Abstract
Objective
Because of the increasing emergence of skin manifestations of COVID-19 worldwide, we investigated the published reports of these lesions.
Methods
We conducted a literature search for original and review articles published from November 11, 2019 to September 30, 2020.
Results
We identified 5 skin lesions common in patients with COVID-19: pseudo-chilblains, rashes containing macules and papules, and urticarial, vesicular, and vaso-occlusive lesions. These lesions manifested at various times in relation to the COVID-19 symptoms, which may indicate whether the lesions are virus-induced or are delayed immunological responses to the infection. Skin lesions were more prevalent among Europeans and United States residents than among Asians, as was pseudo-chilblain, and the morphology of the skin lesions varied among continents. Pseudo-chilblains were the most common COVID-19 skin manifestation in Europe and the United States, but there was only 1 reported case from Asian populations. Additionally, patients with vaso-occlusive lesions were more likely than those with pseudo-chilblains to be admitted to the intensive care unit and to die.
Conclusion
Different cutaneous manifestations in patients with COVID-19 could reflect a wide spectrum of viral interactions with the skin, though reporting bias may play a role as well.
Key words: acral ischemia, coagulopathy, COVID-19, pseudo-chilblains, rash containing macules and papules, skin manifestations, urticaria, vesicle
Capsule Summary.
-
•
There are geographical differences in the morphology and prevalence of reported COVID-19–associated skin manifestations.
-
•
While genetic differences may play a role in the development of cutaneous manifestations and different types of lesions may be predictive of outcomes, reporting bias may be responsible for the observed regional variation.
Introduction
As COVID-19 continues to spread globally, the clinical spectrum of the disease remains incompletely known. The most common clinical features at the onset of illness are fever (85.6%), cough (68.7%), and fatigue (39.7%).1 The spectrum of manifestations of symptomatic infection ranges from mild to critical. An increasing number of reports worldwide concern the cutaneous manifestations of COVID-19 that precede common acute respiratory symptoms. The most commonly described cutaneous manifestation that precedes other COVID-19 symptoms is vesicular lesions, but they are not well characterized.2 For this literature review, we examined the published reports of the cutaneous manifestations of COVID-19, and we described these manifestations in relation to clinical practice. We report the geographical differences in the morphology of rashes, the onset of the rash eruption with reference to the illness progression, and the relationship of the rash to disease severity.
Methods
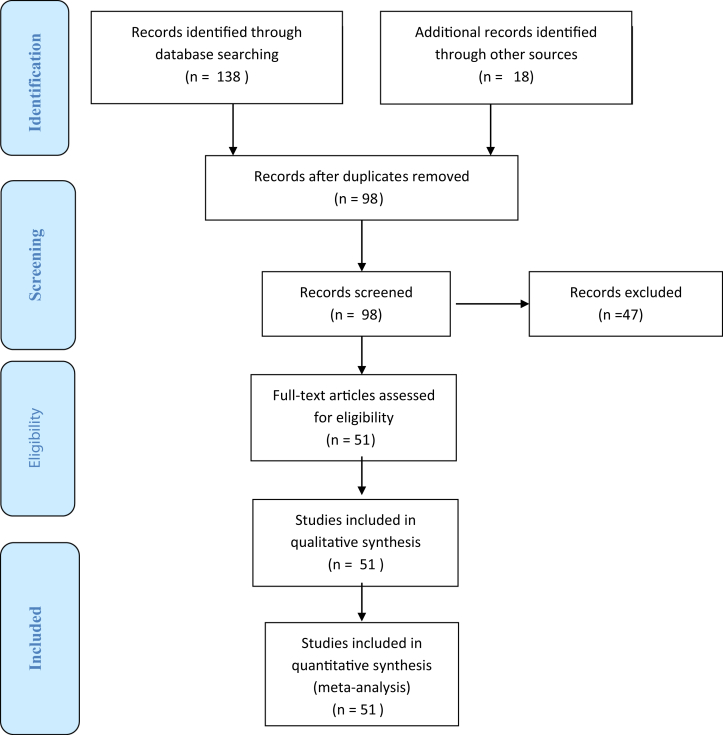
We searched PubMed, OVID, EMBASE, MEDLINE, and Google Scholar for original and review articles written in English and published from November 11, 2019, to September 30, 2020. We used the keywords “cutaneous,” “skin,” “rash,” and “dermatology” in combination with “COVID-19,” “2019-nCOV” (2019 novel coronavirus), and “SARS-CoV-2” (severe acute respiratory syndrome coronavirus 2). We limited the number of articles by eliminating those that lacked direct relevance to cutaneous manifestations (Fig 1). We extracted the following data from the included studies: author, region, age, sex, the morphology of the rash, the location of the skin manifestations, the time of the cutaneous eruption in relation to the other COVID-19 symptoms, and the clinical outcomes of the patients.
Fig 1.
COVID-19: summary of systematic review according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Results
We summarized the findings of 51 articles in this review, of which 27 were case series and 24 were case reports. A total of 1211 patients were described in these articles. The median age of the patients was 41.9 years (range: 15 days to 91 years); the ages of 451 patients were not reported. Of the patients, 336 (27.8%) were male and 424 (35.1%) were female; the gender of 451 patients (37.1%) was not reported. COVID-19 was confirmed in 627 patients (51.8%) and suspected in 584 (48.2%). Tables I and II detail these findings.3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53
Table I.
Characteristics of cutaneous manifestations of suspected and confirmed COVID-19 cases published in the literature in European and United States populations
| Author; region/country | Type of study, number of specific rashes reported (n)/total number of rashes, Age, sex | Cutaneous signs | Clinical outcomes |
|---|---|---|---|
| Vaso-occlusive lesions | |||
| Freeman; USA3 | Case series, n = 11/716 Median age: 66 9 M: 2 F |
Retiform purpura: 11 Vesicular: 18 Rash containing macules and papules: 61 Urticarial: 27 Pseudo-chilblain: 31 |
8 (72.7%) survival |
| Casas; Spain2 | Case series, n = 21/375, Mean age: 63.1 11 M: 10 F |
Acral ischemia: 21 Pseudo-chilblain: 71 Vesicular: 34 Urticarial 73 Rash containing macules and papules: 176 |
19 (90%) survival |
| Magro; New York, USA4 | Case series, n = 3/3 Mean age: 46 1 M: 2 F |
Retiform purpura: 1 Fixed livedoid rash: 2 |
3 (60%) survival |
| Suarez-Valle; Madrid, Spain5 | Case series, n = 3/3 NR, NR |
Acral ischemia | 3 (100%) Survival |
| Young; Cleveland, USA6 | Case series, n = 1/2, Age: 68 1 M |
Case 1 (multiple morphologies on a single patient): Rash containing macules and papules on the abdomen, pseudo-chilblain on digits, retiform purpura on buttock Case 2: Urticaria |
NR |
| De Masson; France7 | Case series, n = 4/277 NR, NR |
Pseudo-chilblain: 106 Rash containing macules and papules: 25 Vesicular lesion: 41 Vaso-occlusive: 4 Urticarial: 26 |
NR |
| Bosch-Amate; Spain8 | Case report, n = 1 Age: 79 1 F |
Painful retiform violaceous patches on both legs | 1 (100%) survival |
| Vesicular lesions | |||
| Freeman; USA3 | Case series, n = 18/716 Median age: 55 8 M: 10 F |
Vesicular: 18 Retiform purpura: 11 Rash containing macules and papules: 61 Urticarial: 27 Pseudo-chilblain: 31 |
18 (100%) survival |
| Askin; Turkey9 | Case series, n = 3/76 NR, NR |
Monomorphic vesicles unilateral at the upper trunk | NR |
| Marzano; Italy10 | Case series, n = 22/22 Mean age: 60 16 M: 6 F |
Varicella-like papulovesicular exanthema on trunk and limbs | 19 (86.4%) survival |
| Tammaro; Spain11 | Case series, n = 3/3 NR, NR |
Herpetiform lesions on the back | NR |
| Casas; Spain2 | Case series, n = 34/375, Mean age: 45.6 15 M: 19 F |
Pseudo-chilblain: 71 Vesicular: 34 Urticarial 73 Rash containing macules and papules: 176 Acral ischemia: 21 |
34 (100%) survival |
| Matar; France12 | Case series, N = 2/8 Mean age: 55.6 6 M: 2 F |
Exanthema with macules and papules: 3 Digitate papulosquamous rash: 1 Herpes recurrence: 1 Papulovesicular rash: 1 Grover's disease: 1 |
NR |
| Recalcati; Lombardy, Italy13 | Case series, n = 1/18 NR, NR |
Vesicles: 1 Rash containing macules and papules: 14 Urticaria: 3 |
NR |
| De Masson; France7 | Case series, n = 41/277 NR, NR |
Pseudo-chilblain: 106 Rash containing macules and papules: 25 Vesicular lesion: 41 Vaso-occlusive: 4 Urticarial: 26 |
NR |
| Mahé; France14 | Case series, n = 3/3 Mean age: 53.3 3 F |
Vesicular rash on the trunk and upper limbs | 3 (100%) survival |
| Bouaziz; France15 | Case series, n = 2/14 NR, NR |
Vesicles: 2 Exanthem: 4 Urticaria: 1 Pseudo-chilblains: 2 Others: 5 |
NR |
| Rash containing macules and papules | |||
| Freeman; USA3 | Case series, n = 78/716 Median age: 40.6 36 M: 42 F |
Vesicular: 18 Retiform purpura: 11 Rash containing macules and papules: 78 Urticarial: 27 Pseudo-chilblain: 31 |
76 (97.4%) survival |
| Recalcati; Lombardy, Italy13 | Case series, n = 3/18 NR, NR |
Urticaria: 3 Rash containing macules and papules: 14 Vesicles: 1 |
NR |
| Casas; Spain2 | Case series, n = 176/375 Mean age: 63.1 78 M: 98 F |
Rash containing macules and papules: 176 Urticaria: 73 Pseudo-chilblain: 71 Vesicular: 34 Acral ischemia: 21 |
172 (98%) survival |
| Sachdeva; Milan, Italy16 | Case series n = 3/3 Mean age: 73.3 3 F |
Macules and papules | 3 (100%) survival |
| Askin; Turkey9 | Case series, n = 12/34 NR, NR |
Rash containing macules and papules: 12 Pseudo-chilblain: 1 Urticaria: 7 |
NR |
| De Masson; France7 | Case series, n = 25/277 NR, NR |
Pseudo-chilblain: 106 Rash containing macules and papules: 25 Vesicular lesion: 41 Vaso-occlusive: 4 Urticarial: 26 |
NR |
| Reymundo; Spain17 | Case series, n = 7/7 Mean age: 66.6 2 M: 5 F |
Erythematous macules and papules | 7 (100%) survival |
| Young; Cleveland, USA6 | Case series, n = 1/2, Age: 68 1 M |
Case 1 (multiple morphologies on a single patient): Rash containing macules and papules, pseudo-chilblain, and retiform purpura Case 2: Urticaria |
1 (100%) survival |
| Matar; France12 | Case series, n = 2/8 Mean age: 55.6 6 M: 2F |
Exanthem with macules and papules: 3 Digitate papulosquamous rash: 1 Herpes recurrence: 1 Papulovesicular rash: 1 Grover's disease: 1 |
NR |
| Bouaziz; France15 | Case series, n = 4/14 NR, NR |
Exanthem: 4 Vesicles: 2 Urticaria: 1 Pseudo-chilblains: 2 Others: 5 |
NR |
| Hunt; New York, USA18 | Case report, n = 1 Age: 20 1 M |
Generalized, morbilliform rash containing macules and papules | NR |
| Jimenez-Cauhe; Madrid, Spain19 | Case report, n = 1 Age: 84 1 F |
Erythematous-purpuric, millimetric, coalescing macules at flexural areas | NR |
| Mahé; Colmar, France20 | Case report, n = 1 Age: 64 1 F |
Erythematous rash on both antecubital fossae, then to the trunk and axillary folds | 1 (100%) survival |
| Ahouach; France21 | Case report, n = 1 Age: 57 1 F |
Diffuse rash containing macules and papules on limbs and trunk | NR |
| Najarian; New Jersey, USA22 | Case report, n = 1 Age: 58 1 M |
Morbilliform exanthem on the trunk, upper limbs, and lower limbs | 1 (100%) survival |
| Maniaci; Catania, Italy23 | Case report, n = 1 Age: 15 1 M |
Erythematous rash on lower limbs | 1 (100%) survival |
| Boix-Vilanova; Spain24 | Case report, n = 1 Age: 59 1 M |
Pruriginous papulovesicular eruption on the trunk | 1 (100%) survival |
| Iancu; Sibiu, Romania25 | Case report, n = 1 Age: 41 1 F |
The rash containing macules and papules started on the trunk and spread centrifugally | 1 (100%) survival |
| Paolino; Milan, Italy26 | Case report, n = 1 Age: 37 1 F |
Cranio-caudal progression of the rash containing macules and papules | 1 (100%) survival |
| Moreno; Madrid, Spain27 | Case report, n = 1 Age: 32 1 F |
Cranio-caudal progression of the rash containing macules and papules | 1 (100%) survival |
| Urticarial lesions | |||
| Freeman; USA3 | Case series, n = 27/716 Median age: 42 years 6 M: 21 F |
Vesicular: 18 Retiform purpura: 11 Rash containing macules and papules: 61 Urticaria: 27 Pseudo-chilblain: 31 |
26 (96.3%) survival |
| Casas; Spain2 | Case series, n = 73/375 Mean age: 45.6 years 26 M: 47 F |
Urticaria: 73 Pseudo-chilblain: 71 Vesicular: 34 Rash containing macules and papules: 176 Acral ischemia: 21 |
100% survival |
| Recalcati; Lombardy, Italy13 | Case series, n = 3/18 NR, NR |
Urticaria: 3 Rash containing macules and papules: 14 Vesicular: 1 |
NR |
| Cepeda-Valdes; Mexico28 | Case series, n = 2/2 Mean age: 35 years 2 F |
Disseminated urticarial rash | 2 (100%) survival |
| Askin; Turkey9 | Case series n = 7/34 NR, NR |
Urticaria: 7 Rash containing macules and papules: 12 Pseudo-chilblain: 1 |
NR |
| De Masson; France7 | Case series, n = 26/277 NR, NR |
Pseudo-chilblain: 106 Rash containing macules and papules: 25 Vesicular: 41 Vaso-occlusive: 4 Urticaria: 26 |
NR |
| Bouaziz; France15 | Case series, n = 1/14 NR, NR |
Urticaria: 1 Vesicular: 2 Exanthem: 4 Pseudo-chilblain: 2 Other: 5 |
NR |
| Morey-Olivé; Barcelona, Spain29 | Case series, n = 2 Mean age: 3 years 1M: 1F |
Urticaria | 2 (100%) survival |
| Young; Cleveland, USA6 | Case series, n = 1/2, Age: 39 years 1 F |
Case 1: multiple morphologies on a single patient Case 2: Urticarial rash on the trunk, thigh |
1 (100%) survival |
| Henry; Orleans, France30 | Case report, n = 1 Age: 27 years 1 F |
Disseminated erythematous urticarial plaque eruption | 1 (100%) survival |
| Sousa Gonçalves; Portugal31 | Case report n = 1 Age: 57 years 1 F |
Urticarial rash on elbow and abdomen | 1 (100%) survival |
| Fernandez-Nieto; Spain32 | Case report, n = 1 Age: 32 years 1 F |
Urticaria | 1 (100%) survival |
| van Damme; Belgium33 | Case report, n = 1 Age: 71 years 1 M |
Urticaria | 0 (0%) survival |
| Pseudo-chilblain lesions | |||
| Freeman; USA, Canada, France, UK, Italy, Mexico, Netherlands, Iran34 | Case series, n = 31/716 Mean age: 32 15 M: 16 F |
Pseudo-chilblain: 31 Macular erythema: 23 Urticaria: 27 Morbilliform: 38 Vesicular: 18 Papulosquamous: 17 Retiform purpura: 11 |
29 (93.5%) survival |
| Casas; Spain2 | Case series, n = 71/375, Mean age: 45.6 26 M: 47 F |
Urticaria: 73 Pseudo-chilblain: 71 Vesicular: 34 Rash containing macules and papules: 176 Acral ischemia: 21 |
71 (100%) survival |
| Fernandez-Nieto; Spain35 | Case series, n = 95/132 Mean age: 23.4 years 49 M: 46 F |
Pseudo-chilblain: 95 Erythema multiform-like: 37 |
NR |
| De Masson; France7 | Case series, n = 106/277 NR, NR |
Pseudo-chilblain: 106 Rash containing macules and papules: 25 Vesicular: 41 Vaso-occlusive: 4 Urticaria: 26 |
NR |
| Duong; France36 | Prospective; crowd-sourced social media n = 146/295 NR, NR |
Pseudo-chilblain: 146 Other: 149 |
NR |
| Askin; Turkey9 | Case series, n = 1/34 NR, NR |
Pseudo-chilblain: 1 Rash containing macules and papules: 12 Urticaria: 7 |
1 (100%) survival |
| Landa; Spain37 | Case series, n = 6/6 Mean age: 35.3 3 M: 3 F |
Pseudo-chilblains on toes, fingers | 6 (100%) survival |
| Colonna; Italy38 | Case series, n = 30 Mean age: 11 17 M: 13 F |
Pseudo-chilblains | 30 (100%) survival |
| Tosti; Italy39 | Case series, n = 4 Mean age: 38 2 M: 2 F |
Pseudo-chilblains at heels and extensor surfaces of toes | 4 (100%) survival |
| Bouaziz; France15 | Case series, n = 2/14 NR, NR |
Pseudo-chilblains: 2 Exanthem: 4 Vesicles: 2 Urticaria: 1 Others: 5 |
NR |
| Young; Cleveland, USA6 | Case series, n = 1/2, Age: 68 1 M |
Case 1 (multiple morphologies on a single patient): Maculopapular rash on abdomen, pseudo-chilblain on digits, retiform purpura on buttock Case 2: urticaria |
NR |
| Mazzotta; Italy40 | Case report, n = 1 Age: 13 1 M |
Erythematous-violet rounded lesions onplantar surfaces of 1st right toe and dorsal surface of 2nd toe on both feet | 1 (100%) survival |
| Estébanez; Spain41 | Case report, n = 1 Age: 28 1 F |
Pruritic, confluent erythematous-yellowish papules on both heels | 1 (100%) survival |
| Other lesions | |||
| Fernandez-Nieto; Spain35 | Case series, n = 37/132 Mean age: 12.2 22 M: 15 F |
Pseudo-chilblain: 95 Erythema multiforme-like: 37 |
NR |
| Askin; Turkey9 | Case series, n = 12/34 | Petechiae (n = 4); aphthous stomatitis (n = 3); Necrosis of maxillary region/sacrum (n = 4); pruritus (n = 1) |
|
| Jimenez-Cauhe; Spain42 | Case series, n = 4/4 | Erythema multiforme-like eruptions | NR |
| Manalo; Atlanta, Georgia, USA43 | Case series, n = 2/2 Mean age: 57 1 M: 1 F |
Livedo reticularis: 2 | NR |
| Bouaziz; France15 | Case series, n = 5/14 NR, NR |
Macules with “porcelain-like” appearance: 1 Livedo reticularis: 1 Non-necrotic purpura: 1 Necrotic purpura: 1 Eruptive cherry angioma: 1 Exanthem: 4 Vesicles: 2 Urticaria: 1 |
NR |
| Verheyden; Brussel44 | Case report, n = 1 Age: 57 1 M |
Relapsing livedo reticularis | NR |
| Kamali Aghdam; Iran45 | Case report, n = 1 Age: 15 days old 1 M |
Cutaneous mottling | NR |
F, Female; M, male; n, number; NR, not reported; USA, United States.
Table II.
Characteristics of cutaneous manifestations of suspected and confirmed COVID-19 cases published in the literature in Asian populations
| Author; Region/country | Type of study, number of specific rashes reported (n)/total number of rashes, Mean age, sex | Cutaneous signs | Clinical outcomes |
|---|---|---|---|
| Vaso-occlusive lesions | |||
| Zhang; China46 | Case series, n = 7/7 Mean age: 59.8 4 M: 3 F |
Vaso-occlusive | 2 (28.6%) survival |
| Alramthan; Middle East/Qatar47 | Case series, n = 2/2 Mean age: 31 years 2 F |
Cases 1, 2: Vaso-occlusive | 2 (100%) survival |
| Pangti; India48 | Case series, n = 2/10 Mean age: 29.5 years 2 M |
Vaso-occlusive: 2 Rash containing macules and papules: 2 Urticaria: 3 Pseudo-chilblain: 1 Other: 2 (desquamation, aphthous ulcer) |
1 (50%) survival |
| Rashes containing macules and papules | |||
| Dalal; North India49 | Case series, n = 3/13 NR, NR |
Rash containing macules and papules: 3 Urticaria: 2 Pruritus: 8 |
NR |
| Pangti; India48 | Case series, n = 2/10 Mean age: 35 2 M |
Vaso-occlusive: 2 Rash containing macules and papules: 2 Urticaria: 3 Pseudo-chilblains: 1 Others: 2 (desquamation, aphthous ulcer) |
2 (100%) survival |
| Ho; Singapore50 | Case series, n = 2 Mean age: 59 1 M: 1 F |
Rash containing macules and papules: 2 | 2 (100%) survival |
| Urticarial lesions | |||
| Pangti; India48 | Case series, n = 3/10 Mean age: 55.5 1 M: 2 F |
Vaso-occlusive: 2 Rash containing macules and papules: 2 Urticaria: 3 Pseudo-chilblains: 1 Others: 2 (desquamation, aphthous ulcer) |
3 (100%) survival |
| Lu; China51 | Case report n = 1 NR, NR |
Urticaria | 1 (100%) survival |
| Abasaeed; Abu Dhabi, United Arab Emirates52 | Case report, n = 1 Age: 40 1 M |
Urticaria with angioedema (negative demographism) | 1 (100%) survival |
| Shanshal; Baghdad, Iraq53 | Case report, n = 1 Age: 35 1 F |
Multiple morphologies in a single patient Urticarial lesions on the trunk, upper and lower extremities, anagen effluvium |
1 (100%) survival |
| Pseudo-chilblain lesions | |||
| Pangti, India48 | Case series, n = 1/10 Age: 50 years 1 F |
Vaso-occlusive: 2 Rash containing macules and papules: 2 Urticaria: 3 Pseudo-chilblain: 1 Other: 2 (desquamation, aphthous ulcer) |
1 (100%) survival |
| Other lesions | |||
| Pangti, India48 | Case series, n = 2/10 Age: 26 years 2 M |
Desquamation: 1 Aphthous ulcer: 1 |
2 (100%) survival |
F, Female; M, male; n, number; NR, not reported.
We found demographic differences in the prevalence and the morphology of the skin manifestations in COVID-19. Of the 1211 patients with COVID-19–associated skin manifestations, 39 (3.1%) patients were from Asian populations and 1172 (96.9%) patients were from Europe and the United States (Tables I and II). Pseudo-chilblains were the most common COVID-19–related skin manifestations among Europeans and United States residents, but there was only 1 reported case from Asia.
We classified cutaneous manifestations in patients with COVID-19 into 5 major classes according to the order of severity (Table III). In nearly all patients, the lesions could be classified into one of these groups:
-
1.
Vaso-occlusive lesions, which included fixed livedo racemosa (netlike violaceous skin lesions composed of irregularly broken macules with an annular pattern), retiform purpura (stellate purpuric skin lesions), and acral ischemia (ischemic lesions on the digits or toes). Vaso-occlusive lesions were the least common but were associated with the lowest survival rate of 78.9% (Table III).
-
2.
Vesicular lesions, which tended to affect the trunk and whose configuration varied. Herpetiform, varicella-zoster–like, and monomorphic vesicle formation had been described previously in the literature on COVID-19. Vesicular lesions were reported as usually occurring at the onset of COVID-19 symptoms (Table IV). Among patients with COVID-19 and vesicular lesions, the survival rate was 96.1% (Table III).
-
3.
Erythematous rash containing macules and papules, predominantly involving the trunk. More than half of the affected patients were female, and itchiness was the major symptom. Among patients with COVID-19 and rash containing macules and papules, the survival rate was 98.2% (Table III).
-
4.
Urticarial lesions, which were transient edematous papules and plaques that disappeared within 24 h. More than half of the affected patients were middle-aged women. Urticarial lesions were associated with a survival rate of 97.5% (Table III).
-
5.
Pseudo-chilblains presented as erythematous or violaceous papules on acral surfaces. Vesicles and pustules with purpuric areas have also been described. This condition was termed “pseudo-chilblains” because of the similar appearance of these lesions to chilblains, but there was no documented exposure to cold or other risk factors for chilblains. Pseudo-chilblains were more common in young adults compared with elderly patients and were associated with a survival rate of 98.7% (Table III).
Table III.
A summary of worldwide cutaneous manifestations of COVID-19 and survival Data
| Characteristics | Vaso-occlusive lesions | Vesicular lesions | Urticarial lesions | Rashes containing macules and papules | Pseudo-chilblains |
|---|---|---|---|---|---|
| Number of patients | 56 | 129 | 153 | 339 | 496 |
| Median age | 63 | 54.3 | 43.7 | 55.5 | 27.2 |
| Sex | 28 M: 21 F 7 not reported |
39 M: 38 F 52 not reported |
36 M: 77 F 40 not reported |
124 M: 155 F 60 not reported |
111 M: 130 F 255 not reported |
| Region/Country | USA 14 Spain 25 France 4 China 7 Kuwait 2 India 2 |
USA 18 Spain 37 Italy 23 France 48 Turkey 3 |
USA 28 Mexico 2 Spain 76 Italy 3 France 28 Belgium 1 Portugal 1 Turkey 7 China 1 India 5 United Arab Emirates 1 |
USA 81 Spain 186 Italy 19 France 33 Romania 1 Turkey 12 India 4 Singapore 2 |
USA 32 Spain 173 Turkey 1 Italy 35 France 254 India 1 |
| Survival | 41 (78.9%); 4 not reported | 74 (96.1%); 52 not reported | 112 (98.2%); 39 not reported | 270 (97.5%); 62 not reported | 145 (98.7%); 349 not reported |
F, Female; M, male; USA, United States.
Table IV.
Prevalence of 5 common skin manifestations in 1211 patients with COVID-19 and the timing of the skin eruption in relation to the COVID-19 symptoms
| Eruption of lesions before the COVID-19 symptoms | Eruption of lesions together with the COVID-19 symptoms | Eruption of lesions after the COVID-19 symptoms | Eruption of lesions not documented | |
|---|---|---|---|---|
| 1. Pseudo-chilblain lesions (n = 496, 40.9%) | 36 (7.3%) | 71 (14.3%) | 177 (35.8%) | 41 (8.2%) not documented; 171 (34.4%) patients did not have other COVID-19 symptoms |
| 2. Rashes containing macules and papules (n = 339, 27.9%) | 17 (4.7%) | 188 (55.8%) | 109 (32%) | 25 (7.5%) |
| 3. Urticarial lesions (n = 153, 12.5%) | 8 (4.6%) | 79 (51.7%) | 51 (33.1%) | 15 (10.6%) |
| 4. Vesicular lesions (n = 129, 10.7%) | 11 (8.5%) | 49 (38%) | 62 (48.1%) | 7 (5.4%) |
| 5. Vaso-occlusive lesions (n = 56, 4.4%) | 3 (3.75%) | 36 (68%) | 14 (24.5%) | 3 (3.75%) |
| 6. Others (n = 38, 3.1%) | 0 | 0 | 18 (47.4%) | 20 (52.6%) |
Thirty-eight of 1211 patients (3%) showed other skin manifestations, such as petechiae, cutaneous mottling, eruptive cherry angioma, violaceous macules with “porcelain-appearance,” non-necrotic or necrotic purpura, aphthous ulcers, purpuric exanthema, telogen effluvium, and relapsing livedo reticularis.9,15,44,54
Discussion
We wished to characterize these manifestations for further diagnostic and prognostic value because cutaneous manifestations of COVID-19 have been increasingly reported worldwide.
In this review, we found that the reported prevalence of COVID-19–associated cutaneous manifestations differed globally, from 0.2% in China55 to 7.25% in India48 and 20.4% in Italy13 The morphology of the skin manifestations in COVID-19 also differed geographically. Pseudo-chilblains were the most common COVID-19 skin manifestations in Europe and the United States, but there was only 1 reported case from Asia.
Pseudo-chilblains presented as erythematous or violaceous papules on acral surfaces, most commonly on the hands and feet. Vesicles and pustules with purpuric areas have also been described. Because of their similar appearance to chilblains, these lesions were termed “pseudo-chilblains” as there was no cold exposure prior to lesion eruption. On March 29, 2020, the first report of chilblain-like lesions appeared in Italy. A series of cases of chilblain-like lesions then began to emerge in Italy, France, Spain, and the United States. Pseudo-chilblains were suspected of being related to COVID-19 because the outbreak of these lesions during the early spring was concurrent with the COVID-19 pandemic. A few teledermatology groups were created in Italy, France, and Spain to collate the details of the patients and skin lesions. Our review showed that pseudo-chilblains appeared in the later stage of the disease and are associated with indolent disease progression. There are multiple postulated pathophysiologic mechanisms of pseudo-chilblains in COVID-19. Kolivras et al56 from Belgium demonstrated histopathologic similarities between pseudo-chilblains and chilblain lupus. Interferon 1 plays an essential role in immune stimulation in both acute viral infections and cutaneous lupus erythematosus. It is hypothesized that a robust antiviral type 1 interferon response may truncate the clinical course and induce microangiopathic changes, producing chilblain-like lesions.56 There is an interethnic discrepancy in the prevalence of pseudo-chilblain lesions. A multicentric case series by Freeman et al34 collated a total of 318 patients with pseudo-chilblains; 89% of patients were white and only 0.7% were black or African American. Pseudo-chilblains were the most common COVID-19 skin manifestations in Europe and the United States, but no cases were reported in China. Interferon-induced helicase C domain-containing protein 1 (IFIH1) is an immune receptor that senses coronavirus RNA and initiates the cascade of antiviral responses, including induction of type 1 interferons and proinflammatory cytokines. The role of the IFIH1 polymorphism, rs1990760 (C>T; aaA946T) is well studied in viral infection, and individuals with the minor allele T have enhanced interferon production.57 The minor allele frequency (Tmaf) is more common in white populations compared with Chinese and African populations.57 This could explain why pseudo-chilblains were more frequently seen in white populations compared with other races. However, another possible explanation for the discrepancy is underreporting of skin manifestations in skin-of-color populations.
Vaso-occlusive lesions included fixed livedo racemosa, retiform purpura, and acral ischemia. Vaso-occlusive lesions were the least common skin manifestations of COVID-19, but they were associated with poorer outcomes. Because they erupted on acral surfaces, vaso-occlusive lesions should be distinguished from pseudo-chilblains. In contrast to pseudo-chilblains, which were more prevalent in young people,37 vaso-occlusive lesions tended to affect elderly patients.2 In comparison with patients who had other cutaneous manifestations, patients with vaso-occlusive lesions were at a higher risk of severe pneumonia requiring intensive care, which was associated with higher mortality rates.2 Vaso-occlusive lesions were linked to markedly elevated levels of D-dimer and disseminated intravascular coagulation.4,46 Histopathologic examination of vaso-occlusive lesions by Magro et al4 demonstrated that thrombogenic vasculopathy with deposition of C5b9 and C4d vaso-occlusive lesions is a pauci-inflammatory thrombotic event. They also found a striking similarity between lung autopsy and skin histology results in 2 patients who succumbed to COVID-19. This suggested that complement system activation led to systematic microvascular injury. Cutaneous microvascular injury that manifests as vaso-occlusive lesions could be a potential marker of severe COVID-19 infection.
There were also differences in the reported prevalence of vaso-occlusive lesion among continents. The reported prevalence of vaso-occlusive lesions in Spain was 5.2%,2 whereas the prevalence of vaso-occlusive lesions from a multicentric study from the United States was 6.4%.3 However, the reported prevalence of vaso-occlusive lesions in India was 1.4%.48 The findings raised the suspicion of the interplay of genetic thrombophilia-related factors within certain ethnic populations in vaso-occlusive lesions in COVID-19. Lipoprotein A (LpA) plays a major role in thrombo-occlusive vasculopathy.58,59 Criado et al demonstrated thrombosis, fibrin, and LpA deposition on cutaneous blood vessels in a patient with livedoid vasculopathy. Convincing data has shown genetic variability in LpA levels between ethnic populations. Studies have consistently shown that black individuals have 2–3-fold higher LpA levels than white individuals. Although there are fewer studies in the Asian population, data showed that Chinese individuals had lower LpA levels compared with Caucasian individuals.60 The interethnic difference in the prevalence of factor V Leiden mutations may also play a role. The mutation was most common among patients of Latino descent (2.21%), followed by patients of American descent (1.25%) and of African descent (1.23%), and least common in patients of Asian descent (0.45%).61 These genetic differences correspond with the reported higher prevalence of vaso-occlusive lesions among US residents and Europeans than among Asians.2,3,13,55,62
Rash containing macules and papules was the second most common cutaneous manifestation of COVID-19. However, rashes containing macules and papules were not specific to COVID-19, and there were reports of misdiagnosed cases of COVID-19 as viral illness in patients with rash containing macules and papules.18 Given the current pandemic, the presence of a rash containing macules and papules should prompt suspicion of COVID-19. This would help with early identification and containment of the disease. Approximately 55.8% of rashes containing macules and papules occurred during the active phase of the disease, which may correspond to the viremia phase (Table IV). Skin biopsy of the rash containing macules and papules showed a nest of Langerhans cells within the epidermis with mild perivascular lymphocytic infiltration in the papillary dermis.63 Young and Fernandez6 described the histopathology of a specimen from an elderly man with a rash containing macules and papules, which showed apoptotic keratinocytes in the epidermis. During the viremic phase, the virus spread in a hematogenous fashion, including to the endothelium of cutaneous vessels. Infected endothelial cells then attracted cytotoxic T cells, which caused rashes containing macules and papules.
Najarian22 reported a 58-year-old Hispanic man who developed morbilliform exanthem on the trunk and limbs on day 2 of COVID-19 symptoms. However, this patient had also taken azithromycin and benzonatate for 2 days prior to the onset of rash. This highlighted another challenge in defining the etiological diagnosis of skin lesions in the COVID-19 pandemic. Some useful clues to differentiate between drug rashes and viral rashes are the morphology and presence of enanthem pustular dusky lesions, which are suggestive of a drug etiology, whereas a petechial or vesicular pattern, involvement of the buttocks or acral sites, and presence of enanthem are suggestive of an infectious etiology, including a viral etiology.64
Joob and Wiwanitkit described a patient in Thailand who initially presented with fever and petechiae, which was misdiagnosed as dengue fever. The patient subsequently developed respiratory symptoms and tested positive for COVID-19 via reverse transcription polymerase chain reaction.54 Thus, COVID-19–associated cutaneous manifestations could mimic other viral rashes. This is of importance in Southeast Asia, where dengue virus infection is endemic.
Urticaria was the third most common skin manifestation in patients with COVID-19. One of the postulated hypotheses about the pathogenesis of urticaria in COVID-19 was virus-induced mast cell degranulation, whereby SARS-CoV-2 enters vascular cells via angiotensin-converting enzyme-2. The deposition of antigen-antibody complexes leads to complement activation, mast cell degranulation, and bradykinin release.65 This is supported by the demonstration of colocalization of SARS-CoV-2 glycoproteins with complement components in cutaneous blood.4 However, Pathania reported that emotional stress related to COVID-19, rather than the infection itself, may trigger the urticaria.66 Hassan described a patient with a history of atopic dermatitis who presented with urticaria as the prodromal cutaneous manifestation of COVID-19.67
Rashes reminiscent of symmetrical drug-related intertriginous and flexural exanthema (SDRIFE) were described in 2 patients with COVID-19 from France and Spain. In both patients, SDRIFE-like skin manifestations developed on day 3 of the illness. The rashes were described as erythematous, millimetric, coalescing macules predominantly distributed at flexural areas.20,68 Although SDRIFE is classically associated with drug reactions, the rashes reported in these 2 cases may have been associated with COVID-19, as no culprit drug was identified in either patient.
This literature review had a few limitations. First, many of the included studies were case reports and studies with small sample sizes. Second, not all the included subjects had COVID-19 confirmatory tests because of the limited resources in certain regions. The difference between the prevalence of cutaneous manifestations in Europeans and United States residents compared with Asians could be attributable to underreporting in Asian countries. However, in countries with a heterogeneous racial make-up, such as the United States, black and Latino populations have been disproportionately affected. The implication of genetic factors in polymorphous cutaneous reactions in COVID-19 remains to be explored.
The scientific understanding of cutaneous manifestations in patients with COVID-19 is still evolving. Polymorphous cutaneous manifestations in patients with COVID-19 infection could potentially reflect a full spectrum of viral interactions with the skin, characterized by direct viral action in infected cells, immune system hyperactivity, and hypercoagulability. Future studies with better scientific documentation would help elucidate the pathophysiologic features and the prognostic factors of the cutaneous manifestations in COVID-19.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Lovato A., de Filippis C. Clinical presentation of COVID-19: a systematic review focusing on upper airway symptoms. Ear Nose Throat J. 2020;99(9) doi: 10.1177/0145561320920762. 0145561320920762. [DOI] [PubMed] [Google Scholar]
- 2.Casas C.G., Català A., Hernández G.C. Classification of the cutaneous manifestations of COVID-19: a rapid prospective nationwide consensus study in Spain with 375 cases. Br J Dermatol. 2020;183(1):71–77. doi: 10.1111/bjd.19163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Freeman E.E., McMahon D.E., Lipoff J.B. The spectrum of COVID-19–associated dermatologic manifestations: an international registry of 716 patients from 31 countries. J Am Acad Dermatol. 2020;83(4):1118–1129. doi: 10.1016/j.jaad.2020.06.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Magro C., Mulvey J.J., Berlin D. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res. 2020;220:1–13. doi: 10.1016/j.trsl.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Suarez-Valle A., Fernandez-Nieto D., Diaz-Guimaraens B., Santas M.D., Carretero I., Garcia B.P. Acro-ischaemia in hospitalized COVID-19 patients. J Eur Acad Dermatol Venereol. 2020;34(9):e455–e457. doi: 10.1111/jdv.16592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Young S., Fernandez A.P. Skin manifestations of COVID-19. Cleve Clin J Med. 2020 doi: 10.3949/ccjm.87a.ccc031. [DOI] [PubMed] [Google Scholar]
- 7.de Masson A., Bouaziz J., Sulimovic L. Chilblains is a common cutaneous finding during the COVID-19 pandemic: a retrospective nationwide study from France. J Am Acad Dermatol. 2020;83(2):667–670. doi: 10.1016/j.jaad.2020.04.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bosch-Amate X., Giavedoni P., Podlipnik S. Retiform purpura as a dermatological sign of coronavirus disease 2019 (COVID-19) coagulopathy. J Eur Acad Dermatol Venereol. 2020;34(10):e548–e549. doi: 10.1111/jdv.16689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Askin O., Altunkalem R.N., Altinisik D.D., Uzuncakmak T.K., Tursen U., Kutlubay Z. Cutaneous manifestations in hospitalized patients diagnosed as COVID-19. Dermatol Ther. 2020:e13896. doi: 10.1111/dth.13896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marzano A.V., Genovese G., Fabbrocini G. Varicella-like exanthem as a specific COVID-19-associated skin manifestation: multicenter case series of 22 patients. J Am Acad Dermatol. 2020;83(1):280–285. doi: 10.1016/j.jaad.2020.04.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tammaro A., Adebanjo GAR., Parisella F.R., Pezzuto A., Rello J. Cutaneous manifestations in COVID-19: the experiences of Barcelona and Rome. J Eur Acad Dermatol Venereol. 2020;34(7):e306–e307. doi: 10.1111/jdv.16530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matar S., Oulès B., Sohier P. Cutaneous manifestations in SARS-CoV-2 infection (COVID-19): a French experience and a systematic review of the literature. J Eur Acad Dermatol Venereol. 2020;34(11):e686–e689. doi: 10.1111/jdv.16775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Recalcati S. Cutaneous manifestations in COVID-19: a first perspective. J Eur Acad Dermatol Venereol. 2020;34(5):e212–e213. doi: 10.1111/jdv.16387. [DOI] [PubMed] [Google Scholar]
- 14.Mahé A., Birckel E., Merklen C. Histology of skin lesions establishes that the vesicular rash associated with COVID-19 is not ‘varicella-like’. J Eur Acad Dermatol Venereol. 2020;34(10):e559–e561. doi: 10.1111/jdv.16706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bouaziz J.D., Duong T., Jachiet M. Vascular skin symptoms in COVID-19: a French observational study. J Eur Acad Dermatol Venereol. 2020;34(9):e451–e452. doi: 10.1111/jdv.16544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sachdeva M., Gianotti R., Shah M. Cutaneous manifestations of COVID-19: report of three cases and a review of literature. J Dermatol Sci. 2020;98(2):75–81. doi: 10.1016/j.jdermsci.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reymundo A., Fernáldez-Bernáldez A., Reolid A. Clinical and histological characterization of late appearance maculopapular eruptions in association with the coronavirus disease 2019. A case series of seven patients. J Eur Acad Dermatol Venereol. 2020;34(12):e755–e757. doi: 10.1111/jdv.16707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hunt M., Koziatek C. A case of COVID-19 pneumonia in a young male with full body rash as a presenting symptom. Clin Pract Cases Emerg Med. 2020;4(2):219–221. doi: 10.5811/cpcem.2020.3.47349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jimenez-Cauhe J., Ortega-Quijano D., Prieto-Barrios M., Moreno-Arrones O.M., Fernandez-Nieto D. Reply to “COVID-19 can present with a rash and be mistaken for Dengue”: petechial rash in a patient with COVID-19 infection. J Am Acad Dermatol. 2020;83(2):e141–e142. doi: 10.1016/j.jaad.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mahé A., Birckel E., Krieger S., Merklen C., Bottlaender L. A distinctive skin rash associated with coronavirus disease 2019? J Eur Acad Dermatol Venereol. 2020;34(6):e246–e247. doi: 10.1111/jdv.16471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ahouach B., Harent S., Ullmer A. Cutaneous lesions in a patient with COVID-19: are they related? Br J Dermatol. 2020;183(2):e31. doi: 10.1111/bjd.19168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Najarian D.J. Morbilliform exanthem associated with COVID-19. JAAD Case Rep. 2020;6(6):493–494. doi: 10.1016/j.jdcr.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maniaci A., Iannella G., Vicini C. A case of COVID-19 with late-onsetrash and transient loss of taste and smell in a 15-year-old boy. Am J Case Rep. 2020;21:e925813. doi: 10.12659/AJCR.925813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boix-Vilanova J., Gracia-Darder I., Saus C. Grover-like skin eruption: another cutaneous manifestation in a COVID-19 patient. Int J Dermatol. 2020;59(10):1290–1292. doi: 10.1111/ijd.15104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Iancu G.M., Solomon A., Birlutiu V. Viral exanthema as manifestation of SARS-CoV-2 infection: a case report. Medicine (Baltimore) 2020;99(35):e21810. doi: 10.1097/MD.0000000000021810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Paolino G., Canti V., Mercuri S.R., Querini P.R., Candiani M., Pasi F. Diffuse cutaneous manifestation in a new mother with COVID-19 (SARS-Cov-2) Int J Dermatol. 2020;59(7):874–875. doi: 10.1111/ijd.14919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moreno R.A., Villa L.M.E., Moreno V.A., Villa C.E., Aparicio M.A.M., Fontanella J.A.A. Cutaneous manifestation of COVID-19 in images: a case report. J Eur Acad Dermatol Venereol. 2020;34(7):e307–e309. doi: 10.1111/jdv.16531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cepeda-Valdes R., Carrion-Alvarez D., Trejo-Castro A., Hernandez-Torre M., Salas-Alanis J. Cutaneous manifestations in COVID-19: familial cluster of urticarial rash. Clin Exp Dermatol. 2020;45(7):895–896. doi: 10.1111/ced.14290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morey-Olivé M., Espiau M., Mercadal-Hally M., Lera-Carballo E., García-Patos V. Cutaneous manifestations in the current pandemic of coronavirus infection disease (COVID 2019) Anal Pediatr (Engl Ed) 2020;92(6):374–375. doi: 10.1016/j.anpede.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Henry D., Ackerman M., Sancelme E., Finon A., Esteve E. Urticarial eruption in COVID-19 infection. J Eur Acadf Dermatol Venereol. 2020;34(6):e244–e245. doi: 10.1111/jdv.16472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sousa Gonçalves C., Reis Carreira N., Passos D. Erythematous papular rash: a dermatological feature of COVID-19. Eur J Case Rep Intern Med. 2020;7(7):001768. doi: 10.12890/2020_001768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fernandez-Nieto D., Ortega-Quijano D., Segurado-Miravalles G., Pindado-Ortega C., Prieto-Barrios M., Jimenez-Cauhe J. Comment on: cutaneous manifestations in COVID-19: a first perspective. Safety concerns of clinical images and skin biopsies. J Eur Acad Dermatol Venereol. 2020;34(6):e252–e254. doi: 10.1111/jdv.16470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van Damme C, Berlingin E., Saussez S., Accaputo O. Acute urticaria with pyrexia as the first manifestations of a COVID-19 infection. J Eur Acad Dermatol Venereol. 2020;34(7):e300–e301. doi: 10.1111/jdv.16523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Freeman E.E., McMahon D.E., Lipoff J.B. Pernio-like skin lesions associated with COVID-19: a case series of 318 patients from 8 countries. J Am Acad Dermatol. 2020;83(2):486–492. doi: 10.1016/j.jaad.2020.05.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fernandez-Nieto D., Jimenez-Cauhe J., Suarez-Valle A. Characterization of acute acral skin lesions in nonhospitalized patients: a case series of 132 patients during the COVID-19 outbreak. J Am Acad Dermatol. 2020;83(1):e61–e63. doi: 10.1016/j.jaad.2020.04.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Duong T.A., Velter C., Rybojad M. Did Whatsapp® reveal a new cutaneous COVID-19 manifestation? J Eur Acad Dermatol Venereol. 2020;34(8):e348–e350. doi: 10.1111/jdv.16534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Landa N., Mendieta-Eckert M., Fonda-Pascual P., Aguirre T. Chilblain-like lesions on feet and hands during the COVID-19 Pandemic. Int J Dermatol. 2020;59(6):739–743. doi: 10.1111/ijd.14937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Colonna C., Genovese G., Monzani N.A. Outbreak of chilblain-like acral lesions in children in the metropolitan area of Milan, Italy, during the COVID-19 pandemic. J Am Acad Dermatol. 2020;83(3):965–969. doi: 10.1016/j.jaad.2020.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tosti G., Barisani A., Queirolo P. Skin signs resembling vascular acrosyndromes during the COVID-19 outbreak in Italy. Clin Exp Dermatol. 2020;45(6):757–758. doi: 10.1111/ced.14267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mazzotta F., Troccoli T. Acute acro-ischemia in the child at the time of COVID-19. Eur J Pediat Dermatol. 2020;30(2):71–74. [Google Scholar]
- 41.Estébanez A., Pérez-Santiago L., Silva E., Guillen-Climent S., García-Vázquez A., Ramón M.D. Cutaneous manifestations in COVID-19: a new contribution. J Eur Acad Dermatol Venereol. 2020;34(6):e250–e251. doi: 10.1111/jdv.16474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jimenez-Cauhe J., Ortega-Quijano D., Carretero-Barrio I. Erythema multiforme-like eruption in patients with COVID-19 infection: clinical and histological findings. Clin Exp Dermatol. 2020;45(7):892–895. doi: 10.1111/ced.14281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Manalo I.F., Smith M.K., Cheeley J., Jacobs R. A dermatologic manifestation of COVID-19: transient livedo reticularis. J Am Acad Dermatol. 2020;83(2):700. doi: 10.1016/j.jaad.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Verheyden M., Grosber M., Gutermuth J., Velkeniers B. Relapsing symmetric livedo reticularis in a patient with COVID-19 infection. J Euro Acad Dermatol Venereol. 2020;34(11):e684–e686. doi: 10.1111/jdv.16773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kamali Aghdam M., Jafari N., Eftekhari K. Novel coronavirus in a 15-day-old neonate with clinical signs of sepsis, a case report. Infect Dis (Lond) 2020;52(6):427–429. doi: 10.1080/23744235.2020.1747634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhang Y., Cao W., Xiao M. Clinical and coagulation characteristics of 7 patients with critical COVID-2019 pneumonia and acro-ischemia. Zhonghua Xue Ye Xue Za Zhi. 2020;41(0):E006. doi: 10.3760/cma.j.issn.0253-2727.2020.0006. Article in Chinese. [DOI] [PubMed] [Google Scholar]
- 47.Alramthan A., Aldaraji W. A case of COVID-19 presenting in clinical picture resembling chilblains disease. First report from the Middle East. Clin Exp Dermatol. 2020;45(6):746–748. doi: 10.1111/ced.14243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pangti R., Gupta S., Nischal N., Trikha A. Recognizable vascular skin manifestations of SARS CoV-2 infection are uncommon in patients with skin-of-color. Clin Exp Dermatol. 2021;46(1):180–182. doi: 10.1111/ced.14421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dalal A., Jakhar D., Agarwal V., Beniwal R. Dermatological findings in SARS-CoV -2 positive patients: an observational study from North India. Dermatol Ther. 2020:e13849. doi: 10.1111/dth.13849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ho W.Y.B., Wang D., Tan L.Y.C., Bundele M.M., Tan C.H., Lim H.L.J. Two cases of cutaneous eruptions due to CoVID-19 infection in Singapore: new insights into the spectrum of clinical presentation and histopathology. J Eur Acade Dermatol Venereol. 2020;34(10):e576–e579. doi: 10.1111/jdv.16736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lu S., Lin J., Zhang Z. Alert for non-respiratory symptoms of coronavirus disease 2019 (COVID-19) patients in epidemic period: a case report of familial cluster with three asymptomatic COVID-19 patients. J Med Virol. 2020 doi: 10.1002/jmv.25776. [DOI] [PubMed] [Google Scholar]
- 52.Abasaeed Elhag S.A., Ibrahim H., Abdelhadi S. Angioedema and urticaria in a COVID-19 patient: a case report and review of the literature. JAAD Case Rep. 2020;6(10):1091–1094. doi: 10.1016/j.jdcr.2020.07.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shanshal M. COVID-19 related anagen effluvium. J Dermatolog Treat. 2020:1–2. doi: 10.1080/09546634.2020.1792400. [DOI] [PubMed] [Google Scholar]
- 54.Joob B., Wiwanitkit V. COVID-19 can present with a rash and be mistaken for dengue. J Am Acad Dermatol. 2020;82(5):e177. doi: 10.1016/j.jaad.2020.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Guan W., Ni Z., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kolivras A., Dehavay F., Delplace D. Coronavirus (COVID-19) infection–induced chilblains: a case report with histopathologic findings. JAAD Case Rep. 2020;6(6):489–492. doi: 10.1016/j.jdcr.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Maiti A.K. The African-American population with a low allele frequency of SNP rs1990760 (T allele) in IFIH1 predicts less IFN-beta expression and potential vulnerability to COVID-19 infection. Immunogenetics. 2020;72(6-7):387–391. doi: 10.1007/s00251-020-01174-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Espinel, Danielle P.G.S., Di Giacomo T.B. Analysis of serum levels and cutaneous expression of lipoprotein (a) in 38 patients with livedoid vasculopathy. J Cutan Pathol. 2017;44(12):1033–1037. doi: 10.1111/cup.13043. [DOI] [PubMed] [Google Scholar]
- 59.Criado P.R., Pagliari C., Carneiro F.R.O., Quaresma J.A.S. Lessons from dermatology about inflammatory responses in Covid-19. Rev Med Virol. 2020;30(5):e2130. doi: 10.1002/rmv.2130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Criado P.R., Espinell D.P.S., Barreto P., Di Giacomo T.H.B., Sotto M.N. Lipoprotein(a) and livedoid vasculopathy: a new thrombophilic factor. Med Hypotheses. 2015;85(5):670–674. doi: 10.1016/j.mehy.2015.08.009. [DOI] [PubMed] [Google Scholar]
- 61.Ridker P.M., Miletich J.P., Hennekens C.H., Buring J.E. Ethnic distribution of factor V Leiden in 4047 men and women. Implications for venous thromboembolism screening. JAMA. 1997;277(16):1305–1307. [PubMed] [Google Scholar]
- 62.Criado P.R., Abdalla B.M.Z., de Assis I.C., van Blarcum de Graaff Mello, Cristina, Caputo G.C., Vieira I.C. Are the cutaneous manifestations during or due to SARS-CoV-2 infection/COVID-19 frequent or not? Revision of possible pathophysiologic mechanisms. Inflamm Res. 2020:1–12. doi: 10.1007/s00011-020-01370-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gianotti R., Zerbi P., Dodiuk-Gad R.P. Clinical and histopathological study of skin dermatoses in patients affected by COVID-19 infection in the Northern part of Italy. J Dermatol Sci. 2020;98(2):141–143. doi: 10.1016/j.jdermsci.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jimenez-Cauhe J., Ortega-Quijano D., de Perosanz-Lobo D. Enanthem in patients with COVID-19 and skin rash. JAMA Dermatol. 2020;156(10):1134–1136. doi: 10.1001/jamadermatol.2020.2550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kaushik A., Parsad D., Kumaran M.S. Urticaria in the times of COVID-19. Dermatol Ther. 2020:e13817. doi: 10.1111/dth.13817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Pathania Y.S. Urticaria and COVID-19 infection: a critical appraisal. J Dermatolog Treat. 2020 doi: 10.1080/09546634.2020.1808155. [DOI] [PubMed] [Google Scholar]
- 67.Hassan K. Urticaria and angioedema as a prodromal cutaneous manifestation of SARS-CoV-2 (COVID-19) infection. BMJ Case Rep. 2020;13(7):e236981. doi: 10.1136/bcr-2020-236981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chicharro P., Rodríguez-Jiménez P., Muñoz-Aceituno E., Argila D.D., Muñoz-Hernández P., Llamas-Velasco M. SDRIFE-like rash associated with COVID-19, clinicopathological correlation. Australas J Dermatol. 2020 doi: 10.1111/ajd.13444. [DOI] [PMC free article] [PubMed] [Google Scholar]