ABSTRACT
Globally, researchers are undertaking significant efforts to design and develop effective vaccines, therapeutics, and antiviral drugs to curb the spread of coronavirus disease 2019 (COVID-19). Plants have been used for the production of vaccines, monoclonal antibodies, immunomodulatory proteins, drugs, and pharmaceuticals via molecular farming/transient expression system and are considered as bioreactors or factories for their bulk production. These biological products are stable, safe, effective, easily available, and affordable. Plant molecular farming could facilitate rapid production of biologics on an industrial scale, and has the potential to fulfill emergency demands, such as in the present situation of the COVID-19 pandemic. This article aims to describe the methodology and basics of plant biopharming, in addition to its prospective applications for developing effective vaccines and antibodies to counter COVID-19.
KEYWORDS: SARS-CoV-2, COVID-19, molecular farming, transgenic plants, vaccines, antibodies
Introduction
The coronavirus disease 2019 (COVID-19), caused by the deadly severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has spread around the globe in a short time period of 6 months. COVID-19 has caused major global health concerns, generated widespread panic, resulted in economic losses, and hampered the efforts undertaken to limit its spread.1–4 SARS-CoV-2 has infected tens of millions of people and caused the deaths of over one million. COVID-19 is the deadliest pandemic since the 1918 Spanish flu pandemic which killed nearly 50 million people.5 At present, no vaccine is available to curb the COVID-19 pandemic. A recently approved antiviral drug, remdesivir is available with limited supply; however, the drug is not affordable in developing countries. Researchers across the globe are working constantly and making extensive efforts to design and develop effective vaccines, therapeutics, and drugs to halt the spread of SARS-CoV-2 to help save the lives of millions. Few of the developed vaccines and drugs are in different stages of clinical trials; however, after their development, a substantial amount of time will be needed for the bulk production to help fulfill the requirements of countries around the globe.6–10
Apart from the major production platforms and technologies used for manufacturing vaccines, drugs, and other biologics by industries and pharmaceutical companies, plant-based production platforms have emerged as an efficient system for bulk production to keep up with the demands of the situation. Plant-based technologies, used in traditional and modern medicine for numerous diseases including infectious diseases, have the potential for developing safe, efficient, stable, and affordable prophylactics, vaccines, and drugs.11–13 Initial attempts were made to produce vaccines by expressing antibodies using tobacco plants.14 The world’s first plant-based vaccine was approved for the Newcastle disease virus (NDV) by the United States Department of Agriculture (USDA) for poultry. It was shown to confer more than 90% protection in chicken, following the challenges faced with NDV.15 The only other plant-based product licensed is the plant-made single-chain fragment variable monoclonal antibody (scFv mAb) used in the production of a recombinant Hepatitis B virus (HBV) vaccine in Cuba.16,17 Considering future prospects and demands, plant-based vaccines have the potential to revolutionize the field of vaccinology. The article highlights the development, production, and applications of plant-based vaccines and antibodies to combat COVID-19.
Plants as factories for developing biological products
Plant-based vaccines for COVID-19 can be developed either by expressing the antigenic component of SARS-CoV-2 for inducing active immunity or expressing the antibody against the virus to provide passive protection.16,17 Plant-based vaccines are considered as third-generation vaccines. The production approach of a plant-based vaccine involves cloning the vaccine candidate into a plant expression system, which is capable of promoting the expression of the candidate gene in the plant, which then produces the antigenic or protective protein. This approach enables vaccine production by using plants as bioreactors and growing them for multiple generations, thereby ensuring continuous manufacturing and availability.18–20 Plant-based systems may offer an efficient platform to produce and manufacture biological products on a large scale within a span of few weeks, compared to a longer time span of months required for cell culture-based approaches. Plants have been used for the production of vaccines, antibodies, immunomodulatory proteins, drugs, and pharmaceuticals and they are considered as bioreactors or factories that could pave way for bulk production of biological products in a timely manner.21–24
Plant expression systems are amendable, and can progress from classical expression systems to transient expression systems to suit the demands of bulk production of specific and effective biopharmaceutical proteins to help circumvent the present crisis.25 Integration of genes of interest coding for a specific antigen, which is characteristic of the disease of concern, into the genome of plant tissue for vaccine production can be achieved by various methods. These include conventional methods such as Agrobacterium-mediated gene transfer and transformation via genetically modified plant virus.16 The current advanced methods exhibit increased efficiency than the older methods, and include biolistics (nuclear transformation and chloroplast transformation), electroporation, agroinfiltration, sonication, and polyethylene glycol treatment.16,26 Microbial genes when incorporated into the plant genome are transcribed into protein antigens of the target pathogen without affecting the plant and without losing their immunogenic property.26 The mechanisms involved in initiating host immunity against the pathogen are the systemic and mucosal immune responses.26 Some vaccines are produced by direct bombardment or biolistic methods, such as the ones against cholera, Lyme disease, anthrax, tetanus, plague, rotavirus, and canine parvovirus26,27 Vaccines produced by indirect methods or Agrobacterium-mediated gene transfer include the ones targeting tuberculosis, dengue, avian flu, and Ebola viruses.28
Several plant-based biological products have reached clinical trials, with a few available commercially as medical devices and pharmaceuticals for the treatment of chronic and infectious diseases.22,24 The primary benefits of plants for producing different biological and pharmaceutical products using plant molecular pharming include cost-effectiveness and scalability, as plants can be commercially cultivated on a large scale.3,29 Plant-based vaccines could facilitate rapid production of biological products on an industrial scale and thus have potential to fulfill emergency demand, such as the current situation of the COVID-19 pandemic.23,30,31 Production of plant-based vaccines is convenient, scientifically and technically sound, economical, does not require cold storage and can be scaled up, and can help provide effective, safe, and cheap vaccines.16,32 Plant-derived biologics can also have synergistic characteristics with other conventional prophylactics and therapeutics.33
Plant-based vaccines and antibodies
Various plants such as tobacco, turnip, and potato, as well as others, have been used for the production of vaccines.19 Human interferon-α was the first recombinant plant-derived pharmaceutical proteins produced in turnip.34 Later, human serum albumin was produced in tobacco and potato for human use.35 Antibodies (scFv mAb) against hepatitis B virus were produced in tobacco and have been approved for use in Cuba.16,36 Antibodies against Streptococcus mutans were also produced in tobacco and have been approved in Europe.11 Plant-based molecular farming has been exploited during earlier epidemics and pandemics, such as the Influenza37–39 pandemic, as well as the ones that surfaced during the 21stcentury, such as HIV,40,41 Zika,42 and Ebola.43 The first drug (ZMapp) used experimentally against the Ebola virus was produced in the tobacco plant. ZMapp is a drug cocktail of antibodies that conferred protection against the Ebola virus.43 Other plant-based pharmaceutical products are insulin produced from transgenic safflower (SemBioSys)44 or potatoes,26 growth factor in transgenic barley,45 taliglucerase alfa (for the treatment of Gaucher’s disease) in transgenic carrot (ProtalixBio Therapeutics),46 avian influenza vaccine in transgenic tobacco (Medicago), and Ebola vaccine in transgenic tobacco (Mapp Biopharmaceutical).16,47,48
Potato is being used for production of vaccines against tetanus, diphtheria, hepatitis B, Norwalk virus, enteritis caused by E. coli strain, mink enteritis, and rabbit hemorrhagic virus.26,49 Rice is used for developing antibodies against E. coli.50 Tomatoes are being used for vaccine production against SARS, Norwalk virus, Vibrio cholera, pneumonia, and bubonic plagues.51 Banana is used for expressing HBsAg.52 Lettuce is used for vaccine production against E. coli-associated enteritis, swine fever, and hepatitis B virus.53 Tobacco is used for vaccine production against Norwalk virus, chicken infectious anemia, hepatitis B and coccidiosis in addition to Newcastle disease virus.54 Alfalfa has been explored for vaccine production against hog pest virus and Echinococcus granulosus.26 Carrots are useful in producing potential vaccines against HIV, E. coli, and Helicobacter pylori.51
The present scenario of the COVID-19 pandemic also needs to be considered as a challenge by researchers to exploit the potential of plant-based platforms to help design and develop effective vaccines, therapeutics, and drugs to counter COVID-19, as well as address future pandemics.
Plant-based SARS-CoV-2 vaccines
It is essential to understand SARS-CoV-2’s interaction with the host immune system in order to develop an effective vaccine against COVID-19. The interaction appears to determine the disease outcome, which can be mild, severe, or asymptomatic. In severe cases, the interaction causes over-activation of the immune system in response to potent virus-induced inflammatory stimuli which leads to excessive inflammation-mediated lung tissue injury and manifestation of acute respiratory distress syndrome (ARDS).2,55,56 A severe immune reaction in COVID-19 patients can also lead to a cytokine storm, wherein an excess of cytokines are released into circulation, leading to organ damage57,58 and severe manifestations.59 Therefore, an ideal COVID-19 vaccine should induce protective cell-mediated and humoral immunity, without inducing excessive pathological immune response.60 Development of SARS-CoV-2 subunit vaccines that utilize individual proteins as antigens in a prime-boost regimen along with an appropriate adjuvant, or as virus-like particles (VLPs) with multiple viral antigens could be useful against COVID-19.55,60,61 SARS-CoV-2’s structural proteins [spike (S), envelope (E), membrane (M) and nucleocapsid (N)] have been found to induce neutralizing antibodies (NAb) and cell-mediated (CD4+/CD8+ T cell-based immunity) immune responses.62 However, the N protein is incompatible, as it is highly conserved among the CoV families. Antibodies against N proteins are unable to render protective immunity, while those against M and E proteins provide weak protection.63 The S protein is a key target for developing effective vaccines, as the virus uses the S protein for entry into the cells through angiotensin-converting enzyme 2 (ACE2) receptor binding. The S protein is cleaved proteolytically into two subunits, namely an S1 subunit (685 amino acids) and an S2 membrane-spanning subunit (588 amino acids). The S2 subunit is highly conserved (99%) among the CoVs. S1 reveals only 70% identity to other human CoVs and the receptor-binding domain (RBD) constitutes the differences in the virus entry and host cell tropism.64 Within the S protein, the RBD is the region that engages with ACE2 receptor. The antigenic mapping of S protein using bioinformatics-based epitope prediction has identified key immunogenic proteins that can be expressed in the plants for the production of a plant-based vaccine against SARS CoV-2.65,66 Antibodies produced against the RBD of the S protein have been shown to neutralize SARS-CoV-2.61 The presence of NAbs after SARS-CoV-2 infection is critical for virus clearance and protection after vaccination. A recent study showed that majority of the infected patients developed high titers of SARS-CoV-2 S1 RBD-specific IgG antibodies; however, only a small fraction (3 out of 26 patients) had antibodies that were able to block SARS-CoV-2 binding to hACE2 receptor.67 The ability of an antigen to induce NAbs is a key factor to be considered while developing plant-based vaccines against SARS-CoV-2.67 SARS-CoV-2 vaccine development strategies exploiting the S protein should also be targeted to induce antibody-dependent cell-mediated cytotoxicity (ADCC) and cross-presentation for obtaining highly effective cell-mediated immune protection.68
Plants have been used for producing subunit vaccine candidates in the past, such as the ones produced for seasonal or pandemic strains of influenza virus rapidly via transient expression in tobacco in the past.69 For the development of the SARS vaccine, tomato plants have been explored.26 SARS-CoV nucleocapsid proteins have been expressed in tobacco plants and evaluated for immunogenicity for vaccine development.70 Currently, Kentucky BioProcessing company (Owensboro, KT, USA), a subsidiary of British American Tobacco (BAT) is attempting to develop a COVID-19 vaccine via SARS-CoV-2 protein subunit expression in tobacco.23,71 The S1 protein sequence (complete polypeptide) or the RBD may be the intended targets for designing the vaccine. SARS-CoV and SARS-CoV-2 S1 proteins are heavily glycosylated,72,73 with glycans having a mixture of complex and high-mannose configurations, which facilitate the expression of recombinant S1 and RBD with N-terminal signal peptides so that the proteins are secreted to the endomembrane.74 The structural differences of complex glycans in humans and plants might affect the efficiency of a plant-based COVID-19 vaccine. A COVID-19 vaccine is under development by British and American Tobacco Company (BAT) using new and fast-growing tobacco plant technology.75 Some fungi such as Saccharomyces cerevisiae have also been used for the development of oral vaccines against COVID-19 that exploit the S protein.76 Plants can be exploited for the production of virus-like particles (VLPs), multiepitopic vaccines, immune complexes, or elastin-like polypeptide fusions, potentially paving the way for COVID-19 vaccine development.77
The bioengineering of VLPs as viral antigens for vaccines renders several advantages, such as their proficient uptake by antigen-presenting cells (APCs), activation of the adaptive immune response, and induction of sturdy cellular and humoral immunity.78 Plant molecular farming of VLPs is safer as the native particles cannot replicate in humans, and bulk quantities can be obtained.79 Using tobacco plants, the VLP platform was exploited by Medicago Inc. (Québec, Canada) to produce 10 million doses of the H1N1 influenza vaccine in a month’s time.80 Medicago has initiated VLP-based plant vaccines for SARS-CoV-2.81 A VLP-based COVID-19 vaccine is also being developed in tobacco plants by iBio (Bryan, TX, USA).82 Similarly, scientists at the Queensland University of Technology evaluated the genome of tobacco plant (Nicotiana benthamiana) and are using the genome sequence of the plant for the development of a COVID-19 vaccine.83 University of California San Diego is also exploring plant-based COVID-19 vaccine development by combining molecular farming and advanced manufacturing strategies.84 The virus infects legumes; however, it does not infect humans, and is engineered to simulate SARS-CoV-2 to induce an appropriate immune response. It is believed to be stable without the need of refrigeration.84 A plant-based subunit (RBD-Fc + adjuvant) vaccine is being explored by Baiya Phytopharm/Chula Vaccine Research Center for SARS-CoV-2 and is in the preclinical stage.85 Antigen production in plants may help quickly fulfill the massive requirements of the COVID-19 vaccine around the world. In plants, the quantity of expression of the desired antigens depends on the specific target tissue such as leaves or seeds, and the promoter used for expressing the gene. Reports have shown that one acre of chloroplast transgenic tobacco plants can produce up to 360 million doses of anthrax vaccine antigens.86 Using the peanut plant as a model, it has been estimated that one plant can yield 15.6 g of protein in seeds and 750 mg of protein in leaf biomass. If we consider 5 µg antigen in one dose of a vaccine, it is possible to produce 468 million doses of vaccines from plants cultivated in one acre using a seed-based expression system.87 An overview on the production of plant-based vaccines to combat COVID-19 is presented in Figure 1
Figure 1.
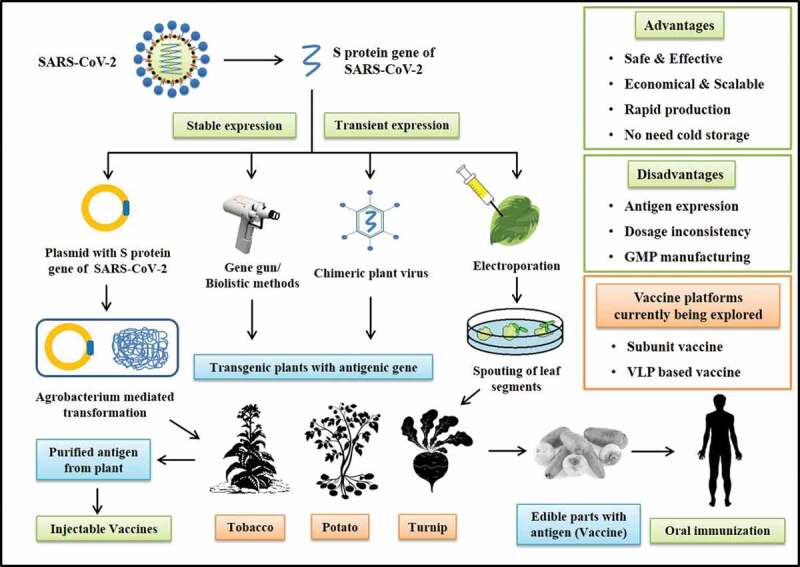
A pictorial representation on production of plant-based vaccines to combat COVID-19
Plant-based antibodies against SARS-CoV-2
Production of antibodies in plants is cheaper than that in animal cell lines. Plants can produce fully functional antibodies that can be used for therapeutic purposes in humans or animals.15 However, unconventional glycosylation is a potential immunological issue with plant-derived MAbs.88 Antibody production in plants can be scaled to an industrial level by using plant suspension cell culture in fermenters or by the cultivation of stably transformed transgenic plants. Antibodies can be produced either in the entire plant or in specific parts of the plants such as the seeds and tubers.89 The production of antibodies in edible parts of the plant would allow for a convenient method of passive immunization through the oral route to confer protection against various pathogens in the gastric mucosal surface.90 Antibodies such as the anti-rabies monoclonal antibody and the anti-colorectal cancer monoclonal antibody have been successfully produced in the plant system.91
Specific antibody-mediated passive immunization can confer immediate protection against infection from highly contagious pathogens such as SARS-CoV-2 and can be used prophylactically to prevent the disease in individuals at high-risk such as healthcare professionals and the people who have been in contact with a person who has tested positive for COVID-19. The serum from convalescent COVID-19 patients containing antibodies has been found to have therapeutic value in reducing the severity of the disease, alleviating symptoms, and aiding rapid recovery. However, nonspecific antibodies and other potential pathogens present in donor serum limit its safety; hence, the development of specific monoclonal antibodies in plants or other viable systems is needed.92 The shortage of serum antibodies from convalescent COVID-19 patients also leads to alternate development efforts, including plant-based vaccines.
Administration of recombinant antibodies produced against SARS-CoV-2 can help cure or slowdown the disease progression and provide adequate time to the body for producing its own antibodies against SARS-CoV-2.93,94 Plants can be used for producing antibodies for use in passive immunotherapy and for producing antigens for active immunization. ZMapp, a cocktail of three NAbs, was developed during the Ebola outbreak in West Africa by Mapp Biopharmaceutical (San Diego, CA, USA) has proven to be a life-saving measure against the Ebola outbreak.14,43,95 Cultivation of transgenic plants on a commercial scale constitutes an economical solution for manufacturing of a product like ZMapp that requires high doses, up to 10 mg of the antibody for every patient. Plant-based molecular pharming has to be explored for the bulk production of therapeutic antibodies such as tocilizumab for inhibiting the cytokine storm observed in SARS-CoV-2 infection. Sarilumab/Kevzara and tocilizumab/Actemra, which have been identified for their therapeutic properties in rheumatoid arthritis due to their binding ability to the interleukin-6 receptor (IL-6 R), are being repurposed to treat COVID-19 patients experiencing the life-threatening cytokine storm.96,97
Following oral administration of plant vaccines, the antigens expressed in edible plant parts have to induce a strong protective immune response. The antigen should not get degraded and has to pass through the mucosal lining in the gut. To ensure that the antigen uptake is sufficient to induce protective immunity, vaccine antigens can be formulated with immunomodulatory adjuvants. The adjuvants can help link antigenic molecules to the immune system components such as the M cells present in the intestinal lining for the efficient uptake of the antigen, which present to the T cells and B cells. Adjuvants such as V. cholerae toxin B subunit (CTB) and E. coli heat labile enterotoxin B subunit (LTB) can be used for passing the antigen to the M cells as they bind directly to the GM1-ganglioside receptor molecules on the M cells. Antigen fusion to these adjuvants ensure their delivery into the M cells to improve the immune response.87,98 Several other adjuvants such as oil-based emulsions, plant-derived saponin, and biodegradable liposomes are also used as adjuvants in vaccines.99
Conclusion and future perspectives
Use of plants as a transient expression system is a potential platform to produce vaccines, antivirals, and drugs for countering various important and emerging deadly pathogens such as SARS-CoV-2. Such pharmacological products can be produced in a short time span of a few weeks by utilizing transient expression in plants. Such products are more economical to produce than those manufactured through traditional and main production methodologies; however, preclinical and clinical stages required for testing the practical efficacy of vaccines and drugs need sufficient time before being commercialized. Such pharmaceuticals need to be produced in accordance with good manufacturing practice (GMP) that adds to the time required and the cost associated with the final development. Tobacco, legumes, or cereal plants have the ability to be grown in different environmental conditions; hence, products such as antibodies and antiviral drugs can be produced by employing regional or local infrastructures, exploiting the widely used distribution networks that are routinely used for food and cereal seeds, in the absence of any cold chain. Plant-based molecular pharming could aid in designing and developing novel vaccines and drugs against emerging pathogens including prospective measures to counter SARS-CoV-2. The Pharma-Planta project evaluated the regulatory guidelines of molecular farming for plant-made pharmaceuticals; such principles may be made practical to aid the development of vaccines and drugs against COVID-19.
Efforts are being made by the molecular farming community to develop plant-based vaccines and drugs against SARS-CoV-2. They would subsequently need promotional avenues and a pipeline for the translation of such biologicals into commercial markets with necessary cooperation and collaboration of pharmaceutical companies and industries after valid clinical trials and bulk production. This would facilitate the fight against the ongoing COVID-19 pandemic as well as pave the way to design a model preparedness plan for strategies to respond rapidly and in a targeted manner to handle future pandemics.
Transient expression systems for developing pharmacological products against COVID-19 require transgenic crops to be grown under containment. Reevaluation of genetically modified organism regulations is needed to ensure the smooth development of beneficial biological products to help efficiently tackle highly infectious pathogens and future pandemics.
Although third-generation vaccines have the potential to revolutionize the field of vaccinology, there is a need to overcome the challenges associated with third-generation vaccines before clinical application. Third-generation vaccines are noninfectious in nature, are capable of modulation, produce adequate immune response, and have reached Phase III of clinical trials, with a few candidates exhibiting successful clinical application; however, none have been made available for human consumption till date. The challenges that need to be addressed in the future are antigen selection and plant host expression, dosage consistency, and following GMP protocols for production. Overcoming these limitations may enable the availability of safe, effective, stable, and affordable plant-based vaccines in future including the COVID-19 vaccine.
Acknowledgments
All the authors acknowledge and thank their respective Institutes and Universities.
Funding Statement
This compilation is a review article written by its authors and required no substantial funding to be stated.
Author contributions
All the authors substantially contributed to the conception, compilation of data, checking, and approving the final version of the manuscript, and agree to be accountable for its contents.
Disclosure statement
All authors declare that there exist no commercial or financial relationships that could, in any way, lead to a potential conflict of interest.
References
- 1.Ahmad T, Haroon BM, Hui J.. Coronavirus disease 2019 (COVID-19) pandemic and economic impact. Pak J Med Sci. 2020;36:S73–S8. doi: 10.12669/pjms.36.COVID19-S4.2638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dhama K, Khan S, Tiwari R, Sircar S, Bhat S, Malik YS, et al. Coronavirus disease 2019-COVID-19. Clin Microbiol Rev. 2020;33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dhama K, Khan S, Tiwari R, Sircar S, Bhat S, Malik YS, Singh KP, Chaicumpa W, Bonilla-Aldana DK, Rodriguez-Morales AJ. Coronavirus disease pandemic (COVID-19): challenges and a global perspective. Pathogens. 2020;9(7):519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Iosifidis C, Agha M, Agha R.. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int J Surg. 2020;78:185–93. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.CDC . 1918. Pandemic (H1N1 virus). https://wwwcdcgov/flu/pandemic-resources/1918-pandemic-h1n1html (Accessed 14th July 2020) 2020.
- 6.Dhama K, Sharun K, Tiwari R, Dadar M, Malik YS, Singh KP, Chaicumpa W. COVID-19, an emerging coronavirus infection: advances and prospects in designing and developing vaccines, immunotherapeutics, and therapeutics. Hum Vaccin Immunother. 2020;16(6):1232–38. doi: 10.1080/21645515.2020.1735227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rodriguez-Morales AJ, Bonilla-Aldana DK, Tiwari R, Sah R, Rabaan AA, Dhama K. COVID-19, an emerging coronavirus infection: current scenario and recent developments-an overview. J Pure Appl Microbiol. 2020;14:6150. doi: 10.22207/JPAM.14.1.02. [DOI] [Google Scholar]
- 8.Weisberg EW, Sattler M, Yang PL, Parent A, Gray N, Griffin JD. Current therapies under investigation for COVID-19. Can J Physiol Pharmacol. 2020;98(8):483–89. [DOI] [PubMed] [Google Scholar]
- 9. Yatoo MI, Hamid Z, Parray OR, Wani AH, Ul Haq A, Saxena A, Patel SK, Pathak M, Tiwari R, Malik YS, et al. COVID-19 - Recent advancements in identifying novel vaccine candidates and current status of upcoming SARS-CoV-2 vaccines. Human Vac Immunotherap. 2020. (In press). doi: 10.1080/2164551520201788310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ciotti M, Ciccozzi M, Terrinoni A, Jiang WC, Wang CB, Bernardini S. The COVID-19 pandemic. Crit Rev Clin Lab Sci. 2020;64(5–6):215–23. [DOI] [PubMed] [Google Scholar]
- 11.Ma JK, Barros E, Bock R, Christou P, Dale PJ, Dix PJ. Molecular farming for new drugs and vaccines. Current perspectives on the production of pharmaceuticals in transgenic plants. EMBO Rep. 2005;6:593–99. doi: 10.1038/sj.embor.7400470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paul J, Yh Teh A M, M Twyman R, Kc Ma J. Target product selection-where can molecular pharming make the difference? Curr Pharm Des. 2013;19:5478–85. [DOI] [PubMed] [Google Scholar]
- 13.Weng JK. Plant solutions for the COVID-19 pandemic and beyond: historical reflections and future perspectives. Mol Plant. 2020;13:803–07. doi: 10.1016/j.molp.2020.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hiatt A, Cafferkey R, Bowdish K. Production of antibodies in transgenic plants. Nature. 1989;342(6245):76–78. doi: 10.1038/342076a0. [DOI] [PubMed] [Google Scholar]
- 15.Vermij P, Waltz E. USDA approves the first plant-based vaccine. Nat Biotechnol. 2006;24:234. [Google Scholar]
- 16.Laere E, Ling APK, Wong YP, Koh RY, Mohd Lila MA, Hussein S. Plant-based vaccines: production and challenges. J Bot. 2016;2016:1–11. doi: 10.1155/2016/4928637. [DOI] [Google Scholar]
- 17.Naderi S, Fakheri B. Overview of plant-based vaccines. Res J Fish Hydrobiol. 2015;10:275–89. [Google Scholar]
- 18.Streatfield SJ, Jilka JM, Hood EE, Turner DD, Bailey MR, Mayor JM, Woodard SL, Beifuss KK, Horn ME, Delaney DE, et al. Plant-based vaccines: unique advantages. Vaccine. 2001;19(17–19):2742–48. doi: 10.1016/S0264-410X(00)00512-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liew PS, Hair-Bejo M. Farming of plant-based veterinary vaccines and their applications for disease prevention in animals. Adv Virol. 2015;2015:936940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Phan HT, Conrad U. Plant-based vaccine antigen production. Methods Mol Biol. 2016;1349:35–47. [DOI] [PubMed] [Google Scholar]
- 21.Dhama K, Wani MY , Deb R, Karthik K, Tiwari R, Barathidasan R, Kumar A, Mahima, Verma AK, Singh SD. Plant based oral vaccines for human and animal pathogens-a new era of prophylaxis: current and future perspectives. J Exp Biol Agric Sci. 2013;1:1–12. [Google Scholar]
- 22.Schillberg S, Raven N, Spiegel H, Rasche S, Buntru M. Critical analysis of the commercial potential of plants for the production of recombinant proteins. Front Plant Sci. 2019;10:720. doi: 10.3389/fpls.2019.00720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Capell T, Twyman RM, Armario-Najera V, Ma JK, Schillberg S, Christou P. Potential applications of plant biotechnology against SARS-CoV-2. Trends Plant Sci. 2020;25(7):635–43. doi: 10.1016/j.tplants.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fischer R, Buyel JF. Molecular farming - The slope of enlightenment. Biotechnol Adv. 2020;40:107519. doi: 10.1016/j.biotechadv.2020.107519. [DOI] [PubMed] [Google Scholar]
- 25.Shanmugaraj B, Malla A, Phoolcharoen W. Emergence of Novel Coronavirus 2019-nCoV: need for rapid vaccine and biologics development. Pathogens. 2020;9(2):148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kurup VM, Thomas J. Edible vaccines: promises and challenges. Mol Biotechnol. 2020;62(2):79–90. doi: 10.1007/s12033-019-00222-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wu L, Jiang L, Zhou Z, Fan J, Zhang Q, Zhu H, Han Q, Xu Z. Expression of foot-and-mouth disease virus epitopes in tobacco by a tobacco mosaic virus-based vector. Vaccine. 2003;21(27–30):4390–98. doi: 10.1016/S0264-410X(03)00428-6. [DOI] [PubMed] [Google Scholar]
- 28.William S. A review of the progression of transgenic plants used to produce plant bodies for human usage. J Young Invest. 2002;4:56–61. [Google Scholar]
- 29.Ma C, Su S, Wang J, Wei L, Du L, Jiang S. From SARS-CoV to SARS-CoV-2: safety and broad-spectrum are important for coronavirus vaccine development. Microbes Infect. 2020;22(6–7):245–53. doi: 10.1016/j.micinf.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stoger E, Fischer R, Moloney M, Ma JK. Plant molecular pharming for the treatment of chronic and infectious diseases. Annu Rev Plant Biol. 2014;65:743–68. [DOI] [PubMed] [Google Scholar]
- 31.Whaley KJ, Hiatt A, Zeitlin L. Emerging antibody products and Nicotiana manufacturing. Hum Vaccin. 2011;7(3):349–56. doi: 10.4161/hv.7.3.14266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aboul-Ata AA, Vitti A, Nuzzaci M, El-Attar AK, Piazzolla G, Tortorella C, Harandi AM, Olson O, Wright SA, Piazzolla P. Plant-based vaccines: novel and low-cost possible route for Mediterranean innovative vaccination strategies. Adv Virus Res. 2014;89:1–37. [DOI] [PubMed] [Google Scholar]
- 33.Prasad A, Muthamilarasan M, Prasad M. Synergistic antiviral effects against SARS-CoV-2 by plant-based molecules. Plant Cell Rep. 2020;39(9):1109–14. doi: 10.1007/s00299-020-02560-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.De Zoeten GA, Penswick JR, Horisberger MA, Ahl P, Schultze M, Hohn T. The expression, localization, and effect of a human interferon in plants. Virology. 1989;172(1):213–22. doi: 10.1016/0042-6822(89)90123-2. [DOI] [PubMed] [Google Scholar]
- 35.Sijmons PC, Dekker BM, Schrammeijer B, Verwoerd TC, van den Elzen PJ, Hoekema A. Production of correctly processed human serum albumin in transgenic plants. Biotechnology (N Y). 1990;8:217–21. [DOI] [PubMed] [Google Scholar]
- 36.Pujol M, Ramirez NI, Ayala M, Gavilondo JV, Valdes R, Rodriguez M, Brito J, Padilla S, Gómez L, Reyes B, et al. An integral approach towards a practical application for a plant-made monoclonal antibody in vaccine purification. Vaccine. 2005;23(15):1833–37. doi: 10.1016/j.vaccine.2004.11.023. [DOI] [PubMed] [Google Scholar]
- 37.Chichester JA, Jones RM, Green BJ, Stow M, Miao F, Moonsammy G, Streatfield SJ, Yusibov V. Safety and immunogenicity of a plant-produced recombinant hemagglutinin-based influenza vaccine (HAI-05) derived from A/Indonesia/05/2005 (H5N1) influenza virus: a phase 1 randomized, double-blind, placebo-controlled, dose-escalation study in healthy adults. Viruses. 2012;4:3227–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cummings JF, Guerrero ML, Moon JE, Waterman P, Nielsen RK, Jefferson S, Gross FL, Hancock K, Katz JM, Yusibov V, et al. Safety and immunogenicity of a plant-produced recombinant monomer hemagglutinin-based influenza vaccine derived from influenza A (H1N1)pdm09 virus: a Phase 1 dose-escalation study in healthy adults. Vaccine. 2014;32(19):2251–59. doi: 10.1016/j.vaccine.2013.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Landry N, Pillet S, Favre D, Poulin JF, Trepanier S, Yassine-Diab B, Ward BJ. Influenza virus-like particle vaccines made in Nicotiana benthamiana elicit durable, poly-functional and cross-reactive T cell responses to influenza HA antigens. Clin Immunol. 2014;154(2):164–77. doi: 10.1016/j.clim.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 40.Scotti N, Buonaguro L, Tornesello ML, Cardi T, Buonaguro FM. Plant-based anti-HIV-1 strategies: vaccine molecules and antiviral approaches. Expert Rev Vaccines. 2010;9(8):925–36. doi: 10.1586/erv.10.79. [DOI] [PubMed] [Google Scholar]
- 41.Webster DE, Thomas MC, Pickering R, Whyte A, Dry IB, Gorry PR. Is there a role for plant‐made vaccines in the prevention of HIV/AIDS? Immunol Cell Biol. 2005;83(3):239–47. doi: 10.1111/j.1440-1711.2005.01341.x. [DOI] [PubMed] [Google Scholar]
- 42.Yang M, Sun H, Lai H, Hurtado J, Chen Q. Plant-produced Zika virus envelope protein elicits neutralizing immune responses that correlate with protective immunity against Zika virus in mice. Plant Biotechnol J. 2018;16:572–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Qiu X, Wong G, Audet J, Bello A, Fernando L, Alimonti JB, Fausther-Bovendo H, Wei H, Aviles J, Hiatt E, et al. Reversion of advanced Ebola virus disease in nonhuman primates with ZMapp. Nature. 2014;514(7520):47–53. doi: 10.1038/nature13777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nykiforuk CL, Boothe JG, Murray EW, Keon RG, Goren HJ, Markley NA, Moloney MM. Transgenic expression and recovery of biologically active recombinant human insulin from Arabidopsis thaliana seeds. Plant Biotechnol J. 2006;4:77–85. doi: 10.1111/j.1467-7652.2005.00159.x. [DOI] [PubMed] [Google Scholar]
- 45.Erlendsson LS, Muench MO, Hellman U, Hrafnkelsdóttir SM, Jonsson A, Balmer Y, Mäntylä E, Örvar BL. Barley as a green factory for the production of functional Flt3 ligand. Biotechnol J. 2010;5(2):163–71. doi: 10.1002/biot.200900111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Loh H-S, Green BJ, Yusibov V. Using transgenic plants and modified plant viruses for the development of treatments for human diseases. Curr Opin Virol. 2017;26:81–89. doi: 10.1016/j.coviro.2017.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Faye L, Gomord V. Success stories in molecular farming-a brief overview. Plant Biotechnol J. 2010;8(5):525–28. doi: 10.1111/j.1467-7652.2010.00521.x. [DOI] [PubMed] [Google Scholar]
- 48.McCarthy M. US signs contract with ZMapp maker to accelerate development of the Ebola drug. BMJ. 2014;349(sep04 10):g5488. doi: 10.1136/bmj.g5488. [DOI] [PubMed] [Google Scholar]
- 49.Concha C, Cañas R, Macuer J, Torres MJ, Herrada AA, Jamett F, Ibáñez C. Disease prevention: an opportunity to expand edible plant-based vaccines? Vaccines (Basel). 2017;5(2):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Oszvald M, Kang TJ, Tomoskozi S, Tamas C, Tamas L, Kim TG, Yang M-S. Expression of a synthetic neutralizing epitope of porcine epidemic diarrhea virus fused with synthetic B subunit of Escherichia coli heat labile enterotoxin in rice endosperm. Mol Biotechnol. 2007;35(3):215–23. doi: 10.1007/BF02686007. [DOI] [PubMed] [Google Scholar]
- 51.Zhang X, Buehner NA, Hutson AM, Estes MK, Mason HS. Tomato is a highly effective vehicle for expression and oral immunization with Norwalk virus capsid protein. Plant Biotechnol J. 2006;4(4):419–32. doi: 10.1111/j.1467-7652.2006.00191.x. [DOI] [PubMed] [Google Scholar]
- 52.Qian B, Shen H, Liang W, Guo X, Zhang C, Wang Y, Li G, Wu A, Cao K, Zhang D. Immunogenicity of recombinant hepatitis B virus surface antigen fused with preS1 epitopes expressed in rice seeds. Transgenic Res. 2008;17(4):621–31. doi: 10.1007/s11248-007-9135-6. [DOI] [PubMed] [Google Scholar]
- 53.Kim TG, Kim MY, Kim BG, Kang TJ, Kim YS, Jang YS, Arntzen CJ, Yang MS. Synthesis and assembly of Escherichia coli heat-labile enterotoxin B subunit in transgenic lettuce (Lactuca sativa). Protein Expr Purif. 2007;51:22–27. [DOI] [PubMed] [Google Scholar]
- 54.Hahn B-S, Jeon I-S, Jung Y-J, Kim J-B, Park J-S, Ha S-H, Kim K-H, Kim H-M, Yang J-S, Kim Y-H, et al. Expression of hemagglutinin-neuraminidase protein of Newcastle disease virus in transgenic tobacco. Plant Biotechnol Rep. 2007;1(2):85–92. doi: 10.1007/s11816-007-0012-9. [DOI] [Google Scholar]
- 55.Dhama K, Patel SK, Pathak M, Yatoo MI, Tiwari R, Malik YS, Singh R, Sah R, Rabaan AA, Bonilla-Aldana DK, et al. An update on SARS-CoV-2/COVID-19 with particular reference to its clinical pathology, pathogenesis, immunopathology and mitigation strategies. Travel Med Infect Dis. 2020;37:101755. doi: 10.1016/j.tmaid.2020.101755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Prete M, Favoino E, Catacchio G, Racanelli V, Perosa F. SARS-CoV-2 inflammatory syndrome. clinical features and rationale for immunological treatment. Int J Mol Sci. 2020;21(9): 3377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ye Q, Wang B, Mao J. The pathogenesis and treatment of the cytokine Storm’in COVID-19. J Infect. 2020;80(6):607–13. doi: 10.1016/j.jinf.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tay MZ, Poh CM, Renia L, MacAry PA, Ng LFP. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. 2020;20:363–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Keam S, Megawati D, Patel S, Tiwari R, Dhama K, Harapan H. Immunopathology and immunotherapeutic strategies in SARS-CoV-2 infection. Rev Medical Virol. 2020;30(5). Accepted manuscript. doi: 10.1002/rmv.2123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Yatoo MI, Hamid Z, Parray OR, Wani AH, Ul Haq A, Saxena A, Patel SK, Pathak M, Tiwari R, Malik YS, et al. COVID-19 - Recent advancements in identifying novel vaccine candidates and current status of upcoming SARS-CoV-2 vaccines. Hum Vaccines Immunotherapeutics. 2020. In press. doi: 10.1080/21645515.2020.1788310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jiang S, He Y, Liu S. SARS vaccine development. Emerg Infect Dis. 2005;11(7):1016–20. doi: 10.3201/1107.050219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shang W, Yang Y, Rao Y, Rao X. The outbreak of SARS-CoV-2 pneumonia calls for viral vaccines. NPJ Vaccines. 2020;5(1):18. doi: 10.1038/s41541-020-0170-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gralinski LE, Menachery VD. Return of the Coronavirus: 2019-nCoV. Viruses. 2020;12(2):135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wan Y, Shang J, Graham R, Baric RS, Li F. Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS Coronavirus. J Virol. 2020;94(7):e00127–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Grifoni A, Sidney J, Zhang Y, Scheuermann RH, Peters B, Sette A. A sequence homology and bioinformatic approach can predict candidate targets for immune responses to SARS-CoV-2. Cell Host Microbe. 2020;27(4):671–80e2. doi: 10.1016/j.chom.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zheng M, Song L. Novel antibody epitopes dominate the antigenicity of spike glycoprotein in SARS-CoV-2 compared to SARS-CoV. Cell Mol Immunol. 2020;17(5):536–38. doi: 10.1038/s41423-020-0385-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chen X, Li R, Pan Z, Qian C, Yang Y, You R, Zhao J, Liu P, Gao L, Li Z, et al. Human monoclonal antibodies block the binding of SARS-CoV-2 spike protein to angiotensin converting enzyme 2 receptor. Cell Mol Immunol. 2020;17(6):647–49. doi: 10.1038/s41423-020-0426-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Du L, He Y, Zhou Y, Liu S, Zheng BJ, Jiang S. The spike protein of SARS-CoV–a target for vaccine and therapeutic development. Nat Rev Microbiol. 2009;7(3):226–36. doi: 10.1038/nrmicro2090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Pandey A, Singh N, Sambhara S, Mittal SK. Egg-independent vaccine strategies for highly pathogenic H5N1 influenza viruses. Hum Vaccin. 2010;6(2):178–88. doi: 10.4161/hv.6.2.9899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zheng N, Xia R, Yang C, Yin B, Li Y, Duan C, Liang L, Guo H, Xie Q. Boosted expression of the SARS-CoV nucleocapsid protein in tobacco and its immunogenicity in mice. Vaccine. 2009;27(36):5001–07. doi: 10.1016/j.vaccine.2009.05.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.British American Tobacco . BAT working on potential COVID-19 vaccine through US bio-tech subsidiary. https://wwwbatcom/group/sites/UK__9D9KCYnsf/vwPagesWebLive/DOBN8QNL (Accessed 1 July 2020) 2020.
- 72.Vankadari N, Wilce JA. Emerging WuHan (COVID-19) coronavirus: glycan shield and structure prediction of spike glycoprotein and its interaction with human CD26. Emerg Microbes Infect. 2020;9(1):601–04. doi: 10.1080/22221751.2020.1739565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Walls AC, Park YJ, Tortorici MA, Wall A, McGuire AT, Structure VD. Function, and antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell. 2020;181(2):281–92e6. doi: 10.1016/j.cell.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Krokhin O, Li Y, Andonov A, Feldmann H, Flick R, Jones S, Stroeher U, Bastien N, Dasuri KVN, Cheng K. Mass spectrometric characterization of proteins from the SARS virus: a preliminary report. Mol Cell Proteomics. 2003;2(5):346–56. doi: 10.1074/mcp.M300048-MCP200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Anon. British and American Tobacco Company . Potential COVID-19 vaccine – BAT in the news. 2020. [accessed 2020 Oct 4]. https://www.bat.com/group/sites/UK__9D9KCY.nsf/vwPagesWebLive/DOBNHBWR
- 76.Zhai P, Ding Y, Wu X, Long J, Zhong Y, Li Y. The epidemiology, diagnosis and treatment of COVID-19. Int J Antimicrob Agents. 2020;55(5):105955. doi: 10.1016/j.ijantimicag.2020.105955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rosales-Mendoza S, Marquez-Escobar VA, Gonzalez-Ortega O, Nieto-Gomez R, Arevalo-Villalobos JI. What does plant-based vaccine technology offer to the fight against COVID-19? Vaccines (Basel). 2020;8(2):183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lua LHL, Connors NK, Sainsbury F, Chuan YP, Wibowo N, Middelberg APJ. Bioengineering virus‐like particles as vaccines. Biotechnol Bioeng. 2014;111(3):425–40. doi: 10.1002/bit.25159. [DOI] [PubMed] [Google Scholar]
- 79.Rybicki EP. Plant molecular farming of virus‐like nanoparticles as vaccines and reagents. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2020;12:e1587. [DOI] [PubMed] [Google Scholar]
- 80.D’Aoust MA, Couture MM, Charland N, Trepanier S, Landry N, Ors F, Vézina L-P. The production of hemagglutinin-based virus-like particles in plants: a rapid, efficient and safe response to pandemic influenza. Plant Biotechnol J. 2010;8(5):607–19. doi: 10.1111/j.1467-7652.2009.00496.x. [DOI] [PubMed] [Google Scholar]
- 81.Phillip Morris International . Medicago develops a plant-based vaccine for Coronavirus. 2020. (Accessed 1 July 2020). https://wwwpmicom/media-center/news/medicago-develops-a-plant-based-vaccine-for-coronavirus
- 82.iBio . iBio announces development of proprietary COVID-19 vaccine candidates. 2020. https://wwwglobenewswirecom/news-release/2020/03/18/2002546/0/en/iBio-Announces-Development-of-Proprietary-COVID-19-Vaccine-Candidateshtml (Accessed 1 July 2020)
- 83.ISAAA . Native australian plant paves way for vaccine development against COVID-19. 2020. http://wwwisaaaorg/kc/cropbiotechupdate/article/defaultasp?ID=18054 (Accessed 1 July 2020)
- 84.ISAAA . Nanoengineers combine molecular farming and advanced manufacturing to develop COVID-19 vaccine. 2020. http://wwwisaaaorg/kc/cropbiotechupdate/article/defaultasp?ID=18090 (Aceessed: 1 July 2020)
- 85.WHO . DRAFT landscape of COVID-19 candidate vaccines – 18 June 2020. 2020. https://wwwwhoint/docs/default-source/coronaviruse/novel-coronavirus-landscape-covid-19f65d59aff81049f5a50d37bebf0caf93pdf?sfvrsn=394d10c9_2%26download (Accessed 7 July 2020)
- 86.Koya V, Moayeri M, Leppla SH, Daniell H. Plant-based vaccine: mice immunized with chloroplast-derived anthrax protective antigen survive anthrax lethal toxin challenge. Infect Immun. 2005;73(12):8266–74. doi: 10.1128/IAI.73.12.8266-8274.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tiwari S, Verma P, Singh P, Tuli R. Plants as bioreactors for the production of vaccine antigens. Biotechnol Adv. 2009;27(4):449–67. doi: 10.1016/j.biotechadv.2009.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ko K, Tekoah Y, Rudd PM, Harvey DJ, Dwek RA, Spitsin S, Hanlon CA, Rupprecht C, Dietzschold B, Golovkin M. Function and glycosylation of plant-derived antiviral monoclonal antibody. Proc Natl Acad Sci U S A. 2003;100(13):8013–18. doi: 10.1073/pnas.0832472100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Fischer R, Hoffmann K, Schillberg S, Emans N. Antibody production by molecular farming in plants. J Biol Regul Homeost Agents. 2000;14:83–92. [PubMed] [Google Scholar]
- 90.Virdi V, Depicker A. Role of plant expression systems in antibody production for passive immunization. Int J Dev Biol. 2013;57(6–7–8):587–93. doi: 10.1387/ijdb.130266ad. [DOI] [PubMed] [Google Scholar]
- 91.Ko K, Brodzik R, Steplewski Z. Production of antibodies in plants: approaches and perspectives. Curr Top Microbiol Immunol. 2009;332:55–78. [DOI] [PubMed] [Google Scholar]
- 92.Shanmugaraj B, Siriwattananon K, Wangkanont K, Phoolcharoen W. Perspectives on monoclonal antibody therapy as potential therapeutic intervention for Coronavirus disease-19 (COVID-19). Asian Pac J Allergy Immunol. 2020;38:10–18. [DOI] [PubMed] [Google Scholar]
- 93.Duan K, Liu B, Li C, Zhang H, Yu T, Qu J, Zhou M, Chen L, Meng S, Hu Y, et al. Effectiveness of convalescent plasma therapy in severe COVID-19 patients. Proc Natl Acad Sci U S A. 2020;117(17):9490–96. doi: 10.1073/pnas.2004168117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Shen C, Wang Z, Zhao F, Yang Y, Li J, Yuan J, Wang F, Li D, Yang M, Xing L, et al. Treatment of 5 critically ill patients with COVID-19 with convalescent plasma. JAMA. 2020;323(16):1582. doi: 10.1001/jama.2020.4783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Na W, Park N, Yeom M, Song D. Ebola outbreak in Western Africa 2014: what is going on with Ebola virus? Clin Exp Vaccine Res. 2015;4(1):17–22. doi: 10.7774/cevr.2015.4.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kuchler H, Mancini D. WHO and Roche launch trials of potential coronavirus treatments. 2020. https://wwwswissinfoch/eng/covid-19_who-and-roche-launch-trials-of-potential-coronavirus-treatments/45630498 (Accessed: 1 July 2020)
- 97.Solnik C Northwell health initiates clinical trials of 2 COVID-19 drugs. 2020. https://wwwlongislandpresscom/2020/03/21/northwell-health-initiates-clinical-trials-of-2-covid-19-drugs/ (Accessed: 1 July 2020)
- 98.Cuatrecasas P. Gangliosides and membrane receptors for cholera toxin. Biochemistry. 1973;12(18):3558–66. doi: 10.1021/bi00742a032. [DOI] [PubMed] [Google Scholar]
- 99.Reed SG, Bertholet S, Coler RN, Friede M. New horizons in adjuvants for vaccine development. Trends Immunol. 2009;30(1):23–32. doi: 10.1016/j.it.2008.09.006. [DOI] [PubMed] [Google Scholar]


