Abstract
Aims
Baduanjin (eight silken movements), a traditional Chinese exercise, is an alternative to the most common cardiac rehabilitation programmes due to their scarcity and unaffordability in China. The aim of this study was to measure the intensity and energy expenditure during Baduanjin and to determine the relative oxygen consumption (VO2) and heart rate (HR) responses of Baduanjin compared with maximal capacity in patients with chronic heart failure.
Methods and results
Twenty participants (age: 65 ± 10 years, male: n = 17) with New York Heart Association II–III volunteered for this study. Participants were examined during two separate sessions, with 1–2 weeks between sessions. During session one, a symptom‐limited cardiopulmonary exercise testing was performed on a cycle ergometer for measurement of maximal exercise capacity. Additionally, participants were taught Baduanjin exercise from a professional coach and were required to do it at home until the second session when their technique was confirmed by the coach. During session two, participants performed one 9 min round of Baduanjin with continuous measurement of VO2 and HR. Measurements obtained during the Baduanjin were compared with data obtained during cardiopulmonary exercise testing. While performing Baduanjin, the mean VO2 and HR were 7.1 ± 1.2 mL/kg/min and 86.1 ± 15.2 b.p.m., respectively. Compared with the cardiopulmonary exercise test, the VO2 was 44% of their VO2max and 67% of their HRmax, categorizing Baduanjin as a moderate‐intensity exercise. The average energy expenditure during Baduanjin was 23.3 ± 4.4 kcal. Additionally, the VO2 and HR responses during Baduanjin both exhibited a bimodal pattern.
Conclusions
The results suggest that Baduanjin is a moderate‐intensity aerobic exercise that could be an effective and safe exercise modality for home‐based cardiac rehabilitation.
Keywords: Baduanjin, Chronic heart failure, Exercise intensity, Oxygen consumption, Heart rate
Introduction
Baduanjin, translated as eight silken movements, is one of the most common forms of Qigong exercise. 1 Qigong is an ancient martial art, and it covers a spectrum of exercises: Daoyinshu (physical and breathing exercises), Wuqinxi (five animals play), Baduanjin (eight silken movements), Yijinjing (changing tendons exercises), and Tai Chi. Although each type of Qigong exercise uses different practice postures or techniques of its own, they all share a unique methodology and theoretical system adopting key ideas of classical Chinese philosophy. 2 Commonly regarded as beneficial to health, 3 , 4 Baduanjin have been practiced for over 1000 years, and now, it is a community exercise throughout mainland China.
Baduanjin is easy to learn, with minimal physical or cognitive demands, as it only entails eight simple movements based on traditional Chinese medicine theory. Moreover, it is an adaptable form of exercise that can be practiced at any place, any time, and without special equipment and minimal time investment. Hence, it is easily incorporated into daily routines and could easily be integrated into a comprehensive cardiac rehabilitation programme.
Baduanjin is characterized by slow movements (physical training) synchronized with meditation (mindfulness‐based training) and regulated breathing (respiratory training) to achieve a harmonious flow of energy (qi) in the body. 4 From the perspective of Western thought and exercise science, Baduanjin is usually referred to as a light‐intensity exercise, regardless of the individual's fitness level. However, for particularly deconditioned patients such as those with chronic heart failure (CHF), it may be considered a moderate‐intensity or even high‐intensity aerobic exercise depending on their age and exercise capacity. 5
In clinical settings, the F.I.T.T. principle describes the four components of exercise prescription: frequency, intensity, time (duration), and type of exercise, which constitute the exercise ‘dose’. Of these, exercise intensity is arguably the most critical component for cardiorespiratory fitness. 6 The gold standard for determining exercise intensity is the measurement of oxygen consumption (VO2). 5 To date, however, there is a lack of evidence on intensity levels for Baduanjin among CHF patients. In addition, no published studies have reported cardiopulmonary responses, such as VO2, heart rate (HR), and other important parameters, during Baduanjin practice among patients with CHF. This shortcoming may exclude Baduanjin from the clinician's toolbox and incorporation into clinical practice. Therefore, the purpose of this study was to (i) measure the intensity and energy expenditure during Baduanjin and (ii) determine the relative cardiopulmonary response of Baduanjin compared with maximal capacity in patients with CHF.
Methods
Participants
This study was conducted as part of a project entitled the ‘BESMILE‐HF study’ testing the efficacy and safety of Baduanjin. 7 The primary study is a randomized controlled trial where data on participants' maximal exercise capacities and cardiopulmonary responses during Baduanjin were collected at baseline. In the present study, individuals were included if they had data for the maximal exercise test and the Baduanjin intensity test. 8 , 9 The study was conducted in accordance with the Declaration of Helsinki, and the BESMILE‐HF study has been approved by the Ethics Committee of the Guangdong Provincial Hospital of Chinese Medicine (number: B2016–202‐01). Study procedures were explained in full to all participants, and written informed consent was obtained.
Data collection
Procedures, equipment, and requirements
Each participant came to the hospital on two separate sessions. During the first session, a maximal exercise test was conducted to determine individual maximal exercise capacity. On the same day, participants were required to learn how to practice Baduanjin until they had mastered it. The standing form of Baduanjin from China's General Administration of Sport 10 was used in this study. It has been standardized as a set of eight sequential movements for limbs, body trunk, and eye movements (Figure 1 ). One professional coach with over 5 years of teaching experience taught and confirmed participants' technique. Patients were then required to practice on their own at home for 1–2 weeks following the instructions of a video with verbal hints. Therefore, a period of at least 7 days separated the two visits, and all experimental procedures were completed within 2 weeks. On the second visit, a Baduanjin intensity test evaluated the cardiopulmonary responses during Baduanjin.
Figure 1.
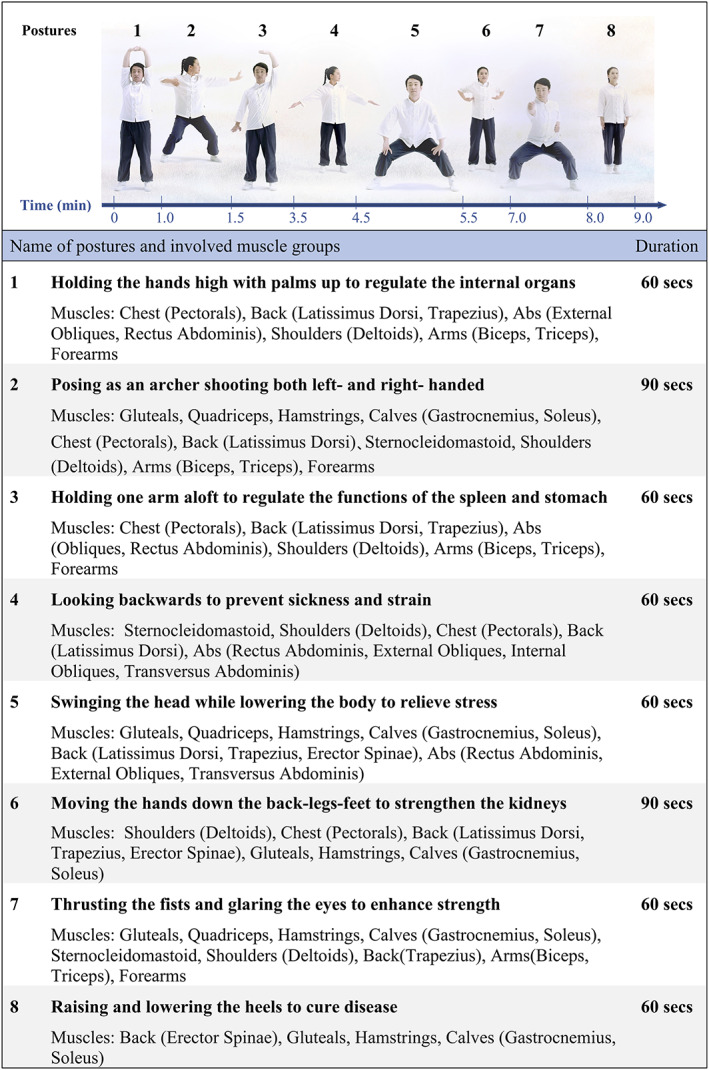
A 9 min Baduanjin exercise training session, including eight postures, involved muscle groups, and their corresponding durations.
An ergospirometry platform (CARDIOVIT, CS‐200; SCHILLER, Baar, Zug, Switzerland) was used for all tests. Respiratory gas analysis was performed on a breath‐by‐breath basis with a metabolic cart (PowerCube; Ganshorn, Niederlauer,Germany) and LF8 software (CARDIOVIT, CS‐200 ergospirometry; SCHILLER). The maximal exercise test used an electronically calibrated upright bicycle (ERG 911S; SCHILLER). All tests were conducted in an air‐conditioned laboratory with a temperature of 20–23°C, barometric pressure of 994–1042 mmHg, and relative humidity of 50–65%. Before each test, the gas analyser was calibrated with gases of a known concentration [15% of oxygen (O2) and 6% of carbon dioxide (CO2)], and the flow metre was calibrated with a 3 L calibration syringe (SCHILLER).
The experiments were carried out in both morning and afternoon. However, for each participant, the maximal exercise test and Baduanjin test were conducted at the same time of the day. All tests were conducted by the same examiner to avoid inter‐examiner variability. The examiner was both trained in and experienced with the tools. All participants were instructed to refrain from eating 2 h before these two visits and to abstain from caffeine, alcohol, and strenuous physical activity on each test day. Water intake was allowed.
Maximal exercise test
Prior to the maximal exercise test, spirometry was conducted according to the American Thoracic Society and European Respiratory Society. 11 Participants were then instructed to lie down and rest in a supine position for 30–40 min before the maximal exercise test. Meanwhile, all subjects read a standardized script of the testing procedures and received an explanation of the Borg 6–20 Rating of Perceived Exertion Scale.
On completion of these preliminary procedures, the maximum exercise test was conducted according to the American Thoracic Society/American College of Chest Physicians Statement on Cardiopulmonary Exercise Testing. 12 This was a symptom‐limited exercise test using a bicycle ramp protocol: initial work rate of 0 W with 10% predicted maximum work rate increments every minute. Participants were verbally encouraged to maintain the desired pedal rate of 60 rpms and to exercise until exhaustion or fatigue. However, the examiner would stop the test according to the established criteria. 13 Perceived exertion was measured using the 6–20 Borg Scale (every 2–3 min) throughout the test.
The exercise test time ranged from 8 to 12 min. HR and rhythm were continuously monitored by 12 lead electrocardiogram. Peripheral oxygen saturation was continuously monitored, and blood pressure was measured at rest and every 3 min until test termination. The following data were collected automatically from the system for each participant (averaged over 10 s): HR (b.p.m.), VO2 (mL/kg/min), carbon dioxide production (VCO2, L/min), respiratory rate (brpm), minute ventilation (VE, L/min), end‐tidal carbon dioxide partial pressure (PETCO2, mmHg), ventilatory equivalents for carbon dioxide (VE/VCO2 slope), and the ratio of VO2 change to work rate change (∆VO2/∆WR). The ventilatory threshold was assessed by the examiner and confirmed by an independent examiner using established criteria. 13 Both of them were experienced and certified physicians who received training before entering the study. If agreement could not be reached, a third physician was to be invited to discuss, and the final ventilatory threshold was determined by consensus.
Baduanjin intensity test
Baduanjin intensity test was conducted on the second visit. Prior to the test, all subjects were instructed to lie down and rest in a supine position for 30 min.
During the test, participants were required to practice one round of Baduanjin lasting 9 min under the instruction of a video with verbal hints on technique to ensure that the same posture, pace, and sequence were followed. A 3 min and a 2 min breathing adjustment before and after practice was also included in the test. Thus, the total test time was 14 min.
The VO2 and VCO2 were measured simultaneously while breathing room air through a face mask covering the nose and mouth. Inhaled and exhaled gases were analysed in real time with a metabolic cart. HR, rhythm, and peripheral O2 saturation were continuously monitored. The same cardiopulmonary data as was collected during the maximal cardiopulmonary exercise test were collected automatically from the system for each participant and averaged over 10 s. Blood pressure was measured at rest and every 3 min until test termination.
Statistical analysis
Data from the maximal exercise test and the average cardiorespiratory parameters obtained during Baduanjin were summarized as mean and standard deviation (SD). The mean VO2 and HR collected during Baduanjin were compared with individual maximal exercise capacity as determined by the cardiopulmonary exercise test and reported as a percentage (expressed as %VO2max and %HRmax). In order to categorize the Baduanjin exercise intensity, we referred to a position statement on exercise intensity terminology. 5 This position statement proposes the use of five categories to reflect clusters of activities that place similar relative physiological stress (within a category) on the exercising individual. The descriptors and cut‐offs for the five categories based on %VO2max and %HRmax were (i) ‘sedentary’: <20% VO2max or <40% HRmax; (ii) ‘light’: 20 < 40% VO2max or 40 < 55% HRmax; (iii) ‘moderate’: 40 < 60% VO2max or 55 < 70% HRmax; (iv) ‘vigorous’: 60 < 85% VO2max or 70 < 90% HRmax; and (v) ‘high’: ≥85% VO2max or ≥90% HRmax. Moreover, in order to explore the cardiopulmonary response patterns throughout the session, all cardiopulmonary parameters, including VO2, HR, blood pressure, O2 pulse, VE, respiratory rate, and the PETCO2, were summarized at 10 s intervals as mean ± SD and plotted over time. No power calculation has been done because only descriptive data and no inferential statistics were provided in this study. All statistical procedures were performed with SPSS (version 18.0, Chicago, IL, USA).
Results
Participants (n = 20, 17 male and 3 female, ages 65 ± 10 years) had a clinical history of heart failure for 4 ± 3.5 years and classified as either New York Heart Association (NYHA) II (n = 17) or NYHA III (n = 3). The mean left ventricular ejection fraction (LVEF) was 46.7 ± 12.1%, and they were either with reduced LVEF (heart failure with reduced ejection fraction, n = 6), perceived LVEF (heart failure with perceived ejection fraction, n = 8), or middle ranged LVEF (heart failure with middle ranged ejection fraction, n = 6). In addition, 75% of participants (n = 15) had been taking beta‐blockers. Details of demographic and anthropometrical characteristics, medical history, heart failure status, and co‐morbidities are presented in Table 1 .
TABLE 1.
Participants' demographic and anthropometrical characteristics, heart failure status, and co‐morbidities (n = 20)
| Characteristic | Mean ± SD or number (%) |
|---|---|
| Demographic and anthropometrical characteristics | |
| Male | 17 (85) |
| Age, years | 64.6 ± 9.9 |
| BMI | 24.5 ± 3.6 |
| Weight, kg | 67.5 ± 11.5 |
| Smokers | 12 (60) |
| Heart failure characteristics | |
| Heart failure history, years | 3.8 ± 3.5 |
| NYHA classification | |
| NYHA II | 17 (85) |
| NYHA III | 3 (15) |
| LVEF classification | |
| HFrEF | 6 (30) |
| HFmrEF | 6 (30) |
| HFpEF | 8 (40) |
| HR, b.p.m. | 78 ± 14 |
| SBP, mmHg | 134 ± 17 |
| DBP, mmHg | 79 ± 12 |
| NT‐proBNP, pg/mL | 1116.2 ± 2335.8 |
| LVEF (Simpson), % | 46.7 ± 12.1 |
| PASP, mmHg | 27.1 ± 7.0 |
| Beta‐blocker users | 15 (75) |
| Co‐morbidities | |
| Coronary heart disease | 15 (75) |
| Previous myocardial infarction | 7 (35) |
| Atrial fibrillation | 4 (20) |
| Hypertension | 10 (50) |
| Type 2 diabetes | 6 (30) |
| Hyperlipidaemia | 8 (40) |
| Chronic kidney disease | 2 (10) |
| Stroke | 3 (15) |
| Peripheral vascular disease | 12 (60) |
BMI, body mass index; b.p.m., beats per minute; DBP, diastolic blood pressure; HFmrEF, heart failure with middle ranged ejection fraction; HFpEF, heart failure with perceived ejection fraction; HFrEF, heart failure with reduced ejection fraction; HR, heart rate; LVEF, left ventricular ejection fraction; NT‐proBNP, N‐terminal B‐type natriuretic peptide; NYHA, New York Heart Association; PASP, pulmonary artery systolic pressure; SBP, systolic blood pressure; SD, standard deviation.
Results of the maximum exercise test are shown in Table 2 . Nineteen out of 20 participants attained respiratory exchange ratio > 1.1, with the other participant achieving a respiratory exchange ratio of 0.97 due to symptom limitation. All of the participants stopped the test due to leg fatigue. Ventilatory threshold was detected in all cases. Participants had an impaired exercise capacity with a mean VO2max of 17.6 ± 4.9 mL/kg/min, corresponding with a mean HRmax of 131.6 ± 18.0 b.p.m. Participants also demonstrated an elevated VE/VCO2 slope (34.0 ± 8.4) and impaired aerobic efficiency measured by the ∆VO2/∆WR ratio (10.3 ± 2.1). Spirometry showed that 55% (n = 11) of participants had normal lung function, and 30% (n = 6) and 15% (n = 3) demonstrated restrictive and obstructive patterns, respectively.
TABLE 2.
Cardiorespiratory parameters obtained by maximal exercise test at the ventilatory threshold and at the maximal threshold from 20 participants with chronic heart failure
| Ventilatory threshold | Maximal intensity | |
|---|---|---|
| Mean ± SD | Mean ± SD | |
| RER | 1.3 ± 1.8 | 1.2 ± 0.1 |
| WR (W) | 54.9 ± 22.5 | 93.1 ± 33.3 |
| VO2/kg (mL/kg/min) | 11.9 ± 2.7 | 17.6 ± 4.9 |
| HR (b.p.m.) | 101.6 ± 17.0 | 131.6 ± 18.0 |
| METs | 3.4 ± 0.8 | 5.0 ± 1.4 |
| SBP (mmHg) | 151.3 ± 25.6 | 176.2 ± 31.4 |
| DBP (mmHg) | 85.7 ± 13.4 | 109.9 ± 69.6 |
| O2 pulse (mL/beat) | 8.1 ± 2.5 | 9.2 ± 3.2 |
| RR (breathes/min) | 25 ± 5 | 33.5 ± 4.9 |
| VE (L/min) | 26.5 ± 4.6 | 50.1 ± 12.3 |
| PETCO2 (mmHg) | 34.9 ± 5.4 | 32.6 ± 7.4 |
b.p.m., beats per minute; DBP, diastolic blood pressure; HR, heart rate; METs, metabolic equivalents; O2 pulse, oxygen pulse (the ratio of oxygen consumption to heart rate); PETCO2, end‐tidal carbon dioxide partial pressure; RER, respiratory exchange ratio; RR, respiratory rate; SBP, systolic blood pressure; SD, standard deviation; VE, minute ventilation;VO2, oxygen consumption; WR, work rate.
The exercise intensity and energy expenditure for all 20 participants during Baduanjin are shown in Table 3 . During Baduanjin, the mean VO2 was 7.1 ± 1.2 mL/kg/min, 44% of VO2max (SD: 18%), categorizing Baduanjin as a moderate‐intensity exercise (40–60% of VO2max). 5 The mean HR was 86.1 ± 15.2 b.p.m., which was 67% of HRmax (SD: 12%). This also categorized Baduanjin as a moderate‐intensity exercise (55–70% of HRmax). 5 However, the mean metabolic equivalent (MET) (2.0 ± 0.4 METs) categorized Baduanjin as a light‐intensity aerobic exercise (1.6–3 METs). 5 The mean energy expenditure was 155.4 ± 29.6 kcal/h. Therefore, average energy expenditure was estimated to be 23.3 ± 4.4 kcal for one 9 min Baduanjin session.
TABLE 3.
Cardiorespiratory parameters obtained during Baduanjin from 20 participants
| Mean ± SD | Range | |
|---|---|---|
| VO2/kg (mL/kg/min) | 7.1 ± 1.2 | (4–9) |
| VO2/VO2max (%) | 44 ± 18 | (21–82) |
| HR (b.p.m.) | 86.1 ± 15.2 | (64–120) |
| HR/HRmax (%) | 67 ± 12 | (54–105) |
| METs | 2.0 ± 0.4 | (1–3) |
| EE (kcal/h) | 155.4 ± 29.6 | (101–211) |
| SBP (mmHg) | 155 ± 22 | (114–200) |
| DBP (mmHg) | 92 ± 13 | (71–119) |
| O2 pulse (mL/beat) | 5.7 ± 1.5 | (3–9) |
| RR (brpm) | 19.8 ± 3.6 | (13–27) |
| VE (L/min) | 15.9 ± 3.8 | (9–23) |
| PETCO2 (mmHg) | 31.1 ± 3.2 | (25–36) |
b.p.m., beats per minute; brpm, breathes per minute; DBP, diastolic blood pressure; EE, energy expenditure; HR, heart rate; METS, metabolic equivalents; O2 pulse, oxygen pulse (the ratio of oxygen consumption to heart rate); PETCO2, end‐tidal carbon dioxide partial pressure; RR, respiratory rate; SBP, systolic blood pressure; SD, standard deviation; VO2, oxygen consumption; VO2max, maximum oxygen consumption; VE, minute ventilation.
The VO2 responses exhibited a bimodal distribution during Baduanjin (Figure 2 ). The VO2 increased from 3.8 (23%VO2max) to 7.5 mL/kg/min (47%VO2max) during the first 3 min when a hemi‐squat posture was involved (second posture), followed by a small drop in VO2 after transition to the third posture. The intensity reached the second peak of 8.5 mL/kg/min (54%VO2max) at the 7th minute during an additional two hemi‐squat postures (5th and 7th). It then dropped to 7.4 mL/kg/min (47%VO2max) at the end of the session (9th minute). Overall, the absolute VO2 response remained under the ventilatory threshold (Figure 2 A ), and the %VO2max response indicating exercise intensity line remained mostly within the moderate‐intensity area (Figure 2 B ).
Figure 2.
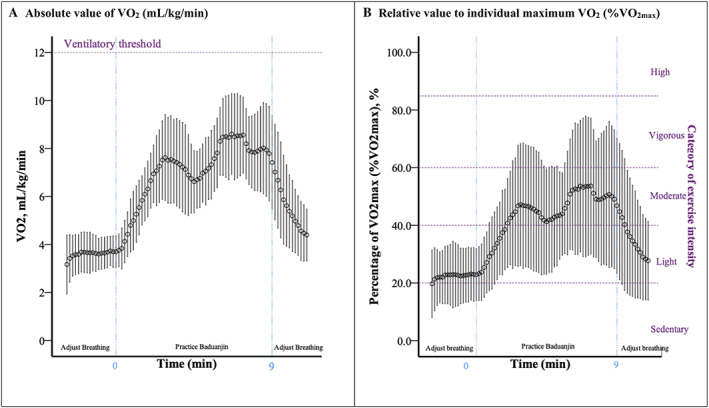
Mean oxygen consumption (VO2, mL/kg/min) response during a 9 min Baduanjin session with a 3 min and a 2 min breathing adjustment before and after practice with chronic heart failure (n = 20). During Baduanjin, the mean VO2 was 7.1 ± 1.2 mL/kg/min, 44% of VO2max (SD: 18%), categorizing Baduanjin as a moderate‐intensity exercise (40–60% of VO2max). The VO2 responses exhibit a bimodal distribution during Baduanjin. Overall, (A) the absolute VO2 response remained under the ventilatory threshold and (B) the %VO2max response indicating exercise intensity line remained mostly within the moderate‐intensity area.
Similar to the VO2 response, the HR response also exhibited a bimodal distribution with smaller magnitudes during Baduanjin (Figure 3 ). The HR increased from 76 (59% HRmax) to 89 b.p.m. (69% HRmax) with a small drop soon after; it then increased again to 95 b.p.m. (74% HRmax) with a small drop to 84 b.p.m. (64% HRmax) at the end of Baduanjin. Overall, the absolute HR response line remained under the equivalent HR for ventilatory threshold (Figure 3 A ), and the %HRmax response line remained within the moderate‐intensity area (Figure 3 B ).
Figure 3.
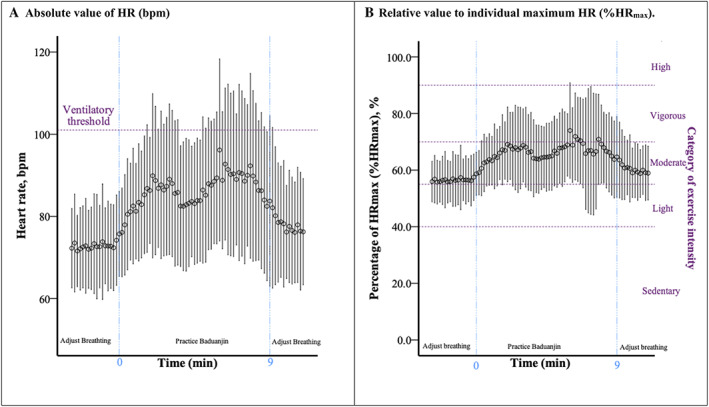
Mean heart rate (HR) response during a 9 min Baduanjin session with a 3 min and a 2 min breathing adjustment before and after practice in patients with chronic heart failure (n = 20). During Baduanjin, the mean HR was 86.1 ± 15.2 b.p.m., which was 67% of HRmax (SD: 12%), categorizing Baduanjin as a moderate‐intensity exercise (55–70% of HRmax). Similar to the VO2 response lines, the HR response also exhibited a bimodal distribution with smaller magnitudes during Baduanjin. Overall, (A) the absolute HR response line remained under the equivalent HR at ventilatory threshold and (B) the %HRmax response line remained within the moderate‐intensity area.
Figure 4 shows the participants ventilatory responses including respiratory rate (Figure 4 A ), VE (Figure 4 B ), and PETCO2 (Figure 4 C ) during Baduanjin. The ventilatory responses demonstrated a pattern similar to VO2 and HR.
Figure 4.
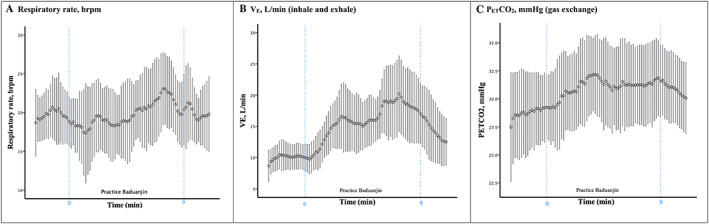
Pulmonary responses during a 9 min Baduanjin session with a 3 min and a 2 min breathing adjustment before and after practice in patients with chronic heart failure (n = 20). (A) respiratiory rate, (B) VE, (C) PETCO2.The ventilatory responses demonstrated a pattern similar to VO2 and HR. SD, standard deviation; brpm, breathes per minute; VE, minute ventilation; PETCO2, end‐tidal carbon dioxide partial pressure (mmHg), indicating gas exchange.
Discussion
This is the first study to investigate Baduanjin intensity based on VO2 and HR, as well as cardiopulmonary responses during Baduanjin among CHF patients. Our results suggest that Baduanjin's moderate intensity makes it suitable for improving exercise capacity in CHF patients. In addition, the VO2 and HR responses both exhibited a bimodal pattern during the exercise session. Further, the average energy expenditure was estimated as 23.3 kcal for a 9 min Baduanjin session. Our findings on Baduanjin intensity are strengthened by comparison with maximal cardiopulmonary exercise testing (%VO2max and %HRmax responses). In this light, exercise intensity can be expressed as either an absolute, for example, HR or MET, or as a relative measure, such as %VO2max or %HRmax, allowing for comparison with other forms of exercise. A challenge when categorizing exercise intensity using absolute measurements is inter‐individual variability with regard to functional capacity. Compared with those who are physically healthy and of similar age, 3 our participants demonstrate an impaired exercise capacity measured by the gold standard VO2max (17.6 ± 5 mL/kg/min). Hence, the intensity of one exercise may differ across the population and may exceed the capabilities of some individuals. 5 In our study, the individual absolute intensity was 2.0 ± 0.4 METs (ranging from 1 to 3 METs). This categorized Baduanjin exercise as a light‐intensity activity (1.6–3 METs) if it is practiced by healthy individuals. However, both measures of relative intensity as measured in this study, %VO2max and %HRmax, categorize Baduanjin as a moderate‐intensity exercise. Moreover, both of the response lines were mostly located within the recommended moderate‐intensity zones. Therefore, we believe that continuous monitoring of %VO2max and %HRmax responses is an appropriate way to provide a composite gauge of exercise intensity, with priority given to %VO2max due to HR modulating impact of pharmacotherapies often prescribed for CHF patients (e.g. beta‐blockers).
Our findings provide further evidence that Baduanjin's eight simple postures are not only accessible and learner‐friendly but also suitable in terms of their exercise intensity for CHF patients. Firstly, the Baduanjin training intensity fulfilled American College of Sports Medicine's recommendations to stimulate the body, causing physiologically oriented outcomes. 6 It has been recommended that the exercise intensity should be set at 40–50% of VO2max or 50–60% of HRmax at the starting point when initiating an exercise‐based rehabilitation programme for CHF patients. 14 , 15 Moreover, Baduanjin intensity level is similar to that of general exercises that are used in rehabilitation programmes for CHF. A recently published Cochrane Systematic Review of exercise‐based cardiac rehabilitation (EBCR) for heart failure shows that most EBCR programmes use moderate‐intensity training at 40–80% of HRmax or 50–85% of VO2max. 16 Therefore, the benefits of exercise capacity should be expected from continuous practice, and previous studies have reported that Baduanjin improves exercise capacity. 17 , 18 , 19 , 20 , 21 , 22
Secondly, Baduanjin is a safe exercise for CHF patients, which can be practiced in a home‐based setting. Both Baduanjin's averaged and instant intensity levels are under or close to the ventialtory threshold, which fulfil the requirement of current clinical practice guidelines. It has also been proposed to be particularly suitable for elderly individuals and thus relevant for patients with CHF who are often older. 23 , 24 In addition, patients with CHF typically demonstrate an excessive ventilatory response to exercise. 25 In the present study, steady exercise‐induced respiratory rates were observed during Baduanjin. The key element of Baduanjin, mindful breathing, emphasizes the coordination of breathing and physical movements, relaxation, focused self‐awareness, and imagery. This decreases cardiac sympathovagal tone and ventricular workload, 26 decreasing the training burden on patients. Therefore, the likelihood of significant adverse arrhythmia, ischaemia, and/or other adverse cardiovascular events is proportionally reduced.
Thirdly, Baduanjin could facilitate initiation of exercise, long‐term exercise adoption, and maintenance. Our results show that the average VO2 during Baduanjin was 44% of participants VO2max, and the average HR was 67% of subject's HRmax. Moreover, a bimodal pattern response related to semi‐squat postures was observed for VO2 and HR. These findings indicate that patients can achieve a suitable level of intensity during training by adjusting their postures, such as modifying the height of the semi‐squat posture. Prior studies have shown that exercise efficacy is more likely to be achieved with a regimen that can provide effective low‐intensity options, particularly as exercise is initiated, but that can also intensify as tolerated or facilitate intermittent intervals of higher intensity. 23 , 27 , 28 In this respect, Baduanjin, which is inherently less strenuous but easily modified to tailor intensity, may address tolerability and accessibility.
Our findings regarding the energy expenditure have implication for the personalization and standardization of exercise‐based rehabilitation programmes using Baduanjin for CHF patients. A meta‐regression analysis reports that the total energy expenditure (product of training intensity, session duration, session frequency, and programme length) of a training programme appears to be the only training characteristic with a significant effect on exercise capacity. 29 This study reported a clinical importance improvement in peak VO2 of 1 mL/kg/min with each 80 kcal/kg increase in total energy expenditure. Together with our finding that energy expenditure averaged 23.3 kcal for one 9 min Baduanjin session, a personalized and goal‐oriented Baduanjin exercise prescription can be made. For example, if a patient weighing 50 kg wants to increase 1 mL/min/kg after a 12 week Baduanjin exercise programme, this means the patient would need a total energy expenditure of 40 000 kcal (80 kcal/kg * 50 kg). This would require at least 172 sessions (4000 kcal/23.3 kcal per session) of Baduanjin in total or ~2 daily sessions over 12 weeks to reach the goal.
As with all studies, there are potential limitations to note. Firstly, the interpretability and generalizability of the results were limited by the clinical characteristics of the analysed population. Our study population only included NYHA II and III CHF patients who are young and suffer from heart failure of mild severity. Therefore, our findings are specific to the population studied. Secondly, our population was relatively homogenous and had limited female participation. Additional studies focused on enrollment of female participants is encouraged. Thirdly, all participants in our study were new to Baduanjin, enabling a similar skill level among participants of varying skill levels. However, whether intensity and cardiopulmonary responses vary among those who are more skilful is unknown. Therefore, future research is needed, with greater heterogeneity of skill levels to investigate the cardiopulmonary responses of Baduanjin in CHF patients and to explore how Baduanjin characteristics, such as the postures, practice sessions, or practice skills, influence intensity and cardiopulmumonary responses. Lastly, it is difficult to render the studies replicable because Baduanjin coaches are not available in all parts of the world. However, with the proliferation of social media, tutorial videos produced by our research team are easy to find online, 30 , 31 and the certified version from China's General Administration of Sport is also available in English. 32 Hence, our study can serve as a skeleton for future studies, which explore the cardiopulmonary responses of Baduanjin or other similar exercises among different races and ethnicities.
Conclusions
Our findings show that Baduanjin is a moderate‐intensity aerobic exercise without excessive cardiopulmonary burden. Considering its advantages of being learner‐friendly and flexible in terms of time commitment and space requirements, Baduanjin could be an effective and safe exercise modality for inclusion in cardiac rehabilitation programmes for CHF patients, especially in home‐based settings.
Conflict of interest
None declared.
Funding
This work was supported by the General Research Fund of Traditional Chinese Medicine Science and Technology from Guangdong Provincial Hospital of Chinese Medicine (YN2018ML02), the Clinical Research Funding of Traditional Chinese Medicine Science and Technology (Project 1010) from Guangdong Provincial Hospital of Chinese Medicine (YN10101910), and the China Scholarship Council (201608440264).
Author contributions
X.C., W.L., and W.J. contributed to the conception and design of the research. W.L. contributed to obtaining funding and supervising the work. X.C. contributed to drafting the manuscript. All authors contributed important intellectual content to the critical revision of the manuscript. All authors read and approved the final manuscript.
Acknowledgements
The authors wish to thank the professional coach (Haojian Yu) from the Department of Cardiology of Guangdong Provincial Hospital of Chinese Medicine for teaching Baduanjin and three research assistants, Yunxiang Fan, Meifen Zhang, and Qinyuan Su, from the Department of Cardiology of Guangdong Provincial Hospital of Chinese Medicine and Shaojun Liao from the Guangzhou University of Traditional Chinese Medicine for assistance with collecting the data.
Chen, X. , Marrone, G. , Olson, T. P. , Lundborg, C. S. , Zhu, H. , Wen, Z. , Lu, W. , and Jiang, W. (2020) Intensity level and cardiorespiratory responses to Baduanjin exercise in patients with chronic heart failure. ESC Heart Failure, 7: 3782–3791. 10.1002/ehf2.12959.
Contributor Information
Weihui Lu, Email: weihui.lu@163.com.
Wei Jiang, Email: drjiangwei@126.com.
References
- 1. Koh TC. Baduanjin—an ancient Chinese exercise. Am J Chin Med 1982; 10: 14–21. [DOI] [PubMed] [Google Scholar]
- 2. Qu J, Wang X. Traditional Chinese Exercises. Newcastle‐upon‐Tyne: Cambridge Scholars Publishing; 2015. [Google Scholar]
- 3. Li R, Jin L, Hong P, He ZH, Huang CY, Zhao JX, Wang M, Tian Y. The effect of Baduanjin on promoting the physical fitness and health of adults. Evid Based Complement Alternat Med 2014; 2014: 784059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zou L, SasaKi JE, Wang H, Xiao Z, Fang Q, Zhang M. A systematic review and meta‐analysis Baduanjin Qigong for health benefits: randomized controlled trials. Evid Based Complement Alternat Med 2017; 2017: 4548706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Norton K, Norton L, Sadgrove D. Position statement on physical activity and exercise intensity terminology. J Sci Med Sport 2010; 13: 496–502. [DOI] [PubMed] [Google Scholar]
- 6. American College of Sports Medicine . In Riebe D, Ehrman JK, Liguori G, Magal M, eds. ACSM's Guidelines for Exercise Testing and Prescription, 10th ed. United States, Philadelphia, PA: Wolters Kluwer; 2017. [Google Scholar]
- 7. Chen X, Jiang W, Lin X, Lundborg CS, Wen Z, Lu W, Marrone G. Effect of an exercise‐based cardiac rehabilitation program “Baduanjin Eight‐Silken‐Movements with self‐efficacy building” for heart failure (BESMILE‐HF study): study protocol for a randomized controlled trial. Trials 2018; 19: 150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lan C, Chen SY, Lai JS, Wong MK. Heart rate responses and oxygen consumption during Tai Chi Chuan practice. Am J Chin Med 2001; 29: 403–410. [DOI] [PubMed] [Google Scholar]
- 9. Lan C, Chou SW, Chen SY, Lai JS, Wong MK. The aerobic capacity and ventilatory efficiency during exercise in Qigong and Tai Chi Chuan practitioners. Am J Chin Med 2004; 32: 141–150. [DOI] [PubMed] [Google Scholar]
- 10. GASC . General Administration of Sport of China: Baduanjin. 2013. [cited 2019 January 1st]. http://www.sport.gov.cn/n16/n1107/n1638/3886341.html
- 11. Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, Enright P, van der Grinten CP, Gustafsson P, Jensen R, Johnson DC, MacIntyre N, McKay R, Navajas D, Pedersen OF, Pellegrino R, Viegi G, Wanger J. Standardisation of spirometry. Eur Respir J 2005; 26: 319–338. [DOI] [PubMed] [Google Scholar]
- 12. ATS/ACCP . ATS/ACCP statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med 2003; 167: 211–277. [DOI] [PubMed] [Google Scholar]
- 13. Wasserman K. Principles of Exercise Testing and Interpretation: Including Pathophysiology and Clinical Applications, 5th ed. Philadelphia: Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2012. [Google Scholar]
- 14. Piepoli MF, Conraads V, Corra U, Dickstein K, Francis DP, Jaarsma T, McMurray J, Pieske B, Piotrowicz E, Schmid JP, Anker SD, Solal AC, Filippatos GS, Hoes AW, Gielen S, Giannuzzi P, Ponikowski PP. Exercise training in heart failure: from theory to practice. A consensus document of the Heart Failure Association and the European Association for Cardiovascular Prevention and Rehabilitation. Eur J Heart Fail 2011; 13: 347–357. [DOI] [PubMed] [Google Scholar]
- 15. Y.Q S. Chronic Heart Failure Cardiac Rehabilitation, 1st ed. China: People's Medical Publishing House; 2017. [Google Scholar]
- 16. Long L, Mordi IR, Bridges C, Sagar VA, Davies EJ, Coats AJ, Dalal H, Rees K, Singh SJ, Taylor RS. Exercise‐based cardiac rehabilitation for adults with heart failure. The Cochrane Database of Systematic Reviews 2019. 29: 1, Cd003331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Xiong X, Xu D. Therapeutic effect of Baduanjin on patients with coronary heart disease and chronic heart failure [in Chinese]. China Modern Medicine Journal 2016; 5: 55–56. [Google Scholar]
- 18. Yang X, Huang F, Shi Y, Wang Y, Ye L. Effect of aerobics training on exercise tolerance in patients with chronic heart failure [in Chinese]. Chin J Nurs 2015; 2: 193–197. [Google Scholar]
- 19. Yan X. Effects of Liuzi and Ba Duan Jin training on exercise tolerance in patients with chronic heart failure [in Chinese]. Chinese Traditional Medicine Modern Distance Education 2016; 16: 126–128. [Google Scholar]
- 20. Jing Y. Effect of TCM aerobics on exercise endurance in patients with chronic heart failure [in Chinese]. Chinese Traditional Medicine Modern Distance Education. 2015; 21: 12–14. [Google Scholar]
- 21. Chen DM, Yu WC, Hung HF, Tsai JC, Wu HY, Chiou AF. The effects of Baduanjin exercise on fatigue and quality of life in patients with heart failure: a randomized controlled trial. Eur J Cardiovasc Nurs 2018; 17: 456–466 [DOI] [PubMed] [Google Scholar]
- 22. Li R. Observation on the improvement of cardiac function and quality of life in elderly patients with chronic heart failure by Ba Duan Jin [in Chinese]. Massage and Rehabilitation Medicine 2017; 24: 23–25. [Google Scholar]
- 23. Xiao X, Wang J, Gu Y, Cai Y, Ma L. Effect of community based practice of Baduanjin on self‐efficacy of adults with cardiovascular diseases. PLOS One 2018; 13: e0200246–e0200246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Zheng G, Chen B, Fang Q, Lin Q, Tao J, Chen L. Baduanjin exercise intervention for community adults at risk of ischamic stroke: a randomized controlled trial. Sci Rep 2019; 9: 1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dube BP, Agostoni P, Laveneziana P. Exertional dyspnoea in chronic heart failure: the role of the lung and respiratory mechanical factors. 2016; 25: 317–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. May RW, Bamber M, Seibert GS, Sanchez‐Gonzalez MA, Leonard JT, Salsbury RA, Fincham FD. Understanding the physiology of mindfulness: aortic hemodynamics and heart rate variability. Stress (Amsterdam, Netherlands) 2016; 19: 168–174. [DOI] [PubMed] [Google Scholar]
- 27. Karmali KN, Davies P, Taylor F, Beswick A, Martin N, Ebrahim S. Promoting patient uptake and adherence in cardiac rehabilitation. Cochrane Database Syst Rev [serial on the Internet]. 2014. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD007131.pub3/abstract=1&t=iwqoicyw&s=3210605527f67fc7979306ec9d9e4dd2df23ddfe [DOI] [PubMed] [Google Scholar]
- 28. Tierney S, Mamas M, Woods S, Rutter MK, Gibson M, Neyses L, Deaton C. What strategies are effective for exercise adherence in heart failure? A systematic review of controlled studies. Heart Fail Rev 2012; 17: 107–115. [DOI] [PubMed] [Google Scholar]
- 29. Vromen T, Kraal JJ, Kuiper J, Spee RF, Peek N, Kemps HM. The influence of training characteristics on the effect of aerobic exercise training in patients with chronic heart failure: a meta‐regression analysis. Int J Cardiol 2016; 208: 120–127. [DOI] [PubMed] [Google Scholar]
- 30. Baduanjin exercises. [YouTube] [cited 2020. June 29]. https://www.youtube.com/watch?v=oqiENrM30Yk&t=661s
- 31. Baduanjin exercise (tutorial). [YouTube] [cited 2020. June 29]; Available from: https://www.youtube.com/watch?v=8r3t6kf5eXQ
- 32. Baduanjin (tuterial vedio): China's General Administration of Sport (in English). [YouTube] [cited 2020. June 29]. https://www.youtube.com/watch?v=5VPJbsdChYo


