Abstract
Prognosis communication in heart failure is often narrowly defined as a discussion of life expectancy, but as clinical guidelines and research suggest, these discussions should provide a broader understanding of the disease, including information about disease trajectory, the experiences of living with heart failure, potential burden on patients and families, and mortality. Furthermore, despite clinical guidelines recommending early discussions, evidence suggests that these discussions occur infrequently or late in the disease trajectory. We review the literature concerning patient, caregiver, and clinician perspectives on discussions of this type, including the frequency, timing, desire for, effects of, and barriers to their occurrence. We propose an alternate view of prognosis communication, in which the patient and family/caregiver are educated about the nature of the disease at the time of diagnosis, and a process of engagement is undertaken so that the patient's full participation in their care is marshalled, and the care team engages the patient in the informed decision making that will guide care throughout the disease trajectory. We also identify and discuss evidence gaps concerning (i) patient preferences and readiness for prognosis information along the trajectory; (ii) best practices for communicating prognosis information; and (iii) effects of prognosis communication on patient's quality of life, mental health, engagement in critical self‐care, and clinical outcomes. Research is needed to determine best practices for engaging patients in prognosis communication and for evaluating the effects of this communication on patient engagement and clinical outcomes.
Keywords: Heart failure, Prognosis, Communication, End of life, Disease progression
Introduction
Unlike in other chronic or serious illnesses where the disease trajectory may be linear and more easily predicted, heart failure (HF) is a chronic disease that is characterized by a heterogeneous disease course and multiple co‐morbidities. 1 , 2 Despite advancements in care and more patients living with late phases of the disease, 5‐year mortality remains at nearly 53%, 3 , 4 comparable with that for several cancers. 5 , 6
The American Heart Association recommends that discussions focused on quality of life (QoL) and the identification of patient values and goals of care, along with information about life expectancy, be conducted at annual care reviews for patients with HF. 4 , 7 Furthermore, the Canadian Cardiovascular Society and the Heart Failure Association of the European Society of Cardiology suggest that discussions about prognosis and related issues occur early in the HF trajectory and following any changes in health status. 8 , 9 It is important to note however that extant prediction models concerning prognosis in HF are poor. 10 , 11 Furthermore, as implied in these recommendations, the notion of ‘prognosis communication’ in HF care may be a misnomer, in that the discussions being recommended by these professional organizations encompass a much broader focus on patient engagement and an iterative discussion of disease trajectory, as opposed to a conversation narrowly focused on life expectancy estimates. Iterative discussions of this kind could serve as opportunities for better informed decision making and to more fully engage patients in their care—e.g. through better adherence to medication and lifestyle recommendations—and thus potentially alter the disease trajectory.
Methodology
We review the limited research to identify promising signals and evidence gaps. Additionally, we propose a new model of prognosis communication across the HF trajectory (see Figure 1 ) and discuss research to address these evidence gaps.
Figure 1.
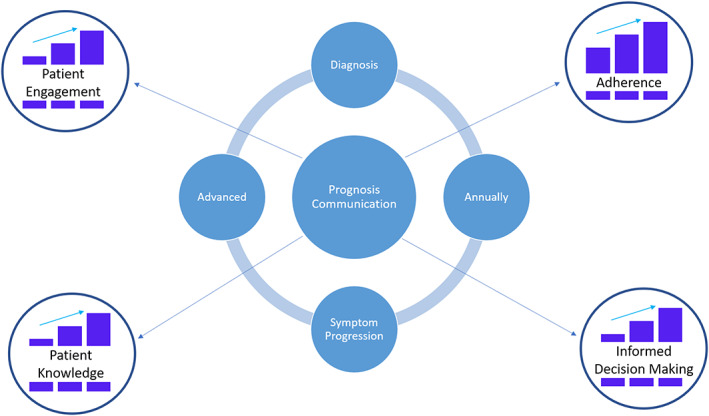
Model of prognosis communication across the heart failure disease trajectory.
For this review, we conducted a search from 1990 to 2017 of PubMed, Scopus, and Cochrane databases. Combinations of terms used include Communicate, Communication, Prognosis, Prognostic, Future, Expectations, and Disease Severity. A limited secondary search was conducted in 2018. Additionally, reference lists from published papers were reviewed for potentially relevant articles. Studies were eligible for inclusion if they were published in peer‐reviewed journals and available in English (see Table 1 for sample characteristics of studies included in the review).
Table 1.
Study characteristics
| Author | Sample size (N) | Sample characteristics | HF class/stage | Methodology | Key points |
|---|---|---|---|---|---|
| Ågård et al. 34 | 40 | PT | II–IV | QL | 1. >75% did not request prognostic information. |
| Ahluwalia et al. 18 | 96 | PT, CL | 93.1% C–D | X+ | 1. In 71 visits, physicians discussed the life‐limiting potential of HF one time. |
| Aldred et al. 12 | 20 | PT, CA | II–IV | QL | 1. Few patients received prognosis information. |
| 2. Patients were able to make realistic life expectancy estimates. | |||||
| Allen et al. 26 | 122 | PT | I–IV | QT | 1. Median patient predicted life expectancy was 13 years as compared with a median model predicted life expectancy of 10 years. |
| Barnes et al. 38 | 123 | PT, CL | III–IV | QL | 1. Few patients received prognosis information. |
| Boyd et al. 39 | 20 a | PT, CA, CL | IV | QL | 1. Patients feared sanctions if they requested additional information from clinicians. |
| Caldwell et al. 23 | 20 | PT | 85% III | QL | 1. Patients preferred learning prognosis information early in the disease trajectory with physicians initiating the discussions and engaging in two‐way conversations with patients. |
| 2. Some patients expressed ambivalence about the amount of prognosis information they wanted. | |||||
| Dougherty et al. 14 | 24 | PT | C–D | QL | 1. Patients expressed that their future was not clearly explained. |
| 2. Patients expressed fear concerning asking clinicians for this information. | |||||
| 3. Patients expressed that specific life expectancy estimates were not helpful. | |||||
| Dunlay et al. 24 | 95 | CL | N/A | QT | 1. 12% of clinicians have end‐of‐life discussions annually. |
| 2. 52% of clinicians were hesitant to have these discussions due to discomfort, perception that patient or family lacked readiness, fear of causing a loss of hope, and lack of time. | |||||
| 3. 30% of clinicians described a low or very low level of confidence in initiating prognosis discussions. | |||||
| Fried et al. 17 | 503 b | PT, CA, CL | + | QT | 1. 55% of patients with HF wanted to know their life expectancy. |
| 2. 20% of patient–clinician and 21% of caregiver–clinician pairs agreed that the fatal nature of their illness had been discussed. | |||||
| 3. 3% of patient–clinician and 7% of caregiver–clinician pairs agreed that they discussed life expectancy. | |||||
| 4. 46% of clinicians (in patient–clinician pairs) reported that the fatal nature of the illness had been discussed, and 23% of clinicians reported that life expectancy had been discussed. | |||||
| Gerlich et al. 15 | 12 | PT | + | QL | 1. Patients and caregivers rarely discussed prognosis. |
| Gordon et al. 19 | 104 | PT | II–III | QT | 1. 68% of patients had discussed prognosis. |
| 2. 80.6% of patients who had not discussed prognosis expressed a desire for this information. | |||||
| Gott et al. 13 | 40 | PT | III–IV | QL | 1. Few patients reported engaging in prognosis discussions. |
| 2. Some patients stated that they did not want prognosis information. | |||||
| Hanratty et al. 43 | 34 | CL | N/A | QL | 1. Clinicians expressed concern about discussing prognosis too soon and having the patient lose faith in the team. |
| 2. Clinicians described themselves as poor at prognostication in HF. | |||||
| Hanratty et al. 40 | 50 b | PT | + | QL | 1. A majority of patients were not informed about their prognosis. |
| 2. Patients reported that they were unlikely to seek information because they feared being perceived as bothersome. | |||||
| Harding et al. 41 | 43 | PT, CA, CL | III–IV | QL | 1. Clinicians attributed non‐adherence to patients' lack of understanding. |
| 2. No patients and caregivers received prognosis information. | |||||
| 3. Clinicians identified the unpredictable trajectory of HF, cognitive impairments, and lack of time and resources as barriers to prognosis communication. | |||||
| Heyland et al. 21 | 600 b | PT, CA | IV or EF ≤ 25% | QT | 1. 18% of patients and 30.1% of family members reported having prognosis discussions with clinicians. |
| 2. Patients who recalled these discussions reported more satisfaction with care. | |||||
| Hjelmfors et al. 44 | 111 | CL | N/A | QT | 1. 96% of HF nurses reported discussing prognosis with patients. |
| 2. 69% of HF nurses reported that clinicians should be primarily responsible for prognosis discussions. | |||||
| 3. HF nurses identified the following as barriers to these conversations: the unpredictable trajectory of HF, patient co‐morbidities, cognitive impairments, worrying about causing a loss of hope, and lack of time. | |||||
| 4. 18% identified a lack of communication skills as a barrier. | |||||
| Hjelmfors et al. 22 | 279 | PT, CL | I–IV | Mixed | 1. 38% of patients received prognosis communication. |
| Horne and Payne 35 | 20 | PT | II–IV | QL | 1. Patient views concerning desire for prognosis information were mixed. |
| Howie‐Esquivel and Dracup 36 | 47 | PT | II–IV | Mixed | 1. 44% of patients wanted more prognosis communication. |
| 2. Patient desire for more prognosis communication was associated with higher self‐efficacy scores and increased odds of rehospitalizations. | |||||
| Klindtworth et al. 27 | 25 | PT | III–IV | QL | 1. Patients often did not perceive the life‐limiting aspect of HF and had little knowledge about prognosis. |
| 2. Patients attributed HF to old age. | |||||
| Murray et al. 16 | 40 a , b | PT, CA, CL | IV | QL | 1. Patients with HF had a poorer understanding of their prognosis than patients with cancer. |
| 2. Patients with HF received fewer services than patients with cancer. | |||||
| Narayan et al. 33 | 24 | PT | II–IV | QL | 1. 17 patients expressed a desire to receive their SHFM estimates. |
| 2. Patients who received their Seattle Heart Failure Mode (SHFM) estimates described experiencing control and hope. | |||||
| O'Donnell et al. 37 | 50 | PT | 64% III–IV | QL | 1. Patients in a palliative care intervention were more likely to report prognoses aligned with clinician assessment. |
| 2. Patients in the intervention group did not experience significant changes in depression, anxiety, or quality of life (QoL). | |||||
| O'Leary et al. 32 | 100 b | PT | III–IV | Mixed | 1. Patients with HF were unsure of the course of HF in the future. |
| Rodriguez et al. 31 | 25 | PT | 52% II | QL | 1. Patients who discussed prognosis with a clinician also described a more uncertain future. |
| 2. Patients who had not discussed prognosis expressed interest in receiving prognosis information. | |||||
| Rogers et al. 29 | 27 | PT | II–IV | QL | 1. Some patients lacked knowledge about their prognosis. |
| 2. Some patients may have been aware of their prognosis but did not acknowledge it. | |||||
| Selman et al. 42 | 43 | PT, CA, CL | III–IV | QL | 1. Clinicians reported that it was difficult to discuss poor prognosis. |
| 2. Clinicians identified a lack of communication skills as a barrier to prognosis communication. | |||||
| Strachan et al. 20 | 106 | PT | IV or EF < 25% | QT | 1. 11.3% of patients had discussed life expectancy with their clinician. |
| van der Wal et al. 25 | 678 | PT | II–IV | QT | 1. 21% of patients were unsure of future expectations concerning HF. |
| 2. 13% of patients expected to be cured. | |||||
| 3. Deterioration expectations were associated with lower QoL score, greater worry about the future, more unsatisfaction with care, higher mortality rate, and more HF readmissions. | |||||
| Willems et al. 28 | 31 | PT | III–IV, or EF < 25%, or at least one hospitalization due to HF | QL | 1. Most patients were unaware that they may die earlier because of HF. |
| Zapka et al. 30 | 90 b | PT | + | Mixed | 1. Patients with HF were less aware of their prognosis as compared with patients with cancer. |
CA, caregiver sample; CL, clinician sample; EF, ejection fraction; QL, qualitative methodology; QT, quantitative methodology; Mixed, mixed‐methods; N/A. NYHA class or ACC/AHA stage not applicable due to sample including only clinicians; Not reported, total sample size not reported; PT, patient sample; X+ qualitative analysis of observational data; +, NYHA class or ACC/AHA stage not reported, but samples described as having a limited life expectancy, advanced HF, or being in the last year of life.
Number of patients included in study, but an unknown number of caregivers and/or clinicians were also included.
Sample included patients with other chronic illnesses (e.g. cancer and chronic obstructive pulmonary disease).
Frequency and timing of prognosis communication
Reports on the frequency of prognosis communication include five qualitative studies, 12 , 13 , 14 , 15 , 16 one mixed‐methods study, 17 one observational study, 18 and several self‐report survey studies, 19 , 20 , 21 , 22 while only three included patients in early HF stages [e.g. New York Heart Association (NYHA) Classes I–II], 12 , 19 , 22 a common occurrence in this literature that limits generalization of findings. In these studies, discussions were largely about prognosis and occurred infrequently 13 , 15 , 18 , 20 , 21 , 22 with rates typically ranging from 11% to 38% of patients. 20 , 22 For example, in one large (n = 600) survey that compared caregivers and patients with HF, chronic obstructive lung disease, cirrhosis, and cancer, discussion of prognosis with a clinician was recalled by only 18% of patients with HF and 30% of their caregivers. 21 Similarly, in one qualitative content analysis of 71 audio‐recorded clinical encounters, it was found that in only 17 instances did physicians explain the nature of HF, and only once was the life‐limiting potential of the disease mentioned. 18 Yet, in one large (n = 104) cross‐sectional study, between 68% and 90% of patients with HF stated that they had had discussions about what to expect in the future, including prognosis. 19 Interestingly, patients, caregivers, and clinicians appear to differ in their perceptions concerning the occurrence of prognosis communication. In one study of 214 patients with cancer, HF, or chronic obstructive pulmonary disease and limited life expectancy, only 20% of patient–clinician and 21% of caregiver–clinician pairs agreed that the fatal nature of the illness had been discussed, and only 3% of patient–clinician and 7% of caregiver–clinician pairs agreed that discussion about life expectancy had occurred. 17 Yet 46% of clinicians (in patient–clinician pairs) reported discussing the fatal nature of the illness with the patient, and 23% reported discussing life expectancy, with similar findings for caregiver–clinician pairs.
This apparent ‘disconnect’ can easily occur at the end stage of a disease such as HF, when the issues at hand are fraught with concerns about impending mortality. Indeed, a small (n = 20) study of patients with HF found that some expressed a preference to receive prognosis information close to the time of HF diagnosis, when they are more likely to be alert, while others expressed a preference for having multiple opportunities to discuss prognosis—e.g. so that they had multiple opportunities to absorb the information. 23 Yet, in one study of HF clinicians (n = 95), 24 only 12% reported having annual focused discussions with patients, and these were limited to end‐of‐life discussions, while in another study (n = 279), from Sweden and the Netherlands, 22 clinicians indicated that prognosis discussions occur most often when a patient experiences a decline in health status or when they are approaching end of life. These clinicians also noted that there was no agreement on the correct timing for these discussions with patients. 22 Thus, there is little data to inform timing of prognosis information from the patient perspective, and the two studies of clinician preference demonstrate deviation from recommendations.
Patient understanding of prognosis communication
The infrequent occurrence of prognosis communication may be a contributing factor to patients' limited understanding of the nature and trajectory of HF. One large study of patients (n = 678) found that 25% had little knowledge about future health expectations and 13% expected to be cured. 25 In addition, in a prospective survey (n = 122), patients with HF estimated their life expectancy as a median of 13 years as compared with model predictions of a median of 10 years. 26 Furthermore, although 51% of patients expected to have HF for the rest of their lives, they did not expect the disease to reduce their lifespan. 26 Several other studies have also shown that patients with HF do not appreciate the terminal nature of their disease even when compared with other chronic or terminal illnesses. 15 , 16 , 27 , 28 , 29 , 30 For example, two studies suggest that patients with HF are less aware of their prognosis as compared with patients with advanced cancer 30 and that patients with advanced HF do not acknowledge the terminal nature of HF, whereas those with lung cancer appear to understand their disease status. 16 Overall, these studies suggest that a lack of prognosis communication may contribute to patients with HF having a limited understanding of prognosis. Also of note, two small qualitative studies (n = 25 31 and n = 27 29 ) suggest that patient understanding of prognosis can be limited even when clinicians have discussed this with them 31 or that while aware of prognosis, they are reluctant to acknowledge it. 29
Yet other research suggests that patients may understand the poor prognosis associated with HF even in the absence of prognosis communication. A small, qualitive study of 10 patients with NYHA Class II–IV HF found that many are aware that their prognosis is poor even when they have not discussed this with their clinician. 12 Similarly, one mixed‐methods study of 50 patients with cancer and 50 patients with HF found that patients may recognize the incurable nature of HF even when they lack an understanding of disease trajectory. 32 These findings suggest that prognosis communication involves a complex discussion, which may be difficult for patients to fully understand, especially if it occurs infrequently throughout the disease trajectory.
Patient desire for prognosis communication
Although largely limited to samples consisting of patients in early stages to mid‐stages of HF, research primarily shows that patients want prognosis discussions to occur, despite some variability in patient and caregiver desire for discussions about prognosis, both within and across studies. 17 , 19 , 33 , 34 , 35 One small, qualitative study (n = 25) showed that most patients desired information about their disease, 31 while a cross‐sectional study with a relatively large sample (n = 104) found that over 87% wanted to discuss what to expect in the future concerning HF and over 80% wanted to specifically discuss their prognosis. 19 Although a smaller study (n = 24), other research has similarly shown that over 70% of patients elected to receive their individualized survival estimates even when informed that available models do not provide clear prediction. 33 Yet other studies show more variability within samples. 17 , 35 , 36 One study of 47 hospitalized patients with HF reported that almost half wanted more discussion about prognosis, while more than half wanted information regarding disease self‐management. 36 Similarly, in one small qualitative study (n = 20), some patients expressed a desire for prognosis information, while others preferred not to discuss prognosis. 35 In another cross‐sectional study, 55% of patients with HF and 75% of their caregivers wanted information concerning life expectancy. 17 Understanding patient preferences is further complicated by one qualitative study (n = 20) showing that even when patients express a preference for receiving prognosis information, they can express ambivalence about how much information they want. 23 Furthermore, a qualitative study of 40 patients reported that most preferred to have only a vague understanding of their prognosis, with fewer than 25% specifically asking for prognosis information. 34 These findings provide a window on the individual nature of the HF patient experience.
Benefits and consequences associated with discussions about prognosis
While observational, several studies suggest that there can be important benefits associated with prognosis communication. For example, in a large survey (n = 600), patients who recalled having a prognosis discussion with a clinician endorsed higher satisfaction with decision making, end‐of‐life care, and with communication vs. those who did not recall having these discussions. 21 Additionally, in a small, qualitative study of patients with NYHA Class II–IV HF (n = 24), those who elected to receive life expectancy estimates reported greater clarity and a sense of control and hope, regardless of whether the information received was positive or negative, though in this study, no data were reported for patients who declined this information. 33 Furthermore, in a pilot randomized trial of a palliative care intervention for high‐risk patients with HF (n = 50), those randomized to receive the intervention were more likely to have revised their own prognosis assessment to align with that of their physician, with no adverse effects as reflected by depression, anxiety, or QoL. 37 Overall, these findings suggest that discussions about prognosis specifically can promote a better understanding of HF and facilitate informed decision making and future planning, without compromising QoL.
In contrast, other studies have shown an association between awareness of prognosis or desire for prognosis information and consequences. For example, one small study of hospitalized patients with HF (n = 47) found that those who wanted more discussion about prognosis were more likely to be rehospitalized, 36 while in a larger study (n = 678), patients who expected a deterioration in their health had a lower QoL, were more worried about future health and more unsatisfied, and had more HF readmissions, more days hospitalized due to HF, and a higher mortality, 25 though the expectation of decline and the poorer outcomes may both have been reflective of patients being highly compromised by their disease. Although these studies may suggest that prognosis communication is associated with consequences, it is important to note that prognosis communication was not delivered as part of either study.
Barriers to prognosis communication
Research concerning barriers to prognosis communication includes eight qualitative studies with mostly small samples, 14 , 23 , 38 , 39 , 40 , 41 , 42 , 43 thereby limiting generalization of findings. Despite these limitations, clear themes in patient barriers emerge. Patients with HF who desire prognosis information are unlikely to independently seek it, due in part to fears about what they might learn concerning their future health (according to one small qualitive study, n = 24) 14 but more importantly because of fear that asking for this information might affect their care. 39 In two small qualitative studies, some patients expressed worry about being perceived as bothersome to clinicians 40 or feeling as though their request for information would make their clinician uncomfortable. 23 One qualitative study found that some patients even feel that clinicians may enforce sanctions against them if patients are viewed as difficult. 39 Similarly, in another small qualitative study (n = 43), 41 caregivers and patients described a lack of power in their relationship with clinicians, which reduced their comfort for initiating discussions about prognosis, thereby leaving these conversations for clinicians to initiate.
Clinicians have identified a range of barriers related to both patient characteristics and the nature of HF. For example, one small qualitative study (n = 43) 41 found that clinicians were concerned that cognitive or other sensory impairments could limit a patient's ability to understand the information presented. Additionally, evidence from a large national survey (n = 111) 44 showed that clinicians also expressed concern that prognosis discussions could lead to hopelessness and broader negative effects on patients who specifically may be reluctant to receive any prognosis‐related information. Similarly, clinicians in a large qualitative study (n = 123) 38 expressed concern that these discussions could cause alarm, depression, and anxiety among patients with HF. Furthermore, clinicians have also described a reluctance to discuss prognosis in cases in which a patient has multiple co‐morbidities, and there is a perception that another illness may contribute to the patient's death. 44 Many clinicians are also unclear if prognosis information has previously been communicated, given the number of providers typically involved in HF care. 41 Some describe a lack of time and resources needed to effectively engage in these conversations, 41 , 44 while still others describe a lack of confidence, 24 believing they do not have sufficient skills to engage patients and their caregivers in prognosis discussions. 39 , 42 , 44 This hesitancy is further complicated by the non‐linear nature of the HF disease trajectory 38 , 41 , 44 and the limitations of current predictive models. 10 , 11
One important barrier concerns the imprecision of predictive models in HF, which results in poor to modest prognostication. 11 A prior systematic review concluded that many prediction models were only moderately successful at predicting mortality. 10 Despite these concerns, HF clinicians acknowledge the value of discussions concerning prognosis.
Summary
Of the reviewed studies, the great majority were small and qualitative in nature or used mixed methods, with only one—pilot—randomized, controlled trial. Yet a general lack of communication concerning prognosis and related issues is apparent. Both patient and clinician barriers to this communication are evident and are primarily related to patient reluctance to ask for this information 14 , 23 , 39 , 40 , 41 and clinician ambivalence to engage patients in these discussions, in part, because of limitations in predictive models 11 and the inherent unpredictable disease trajectory of HF. 45 Clinicians also feel unprepared to engage patients 24 , 38 , 39 , 42 , 44 and are worried about negative consequences, including the potential impact on patients' QoL. 39 , 43 , 44 For example, clinicians express concern that patients may become hopeless or depressed if they receive information concerning their prognosis. 38 , 44 Less clear is how to engage patients in prognosis discussions, how to adapt these discussions according to each patient's information preferences, the timing for delivering of this information, and how best to assess the effects of these discussions on the patient. Several key knowledge gaps in HF care emerge. These include (i) how to determine patient readiness and preferences for prognosis information as they progress along the disease trajectory; (ii) what are the best practices for communicating prognosis information; and (iii) what are the effects of prognosis communication on patient QoL, mental health, engagement in critical self‐care, and outcomes.
Discussion
Given the poor discrimination of many prognostic models and the inherent unpredictable disease trajectory of HF, uncertainty in prognostication persists. 46 Although this uncertainty is difficult for patients, caregivers, and clinicians to accept, 47 , 48 experts argue that research on communication concerning prognostic uncertainty is just as important as the development of better prognostic models 48 as prognosis communication will allow patients to more fully engage in their care and in decision making. 49 In Figure 1 , we propose a model of prognosis communication across the HF disease trajectory. This model emphasizes the importance of prognosis communication occurring at critical milestones in a patient's trajectory, including at the time of diagnosis, annually, during episodes of symptom progression (e.g. hospitalization, change from NYHA Class II to III, device implantation or replacement, adjustments to guideline‐directed medical therapy, or device management), and when HF has entered an advanced stage. Although some clinical milestones, such as prior to device implantation or replacement, have long been recognized as necessitating discussion about prognosis, 4 other milestones, such as adjustments to guideline‐directed medical therapy, are more subtle and as a result have often been overlooked. 4 Yet these more subtle milestones must be recognized as critical opportunities to engage patients in their care and thus as opportunities to increase patient knowledge, adherence, and informed decision making. Engaging patients in these iterative conversations is necessary to address the barriers identified by clinicians, including the potential for cognitive impairments to limit patients' ability to understand this information. Furthermore, these conversations provide an opportunity for clinicians to discuss goals of care with patients, such as the potential for disease modification. Given the HF disease trajectory, improvement may not always be a reasonable or attainable goal, despite cardiology's focus on disease improvement. Rather, clinicians may want to consider the importance of disease modification as a motivating factor for engaging patients in their care as their ability to promote disease modification is at least partially under their control and related to adherence to medications as well as to dietary and physical activity recommendations.
Patient‐centric communication guides, such as the ‘Ask‐Tell‐Ask’ model 50 and the ‘Serious Illness Conversation Guide’, 51 may provide a structure for clinicians to engage patients in prognosis communication.
These guides allow clinicians to acknowledge and normalize the uncertainty associated with prognosis discussions in HF care while helping the patient and caregiver manage the uncertainty. 48 The guides also provide recommended communication strategies for an individualized approach to the delivery of health information with a goal of promoting patient engagement in their own care. An essential ingredient in these communication guides is an assessment of patient readiness to receive health information at each clinical encounter, along with an assessment of patient preferences for the types of health information they wish to receive at the encounter. 50 , 51 This encourages the patient to ask questions and discuss care preferences, without having the discussion move beyond what the patient wants or is ready for. It also allows for change over time, as what the patient wants and is ready to discuss changes with the progression of the disease—e.g. as symptom management becomes more difficult and life limiting. 52 Figure 2 provides an overview of prognosis communication at several different points along the disease trajectory, using principles of the ‘Ask‐Tell‐Ask’ model and related communication strategies.
Figure 2.
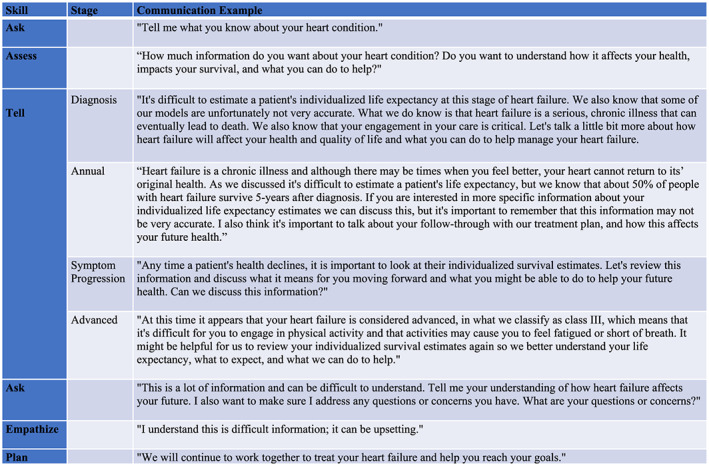
Prognosis communication in heart failure across the disease trajectory.
While these patient‐centred guides provide a framework that holds promise for realizing regular and effective prognosis communication in HF care, the testing of their utilization in clinical trials remains to be realized. The nature of HF care provides a number of obstacles to testing implementation, some of which are based in structural elements of care delivery. Cluster randomization provides one approach to meeting these structural obstacles, leveraging the expansion of healthcare systems composed of multiple hospital and outpatient settings, and the use of quality improvement efforts that test implementation of new care pathways holds promise. Additionally, given the uneven and unpredictable disease trajectory, outcomes in trials that test these guides should perhaps focus initially on whether the communication with the patient is ‘working’—e.g. whether there is consensus between patient and clinician that communication occurred, whether the patient and their caregiver can demonstrate understanding of the communication, and whether the receipt of this communication affects overall adherence, QoL, and satisfaction with care. Additionally, it will be important to test different delivery models—e.g. training of HF staff in a given clinic/hospital setting vs. incorporation of a prognosis communication specialist on the care team. Future research examining prognosis communication will need to address these gaps in the literature.
Furthermore, training of clinicians in patient‐centred communication should be prioritized. Incorporating training in this type of patient‐centred communication for clinicians in medical school and residency as well as requiring continuing medical education in this style of communication would potentially increase the likelihood that clinicians are prepared to engage patients in these types of conversations. Critically, this type of training will need to include interactive components, such as through simulated patients and role‐playing exercises. Training utilizing these methods will better prepare clinicians to engage in patient‐centred communication throughout the HF disease trajectory. Future research will need to examine optimal training methods in patient‐centred communication with a focus on addressing the barriers identified by both patients and clinicians. It will also be important for future research to consider clinicians' training pathways and cultural differences when designing and implementing training in patient‐centred and prognosis communication.
Critically, promoting uptake of prognosis communication will require a shift in the HF model of care, such as a team‐based care programme. Given that HF care, unlike cancer, typically involves a number of clinicians who often operate in silos, HF clinicians often feel unsure if prognosis communication has occurred previously 41 and are hesitant to engage patients in these conversations due to concern about patients' emotional responses to this information. 39 , 43 , 44 Implementing a team‐based care programme would ensure consistency in care and communication, which may help to mitigate any potential negative patient responses and help to identify a primary clinician responsible for engaging patients in these conversations. Furthermore, previous research has shown the effectiveness of team‐based care in reducing hospitalizations and improving functional status as well as QoL. 53 Yet research is needed to examine how prognosis communication can be incorporated into team‐based care programmes and to examine the effects of this communication within these programmes.
Conclusions
While preliminary, research indicates that most patients with HF and their caregivers desire information regarding prognosis and disease trajectory. Yet there are multiple barriers and concerns to conveying this information, and best practices are limited. Moreover, the effects of this information on relevant patient and clinical outcomes are not well studied. Future research will need to investigate how best to engage patients with HF in prognosis communication along the disease trajectory.
Conflict of interest
Dr E.S.S. reports receiving support from the Centers for Medicare and Medicaid Services to develop and maintain performance measures used in public reporting programmes. Dr T.F. reports receiving support from the Claude D. Pepper Older Americans Independence Center at Yale University School of Medicine (P30AG2134). Additionally, Dr L.R. reports receiving support from a grant from the National Heart, Lung, and Blood Institute of the National Institutes of Health (K23HL141644). Dr M.M.B. receives support from the National Heart, Lung, and Blood Institute of the National Institutes of Health (R01HL125587). Drs C.E.C., P.U.G., and R.J.S. report no disclosures. None of the funders had a direct role in the review.
Funding
There were no direct funding sources for this manuscript. Dr. C.E.C's effort was sponspored by HSR&D post‐doctoral fellowship VA Office of Academic Affairs (Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, and Health Services Research and Development #CIN 13‐407).
Author contributions
C.E.C. and M.M.B. contributed to the design conception and drafted the manuscript. All authors performed major revisions to the manuscript.
Cavanagh, C. E. , Rosman, L. , Spatz, E. S. , Fried, T. , Gandhi, P. U. , Soucier, R. J. , and Burg, M. M. (2020) Dying to know: prognosis communication in heart failure. ESC Heart Failure, 7: 3452–3463. 10.1002/ehf2.12941.
References
- 1. Murad K, Goff DC, Morgan TM, Burke GL, Bartz TM, Kizer JR, Chaudhry SI, Gottdiener JS, Kitzman DW. Burden of comorbidities and functional and cognitive impairments in elderly patients at the initial diagnosis of heart failure and their impact on total mortality. JACC Hear Fail 2015; 3: 542–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ahmad T, Pencina MJ, Schulte PJ, O'Brien E, Whellan DJ, Piña IL, Kitzman DW, Lee KL, O'Connor CM, Felker GM. Clinical implications of chronic heart failure phenotypes defined by cluster analysis. J Am Coll Cardiol 2014; 64: 1765–1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, de Ferranti SD, Floyd J, Fornage M, Gillespie C. Heart disease and stroke statistics‐2017 update: a report from the American Heart Association. Circ 2017; 135: e146–e603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Allen LA, Stevenson LW, Grady KL, Goldstein NE, Matlock DD, Arnold RM, Cook NR, Felker GM, Francis GS, Hauptman PJ, Havranek EP, Krumholz HM, Mancini D, Riegel B, Spertus JA, American Heart Association, Council on Quality of Care and Outcomes Research, Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Cardiovascular Radiology and Intervention, Council on Cardiovascular Surgery and Anesthesia . Decision making in advanced heart failure: a scientific statement from the American Heart Association. Circ 2012; 125: 1928–1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Stewart S, MacIntyre K, Hole DJ, Capewell S, McMurray JJV. More ‘malignant’ than cancer? Five‐year survival following a first admission for heart failure. Eur J Heart Fail 2001; 3: 315–322. [DOI] [PubMed] [Google Scholar]
- 6. Stewart S, Ekman I, Ekman T, Odén A, Rosengren A. Population impact of heart failure and the most common forms of cancer. Circ Cardiovasc Qual Outcomes 2010; 3: 573–580. [DOI] [PubMed] [Google Scholar]
- 7. Yancy CW, Januzzi JL, Allen LA, Butler J, Davis LL, Fonarow GC, Ibrahim NE, Jessup M, Lindenfeld J, Maddox TM, Masoudi FA. 2017 ACC expert consensus decision pathway for optimization of heart failure treatment: answers to 10 pivotal issues about heart failure with reduced ejection fraction. J Am Coll Cardiol 2018; 71: 201–230. [DOI] [PubMed] [Google Scholar]
- 8. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, González‐Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 2016; 37: 2129–2200.27206819 [Google Scholar]
- 9. Arnold JMO, Liu P, Demers C, Dorian P, Giannetti N, Haddad H, Heckman GA, Howlett JG, Ignaszewski A, Johnstone DE, Jong P, McKelvie R, Moe GW, Parker JD, Rao V, Ross HJ, Sequeira EJ, Svendsen AM, Teo K, Tsuyuki RT, White M, Canadian Cardiovascular Society . Canadian Cardiovascular Society consensus conference recommendations on heart failure 2006: diagnosis and management. Can J Cardiol 2006; 22: 23–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ouwerkerk W, Voors AA, Zwinderman AH. Factors influencing the predictive power of models for predicting mortality and/or heart failure hospitalization in patients with heart failure. JACC Hear Fail 2014; 2: 429–436. [DOI] [PubMed] [Google Scholar]
- 11. Alba AC, Agoritsas T, Jankowski M, Courvoisier D, Walter SD, Guyatt GH, Ross HJ. Risk prediction models for mortality in ambulatory patients with heart failure. Circ Hear Fail 2013; 6: 881–889. [DOI] [PubMed] [Google Scholar]
- 12. Aldred H, Gott M, Gariballa S. Advanced heart failure: impact on older patients and informal carers. J Adv Nurs 2005; 49: 116–124. [DOI] [PubMed] [Google Scholar]
- 13. Gott M, Small N, Barnes S, Payne S, Seamark D. Older people's views of a good death in heart failure: implications for palliative care provision. Soc Sci Med 2008; 67: 1113–1121. [DOI] [PubMed] [Google Scholar]
- 14. Dougherty CM, Pyper GP, Au DH, Levy WC, Sullivan MD. Drifting in a shrinking future living with advanced heart failure. J Cardiovasc Nurs 2007; 22: 480–487. [DOI] [PubMed] [Google Scholar]
- 15. Gerlich MG, Klindtworth K, Oster P, Pfisterer M, Hager K, Schneider N. ‘Who is going to explain it to me so that I understand?’ Health care needs and experiences of older patients with advanced heart failure. Eur J Ageing 2012; 9: 297–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Murray SA, Boyd K, Kendall M, Worth A, Benton F, Clausen H. Dying of lung cancer or cardiac failure: prospective qualitative interview study of patients and their carers in the community. BMJ 2002; 325: 929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fried TR, Bradley EH, O'Leary J. Prognosis communication in serious illness: perceptions of older patients, caregivers, and clinicians. J Am Geriatr Soc 2003; 51: 1398–1403. [DOI] [PubMed] [Google Scholar]
- 18. Ahluwalia SC, Levin JR, Lorenz KA, Gordon HS. “There's no cure for this condition”: how physicians discuss advance care planning in heart failure. Patient Educ Couns 2013; 91: 200–205. [DOI] [PubMed] [Google Scholar]
- 19. Gordon NA, O'Riordan DL, Dracup KA, De Marco T, Pantilat SZ. Let us talk about It: heart failure patients' preferences toward discussions about prognosis, advance care planning, and spiritual support. J Palliat Med 2017; 20: 79–83. [DOI] [PubMed] [Google Scholar]
- 20. Strachan PH, Ross H, Rocker GM, Dodek PM, Heyland DK. Mind the gap: opportunities for improving end‐of‐life care for patients with advanced heart failure. Can J Cardiol 2009; 25: 635–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Heyland DK, Allan DE, Rocker G, Dodek P, Pichora D. Discussing prognosis with patients and their families near the end of life: impact on satisfaction with end‐of‐life care. Open Med 2009; 3: e101–e110. [PMC free article] [PubMed] [Google Scholar]
- 22. Hjelmfors L, van der Wal MHL, Friedrichsen MJ, Mårtensson J, Strömberg A, Jaarsma T. Patient‑nurse communication about prognosis and end‐of‐life care. J Palliat Med 2015; 18: 865–871. [DOI] [PubMed] [Google Scholar]
- 23. Caldwell PH, Arthur HM, Demers C. Preferences of patients with heart failure for prognosis communication. Can J Cardiol 2007; 23: 791–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Dunlay SM, Foxen JL, Cole T, Feely MA, Loth AR, Strand JJ, Wagner JA, Swetz KM, Redfield MM. A survey of clinician attitudes and self‐reported practices regarding end‐of‐life care in heart failure. Palliat Med 2015; 29: 260–267. [DOI] [PubMed] [Google Scholar]
- 25. van der Wal MHL, Strömberg A, van Veldhuisen DJ, Jaarsma T. Heart failure patients' future expectations and their association with disease severity, quality of life, depressive symptoms and clinical outcomes. Int J Clin Pract 2016; 70: 469–476. [DOI] [PubMed] [Google Scholar]
- 26. Allen LA, Yager JE, Funk MJ, Levy WC, Tulsky JA, Bowers MT, Dodson GC, O'Connor CM, Felker GM. Discordance between patient‐predicted and model‐predicted life expectancy among ambulatory patients with heart failure. JAMA 2008; 299: 2533–2542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Klindtworth K, Oster P, Hager K, Krause O, Bleidorn J, Schneider N. Living with and dying from advanced heart failure: understanding the needs of older patients at the end of life. BMC Geriatr 2015; 15: 125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Willems DL, Hak A, Visser F, Van der Wal G. Thoughts of patients with advanced heart failure on dying. Palliat Med 2004; 18: 564–572. [DOI] [PubMed] [Google Scholar]
- 29. Rogers AE, Addington‐Hall JM, Abery AJ, Mccoy ASM, Bulpitt C, Coats AJS, Gibbs JS. Knowledge and communication difficulties for patients with chronic heart failure: qualitative study. BMJ 2000; 321: 605–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Zapka JG, Carter R, Carter CL, Hennessy W, Kurent JE, DesHarnais S. Care at the end of life. J Aging Health 2006; 18: 791–813. [DOI] [PubMed] [Google Scholar]
- 31. Rodriguez KL, Appelt CJ, Switzer GE, Sonel AF, Arnold RM. “They diagnosed bad heart”: a qualitative exploration of patients' knowledge about and experiences with heart failure. Heart & Lung 2008; 37: 257–265. [DOI] [PubMed] [Google Scholar]
- 32. O'Leary N, Murphy NF, O'Loughlin C, Tiernan E, McDonald K. A comparative study of the palliative care needs of heart failure and cancer patients. Eur J Heart Fail 2009; 11: 406–412. [DOI] [PubMed] [Google Scholar]
- 33. Narayan M, Jones J, Portalupi LB, McIlvennan CK, Matlock DD, Allen LA. Patient perspectives on communication of individualized survival estimates in heart failure. J Card Fail 2017; 23: 272–277. [DOI] [PubMed] [Google Scholar]
- 34. Ågård A, Hermerén G, Herlitz J. When is a patient with heart failure adequately informed? A study of patients' knowledge of and attitudes toward medical information. Heart & Lung 2004; 33: 219–226. [DOI] [PubMed] [Google Scholar]
- 35. Horne G, Payne S. Removing the boundaries: palliative care for patients with heart failure. Palliat Med 2004; 18: 291–296. [DOI] [PubMed] [Google Scholar]
- 36. Howie‐Esquivel J, Dracup K. Communication with hospitalized heart failure patients. Eur J Cardiovasc Nurs 2012; 11: 216–222. [DOI] [PubMed] [Google Scholar]
- 37. O'Donnell AE, Schaefer KG, Stevenson LW, DeVoe K, Walsh K, Mehra MR, Desai AS. Social Worker‐Aided Palliative Care Intervention in High‐risk Patients With Heart Failure (SWAP‐HF). JAMA Cardiol 2018; 3: 516–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Barnes S, Gott M, Payne S, Seamark D, Parker C, Gariballa S, Small N. Communication in heart failure: perspectives from older people and primary care professionals. Heal Soc Care Community 2006; 14: 482–490. [DOI] [PubMed] [Google Scholar]
- 39. Boyd KJ, Murray SA, Kendall M, Worth A, Benton TF, Clausen H. Living with advanced heart failure: a prospective, community based study of patients and their carers. Eur J Heart Fail 2004; 6: 585–591. [DOI] [PubMed] [Google Scholar]
- 40. Hanratty B, Lowson E, Holmes L, Grande G, Jacoby A, Payne S, Seymour J, Whitehead M. Breaking bad news sensitively: what is important to patients in their last year of life? BMJ Support Palliat Care 2012; 2: 24–28. [DOI] [PubMed] [Google Scholar]
- 41. Harding R, Selman L, Beynon T, Hodson F, Coady E, Read C, Walton M, Gibbs L, Higginson IJ. Meeting the communication and information needs of chronic heart failure patients. J Pain Symptom Manage 2008; 36: 149–156. [DOI] [PubMed] [Google Scholar]
- 42. Selman L, Harding R, Beynon T, Hodson F, Coady E, Hazeldine C, Walton M, Gibbs L, Higginson IJ. Improving end‐of‐life care for patients with chronic heart failure: “let's hope it'll get better, when I know in my heart of hearts it won't.”. Heart 2007; 93: 963–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hanratty B, Hibbert D, Mair F, May C, Ward C, Capewell S, Litva A, Corcoran G. Doctors' perceptions of palliative care for heart failure: focus group study. BMJ 2002; 325 :581–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Hjelmfors L, Strömberg A, Friedrichsen M, Mårtensson J, Jaarsma T. Communicating prognosis and end‐of‐life care to heart failure patients: a survey of heart failure nurses' perspectives. Eur J Cardiovasc Nurs 2014; 13: 152–161. [DOI] [PubMed] [Google Scholar]
- 45. Gill TM. The central role of prognosis in clinical decision making. JAMA 2012; 307: 199–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Yourman LC, Lee SJ, Schonberg MA, Widera EW, Smith AK. Prognostic indices for older adults. JAMA 2012; 307: 182–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Drazen JM, Yialamas MA. Certain about dying with uncertainty. N Engl J Med 2017; 377: 208–209. [DOI] [PubMed] [Google Scholar]
- 48. Smith AK, White DB, Arnold RM. Uncertainty—the other side of prognosis. N Engl J Med 2013; 368: 2448–2450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Simpkin AL, Schwartzstein RM. Tolerating uncertainty—the next medical revolution? N Engl J Med 2016; 375: 1713–1715. [DOI] [PubMed] [Google Scholar]
- 50. Goodlin SJ, Quill TE, Arnold RM. Communication and decision‐making about prognosis in heart failure care. J Card Fail 2008; 14: 106–113. [DOI] [PubMed] [Google Scholar]
- 51. Bernacki R, Hutchings M, Vick J, Smith G, Paladino J, Lipsitz S, Gawande AA, Block SD. Development of the Serious Illness Care Program: a randomised controlled trial of a palliative care communication intervention. BMJ Open 2015; 5: e009032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Schoenborn NL, Janssen EM, Boyd C, Bridges JFP, Wolff AC, Xue Q‐L, Pollack CE. Older adults' preferences for discussing Long‐term life expectancy: results from a national survey. Ann Fam Med 2018; 16: 530–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Creaser JW, DePasquale EC, Vandenbogaart E, Rourke D, Chaker T, Fonarow GC. Team‐based care for outpatients with heart failure. Heart Fail Clin 2015; 11: 379–405. [DOI] [PubMed] [Google Scholar]


