Abstract
Aims
The recent coronavirus disease 19 (COVID‐19) pandemic outbreak forced the adoption of restraint measures, which modified the hospital admission patterns for several diseases. The aim of the study is to investigate the rate of hospital admissions for heart failure (HF) during the early days of the COVID‐19 outbreak in Italy, compared with a corresponding period during the previous year and an earlier period during the same year.
Methods and results
We performed a retrospective analysis on HF admissions number at eight hospitals in Italy throughout the study period (21 February to 31 March 2020), compared with an inter‐year period (21 February to 31 March 2019) and an intra‐year period (1 January to 20 February 2020). The primary outcome was the overall rate of hospital admissions for HF. A total of 505 HF patients were included in this survey: 112 during the case period, 201 during intra‐year period, and 192 during inter‐year period. The mean admission rate during the case period was 2.80 admissions per day, significantly lower compared with intra‐year period (3.94 admissions per day; incidence rate ratio, 0.71; 95% confidence interval [CI], 0.56–0.89; P = 0.0037), or with inter‐year (4.92 admissions per day; incidence rate ratio, 0.57; 95% confidence interval, 0.45–0.72; P < 0.001). Patients admitted during study period were less frequently admitted in New York Heart Association (NYHA) Class II compared with inter‐year period (P = 0.019). At covariance analysis NYHA class was significantly lower in patients admitted during inter‐year control period, compared with patients admitted during case period (P = 0.014).
Conclusions
Admissions for HF were significantly reduced during the lockdown due to the COVID‐19 pandemic in Italy.
Keywords: Heart failure, COVID‐19, Hospitalization, Pandemic
Introduction
In December 2019, a cluster of viral pneumonia cases emerged in Wuhan, Hubei, China, caused by a new RNA beta‐coronavirus, named severe acute respiratory syndrome—coronavirus 2 (SARS‐CoV‐2). 1 , 2 The infection sustained by SARS‐CoV‐2 has been named coronavirus disease 19 (COVID‐19), and it was then classified as pandemic by the World Health Organization (WHO), imposing the adoption of tight restraint measures worldwide, such as social distancing and prohibition to attend public milieu, which had forced people to stay at home.
In Italy, after the infectious diseases spread and diffused, a national government lockdown was adopted. 3 Lockdown measures and the conversion of several hospitals in specific centres to treat only COVID‐19 patients brought to a drastic reduction of non‐COVID‐19 specialist outpatient performances. Moreover, during lockdown period, a change in hospital admission patterns for other diseases, such as cardiovascular disease, has been observed. 4 , 5 , 6 , 7 Although these measures are decisive for infection control, their impact on non‐COVID‐19‐related life‐threatening medical conditions is yet unknown.
Heart failure (HF) represents an important health problem with a prevalence around 1–2% in industrialized countries with a peak ≥10% in individuals aged more than 70 years. 8 , 9 , 10 At 1 year, hospitalization rates were 32% for patients with ambulatory managed HF and 44% for HF hospitalized patients, while the rate for all‐causes mortality were 7% and 17%, respectively. 11 , 12 , 13 HF patients represent a frail population, prone to frequent recurrences and destabilization, with worse outcome for COVID‐19. 13 , 14 Because of frequent re‐activation and clinical deterioration, HF patients cannot access to the routinely outpatients check‐up, during the lockdown period, being able to reveal a worse outcome that appears to be particularly impacted by COVID‐19 outbreak and associated lockdown.
In this context, we hypothesize that hospitalization rates for HF have changed in response to measures to control COVID‐19 pandemic. The aim of the present study was to evaluate hospitalization rates for HF during COVID‐19 pandemic, from the day after the first confirmed case in Italy (21 February 2020) to 31 March 2020, compared with the period of 2020 before the first confirmed case of COVID‐19, from 1 January to 20 February 2020, and with the same period of 2019, from 21 February to 31 March.
Methods
The present is a multicentre, observational, retrospective study. The aim was to retrospectively assess HF‐related hospitalization rates in eight hospitals in Italy, during early days of COVID‐19 outbreak (i.e. 20 February 2020), compared with a corresponding period, during the previous year, and an earlier period, during the same year.
Study protocol
Three periods were identified:
The case period, from the day after the first confirmed case of COVID‐19 in Italy, that is 21 February, until 31 March 2020.
An ‘intra‐year’ control period, from 1 January to 20 February 2020.
An ‘inter‐year’ control period, from 21 February to 31 March 2019.
Incidence rate (IR) of HF hospitalization during Italian outbreaks of COVID‐19 was the primary endpoint. Hospitalization rates for HF were compared between the case‐period and the two control periods.
Consecutive patients admitted for HF in participating centres >18 years old were included in the present study.
Epidemiological and clinical [i.e. age, gender, HF aetiology, percentage of HF hospitalization episode, and ejection fraction (EF)] data were retrospectively retrieved by checking clinical records, and hospital discharge letters were obtained from electronic database developed in each hospital, and study investigators carefully checked them. HF was identified by definition of current guidelines. 8 The study protocol was approved by ethical committee of Policlinico Umberto I (n.5838). The study was conducted according to the Declaration of Helsinki.
Statistical analysis
Categorical variables were reported as percentages, while continuous variables were reported as median (interquartile range) or mean (standard deviation). Continuous variables were compared using t test, while categorical variables were compared using χ 2 test.
Incidence rates for the primary outcome (HF‐related hospitalizations) were calculated by dividing the number of cumulative events by the number of days for each time period. Incidence‐rate ratios (IRRs) comparing the case period to each of the control periods were calculated using Poisson regression to model the number of HF‐related hospitalizations per day, accounting for potential clustering effect by hospital centres. P values <0.05 were considered statistically significant. Statistical analysis was performed using SPSS 24 (IBM Corporation, Armonk, NY, USA) and R Studio version 3.3.0. For the confounding variables age, male sex, and heart failure with reduced EF (HFrEF)/heart failure with preserved EF (HFpEF), we performed the analysis of covariance (ANCOVA).
Results
A total of 505 patients admitted in eight hospitals in Italy with diagnosis of HF were included in this study. During the case period, from 21 February to 31 March 2020, the HF patients were 112. Of these, 57 (50.89%) were male, the mean age (±SD) was 76 ± 19 years, 45 (40.1%) were at their first HF episode, and the aetiology was ischaemia in 47 (41.9%) patients. Regarding New York Heart Association (NYHA) class, 12 (10.7%), 59 (52.6%), and 39 (34.8%) were in Classes II, III, and IV, respectively. The mean (±SD) biplane EF was 39% (±11) (Table 1 ).
Table 1.
Characteristics of patients admitted for heart failure during the study period (21 February to 31 March 2020) as compared with intra‐year (1 January to 20 February 2020) and inter‐year (21 February to 31 March 2019) control periods
| Study period (N = 112) | Control period | P value | ||
|---|---|---|---|---|
| Same year (N = 201) | Previous year (N = 192) | |||
| Age (±SD) | 76 (±19) | 78 (±10.94) | 0.238 | |
| 79 (±10.87) | 0.080 | |||
| Gender, male | 57 (50.9%) | 113 (56.2%) | 0.400 | |
| 115 (59.8%) | 0.150 | |||
| NYHA class | ||||
| I | 2 (<1%) | 1 (<1%) | 1.000 | |
| 15 (7.5%) | 0.058 | |||
| II | 12 (10.7%) | 31 (15.4%) | 0.304 | |
| 42 (21.3%) | 0.019 | |||
| III | 59 (52.6%) | 88 (43.7%) | 0.130 | |
| 79 (41.1%) | 0.056 | |||
| IV | 39 (34.8%) | 81 (40.2%) | 0.396 | |
| 56 (29.1%) | 0.308 | |||
| Hospitalization, 1st episode | 45 (40.1%) | 83 (41.2%) | 0.904 | |
| 94 (46.7%) | 0.153 | |||
| LVEF, % (±SD) | 39 (±11) | 43 (±13) | 0.015 | |
| 42 (±13) | 0.034 | |||
| HFpEF | 33 (29.4%) | 77 (38.3%) | 0.792 | |
| 59 (30.7%) | 0.138 | |||
| HFrEF | 79 (70.5%) | 124 (61.6%) | 0.260 | |
| 133 (69.2%) | 0.138 | |||
| HF aetiology, ischemic | 47 (41.9%) | 86 (42.7%) | 0.905 | |
| 85 (44.2%) | 0.720 | |||
| In‐hospital mortality | 10 (<1%) | 13 (<1%) | 0.498 | |
| 9 (<1%) | 0.148 | |||
LVEF, left ventricular ejection fraction; NYHA, New York Heart Association; HF, heart failure; HFpEF, heart failure with preserved (>50%) ejection fraction; HFrEF, heart failure with reduced (<50%) ejection fraction; SD, standard deviation.
During the case period, the mean daily admission was 2.80 hospitalizations per day. This rate was significantly lower when compared with the two control periods. In particular, during inter‐year control period, a total of 192 patients were admitted {IRR case period vs. inter‐year control period: 0.57 [95% confidence interval (CI) 0.45–0.72] P <0.001; mean daily admission: 4.92 hospitalization per day}, while during intra‐year control period, a total of 201 patients were admitted [IRR case period vs. intra‐year control period: 0.71 (95% CI 0.564–0.89) P = 0.003; mean daily admission: 3.94 hospitalization per day] (Figure 1 and Table 2 ). The participant centres and the number of HF admission of each hospital and period are listed in Table 3 . Patients admitted during the study period were comparable with those admitted during intra‐year and inter‐year control periods, in terms of age, gender, percentage of first episode of HF, preserved EF, aetiology (i.e. ischemic and non‐ischemic), and in‐hospital mortality (Table 1 ). Regarding NYHA classes, during the study period, patients were less frequently admitted in Class II compared with inter‐year period (P = 0.019). This difference in terms of NYHA class is independent from the ischemic aetiology of HF (Table 4 ). Moreover, EF was lower in patients admitted during study period, compared with intra‐year period (43 ± 13; P = 0.015) and with inter‐year period (42 ± 13; P = 0.034) (Table 1 ). We performed the covariance analysis to evaluate whether the variable period influences the results of EF and NHYA class, considering the confounding variables as age, male sex, and HFrEF/HFpEF ratio. About that, we observed that the parameter NYHA class showed statistically significant differences between the case period and inter‐year control period (P = 0.014). In particular, patients admitted during inter‐year control period showed a lower NYHA class compared with patients admitted during case period. Regarding NYHA class, no statistically significant differences have been observed between the case period and intra‐year control period (P = 0.29). No statistically significant differences have been observed regarding EF between the case period and inter‐year control period (P = 0.83) and between the case period and intra‐year control period (P = 0.80).
Figure 1.
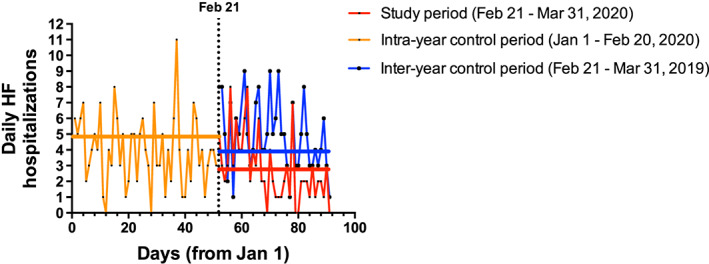
Daily heart failure hospitalizations of the study population. HF, heart failure. Red line: HF hospitalizations during the time from the first confirmed coronavirus disease 19 (COVID‐19) case (21 February 2020) to 31 March 2020 (study period). Blue line: HF hospitalizations during the time from 21 February 2019 to 31 March 2019 (inter‐year control period). Orange line: HF hospitalizations during the time from 1 January 2020 to the day before the first confirmed COVID‐19 case (20 February 2020; intra‐year control period). The vertical line represents 21 February 2020, the date of the first confirmed COVID‐19 case in Italy. The blue, orange, and red horizontal lines represent the mean daily admission of inter‐year control period, intra‐year control period, and study period, respectively.
Table 2.
Comparison of hospital admissions for heart failure in Italy between the onset of the coronavirus disease 19 outbreak and two control periods
| Study period (N = 112) | Control periods | ||
|---|---|---|---|
| Same year (N = 201) | Previous year (N = 192) | ||
| No. of daily admissions | 2.80 | 3.94 | 4.92 |
| Incidence rate ratio (95% CI) | 0.71 (0.56–0.89) | 0.57 (0.45–0.72) | |
| P value | 0.003 | <0.001 | |
The study period was defined as the time between the day after the first confirmed case of coronavirus disease 19 in Italy (20 February 2020) and 31 March 2020. The two control periods were from 1 January to 19 February 2020 (same year) and from 20 February 20 to 31 March 2019 (previous year). The 95% confidence intervals (CIs) are not adjusted for multiple testing and therefore should not be used to infer definitive effects.
Table 3.
Representation of participant centres to the study with the number of heart failure admission for each centre and period and number of mean daily admission
| Hospital | Region | Number of admission (mean daily admission) | Total admission/hospital | ||
|---|---|---|---|---|---|
| Inter‐year period a | Intra‐year period a | Case period a | |||
| Sapienza University of Rome, Rome | Lazio | 26 (0.66) | 24 (0.47) | 14 (0.35) | 64 |
| M.G. Vannini Hospital, Rome | Lazio | 6 (0.15) | 7 (0.14) | 5 (0.12) | 18 |
| Grande Ospedale Metropolitano Niguarda, Milan | Lombardy | 63(1.61) | 94 (1.84) | 30 (0.75) | 187 |
| S. Andrea Hospital, Vercelli | Piedmont | 6 (0.15) | 4 (0.078) | 3 (0.075) | 13 |
| A.O.U. Senese, Policlinico Le Scotte, Siena | Tuscany | 34 (0.87) | 0 (0) | 25 (0.625) | 59 |
| Luigi Sacco Hospital, Milan | Lombardy | 39 (1) | 43 (0.84) | 20 (0.5) | 102 |
| Ospedale Maggiore di Novara, Novara | Piedmont | 12 (0.31) | 12 (0.23) | 6 (0.15) | 30 |
| Ivrea Hospital, Ivrea | Piedmont | 6 (0.15) | 17 (0.33) | 9 (0.22) | 32 |
| Total admission/period | 192 (4.92) | 201 (3.94) | 112 (2.8) | 505 | |
Inter‐year period (from 21 February to 31 March 2019). Intra‐year period (from 1 January to 20 February 2020) and case period (from 21 February to 31 March 2020). Mean daily admission (hospitalization per day).
Table 4.
Comparison among ischemic and non‐ischemic HF patients in term of NYHA class at hospital admission, for each period of study
| Study period (N = 112) | ||||
|---|---|---|---|---|
| NYHA Class | Ischemic HF | Non‐ischemic HF | P value | |
| I [N = 2 (<1%)] | 0 | 2 (100%) | 0.508 | |
| II [N = 12 (10.7%)] | 5 (42%) | 7 (58%) | 1 | |
| III [N = 59 (52.6%)] | 24 (41%) | 35 (59%) | 0.848 | |
| IV [N = 39 (34.8%)] | 18 (46.1%) | 21 (53.9%) | 0.55 | |
| Total | 112 | 47 (41.9%) | 65 (58.1%) | |
| Inter‐year period (N = 192) | ||||
| I [N = 15 (7.5%)] | 4 (26%) | 11 (74%) | 0.183 | |
| II [N = 42 (21.3%)] | 23 (55%) | 19 (45%) | 0.159 | |
| III [N = 79 (41.1%)] | 35 (44%) | 44 (56%) | 1 | |
| IV [N = 56 (29.1%)] | 23 (41%) | 33 (59%) | 0.632 | |
| Total | 192 | 85 (44%) | 107 (56%) | |
| Intra‐year period (N = 201) | ||||
| I [N = 1 (<1%)] | 0 | 1 (100%) | 1 | |
| II [N = 31 (15.4%)] | 14 (45%) | 17 (55%) | 0.844 | |
| III [N = 88 (43.7%)] | 38 (43%) | 50 (57%) | 1 | |
| IV [N = 81 (40.2%)] | 34 (42%) | 47 (58%) | 0.885 | |
| Total | 201 | 86 (42.8%) | 115 (57.2%) | |
HF, heart failure; NYHA, New York Heart Association.
Discussion
Heart failure represents a multifaceted syndrome, and it is associated with high rates of death and hospitalization worldwide. 10 , 11 , 12 , 13 , 14
During COVID‐19 lockdown, lifestyle and dietary modification, separation of patients from relatives, and caregivers together with an increase of health inequalities might bring to higher incidence of new cases of HF as well as HF destabilization. 15 , 16 , 17 Moreover, several cardiovascular conditions, as acute coronary syndromes, which are often related to subsequent HF occurrence, were underdiagnosed and undertreated, during lockdown period. 5 , 18 , 19
Our results suggest a significant reduction of HF hospitalization rates across cardiovascular departments in 8 hospitals in Italy, during COVID‐19 pandemic. Patients hospitalized for HF during the study period were comparable to those admitted during intra‐year and inter‐year control periods, in terms of age, gender, percentage of first episode of HF, in‐hospital mortality, and aetiology. Patients admitted during the study period showed a worse NYHA class compared with patients hospitalized during the same period in the previous year. At the same time, EF was lower in patients admitted during study period, compared with both control periods. Correcting the EF and NYHA class values for age, male sex, and HFrEF/HFpEF ratio, NYHA class was significantly lower in patients admitted during inter‐year control period compared to patients admitted during case period; no significant result was observed for EF.
Albeit the shortness of the study period, our results raise the question whether restraint measures, which were able to contrast COVID‐19 pandemic, did not prevent HF patients from receiving the diagnostic and therapeutic options. On the other hand, patients probably delayed presentation, as a result of either the fear of contracting the virus or a misinterpretation of clinical status and symptoms. 15 , 16 , 17 Interestingly, we can argue that events reduction could be related to a better self‐care and more stringent lifestyle recommendation over this period. Whereas, recent data showed a significant increase in mortality, during lockdown period in Italy, that was not fully explained by COVID‐19 cases alone. 19 In fact, in some cases, HF patients may have died at home without seeking medical attention during the COVID‐19 lockdown. Although public opinion, mass media, and healthcare systems focus on the COVID‐19, there is the need of a change in perspective facing the complex syndrome of HF. 15 , 20 , 21 , 22
In conclusion, a significant reduction in hospital admissions for HF was observed in Italy, during the early days of COVID‐19 outbreak. Similar findings have been noted in the state of Mississippi (USA). 23
Study limitations
The present observational retrospective study has some limitations owing to the difficulties in collecting clinical data during the pandemic emergency. Extensive data collection was not possible for all centres, especially during the initial phase of the pandemic. Data regarding HF presentation and subtypes during lockdown may deserve a further investigation, in order to better investigate HF‐related hospitalization and outpatient risk. The study period is short and, more importantly, the present is a retrospective observational study; thus, other prospective studies on longer period investigating the reasons for delay in contacting the hospital are required to confirm our observations. The differences, regarding data collection, among regions should be explained primarily considering the different sizes and typologies of the hospitals' cardiology departments included in the study. Another reason might be also the different spread of the virus SARS‐CoV‐2, according to the different regions, which influenced the role and the reorganization, of each hospital in the management of COVID‐19 and non‐COVID‐19 patients, during pandemic outbreak.
Conflict of interest
None declared.
Funding
None.
Acknowledgements
The conceptualization of the study was performed by P.S., M.M., and F.F. Data curation was carried out by P.S., A.D.A., A.S., F.D.A., C.M., M.S., N.G., F.P., F.T., M.C., G.A., F.I., M.P., M.M., A.R., F.R., and A.G. Formal analysis was accomplished by P.S., A.D.A., A.S., F.D.A., and M.M. The methodology was created by P.S., A.D.A., A.S., F.D.A., C.M., M.S., N.G., F.P., F.T., M.C., G.A., F.I., M.P., M.M., A.R., F.R., A.G., and M.M. Supervision was performed by G.M.D.F., L.C., W.G.M., F.U., G.F., M.V., N.M., A.P., G.P., P.J.M., and F.F. Validation was carried out by G.M.D.F., L.C., W.G.M, F.U., G.F., M.V., N.M., A.P., G.P., P.J.M., and F.F. Visualization was accomplished by G.M.D.F., L.C., W.G.M, F.U., G.F., M.V., N.M., A.P., G.P., P.J.M., and F.F. The original draft was written by P.S., A.D.A., A.S., F.D.A., and M.M. Writing review and editing were carried out by P.S., A.D.A., A.S., F.D.A, C.M. M.S., N.G., F.P., F.T., M.C., G.A., F.I., M.P., M.M., A.R., F.R., A.G., G.M.D.F., L.C., W.G.M, F.U., P.J.M., G.F., M.V., N.M., A.P., G.P., M.M., and F.F.
Severino, P. , D'Amato, A. , Saglietto, A. , D'Ascenzo, F. , Marini, C. , Schiavone, M. , Ghionzoli, N. , Pirrotta, F. , Troiano, F. , Cannillo, M. , Mennuni, M. , Rognoni, A. , Rametta, F. , Galluzzo, A. , Agnes, G. , Infusino, F. , Pucci, M. , Lavalle, C. , Cacciotti, L. , Mather, P. J. , Grosso Marra, W. , Ugo, F. , Forleo, G. , Viecca, M. , Morici, N. , Patti, G. , De Ferrari, G. M. , Palazzuoli, A. , Mancone, M. , and Fedele, F. (2020) Reduction in heart failure hospitalization rate during coronavirus disease 19 pandemic outbreak. ESC Heart Failure, 7: 4182–4188. 10.1002/ehf2.13043.
References
- 1. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395: 497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W, China Novel Coronavirus Investigating and Research Team . A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020; 382: 727–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Remuzzi A, Remuzzi G. COVID‐19 and Italy: what next? Lancet 2020; 395: 1225–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi‐Zoccai G, Brown TS, Der Nigoghossian C, Zidar DA, Haythe J, Brodie D, Beckman JA, Kirtane AJ, Stone GW, Krumholz HM, Parikh SA. Cardiovascular considerations for patients, health care workers, and health systems during the COVID‐19 pandemic. J Am Coll Cardiol 2020; 75: 2352–2371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. De Filippo O, D'Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A, Secco GG, Campo G, Gallone G, Verardi R, Gaido L, Iannaccone M, Galvani M, Ugo F, Barbero U, Infantino V, Olivotti L, Mennuni M, Gili S, Infusino F, Vercellino M, Zucchetti O, Casella G, Giammaria M, Boccuzzi G, Tolomeo P, Doronzo B, Senatore G, Grosso Marra W, Rognoni A, Trabattoni D, Franchin L, Borin A, Bruno F, Galluzzo A, Gambino A, Nicolino A, Truffa Giachet A, Sardella G, Fedele F, Monticone S, Montefusco A, Omedè P, Pennone M, Patti G, Mancone M, De Ferrari GM. Reduced rate of hospital admissions for ACS during Covid‐19 outbreak in northern Italy. N Engl J Med 2020; 383: 88–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. De Rosa S, Spaccarotella C, Basso C, Calabrò MP, Curcio A, Perrone Filardi P, Mancone M, Mercuro G, Muscoli S, Nodari S, Pedrinelli R, Sinagra G, Indolfi C. Reduction of hospitalizations for myocardial infarction in Italy in the COVID‐19 era. Eur Heart J Published online ahead of print 15 May 2020; 41: 2083–2088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Solomon MD, McNulty EJ, Rana JS, Leong TK, Ambrosy SP, Sidney S, Go AS. The Covid‐19 pandemic and the incidence of acute myocardial infarction. N Engl J Med 2020; 383: 691–693. [DOI] [PubMed] [Google Scholar]
- 8. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, González‐Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P, ESC Scientific Document Group . 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016; 37: 2129–2200. [DOI] [PubMed] [Google Scholar]
- 9. Mosterd A, Hoes AW. Clinical epidemiology of heart failure. Heart 2007; 93: 1137–1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bleumink GS, Knetsch AM, Sturkenboom MCJM, Straus SMJM, Hofman A, Deckers JW, Witteman JCM, Stricker BHC. Quantifying the heart failure epidemic: prevalence, incidence rate, lifetime risk and prognosis of heart failure The Rotterdam Study. Eur Heart J 2004; 25: 1614–1619. [DOI] [PubMed] [Google Scholar]
- 11. Maggioni AP, Dahlström U, Filippatos G, Chioncel O, Crespo Leiro M, Drozdz J, Fruhwald F, Gullestad L, Logeart D, Fabbri G, Urso R, Metra M, Parissis J, Persson H, Ponikowski P, Rauchhaus M, Voors AA, Nielsen OW, Zannad F, Tavazzi L. Heart Failure Association of the European Society of Cardiology (HFA) EURObservational Research Programme: regional differences and 1‐year follow‐up results of the Heart Failure Pi‐lot Survey (ESC‐HF Pilot). Eur J Heart Fail 2013; 15: 808–817. [DOI] [PubMed] [Google Scholar]
- 12. Crespo‐Leiro MG, Anker SD, Maggioni AP, Coats AJ, Filippatos G, Ruschitzka F, Ferrari R, Piepoli MF, Delgado Jimenez JF, Metra M, Fonseca C, Hradec J, Amir O, Logeart D, Dahlström U, Merkely B, Drozdz J, Goncalvesova E, Hassanein M, Chioncel O, Lainscak M, Seferovic PM, Tousoulis D, Kavoliuniene A, Fruhwald F, Fazlibegovic E, Temizhan A, Gatzov P, Erglis A, Laroche C, Mebazaa A. European Society of Cardiology Heart Failure Long‐Term Registry (ESC‐HF‐LT): 1‐year follow‐up outcomes and differences across regions. Eur J Heart Fail 2016; 18: 613–625. [DOI] [PubMed] [Google Scholar]
- 13. Liu PP, Blet A, Smyth D, Li H. The science underlying COVID‐19: implications for the cardiovascular system. Circulation. Published online ahead of print 15 April 2020; 142: 68–78. [DOI] [PubMed] [Google Scholar]
- 14. Severino P, Mather PJ, Pucci M, D'Amato A, Mariani MV, Infusino F, Birtolo LI, Maestrini V, Mancone M, Fedele F. Advanced heart failure and end‐stage heart failure: does a difference exist. Diagnostics (Basel) 2019; 9: 170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Vitale C, Jankowska E, Hill L, Piepoli M, Doehner W, Stefan DA, Lainscak M, Jaarsma T, Ponikowski P, Rosano GMC, Seferovic P, Coats AJ. Heart Failure Association/European Society of Cardiology position paper on frailty in patients with heart failure. Eur J Heart Fail 2019; 21: 1299–1305. [DOI] [PubMed] [Google Scholar]
- 16. Reza N, DeFilippis EM, Jessup M. Secondary impact of the COVID‐19 pandemic on patients with heart failure. Circ Heart Fail 2020; 13: e007219. [DOI] [PubMed] [Google Scholar]
- 17. Abraham WT, Fiuzat M, Psotka MA, O'Connor CM. Heart failure collaboratory statement on clinical trials in the landscape of COVID‐19. JACC Heart Fail 2020; 8: 423–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ahmad K, Chen EW, Nazir U, Cotts W, Andrade A, Trivedi AN, Erqou S, Wu WC. Regional variation in the association of poverty and heart failure mortality in the 3135 counties of the United States. J Am Heart Assoc 2019; 8: e012422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Istat L'andamento dei decessi del 2020. Dati anticipatori sulla base del sistema ANPR. March 31, 2020. https://www.istat.it/it/files/2020/03/Decessi_2020_Nota.pdf
- 20. Severino P, Mariani MV, Fedele F. Futility in cardiology: the need for a change in perspectives. Eur J Heart Fail 2019; 21: 1483–1484. [DOI] [PubMed] [Google Scholar]
- 21. Severino P, Maestrini V, Mariani MV, Birtolo LI, Scarpati R, Mancone M, Fedele F. Structural and myocardial dysfunction in heart failure beyond ejection fraction. Heart Fail Rev 2020; 25: 9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gorodeski EZ, Goyal P, Cox ZL, Thibodeau JT, Reay R, Rasmusson K, Rogers JG, Starling RC. Virtual visits for care of patients with heart failure in the era of COVID‐19: a statement from the Heart Failure Society of America. J Card Fail 2020; S1071‐9164: 30367–30365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hall ME, Vaduganathan M, Khan MS, Papadimitriou L, Long RC, Hernandez RA, Moore CK, Lennep BW, Mcmullan MR, Butler J. Reductions in heart failure hospitalizations during the COVID‐19 pandemic. J Card Fail 2020; 26: 462–463. [DOI] [PMC free article] [PubMed] [Google Scholar]


