Assoc 2016;66:235–7. [PubMed] [Google Scholar]
- 29.Porter R. Patients and healers in the context of culture. An exploration of the borderland between anthropology, medicine, and psychiatry. Med History 1981;25:435. [Google Scholar]
- 30.Luz MT, Camargo K. A comparative study of medical rationlitlies. Curare J Ethnomed 1997;12:47–58. [Google Scholar]
- 31.Mainous AG, Diaz VA, Carnemolla M. Factors affecting Latino adults’ use of antibiotics for self-medication. J Am Board Fam Med 2008;21): :128–34. 10.3122/jabfm.2008.02.070149 [DOI] [PubMed] [Google Scholar]
- 32.Minayo MCdeS. Saúde-doença: uma concepção popular dA etiologia. Cadernos de Saúde Pública 1988;4:363–81. 10.1590/S0102-311X1988000400003 [DOI] [Google Scholar]
- 33.Cambaco O, Alonso Menendez Y, Kinsman J, et al. Community knowledge and practices regarding antibiotic use in rural Mozambique: where is the starting point for prevention of antibiotic resistance? BMC Public Health 2020;20:1–15. 10.1186/s12889-020-09243-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Webster A, Douglas C, Lewis G. Making Sense of Medicines: ‘Lay Pharmacology’ and Narratives of Safety and Efficacy. Sci Cult 2009;18:233–47. 10.1080/09505430902885631 [DOI] [Google Scholar]
- 35.Davis R, Campbell R, Hildon Z, et al. Theories of behaviour and behaviour change across the social and behavioural sciences: a scoping review. Health Psychol Rev 2015;9:323–44. 10.1080/17437199.2014.941722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pinder RJ, Sallis A, Berry D. Behaviour change and antibiotic prescribing in healthcare settings literature review and behavioural analysis, 2015. [Google Scholar]
- 37.Israel E, Emmanuel E, Sylvester E, et al. Self-medication with antibiotics amongst civil servants in Uyo, Southern Nigeria. J Adv Med Pharm Sci 2015;2:89–97. 10.9734/JAMPS/2015/15147 [DOI] [Google Scholar]
- 38.Ramay BM, Córdova L, Cerón A. Self-medication with antibiotics in four Guatemala City pharmacies: characteristics, sources of information, perceived effects, and motives. Revista Cientifica 2016;26:19. [Google Scholar]
- 39.Ramay BM, Lambour P, Cerón A. Comparing antibiotic self-medication in two socio-economic groups in Guatemala City: a descriptive cross-sectional study. BMC Pharmacol Toxicol 2015;16:11. 10.1186/s40360-015-0011-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kalungia AC, Burger J, Godman B, et al. Non-Prescription sale and dispensing of antibiotics in community pharmacies in Zambia. Expert Rev Anti Infect Ther 2016;14:1215–23. 10.1080/14787210.2016.1227702 [DOI] [PubMed] [Google Scholar]
- 41.Eticha T, Araya H, Alemayehu A, et al. Prevalence and predictors of self-medication with antibiotics among Adi-haqi campus students of Mekelle University,. Ethiopia. Internat J Pharma Sci Res 2014;5:678–84. [Google Scholar]
- 42.Chaudhuri S, Mackintosh M, Mujinja PGM. Indian generics producers, access to essential medicines and local production in Africa: an argument with reference to Tanzania. Eur J Dev Res 2010;22:451–68. 10.1057/ejdr.2010.27 [DOI] [Google Scholar]
- 43.Kotwani A, Wattal C, Joshi PC, et al. Irrational use of antibiotics and role of the pharmacist: an insight from a qualitative study in New Delhi, India. J Clin Pharm Ther 2012;37:308–12. 10.1111/j.1365-2710.2011.01293.x [DOI] [PubMed] [Google Scholar]
- 44.WHO Global action plan on antimicrobial resistance. Geneva: Google Scholar, 2015. [Google Scholar]
- 45.WHO Worldwide country situation analysis: response to antimicrobial resistance: summary. Geneva: World Health Organization, 2015. [Google Scholar]
- 46.WHO Assessing non-prescription and inappropriate use of antibiotics: report on survey, 2019. [Google Scholar]
- 47.Ajayi I. Self medication practices among patients seen in a suburban tertiary eye care centre in Nigeria, 2014. [Google Scholar]
- 48.Alhomoud F, Aljamea Z, Almahasnah R, et al. Self-medication and self-prescription with antibiotics in the Middle East-do they really happen? A systematic review of the prevalence, possible reasons, and outcomes. Int J Infect Dis 2017;57:3–12. 10.1016/j.ijid.2017.01.014 [DOI] [PubMed] [Google Scholar]
- 49.Zhu X, Pan H, Yang Z, et al. Self-medication practices with antibiotics among Chinese university students. Public Health 2016;130:78–83. 10.1016/j.puhe.2015.04.005 [DOI] [PubMed] [Google Scholar]
- 50.Ngigi CK, Mwagiru P, Wala J. Self-medication with antibiotics prior to seeking treatment among adult patients attending outpatient department at gatundu sub-county hospital, Kiambu County, Kenya. Imp J Interdiscip Res 2016;2. [Google Scholar]
- 51.Gajdács M, Paulik E, Szabó A. Knowledge, attitude and practice of community pharmacists regarding antibiotic use and infectious diseases: a cross-sectional survey in Hungary (KAPPhA-HU). Antibiotics 2020;9:41 10.3390/antibiotics9020041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Aslam A, Gajdács M, Zin CS, et al. Public awareness and practices towards self-medication with antibiotics among the Malaysian population. A development of questionnaire and pilot-testing. Antibiotics 2020;9:97. 10.3390/antibiotics9020097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Alrasheedy AA, Alsalloum MA, Almuqbil FA, et al. The impact of law enforcement on dispensing antibiotics without prescription: a multi-methods study from Saudi Arabia. Expert Rev Anti Infect Ther 2020;18:87–97. 10.1080/14787210.2020.1705156 [DOI] [PubMed] [Google Scholar]
- 54.Zapata-Cachafeiro M, Piñeiro-Lamas M, Guinovart MC, et al. Magnitude and determinants of antibiotic dispensing without prescription in Spain: a simulated patient study. J Antimicrob Chemother 2019;74:511–4. 10.1093/jac/dky440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Torres NF, Chibi B, Middleton LE, et al. Evidence of factors influencing self-medication with antibiotics in low and middle-income countries: a systematic scoping review. Public Health 2019;168:92–101. 10.1016/j.puhe.2018.11.018 [DOI] [PubMed] [Google Scholar]
- 56.Jakupi A, Raka D, Kaae S, et al. Culture of antibiotic use in Kosovo - an interview study with patients and health professionals. Pharm Pract 2019;17:1540. 10.18549/PharmPract.2019.3.1540 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


