Abstract
Objectives
The COVID-19 pandemic caused by the novel SARS-CoV-2 coronavirus has drastically altered the global realities. Harnessing national scale data from the COVID-19 pandemic may better inform policy makers in decision making surrounding the reopening of society. We examined country-level, daily-confirmed, COVID-19 case data from the World Health Organization (WHO) to better understand the comparative dynamics associated with the ongoing global pandemic at a national scale.
Study design
Observational study.
Methods
We included data from 20 countries in Europe, the Americas, Africa, Eastern Mediterranean and West Pacific regions, and obtained the aggregated daily new case data for the European Union including 27 countries. We utilized an innovative analytic approach by applying statistical change point models, which have been previously employed to model volatility in stock markets, changes in genomic data, and data dynamics in other scientific disciplines, to segment the transformed case data. This allowed us to identify possible change or turning points as indicated by the dynamics of daily COVID-19 incidences. We also employed B-spline regression models to express the estimated (predicted) trend of daily new incidences for each country’s COVID-19 disease burden with the identified key change points in the model.
Results
We identified subtle, yet different change points (translated to actual calendar days) by either the mean and variance change point model with small p-values or by a Bayesian online change point algorithm with large posterior probability in the trend of COVID-19 incidences for different countries. We correlated these statistically identified change points with evidence from the literature surrounding these countries’ policies regarding opening and closing of their societies in an effort to slow the spread of COVID-19. The days when change points were detected were ahead of the actual policy implementation days, and in most of the countries included in this study the decision lagged the change point days too long to prevent potential widespread extension of the pandemic.
Conclusions
Our models describe the behavior of COVID-19 prevalence at a national scale and identify changes in national disease burden as relating to chronological changes in restrictive societal activity. Globally, social distancing measures may have been most effective in smaller countries with single governmental and public health organizational structures. Further research examining the impact of heterogeneous governmental responses to pandemic management appears warranted.
Keywords: COVID-19, Health policy, Incidences, B-spline trend fitting and prediction, Change point models, Confidence intervals
Highlights
-
•
Daily-confirmed, new COVID-19 case data are obtained from WHO for 20 individual countries in Europe, the Americas, Africa, Eastern Mediterranean and West Pacific regions, and for the European Union.
-
•
An innovative analytic approach that uses change point models to identify possible turning points is utilized to better understand the comparative dynamics of the pandemic at a national scale based on the data up to June 5th, 2020.
-
•
The estimated trend of daily new incidences for each country’s COVID-19 disease burden is provided and confidence intervals for average case numbers in periods between two identified turning days were obtained.
-
•
We correlated these statistically identified change points with evidence from the literature surrounding these countries’ policies regarding opening and closing of their societies in an effort to slow the spread of COVID-19.
-
•
The days when change patterns were detected were ahead of the actual policy implementation days, and in most of the countries included in this study the decision to implement a public health policy lagged the change point days too long to prevent potential widespread of the pandemic.
1. Introduction
SARS-CoV-2 is a novel coronavirus responsible for COVID-19 illness. COVID-19 infections were first detected in humans in late 2019 when a cluster of cases of pneumonia of unknown origin occurred in Wuhan, China [1]. COVID-19 causes serious morbidity and mortality. The World Health Organization (WHO) declared the disease a Public Health Emergency of International Concern on January 31, 2020 and declared it a pandemic on March 11, 2020. By March 16, 2020, the number of cases of COVID-19 outside China had increased drastically and the number of affected countries, states, or territories reporting infections to WHO was 143 [2]. During the COVID-19 pandemic, significant global COVID-19 epicenters include Italy, France, Spain, Iran, South Korea, Japan, Germany, the United States, and the initial place of the outbreak, China [3]. From January to March 2020, the United States closed its borders to travelers from China, Iran and Europe. In mid-March, the European Union closed all of its external borders to prevent further spreading of the virus [4].
Although there are different public health policy approaches to COVID-19 containment and mitigation (e.g., quarantine, curfews, lockdowns, travel restrictions, border shutdowns), the consistent theme has been to reduce interactions between unidentified infected individuals and noninfected individuals. Most national response strategies include varying levels of contact tracing and self-isolation or quarantine; promotion of public health measures such as handwashing, respiratory etiquette, and social distancing; strengthening of health facility infection control (including nursing homes and long-term care facilities); and postponement or cancellation of large-scale public gatherings [2].
Monitoring the COVID-19 incidence trends and analyzing the data will help make informed public health decisions while the global pandemic is still not under containment. A recent study [5] on the effects of non-pharmaceutical interventions (NPI) on COVID-19 using a stochastic age-structured transmission model on COVID-19 cases and mortality data in the United Kingdom (UK) revealed that restrictive measures may be required to lower the COVID-19 mortality rates and reduce excess of demand for hospital beds, especially those in the intensive care units (ICUs). To estimate the effect of very strict strategies of reducing social mixing on containing the COVID-19 in Wuhan, China, use of an age-structured susceptible-exposed-infected-removed (SEIR) model revealed that if the strict measures were prolonged to April, it would probably help to delay the pandemic peak [6]. A survival and mortality analysis of monthly United States household survey data concluded [7] that potential contagion prevention from school closures should be carefully weighted with the potential loss of health-care workers from the standpoint of reducing cumulative mortality due to COVID-19, in the absence of mitigating measures.
Although these recent works analyzed COVID-19 data for the effect of health measures, NPI, or school closures in different countries respectively, no work has been performed to detect subtle changes indicated in the data to help inform the heath policy creation while simultaneously providing preventive strategy and guidance for the future in such a pandemic. Consequently, we sought to examine whether the COVID-19 public health policies have yielded impacts on the daily trend of new cases from countries distributed across five global regions. We hypothesized that applying the proposed novel analytic approach to monitor COVID-19 surveillance data could help provide early detection of incidence change pattern and reveal the impact of public health policy implementation.
2. Methods
2.1. Data sources and the study design
This is an observational study. COVID-19 incidence data of 20 individual countries in five WHO defined regions were obtained from the WHO website (https://covid19.who.int/). These 20 individual countries were selected by these considerations: i) following the rough timeline of the outbreak of the disease: cases were first reported in China, then in other Asian countries, Europe, North America, Africa and South America; ii) the population sizes of the countries and the social-economic scales of the countries, and iii) for those we are able to research their public health policy documentations and publications. In addition, the aggregated daily new case data for the European Union including its 27 member countries were also obtained.
2.2. Analytics
To fulfill the purpose of our study, we sought to better understand how the implementation of public health policy measures at a national scale is reflected in the actual trend of the daily new cases in each respective country. Our analytic approach consisted of two parts. The first was to use a B-spline model [8] to estimate the trend of the new cases. With the daily case trend fitted by the splines, we hope to find where the potential and subtle changes are in the trend for each country. This question can be answered by using statistical change point models [[9], [10], [11]], which is the second part of our analytics. The identified change points combined with the spline-fitted trend can provide interpretation of how the change points may have provided better or sooner mandate dates for the implementation of public restrictive interventions in each country. The proposed analytics were applied to the WHO daily new cases for the period from January 2020 through May 11, 2020. In addition, we computed a 95% a confidence interval (CI) for each country’s unknown true average incidence number between the change dates using the updated incidence data from WHO until June 5th. For more details of our analytics, please refer to the Supplemental Materials.
3. Results
For the European region, we analyzed both the aggregated data for all 27 countries in the European Union (EU) and individual country level data for 6 countries: Italy, Germany, Great Britain, Spain, France, and Turkey. The motivation to analyze the aggregated data for the 27 countries in the EU is based on two considerations: i) the 50 states of the United States (US) have different approaches in this pandemic and have different healthcare systems, yet the data of US is aggregated as the country level data, therefore, examining the trend of the cases in EU as a whole economic block in comparison with the US is of interest; and ii) as a comparison to the EU, how the 6 selected countries in the EU are individually doing is of interest.
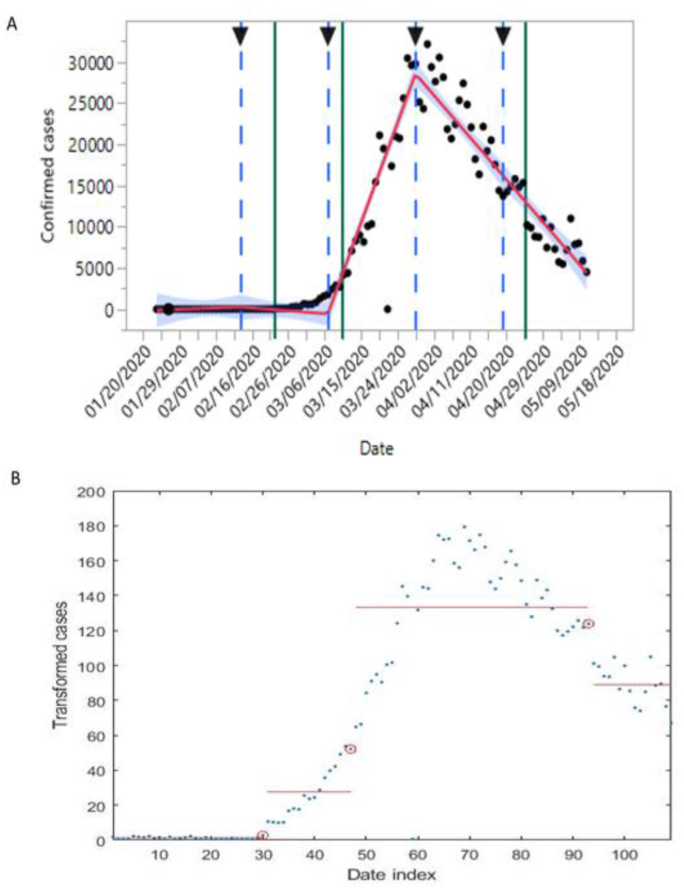
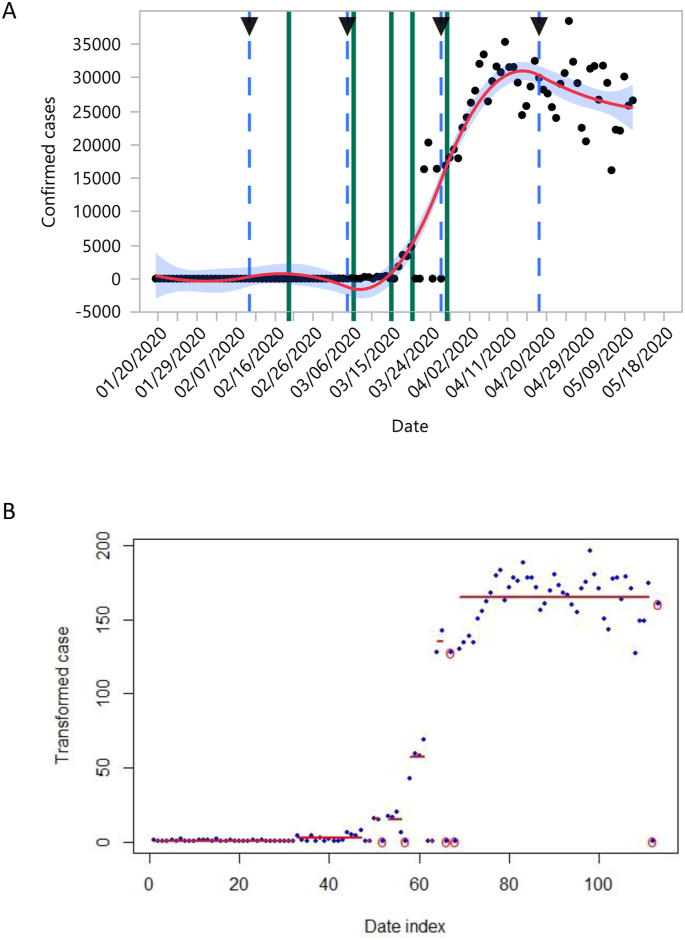
Examining various reports on the pandemic in the Europe region revealed that the first official case of COVID-19 in this region was reported in France on January 24, 2020, followed by Germany only three days later [4]. Within six weeks, all 27 countries of the European Union were affected [4]. Our analysis of the EU data provided the detailed dynamics of the incidences. Fig. 1 A illustrates the trend of daily new cases in the European Union with green vertical line segments indicating the change points (Fig. 1 B) identified by modeling the transformed cases (see Methods). The daily cases changed from a single initial case to 7 cases on Feb 22 (a change point marked as the first green vertical line (from the left) in Fig. 1 A, accumulated to 44 cases by this date). Then the newly confirmed case number begins with 113 on Feb 23 and increased to nearly 3000 on March 10 (the second identified change point). These spikes of cases in early days may have contributed to decisions made by EU member countries to implement area lockdowns or national lockdowns around March 10 (the second change point). For example, Italy’s national lockdown occurred on March 9, Germany closed schools and borders on March 13, 2020, followed by Spain on March 14th, and France on March 16, along with implemented
Fig. 1.
B-spline fitting of the trend of new daily cases for 27 countries in the European Union (panel A) with change points identified according to a change point model (panel B). In this figure and all figures hereafter, the horizontal axis in panel B represents the date index with 1 refers to the first day of observed cases for the country understudy and the vertical blue based lines in panel A are the estimated knots for the B-spline model. The three vertical green lines in panel A are marked at the change points (red cricles in panel B) identified by the mean and variance change point model with p-values respectively as 0.0000, 0.0000, and 0.0029. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
measures such as social distancing [4]. France started a national lockdown on March 17th [12]. The daily cases continued to go up because of the wide spread of the virus accumulated to that point. After reaching the peak around March 28 (the blue dashed line in Fig. 1 A), the cases started to go downward and by April 26 (another change point identified as the third green vertical segment on Fig. 1 A) the daily cases had the smallest increase thus showing the gradual containment of the cases after April 26th in European Union countries. Arguably, if the closure policy was implemented when the first change point (Feb 23rd) occurred, the curve would have been flattened much faster. Of course, when the actual lockdown or closure policy was implemented at the second change point (on March 10), it still prevented a potentially much taller curve than the actual curve. It is reassuring to see that the trend of cases was going down slowly after the third change point on April 25. This could be partly due to the functional health care system in European Union countries and various public policy measures installed during the pandemic. The change dates detected and discussed above for the European Union are summarized in column 2 of Table 1, along with other countries’ change dates detected by our method. The earliest implementation date of public health policy, such as lock-down, border closing, travel bans, social distancing, etc., are given in column 3. The red font date for a country indicates that the policy implementation date is behind the first change point detected for that country. The CIs for the different periods, segmented by the detect change dates, are summarized in Table 2 for all countries. From Table 2, one can observe that for European Union, the last CI from April 26 (after the last change pointed detected on April 25th) to June 5th is narrower than the CI in the previous period between 2 change points (March 10 and April 25). It echoed the downturn indicated in Fig. 1A, moreover, the CI gives the estimated average incidence number in the interval of (6964, 8972), in comparison with CI of (15129, 20540) for the previous period from March 11 to April 25, indicating a slow downturn for European Union and the containment has a long way to go.
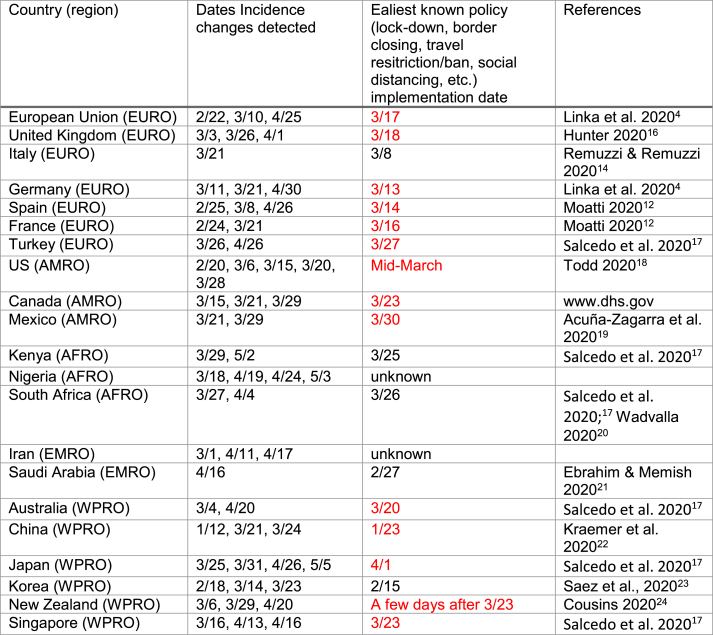
Table 1.
Table 2.
The estimated 95% confidence intervals (CIs) for each country. The first CI for a country is computed using data from the first day of incidences for that country to the first change point date, the next CI is between the first and second change point dates, etc., and the last CI is from the last change point date to June 5. When the last interval is red, it indicates an upward case trend and when the last interval is green, it indicates a downward trend for that country beyond June 5. All confidence limits were rounded to the nearest whole number except the first interval for which one decimal point is kept as the first CI usually starts with 0 followed by a single digit number of cases at the beginning.
Our analysis shows that the daily new COVID-19 cases of European countries such as Italy, Germany, Spain, and France all have similar trends (see Supplemental Figures 1-4, respectively) to the trend of the combined European Union countries (Fig. 1) while the downward trend was more obvious in Germany and France than in Fig. 1. The 95% CIs, provided in Table 2, gives the range of average case number for Italy, Germany, Spain, and France, respectively, for each of their last period (from the last change point date to June 5), but the downturn is not that obvious for Italy and France yet. In fact, on March 8th, 2020 the Italian Government implemented extraordinary measures to limit viral transmission, including restricting movement in the Lombardy region [13,14]. Italy introduced a national lockdown on March 8, 2020 [4,15]. From its European origin in Italy, the novel coronavirus spread rapidly via global mobility patterns of air passenger travel to Germany, Spain, and France [4]. Germany implemented school and border closures beginning March 13, 2020 [4]. Spain followed on March 14th, and France on March 16th. France implemented a lockdown of the country on March 17th [14]. By March 18, 2020, more than 250 million people in Europe were in lockdown [4].
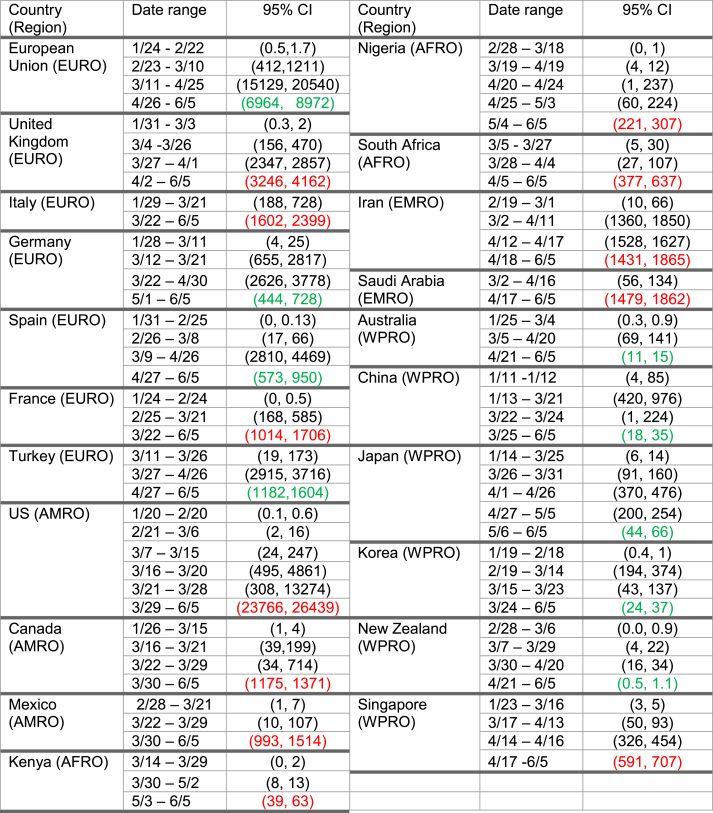
The UK had its first two COVID-19 cases recorded on January 31 according to the WHO database. The initial focus of the UK public health policy was on the identification of people infected with SARS-Cov-2, contact tracing, and isolation of people with proven exposure [16]. In the first two weeks of March, concerns were raised about government inaction, including a failure to shut down sporting and racing events [16]. Our analysis showed that the observed first spike occurred around March 3 (as indicated by the change point detection method, the first green vertical line on the trend plot (Fig. 2 A), and the schools were officially closed on March 18, 2020 [16]. In the window between March 26 and April 1, the cases dramatically increased, indicated by the two change points (the second and third circle in Fig. 2 B or the second and third vertical green lines on Fig. 2 A). Factors that contributed to the acceleration of dissemination in March included continued importation of the virus by travelers infected elsewhere; attendance at professional and social events; introduction of the virus into facilities or settings prone to amplification such as long-term care facilities and high-density urban areas; and challenges in virus detection [25]. Beyond April 1st (the last detected change point for the UK, see Table 1), the trend was not having any obvious downturn. The last 95% CI for the UK from April 2 to June 5, was (3246, 4162) (see Table 2), showing that the average incidence number is still not going down.
Fig. 2.
B-spline fitting of the trend of new daily cases for the United Kingdom (A) with change points identified according to a change point model (B). The three vertical green lines in panel A are the change points (red cricles in panel B) identified by the mean and variance change point model with p-values respectively as 0.0000, 0.0000, and 0.0015. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
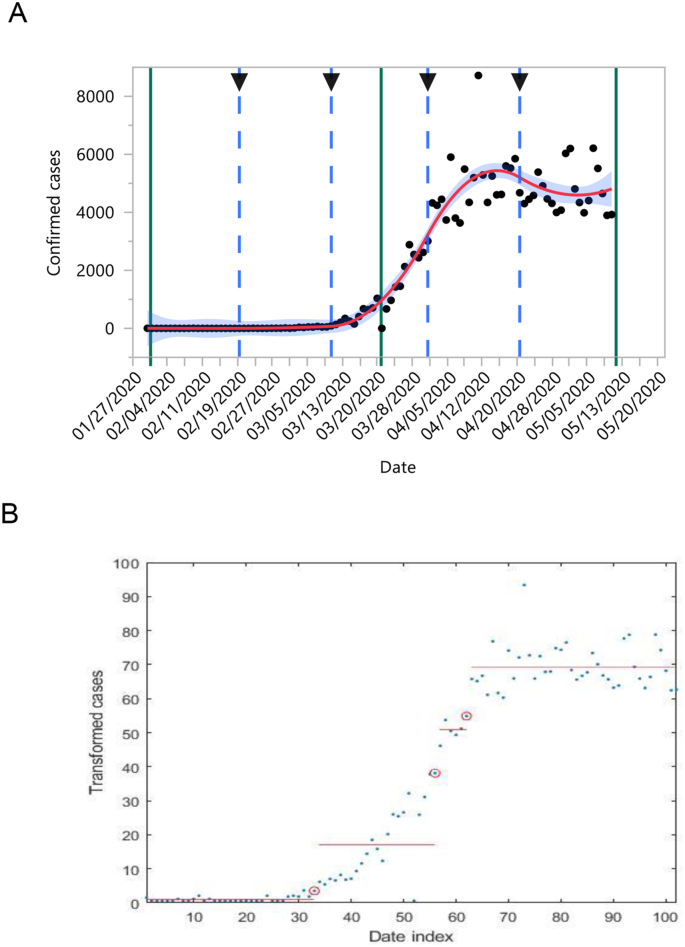
In the Americas region, the United States (US) identified its first confirmed case on January 20 [26]. By mid-March, all 50 states, the District of Columbia and four US territories had reported cases of COVID-19 [27]. The number of daily new cases were in single digits for about a month until the first change point was detected on February 20 (the first vertical green line, Fig. 3 A). The cases increased to 19 beginning February 21 and continued with two-digits until March 6; and then increased to three-digits on March 9 (three days later than the second detected change point on March 6, or the second vertical green line, Fig. 3 A). After March 15 (the third vertical green line, Fig. 3 A) the cases moved upward and quickly escalated after March 20 (the fourth vertical green line, Fig. 3 A) from three-digits to four-digits. Beyond March 28 (the fifth vertical green line, Fig. 3 A), the cases continuously lingered in the 5-digit number range until May 11. The trend in Fig. 3 A shows that beyond May 11th the cases were not clearly entering a downturn phase in the US. At the time of this writing, we continue to see daily 5-digit new case numbers for the United States recorded in the WHO database. It was noted that in the United States, the initial public health measures to contain the epidemic included the identification of cases and contacts of persons with COVID-19, and the assessment, monitoring, and care of travelers arriving from areas with substantial COVID-19 transmission.28 These measures did not prevent the widespread transmission of the virus in the United States but may have slowed the spread of illness while providing additional time to better prepare state and local health departments, health care systems, businesses, educational organizations, and the general public [28]. By April, the governors of 21 states had issued statewide stay-at-home orders to reduce the spread of COVID-19, and officials in 15 additional states ordered similar city- or county-wide shutdowns [18]. These social distancing policies in different states may have aided in slowing the spread of the COVID-19. The last 95% CI for the average case number of the United States, from March 29 to June 5, ranges from 23,766 to 26,439 (see Table 2), which echoes the observed trend in Fig. 3 A, that there is no obvious downturn yet.
Fig. 3.
B-spline fitting of the trend of new daily cases for the United States of America (A) with change points identified according to a change point model (B). The five vertical green lines are marked at the change points (red cricles in panel B, adjacent circles were grouped together) identified by the online change point detection algorithm with posterior probability respectively as 0.7015, 0.6729, 0.7638, 0.9496, and 0.8879. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
For the results of our analysis of incidence data of Turkey, Canada, Mexico, Kenya, Nigeria, South Africa, Iran, Saudi Arabia, China, Korea, Japan, Korea, Australia and New Zealand, please refer to the Supplemental Materials.
In summary, Table 1 reveals that there seems to be a long lag between the implementation dates of the policies and the detected change dates in the countries included in this study. If the health policy were made by the early detected date of the changing pattern of incidences, the cases may have been contained earlier. The confidence interval (CI) estimates given in Table 2 are useful in the current pandemic as multiple organizations are collecting COVID-19 incidence data and those data do not necessarily compeletly match due to different data sources, how the data were gathered, recording errors, etc. The last CI, from the last detected change date to June 5th, gives a range of what the average incidence number was for a country. If the last CI is wider than the CI interval in the proceeding period, it indicates that the disease is not yet contained for that country as of June 5th, or if the two ends of the last CI are still of two or more digits, the situation is not optimistic for the country. These results indicate that earlier implementation of health policies can shape a better picture for the second wave of the pandemic and any future pandemic.
4. Discussion
Our analytics approach for the daily COVID-19 data demonstrated that the change point detection methods can be very useful in identifying subtle changes in the incidence trend. Unlike other methods that have been used in epidemic modeling, the online change point detection algorithm can provide the posterior probability of the next day being a possible change point or not when new daily data become available. It can be useful to predict future changes when the pandemic is still with us based on past observed data and future incoming data.
The results indicate that public health policy measures instituted by countries in different regions of the world yielded varying successes in flattening their national COVID-19 epidemic curves. The goals of containment and mitigation measures are to delay major surges of patients requiring in-hospital care, preserving adequate hospital resources such as ventilators, while simultaneously protecting vulnerable people (e.g., those with comorbidities and the elderly). When the total number of cases in a country is small, containment measures such as isolation and contact tracing may be successful in slowing or eliminating the spread of COVID-19. However, once the number of cases exceeds a certain threshold, mitigation measures become necessary to delay patient surges and flatten epidemic curves. China’s approach to the COVID-19 outbreak exceeded the classic definition of local confinement, lockdown, and isolation [3]. The extraordinary community measures taken in Wuhan are unlikely to be replicated elsewhere [14].
The positive experience of South Korea was due to extensive contact tracing and use of mobile apps to monitor people who were quarantined. The measures taken by South Korea appears to have flattened the epidemic curve prior to any other country (roughly 10–15 days after the outbreak) [23]. Additionally, the stringent lockdown policies adopted in China, Italy, and Spain were among the most effective national-scale policies we reviewed [29].
In Italy, the National Healthcare Service suffered financial cuts of more than 37 billion Euros over the period 2010–2019; the healthcare system in Italy is decentralized and fragmented [30]. Inadequate national coordination likely restricted timely interventions and effectiveness [30]. Another important issue is the capacity of a country’s health care infrastructure. In addition, the extent of international air travel varies across countries (e.g., more limited air travel in large parts of Africa) possibly influencing the slower spread of the pandemic across many African countries.
With respect to limitations, COVID-19 case data have uncertainties due to differences in testing, inconsistent diagnostics, incomplete and under counting, and delayed reporting across countries [4]. This is a retrospective observational study on how the health policy implementation is related to the actual subtle changes in the incidence data of the pandemic. Policy interventions are not straight forward to examine as there is no control group to use. The conclusions are applicable to only the countries listed in this research. The analytics can be used to analyze the incidence data for other countries which remain to be done.
5. Conclusions
The application of statistical techniques historically applied to financial markets and bioinformatics allows for detection of subtle changes in COVID-19 incidence trends at a national level. When combined with health policy intervention data, we observe the effectiveness of these measures in preventing increases in COVID-19 burden. Globally, social distancing measures may have been most effective in smaller countries with single governmental and public health organizational structures. Further research examining the impact of heterogeneous governmental responses to pandemic management appears warranted.
CRediT authorship contribution statement
Steven S. Coughlin: Writing - original draft, review & editing, led the manuscript writing. Ayten Yiǧiter: Formal analysis, Writing - original draft, coded the programs and ran the computation & analytics. Hongyan Xu: Data curation, Writing - original draft, did data processing and made the figures. Adam E. Berman: Writing - original draft, review & editing. Jie Chen: Writing - original draft, review & editing, Formal analysis, conceived the study, coded the programs and ran the computation & analytics, led the manuscript writing. All authors participated in the planning of this research.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.puhip.2020.100064.
Contributor Information
Adam E. Berman, Email: ABERMAN@augusta.edu.
Jie Chen, Email: jiechen@augusta.edu.
Funding
None.
Ethical approval
Not required.
Data sharing
Data are available at WHO COVID-19 data map: https://covid19.who.int/
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Salzberger B., Gluck T., Ehrenstein B. Successful containment of COVID-19: the WHO-report on the COVID-19 outbreak in China. Infection. 2020;48:151–153. doi: 10.1007/s15010-020-01409-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bedford J., Enria D., Gisecke J., et al. COVID-19: towards controlling of a pandemic. Lancet. 2020;395:1015–1017. doi: 10.1016/S0140-6736(20)30673-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khosrawipour V., Lau H., Khosrawipour T., et al. Failure in initial stage containment of global COVID-19 epicenters. Med Virol. 2020:1–5. doi: 10.1002/jmv.25883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Linka K., Peirlinck M., Costabal F.S., et al. Outbreak dynamics of COVID-19 in Europe and the effect of travel restrictions. Comput. Methods Biomech. Biomed. Eng. 2020 Aug;23(11):710–717. doi: 10.1080/10255842.2020.1759560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davies NG, Kucharski AJ, Eggo RM, Gimma A. Effects of non-pharmaceutical interventions on COVID-19 cases, deaths, and demand for hospital services in the UK: a modelling study. Lancet Public Health. 2020 Jul;5(7):e375–e385. doi: 10.1016/S2468-2667(20)30133-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prem K, Liu Y, Russell TW, Kucharski AJ, Eggo RM, Davies N. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health. 2020 May;5(5):e261–e270. doi: 10.1016/S2468-2667(20)30073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bayham J, Fenichel EP. May. Impact of school closures for COVID-19 on the US health-care workforce and net mortality: a modelling study. Lancet Public Health. 2020;5(5):e271–e278. doi: 10.1016/S2468-2667(20)30082-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eilers P.H.C., Marx B. Flexible smoothing with B-splines and penalties. Stat. Sci. 1996;11(2):89–121. [Google Scholar]
- 9.Chen J., Gupta A.K. ” second ed. Birkhauser, and copyrighted by Springer Science+Business Media LLC; New York: 2012. Parametric Statistical Change Point Analysis - with Applications to Genetics, Medicine, and Finance. [Google Scholar]
- 10.Chen J., Wang Y.P. A statistical change point model approach for the detection of DNA copy number variations in array CGH data. IEEE ACM Trans. Comput. Biol. Bioinf. 2009;6:529–541. doi: 10.1109/TCBB.2008.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yiğiter A., Chen J., An L., Danacioğlu N. An online copy number variant detection method for short sequencing reads. J. Appl. Stat. 2015;42(7):1556–1571. [Google Scholar]
- 12.Moatti J.-P. The French response to COVID-19: intrinsic difficulties at the interface of science, public health, and policy. Lancet. 2020;5:e255. doi: 10.1016/S2468-2667(20)30087-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lazzerini M., Putoto G. COVID-19 in Italy: momentous decisions and many uncertainties (letter) Lancet. 2020;8:e641. doi: 10.1016/S2214-109X(20)30110-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Remuzzi A., Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395:1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Saglietto A., D’Ascenzo, Zoccai G.B., et al. COVID-19 in Europe: the Italian lesson (letter) Lancet. 2020;395:1110–1111. doi: 10.1016/S0140-6736(20)30690-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hunter D.J. COVID-19 and the stiff upper lip—the pandemic response in the United Kingdom. N. Engl. J. Med. 2020;382(1–3):e31. doi: 10.1056/NEJMp2005755. [DOI] [PubMed] [Google Scholar]
- 17.Salcedo A., Yar S., Cherelus G. The New York Times; 2020. Coronavirus Travel Restrictions, across the Globe.https://www.nytimes.com/article/coronavirus-travel-restrictions.html June 8. [Google Scholar]
- 18.Todd B. The United States responds to COVID-19. Ventilators, masks, and tests are in short supply. 2020;120:15. [Google Scholar]
- 19.Acuña-Zegarra M.A., Santana-Cibrian M., Velasco-Hernandez J.X. Modeling behavioral change and COVID-19 containment in Mexico: a trade-off between lockdown and compliance. Math. Biosci. 2020;325:108370. doi: 10.1016/j.mbs.2020.108370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wadvalla B.-A. Covid-19: decisive action is the hallmark of South Africa’s early success against coronavirus. BMJ. 2020;369:1623. doi: 10.1136/bmj.m1623. [DOI] [PubMed] [Google Scholar]
- 21.Erahim S.H., Memish Z.A. Saudi Arabia’s drastic measure to curb the COVID-19 outbreak: temporary suspension of the Umrah pilgrimage. J. Trav. Med. 2020:1–2. doi: 10.1093/jtm/taaa029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kraemer M.U.G., et al. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020;368(6490):493–497. doi: 10.1126/science.abb4218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saez M., Tobias A., Varga D., et al. Effectiveness of the measures to flatten the epidemic cure of COVID-19. Case Spain. Sci. Total Environ. 2020;727:138761. doi: 10.1016/j.scitotenv.2020.138761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cousins S. New Zealand eliminates COVID-19. Lancet World Rep. 2020;395(10235):P1474. doi: 10.1016/S0140-6736(20)31097-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schuchat A. Public health response to the initiation and spread of pandemic COVID-19 in the United States. MMWR (Morb. Mortal. Wkly. Rep.) 2020;69:551–556. doi: 10.15585/mmwr.mm6918e2. February 24—April 21, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Holshue M.L., DeBolt C., Lindquist S., et al. First case of 2019 novel coronavirus in the United States. N. Engl. J. Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.CDC COVID-19 Response Team Geographic differences in COVID-19 cases, deaths, and incidence—United States. MMWR (Morb. Mortal. Wkly. Rep.) 2020;69:465–471. doi: 10.15585/mmwr.mm6915e4. February 12—April 7, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jernigan D.B. Update: public health response to the coronavirus disease 2019 outbreak—United States. MMWR (Morb. Mortal. Wkly. Rep.) 2020;69:216–219. doi: 10.15585/mmwr.mm6908e1. February 24, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dehkordi A.H., Alizadeh M., Derakhshan P., et al. Understanding epidemic data and statistics: a case study of COVID-19. Med Virol. 2020:1–15. doi: 10.1002/jmv.25885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Armocida B., Formenti B., Ussai S., et al. The Italian health system and the COVID-19 challenge (letter) Lancet. 2020;5:e253. doi: 10.1016/S2468-2667(20)30074-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.