Abstract
OBJECTIVE:
We aimed to develop a simple, rapid urine test based on the level of foaming that occurs in the urine sample due to the excretion of peptide structures containing amino acids specific to the antigenic structure of COVID-19. In this study, we present the preliminary results of the first clinical study with a newly developed urine foaming test (UFT).
METHODS:
This study was conducted in a tertiary hospital in Istanbul. After obtaining the approval of the ethics committee, urine samples were taken from three groups of patients whose informed consent was obtained. The groups were created according to the COVID-19 Diagnostic Guide of Ministry of Health: A: outpatients with suspected COVID-19, B: inpatients for follow-up and treatment, C: patients treated in intensive care unit (ICU). Also, 30 healthy volunteers were included as the control group D. Urine samples taken from all groups were delivered to the laboratory. 2.5 ml urine sample was added to the test tube and shaken for 15 seconds and the level of foam formed was visually evaluated according to the color scale. Other data of the patients were obtained from the hospital information management system and the physician caring for the patient. The clinical status, PCR test results, computed tomography (CT), if any, laboratory tests, and UFT results were compared and the level of statistical significance was expressed as p≤0.05 in the 95% confidence intervals (CI). Performance characteristics, such as sensitivity, specificity, positive and negative predictive value of the UFT, were statistically calculated according to the RT-PCR result and/or CT.
RESULTS:
A statistically significant difference was observed between UFT distributions of the control, outpatient, inpatient and ICU patients (p=0.0001). The results of UFT orange and red in inpatients and ICU patients were statistically significantly higher than in the control and outpatient groups. The diagnostic accuracy of UFT was detected in all group, the pooled sensitivity was 92% (95% CI: 87–95%) and specificity was 89% (95% CI: 80–98%).
CONCLUSION:
Our preliminary results suggest that the UFT is useful, particularly in predicting the clinical severity of COVID-19. The UFT could be recommended as a point of care test, rapid and non-invasive method in the diagnosis and follow-up of COVID-19.
Keywords: COVID-19, urine foaming test, prognostic predictive value
Analytical tests for the COVID-19 are very important for the management of disease and prevent spreading. A positive real-time reverse-transcriptase polymerase chain reaction (RT-rtPCR), in combination with medical and epidemiologic data, is the present classic for identification, but many difficulties still occur. Serological assays help know epidemiology improved and assess vaccine responses, but they are unpredictable for the diagnosis in the acute phase of infection [1]. Prospective and comparative assessments of rapid, simple, reliable tests for COVID-19 infection in clinically applicable locations are immediately required [2]. The features for optimal testing for diagnosis of COVID-19 should contain a short turnaround time, low equipment requirements, high accuracy, low cost to let admission to testing, also considering testing priorities to diagnose vulnerable populations. RT rt-qPCR on nasopharyngeal specimens has some of these features; thus, signifying the current gold standard in the diagnosis of COVID-19 [3]. However, many reasons, both procedural and virus-related, may damage its reliability [4], such as a one-time sampling [5] and lack of procedural standardization (sample collection, swab types, processing) [6]. Also, it remains difficult because of lack of personnel and supplies [7]. These recent concerns for the laboratory diagnosis of COVID-19 should be understood by clinicians, microbiology laboratories, public health authorities and policymakers [8]. Therefore, novel rapid tests and point-of-care (POC) assays would support infection recognition and prevention in communities without infrastructure, also in low- and middle-income locations. With this need in mind, we planned to develop a test to identify metabolites excreted specifically for COVID-19 in urine, which is the most easily taken biological sample. In current studies on patients with COVID-19, some urine biochemical parameters, such as blood and protein, are different between patients with severe COVID-19 and healthy controls [9, 10]. Proteinuria is a cardinal sign of diverse renal diseases and may result in foamy urine. Foaming occurs because albumin has a soap-like effect that reduces the surface tension of urine [11]. Foam forms by trapping pockets of gas in liquid with the help of surfactant. A surfactant is an organic compound that is amphiphilic (or amphipathic), meaning containing both hydrophilic and hydrophobic ends. A surfactant diffuses in water and adsorbs at interfaces between air and water, where the water-insoluble hydrophobic ends aggregate to form foam. In general, proteins or polypeptides have amphiphilic properties that can function as a surfactant and form foam in the urine. On the other hand, certain free amino acids share this property and potentially may also contribute to foam formation [12]. After suspicious contact or exposure with the COVID-19, if the transmission has occurred, as the viral load increases, the peptides of the virus and the metabolites of chemical reactions caused by the virus are excreted in the urine. The onset time and amount of excretion in the urine are related to the virulence of the causative pathogen, the amount of viral load at the time of first exposure, individual immunity, metabolism and existing comorbid diseases. Reagent in a foaming test tube specially prepared in the R&D Laboratory (MSK®) reacts with both COVID-19-specific metabolites and metabolic degradation products secondary to the virus found in urine. At this stage, the urine sample foams by shaking the test tube for 15 seconds. The foaming rate increases in direct proportion to the virus load in the body. Less foam in the urine of the patient with a low virus load and more foam occur in patients. Calibration studies were conducted in the R&D laboratory with urine samples taken from patients diagnosed with COVID-19 and healthy individuals known to have not had COVID-19. As a result of the data obtained, the color scale has been set on the test tube. Urine Foaming Test (UFT) results are evaluated according to this color scale; Green Zone: No virus-specific metabolites in urine, negative or mild clinical features (Fig. 1A). Yellow Zone: The presence of a low amount of virus-specific metabolites in the urine, requiring further investigation and follow-up. Orange Zone: Increased virus-specific metabolite in urine, adverse clinical picture, requiring further investigation and follow-up (Fig. 1B). Red Zone: Presence of intense viral metabolites in urine (and/or substances that should not be in urine), severe clinical picture. Although there are no symptoms and signs of COVID -19, people who have been detected in the especially Orange Zone or Red zone should be evaluated concerning urinary system pathologies.
FIGURE 1.
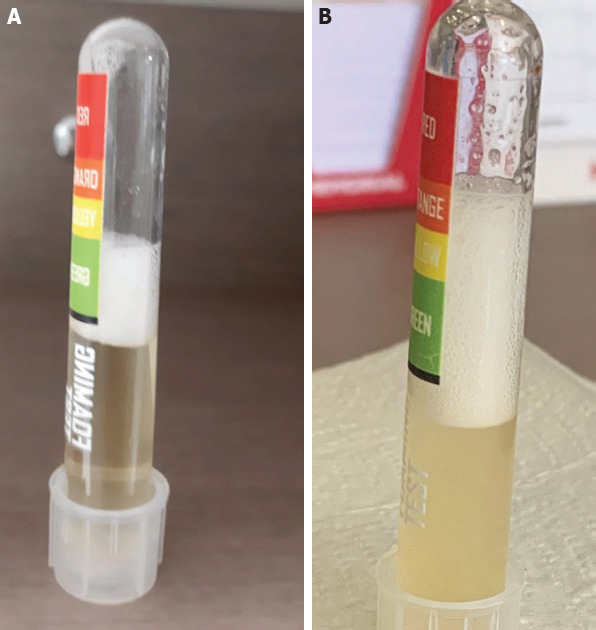
Two examples of urine foaming test with foam levels in the green zone (A) and orange zone (B).
MATERIALS AND METHODS
This study, which was designed as a prospective, randomized, single-blind (evaluator), was conducted in a tertiary training and research hospital of the Ministry of Health in Istanbul. This research was approved by the local Clinical Research Ethics Committee on October 5, 2020 (2011-KAEK-40 no: 2020-437), and permission was obtained from the Ministry of Health (2020-09-29T19_05_46). Also, written informed consent for this study was obtained from each participant included. This study, consecutively, included outpatients and/or hospitalized patients with a suspected case of COVID-19 from October 8, 2020, to October 15, 2020 were identified at a single tertiary care referral hospital and followed up to the end of November 2020. All suspected COVID-19 patients were included in this cohort study, but patients with diabetes and nephrotic disease were excluded from this study. All suspected COVID-19 patients were evaluated in the infectious diseases clinic of the hospital. Then, suspected patients experienced physical examinations with routine blood tests, RT-PCR and chest CT scans. According to the inclusion and exclusion criteria, 171 patients were included in this study divided into three groups as follows: group A: outpatients with suspected COVID-19 (n=80), group B: inpatients for follow-up and treatment (57), group C: patients in an intensive care unit (n=34). In addition, 30 healthy volunteers were included as the control group D (n=30). The cases evaluated as “probable cases” according to the COVID-19 diagnostic criteria guideline published by the Ministry of Health were included in the A group. The cases defined as “B and C” according to the same guideline were included in the B group. In group C, there were cases defined as C and D (COVID-19 General Information, Epidemiology and Diagnosis, TR Ministry of Health, June 2020). Mild symptoms were low-grade fever (<38 degrees celsius), dry cough, fatigue, sore throat, headache, the new loss of taste and smell. Moderate symptoms were fever of about 38.5–39 degrees celsius, chills, deep cough, fatigue and body aches, muscle pain, the general feeling of being unwell. Severe symptoms were shortness of breath, chest discomfort, confusion/unresponsiveness, possible gastrointestinal issues, like diarrhea or nausea, cardiovascular or central nervous system findings. All data of the patients were obtained from the hospital information management system and the physician who was caring for the patient.
Specimen Collection and Handling
10 ml of urine samples were taken from all patients and the control group into a sterile urine glass and transferred to the laboratory as soon as possible. All urine samples, as soon as accepted by the laboratory, were analyzed by the same technician with a urine foaming test tube and evaluated by the same biochemist according to the color scale. Urine was added to the test tube with foaming urine with the help of a Pasteur pipette to the black line of the tube (approximately 2.5 ml) and shaken for 15 seconds. The foam level formed was recorded as one of the green, yellow, orange and red zones indicated on the tube.
Statistical Analysis
All analyses were performed using the NCSS (Number Cruncher Statistical System) 2007 Statistical Software (Utah, USA) package program. In the evaluation of the data, in addition to descriptive statistical methods (mean, standard deviation), Shapiro-Wilk normality test was used to examine the distribution of variables, Kruskal Wallis test for subgroup comparisons of variables that did not show normal distribution, Dunn’s multiple comparison test for comparison of paired groups, Mann-Whitney U test for comparison of paired groups, Chi-square test was used to analyze qualitative data. According to the RT-PCR test and CT results, sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and likelihood- ratio LR (+) values were determined in the patient group. The results were evaluated at the significance level of p<0.05 in the 95% confidence intervals (CI).
RESULTS
The number of patients in each group and the distribution of the results of UFT, RT-PCR and CT are given in Table 1. A statistically significant difference was observed between the clinical situation, UFT results, RT-PCR results and CT image features distributions of control, outpatient, inpatient and intensive care patients (all of them p=0.0001). The results of UFT test orange and red, positive RT-PCR and positive CT in inpatients and intensive care patients were statistically significantly higher than in the outpatient and control groups (Table 2). Statistically significant differences were observed between the biochemical parameters and the results of UFT green, yellow, orange and red region in inpatient and intensive care patients (p<0.01). All biochemical parameters increased from green to red according to the color scale of the UFT test in inpatients and intensive care patients. The comparison of the results of C-RP, D-Dimer, ferritin, procalcitonin, interleukin-6 with the results obtained according to the UFT color scale is given in Table 3. The diagnostic accuracy of UFT was determined in all group, the pooled sensitivity was 92% (95% CI: 87–95%) and specificity was 89% (95% CI: 80–98%) (Table 4).
TABLE 1.
The number of patients in each group and the distribution of the results of UFT, RT-PCR and CT
| % (n=201) | |
|---|---|
| Group | |
| A (Outpatient) | 39.80 |
| B (Inpatient) | 28.36 |
| C (ICU) | 16.92 |
| D (Control) | 14.93 |
| UFT | |
| Green zone | 50.75 |
| Yellow zone | 25.37 |
| Orange zone | 16.42 |
| Red zone | 7.46 |
| RT-PCR | |
| Negative | 56.72 |
| Positive | 43.28 |
| CT image feature | |
| COVID-19 negative n=15 | 16.48 |
| COVID-19 positive n=76 | 83.51 |
UFT: Urine foaming test; RT-PCR: Real-time polymerase chain reaction; CT: Computerized tomography; ICU: Intensive care unit.
TABLE 2.
Comparison of the patients with COVID-19 in outpatient, inpatient and intensive care units according to clinical status, UFT, RT-PCR and CT images
| A (outpatient n=80) % | B (inpatient n=57) % | C (ICU n=34) % | D (Control n=30) % | p+ | |
|---|---|---|---|---|---|
| Clinical situation | |||||
| Mild | 72.50 | 19.30 | 2.94 | 0.00 | |
| Moderate | 27.50 | 80.70 | 23.53 | 0.00 | 0.0001 |
| Severe | 0.00 | 0.00 | 73.53 | 0.00 | |
| UFT | |||||
| Green | 63.75 | 19.29 | 8.82 | 100.00 | |
| Yellow | 32.50 | 38.59 | 29.41 | 0.00 | 0.0001 |
| Orange | 3.75 | 26.32 | 44.12 | 0.00 | |
| Red zone | 0.00 | 15.79 | 17.65 | 0.00 | |
| RT-PCR | |||||
| Negative | 80.00 | 21.05 | 23.53 | 100.00 | 0.0001 |
| Positive | 20.00 | 78.95 | 76.47 | 0.00 | |
| CT image features | |||||
| Negative | 95.00 | 31.58 | 2.94 | 0.00 | 0.0001 |
| Positive | 5.00 | 68.42 | 97.06 | 0.00 |
: Chi-Square test; UFT: Urine foaming test; RT-PCR: Real-time polymerase chain reaction; CT: Computerized tomography; ICU: Intensive care unit.
TABLE 3.
Comparison of the biochemical parameters according to color scale of urine foaming test (UFT) in inpatients and intensive care (ICU) patients
| Inpatient/ICU patients | Green zone n=14 | Yellow zone n=32 | Orange zone n=30 | Red zone n=15 | p† |
|---|---|---|---|---|---|
| C-RP | 57±64.82 | 60.42±43.23 | 193.18±151.56 | 205.36±100.92 | 0.0001† |
| D-Dimer | 2.48±1.21 | 4.74±8.04 | 8.14±8.21 | 13.47±12.63 | 0.004† |
| Ferritin | 306.84±462.63 | 641.58±446.04 | 1322.62±1879.75 | 1846.91±4887.84 | 0.006† |
| Procalcitonin | 0.64±1.32 | 0.99±2.19 | 3.89±5.12 | 8.61±19.72 | 0.007† |
| Interleukin-6 | 12.85±9.18 | 75.36±46.16 | 446.18±378.5 | 727.05±950.64 | 0.01* |
| Dunn’s multiple comparison tests | C-RP | D-Dimer | Ferritin | Procalcitonin | Interleukin-6 |
| Green/Yellow | 0.678 | 0.998 | 0.004 | 0.629 | 0.164 |
| Green/Orange | 0.002 | 0.009 | 0.008 | 0.016 | 0.047 |
| Green/Red | 0.005 | 0.013 | 0.001 | 0.01 | 0.001 |
UFT: Urine foaming test; ICU: Intensive care unit;
: Kruskal Wallis test;
: Mann-Whitney U test.
TABLE 4.
Performance of orange-red zone results of UFT test according to the clinical situation, RT-PCR and CT findings. The last line shows the total performance for all color scales of the UFT concerning the RT-PCR and/or CT positive COVID-19 status. According to the table, the UFT test shows the highest sensitivity when compared to the clinical situation (in this case the CT results are also positive)
| Sensitivity | Specificity | PPV | NPV | Accuracy | LR(+) | ||
|---|---|---|---|---|---|---|---|
| Mild/Moderate | Orange/Red zone | 0.95 | 0.85 | 0.56 | 0.99 | 0.87 | 6.33 |
| Severe/Critical | Orange/Red zone | 0.93 | 0.98 | 0.87 | 0.99 | 0.97 | 40.39 |
| RT-PCR | Orange/Red zone | 0.87 | 0.80 | 0.85 | 0.83 | 0.84 | 4.47 |
| CT | Orange/Red zone | 0.93 | 0.87 | 0.67 | 0.99 | 0.88 | 7.32 |
| RT-PCR and/or CT | UFT/Al | 0.87 | 0.80 | 0.97 | 0.35 | 0.84 | 5.47 |
UFT: Urine foaming test; RT-PCR: Real-time polymerase chain reaction; CT: Computerized tomography; PPV: Positive predictive value; NPV: Negative predictive value; LR: Likelihood-ratio.
DISCUSSION
Rapid and accurate diagnosis of COVID-19 is essential to establish an adequate therapeutic strategy to reduce morbidity and mortality, as well as pandemic control. In the pandemic, significant challenges have arisen in screening, diagnostic and follow-up testing. It is also important to identify patients who can be followed at home to reduce the burden of healthcare. Several diagnostic tools are needed to identify or rule out current infection, identify people in need of inpatient treatment or intensive care [13]. For this purpose, we aimed to develop a point of care test that is evaluated with different foaming levels by a chemical reaction specific to the amino acid content of virus-specific peptides in the urine sample. Normal urine is clear, with a yellowish hue, no blood or foam. Foamy urine is a sign of protein in the urine. This could be caused by some diseases that directly impact the kidneys but may also be a symptom of a medical issue affecting other systems. The peptides of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (the cause of COVID-19 in humans) and the metabolites of specific chemical reactions caused by the virus are excreted in the urine. The foam level is proportional to the amount of the amino acid content of the peptide structures of the SARS-COV2 virus in the urine. Our preliminary results suggest that the urine foaming (UFT) test is useful and usable, particularly in predicting the clinical severity of the disease.
The WHO recommends COVID-19 diagnosis to be made by laboratories using molecular tests targeting SARS-CoV-2 virus RNA. Even if RT-PCR is the most commonly accepted method for diagnosis, it may cause false-negative results, and its use is restricted by the necessity of laboratory infrastructure [14]. False-negative results may arise mostly because of insufficient extraction of nucleic acid, poor sample quality, low viral load, sample collection time, improper sample storage, transport, and handling and PCR inhibition [15, 16]. Results of various RT-PCRs protocols have revealed difference in their performance depending on the primers and probes. In many RT- PCR tests, the primers were designed against the envelope (E) and RNA-dependent RNA polymerase (RdRp) regions [17]. The E-region was used for screening, while the RdRp region was used for confirmation. Some researchers settled one-step RT-PCR tests to sense open reading frame (ORF) 1b and N regions of SARS-CoV-2 [18]. The N region assay was used for screening, while ORF1b testing served as a confirmatory test. On the other hand, since ORF1b and N regions are highly conserved in Sarbecoviruses, the specific primers may also bind other coronaviruses and associated viruses. The custom of specific primers provides the high specificity of result, but the possibility of false-positives cannot be excluded [13]. A chest computerized tomography (CT) scan can be secondhand as a diagnostic tool that allows physicians to well identify COVID-19 infection in many RT-PCR false-negative cases. Repeat tests can be needed if the patient has a clinical feature of viral pneumonia, and/or radiographic findings likeminded with COVID-19 pneumonia [19]. Some Chinese articles explain the challenge of recognizing gold standard for laboratory testing. In a study of 1.014 patients with suspected COVID-19 who experienced both CT and RT-PCR testing, 580 offered with positive RT-PCR and positive CT findings, while 105 were negative by both laboratory tests [20]. Of the 329 patients with conflicting results, only 19 were positive by RT-PCR, whereas 308 patients had positive CT findings. Therefore, 97% of patients with positive RT-PCR had positive chest CT, but most of patients with negative RT-PCR demonstrated viral pneumonia. Some of these patients later had positive RT-PCR. This study makes clear the challenge of developing a gold standard for diagnosis. RT-PCR results from a nasal swab are most likely to be positive in the first week after onset of symptoms, with the likelihood of a positive result dropping after that. Similarly, in our study, patients with moderate clinical findings and positive CT findings were detected in outpatients and inpatients, although RT-PCR was negative.
Although the duration of SARS-CoV-2 viral shedding in the upper and lower respiratory tract and stool has been reported that limited data are available for that in the urine. Nomoto et al. [21] investigated the detectability and duration of SARSCoV-2 RNA in the urine among patients with different severities of COVID-19. In their study, SARS-CoV-2 RNA was detected in the urine of two of 20 patients (10%). Their results suggest that SARS-CoV-2 RNA may excrete in the urine depending on the severity of COVID-19. The other two previous reports have evaluated the presence of this virus in urine [22, 23]. In one of the studies, the virus was detected in one of nine patients (11.1%) and, the other study included 72 urine specimens from patients; however, no patients were tested positive for SARS CoV-2 RNA [23]. In a meta-analysis examining the viral transmission of COVID-19 with urine and its clinical relationships, while COVID-19 was rarely detected in infected urine, infection transmission through urine was reported. Also, infected urine is more likely in the presence of moderate or severe disease [24].
Recently, research and development (R&D) studies on urine tests in the diagnosis of COVID-19 are common because urine is a simple and noninvasive biological sample. At the Medical Center of Göttingen University (Germany), researchers detected pathologies in the urine samples of patients with COVID-19 who became very sick within a few days (urine samples positive for blood, albumin, and leukocytes). They report that analysis of a urine sample on admission to hospital can be used to identify the systemic capillary leak syndrome, which can be a predictor of fluid overload, respiratory failure, need for ICU admission, and death [25]. They summarized that the respiratory tract is the entry for SARS-CoV-2 infection; however, COVID-19- related nephritis, which can be just screened for through a simple and low-cost urine sample analysis, may help predict complications. In another project, Chemists at Iowa State University are developing a paper-strip urine test to detect infection by the coronavirus that causes COVID-19. The test is designed to detect the presence of a coronavirus protein in a urine sample. The research group uses electric fields to boost test sensitivity. This technology, called electrokinetics, is used to concentrate, separate, isolate and manipulate charged particles [26]. We also propose this method we developed in a urine sample as a cost-effective and efficient tool. The limitation of the study is that it was not compared with a gold standard diagnostic method. However, to our knowledge, currently, there is no such lab test. We will initiate a multicentre observational study in Istanbul to confirm our findings. If validated, we believe that this test can allow early anticipation of later need for ICU admission, improved allocation of patients for special therapies. The same test could be used for the risk evaluation of the outpatients.
Consequently, easy-access, non-invasive, available at the point of care, with a scalable color urine foaming test can facilitate the rapid and accurate diagnosis and monitoring of COVID-19 infections and considerably assist in the control of this pandemic.
Footnotes
Ethics Committee Approval: This research was approved by the local Clinical Research Ethics Committee on October 5, 2020 (2011-KAEK-40 no: 2020-437), and permission was obtained from the Ministry of Health (2020-09-29T19_05_46).
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
Authorship Contributions: Concept – MSK, CK; Design – MSK, CK, BC; Supervision – HY, AEG; Fundings – HY, AEG; Materials – CK, MSK; Data collection and/or processing – CK, HY; Analysis and/or interpretation – CK, HY; Literature review – MSK, BC, AEG, HY; Writing – CK; Critical review – MSK, BC, HY, AEG.
REFERENCES
- 1.Shyu D, Dorroh J, Holtmeyer C, Ritter D, Upendran A, Kannan R, et al. Laboratory Tests for COVID-19:A Review of Peer-Reviewed Publications and Implications for Clinical UIse. Mo Med. 2020;117:184–95. [PMC free article] [PubMed] [Google Scholar]
- 2.Dinnes J, Deeks JJ, Adriano A, Berhane S, Davenport C, Dittrich S, et al. Cochrane COVID-19 Diagnostic Test Accuracy Group. Rapid point-of-care antigen and molecular-based tests for diagnosis of SARS-CoV-2 infection. Cochrane Database Syst Rev. 2020;8:CD013705. doi: 10.1002/14651858.CD013705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Russo A, Minichini C, Starace M, Astorri R, Calò F, Coppola N. Vanvitelli COVID-19 group. Current Status of Laboratory Diagnosis for COVID-19:A Narrative Review. Infect Drug Resist. 2020;13:2657–65. doi: 10.2147/IDR.S264020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lippi G, Simundic AM, Plebani M. Potential preanalytical and analytical vulnerabilities in the laboratory diagnosis of coronavirus disease 2019 (COVID-19) Clin Chem Lab Med. 2020;58:1070–6. doi: 10.1515/cclm-2020-0285. [DOI] [PubMed] [Google Scholar]
- 5.Cheng MP, Papenburg J, Desjardins M, Kanjilal S, Quach C, Libman M, et al. Diagnostic Testing for Severe Acute Respiratory Syndrome-Related Coronavirus 2:A Narrative Review. Ann Intern Med. 2020;172:726–34. doi: 10.7326/M20-1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu Y, Yan LM, Wan L, Xiang TX, Le A, Liu JM, et al. Viral dynamics in mild and severe cases of COVID-19. Lancet Infect Dis. 2020;20:656–7. doi: 10.1016/S1473-3099(20)30232-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vermeiren C, Marchand-Senécal X, Sheldrake E, Bulir D, Smieja M, Chong S, et al. Comparison of Copan ESwab and FLOQSwab for COVID-19 Diagnosis:Working around a Supply Shortage. J Clin Microbiol. 2020;58:e00669–20. doi: 10.1128/JCM.00669-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tang YW, Schmitz JE, Persing DH, Stratton CW. Laboratory Diagnosis of COVID-19:Current Issues and Challenges. J Clin Microbiol. 2020;58:e00512–20. doi: 10.1128/JCM.00512-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu R, Ma Q, Han H, Su H, Liu F, Wu K, et al. The value of urine biochemical parameters in the prediction of the severity of coronavirus disease 2019. Clin Chem Lab Med. 2020;58:1121–4. doi: 10.1515/cclm-2020-0220. [DOI] [PubMed] [Google Scholar]
- 10.Bonetti G, Manelli F, Bettinardi A, Borrelli G, Fiordalisi G, Marino A, et al. Urinalysis parameters for predicting severity in coronavirus disease 2019 (COVID-19) Clin Chem Lab Med. 2020;58:e163–5. doi: 10.1515/cclm-2020-0576. [DOI] [PubMed] [Google Scholar]
- 11.Kang KK, Choi JR, Song JY, Han SW, Park SH, Yoo WS, Kim HW, Lee D, Moon KH, Lee MH, Kim B. Clinical significance of subjective foamy urine. Chonnam Med J. 2012;48:164–8. doi: 10.4068/cmj.2012.48.3.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khitan ZJ, Glassock RJ. Foamy Urine:Is This a Sign of Kidney Disease? Clin J Am Soc Nephrol. 2019;14:1664–6. doi: 10.2215/CJN.06840619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pizzol JLD, Hora VPD, Reis AJ, Vianna J, Ramis I, Groll AV, et al. Laboratory diagnosis for Covid-19:A mini-review. Rev Soc Bras Med Trop. 2020;53:e20200451. doi: 10.1590/0037-8682-0451-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Venter M, Richter K. Towards effective diagnostic assays for COVID-19:a review. J Clin Pathol. 2020;73:370–7. doi: 10.1136/jclinpath-2020-206685. [DOI] [PubMed] [Google Scholar]
- 15.Vashist SK. In Vitro Diagnostic Assays for COVID-19:Recent Advances and Emerging Trends. Diagnostics (Basel) 2020;10:202. doi: 10.3390/diagnostics10040202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lv DF, Ying QM, Weng YS, Shen CB, Chu JG, Kong JP, et al. Dynamic change process of target genes by RT-PCR testing of SARS-Cov-2 during the course of a Coronavirus Disease 2019 patient. Clin Chim Acta. 2020;506:172–5. doi: 10.1016/j.cca.2020.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Corman VM, Landt O, Kaiser M, Molenkamp R, Meijer A, Chu DK, et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25:2000045. doi: 10.2807/1560-7917.ES.2020.25.3.2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chu DKW, Pan Y, Cheng SMS, Hui KPY, Krishnan P, Liu Y, et al. Molecular Diagnosis of a Novel Coronavirus (2019-nCoV) Causing an Outbreak of Pneumonia. Clin Chem. 2020;66:549–55. doi: 10.1093/clinchem/hvaa029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tu YP, O'Leary TJ. Testing for Severe Acute Respiratory Syndrome-Coronavirus 2:Challenges in Getting Good Specimens Choosing the Right Test and Interpreting the Results. Crit Care Med. 2020;48:1680–9. doi: 10.1097/CCM.0000000000004594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China:A Report of 1014 Cases. Radiology. 2020;296:E32–40. doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nomoto H, Ishikane M, Katagiri D, Kinoshita N, Nagashima M, Sadamasu K, Yoshimura K, Ohmagari N. Cautious handling of urine from moderate to severe COVID-19 patients. Am J Infect Control. 2020;48:969–71. doi: 10.1016/j.ajic.2020.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peng L, Liu J, Xu W, Luo Q, Chen D, Lei Z, et al. SARS-CoV-2 can be detected in urine blood, anal swabs and oropharyngeal swabs specimens. J Med Virol. 2020 Apr 24; doi: 10.1002/jmv.25936. [Epub ahead of print] doi:10.1002/jmv.25936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, et al. Detection of SARS-CoV-2 in Different Types of Clinical Specimens. JAMA. 2020;323:1843–4. doi: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kashi AH, De la Rosette J, Amini E, Abdi H, Fallah-Karkan M, Vaezjalali M. Urinary Viral Shedding of COVID-19 and its Clinical Associations:A Systematic Review and Meta-analysis of Observational Studies. Urol J. 2020;17:433–41. doi: 10.22037/uj.v16i7.6248. [DOI] [PubMed] [Google Scholar]
- 25.Gross O, Moerer O, Weber M, Huber TB, Scheithauer S. COVID-19-associated nephritis:early warning for disease severity and complications? Lancet. 2020;395:e87–8. doi: 10.1016/S0140-6736(20)31041-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim S, Ganapathysubramanian B, Anand RK. Concentration Enrichment Separation, and Cation Exchange in Nanoliter-Scale Water-in-Oil Droplets. J Am Chem Soc. 2020;142:3196–204. doi: 10.1021/jacs.9b13268. [DOI] [PubMed] [Google Scholar]


