Abstract
Coronavirus disease 2019 (COVID‐19) patients with cardiac injury have an increased risk of mortality. It remains to be determined the mechanism of cardiac injury and the identification of specific conditions that affect the heart during COVID‐19. We present the case of a 76‐year‐old woman with COVID‐19 pneumonia that developed a takotsubo syndrome (TTS). Although the patient presented normal left ventricular ejection fraction and normal levels of troponin on admission, after 16 days in intensive care unit due to respiratory distress, she suddenly developed cardiogenic shock. Shock occurred few hours after a spontaneous breathing trial through her tracheostomy. Bed‐side echocardiographic revealed apical ballooning promptly supporting the diagnosis of TTS. She was successfully treated with deep sedation and low dosage of epinephrine. The relevance of this case is that TTS can occur in the late phase of COVID‐19. Awareness of late TTS and bed‐side echocardiographic evaluation can lead to prompt identification and treatment.
Keywords: Takotsubo syndrome, Cardiac injury, Coronavirus disease 2019, Severe acute respiratory syndrome coronavirus 2
Introduction
Cardiac injury, defined as increased levels of troponin, has been reported between 7% and 27% among patients affected by coronavirus disease 2019 (COVID‐19). 1 , 2 , 3 Those who develop cardiac injury have an increased risk of mortality, 1 , 3 but mechanisms of cardiac injury in COVID‐19 are still under investigation. 4 Myocarditis has been proposed as a possible explanation. 5 Alongside, some cases of takotsubo syndrome (TTS) have been reported during COVID‐19 pandemic. 6 , 7 , 8 Physio‐pathological pathways are yet to be elucidated. Here, we present a case of TTS as a complication of COVID‐19 pneumonia in a 76‐year‐old woman with severe respiratory failure.
Case report
A 76‐year‐old Caucasian woman presented at Emergency Department complaining shortness of breath after 9 days of fever and cough in March 2020. At admission, the temperature was 38.2°C, blood pressure 135/65 mmHg, heart rate 81 beats per minute, respiratory rate (RR) 22 breaths per minute, and oxygen saturation 90% while the patient was receiving supplemental oxygen through a nasal cannula at a rate of 8 L/min. Nucleic acid testing of a nasopharyngeal swab for severe acute respiratory coronavirus (SARS‐CoV)‐2 virus was positive.
Chest radiography showed diffuse opacities mainly in the right lung, and computed tomography scan revealed diffuse bilateral ground glass opacities confirming interstitial pneumonia (Figure 1 A and 1 B ). After a short trial of continuous positive airway pressure with helmet for ongoing acute respiratory distress syndrome [pH 7.44, arterial partial pressure of carbon dioxide (PaCO2) of 30 mmHg and of oxygen (PaO2) of 65 mmHg with fraction of inspired oxygen (FiO2) of 0.7], the patient was intubated and underwent invasive mechanical ventilation. An antiviral therapy was started with lopinavir/ritonavir (500/125 mg BID) and hydroxychloroquine (200 mg BID) and discontinued after 10 days. Electrocardiogram (ECG) on intensive care unit admission revealed sinus rhythm without abnormalities (Figure 1 C ). On Day 1, echocardiogram revealed preserved biventricular function, without wall motion or valvular abnormalities. On Day 7, because acute respiratory distress syndrome was unresolved and prolonged mechanical ventilation was expected, a surgical tracheostomy was performed. After a gradual improvement of her respiratory parameters (RR of 16, PaO2/FiO2 of 325 with FiO2 0.3 in pressure support ventilation), on Day 16, a spontaneous breathing trial was attempted through her tracheostomy but shortly interrupted after 3 h for respiratory distress. A few hours later, the patient developed cardiogenic shock with confusion, skin hypoperfusion, oliguria, and hypotension (blood pressure 80/40 mmHg, heart rate 110 b.p.m.). ECG revealed a slight ST‐segment elevation with loss of R‐waves in leads V2 to V4 (Figure 1 D ). Laboratory tests showed an increase in high sensitivity troponin‐T level with creatine kinase‐MB within upper reference limit and a sharp increase in N‐terminal pro‐B‐type natriuretic peptide (Supporting Information, Table S1 ). A prompt echocardiographic exam revealed normal size of ventricular chambers, severe left ventricular (LV) systolic dysfunction with an LV ejection fraction (EF) of 25%, and akinesia of middle and apical segments (apex ballooning) with hyperkinetic motion of basal segments (Supporting Information, Video S1 ). Clinical, laboratory, and imaging findings supported the diagnosis of TTS rather than acute coronary syndrome, and we preferred to avoid a coronary angiography. The patient was then treated with deep sedation (continuous infusion of propofol 3 mg/kg/h and remifentanil 0.1 µg/kg/min), low‐dose epinephrine (0.04 µg/kg/min), and controlled mechanical ventilation (tidal volume 6 mL/kg of predicted body weight, RR of 20, and positive end‐expiratory pressure of 10 cmH2O). The following days, the patient was haemodynamically stable, and epinephrine was withdrawn. On Day 23, echocardiogram revealed a partial recovery of LVEF up to 38% with improvement of the wall motion of apical segments (Supporting Information, Video S2 ); low beta‐blocker therapy was started. On Day 28, the patient was finally decannulated in autonomous breathing on room air and then discharged from intensive care unit with levels of troponin and N‐terminal pro‐B‐type natriuretic peptide significantly decreased and precordial R‐wave reappearance and biphasic T‐waves in V2–V4 leads on ECG (Figure 1 E ). On Day 62, an echocardiogram before hospital discharge showed a complete recovery of LVEF up to normal values.
FIGURE 1.
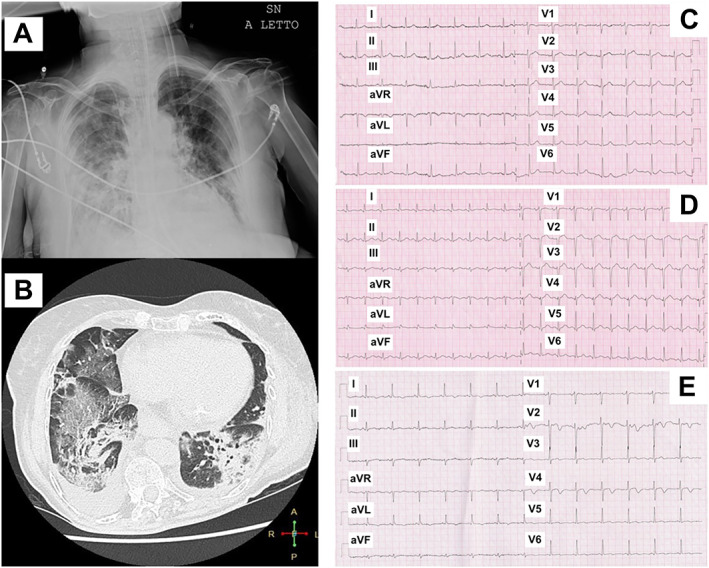
(A) Chest X‐ray and (B) computed tomography of interstitial pneumonia. (C–E) Serial electrocardiograms before, during, and after takotsubo syndrome.
Discussion
Although respiratory distress prevail as clinical presentation of COVID‐19, cardiac injury is commonly reported especially in severe or critically ill patients. 1 , 3 Based on a study that examined 54 COVID‐19 patients who died compared with 137 that were discharged, a significant increase in troponin was found between Days 13 and 16 from illness onset. 9 Cardiovascular manifestations of COVID‐19 range from acute coronary syndromes to myocarditis, arrhythmias, pulmonary embolism, and stroke. Up to our knowledge, only three cases of TTS were reported as a potential cardiac complication in critically ill COVID‐19 patients. 6 , 7 , 8 Physio‐pathological mechanism leading to TTS in COVID‐19 remains unclear; nevertheless, microvascular dysfunction, coronary artery vasospasm cytokine storm triggered by viral infection, and myocarditis have been proposed as potential pathways. Previously, other authors yet described cases of TTS related to respiratory infection. 10 Another intriguing hypothesis suggested that direct endothelial cell infection by SARS‐CoV‐2 might promote a sort of endotheliitis, thus predisposing to microcirculatory endothelial dysfunction and stress cardiomyopathy. 11 , 12 Finally, a reverse TTS has been described during a histologically proven acute myocarditis in a COVID‐19 woman admitted with chest pain. 13
Takotsubo syndrome is usually expected in post‐menopausal women exposed to an emotional stress leading to catecholaminergic discharge. Interestingly, in this case, the triggers for TTS could be both physical and emotional distress. In fact, during spontaneous breathing trial, the patient might attempt either fatigue (due to the acute increase in the respiratory workload) or anxiety for the breathless sensation.
The differential diagnosis in our case included ACS and acute myocarditis. Coronary angiography is a key invasive diagnostic test to rule‐out ACS in patients presenting with suspected TTS. Nevertheless, the risk of invasive test needs to be weight especially in old and fragile patients at increased risk of acute kidney injury. In our case, anamnestic, echocardiographic finding of an acute onset of an apical balloon and ECG findings without significant increase of myocardial markers were classic for TTS. For these reasons, we preferred to differ coronary angiography in such a fragile patient to mitigate periprocedural risks. Furthermore, the risk score that help differentiation of TTS from ACS (InterTAK score) revealed a pre‐test probability of TTS of 92.9% [InterTAK score of 74 based on the presence of female sex (25 points), emotional stress (24 points), physical stress (13 points), and no ST‐segment depression (12 points)]. 14 This strategy was further supported by clinical/echocardiographic improvement of the patient and absence of Q waves on ECG at follow‐up. Endomyocardial biopsy can exclude or confirm an ongoing myocarditis; nevertheless, in this specific setting, the potential risks overweighed the diagnostic benefit; thus, it was deemed unnecessary. The rapid improvement and the high likelihood of a TTS deemed the endomyocardial biopsy as unnecessary. Finally, even if cardiac magnetic resonance imaging can support the diagnosis of acute myocarditis or ischaemic heart disease, the haemodynamic instability of the patient did not allow to perform this exam.
In conclusion, awareness of TTS as potential complication in COVID‐19 patients, even in a delayed phase of disease, and prompt bed‐side echocardiographic evaluation can lead to rapid identification and treatment.
Conflict of interest
None declared.
Funding
None.
Supporting information
Video S1. Supporting information
Video S2. Supporting information
Table S1. Supporting information
Acknowledgements
We acknowledge all doctors and nurses who took care of our patients: they did not contribute directly to this manuscript, but with their effort, they were essential in saving patients affected by COVID‐19.
Bottiroli, M. , De Caria, D. , Belli, O. , Calini, A. , Andreoni, P. , Siragusa, A. , Moreo, A. , Ammirati, E. , Mondino, M. , and Fumagalli, R. (2020) Takotsubo syndrome as a complication in a critically ill COVID‐19 patient. ESC Heart Failure, 7: 4297–4300. 10.1002/ehf2.12912.
References
- 1. Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, Wang H, Wan J, Wang X, Lu Z. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID‐19). JAMA Cardiol. Published online March 2020; 27: 811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan. China JAMA 2020; 323: 1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, Gong W, Liu X, Liang J, Zhao Q, Huang H, Yang B, Huang C. Association of cardiac injury with mortality in hospitalized patients with COVID‐19 in Wuhan. China JAMA Cardiol Published online March 2020; 25: 802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Boukhris M, Hillani A, Moroni F, Annabi MS, Addad F, Ribeiro MH, Mansour S, Zhao X, Ybarra LF, Abbate A, Vilca LM, Azzalini L. Cardiovascular implications of the COVID‐19 pandemic: a global perspective. Can J Cardiol. 2020; 36: 1068–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, Tomasoni D, Cani DS, Cerini M, Farina D, Gavazzi E, Maroldi R, Adamo M, Ammirati E, Sinagra G, Lombardi CM, Metra M. Cardiac involvement in a patient with coronavirus disease 2019 (COVID‐19). JAMA Cardiol Published online March 2020; 27: 819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Solano‐López J, Sánchez‐Recalde A, Zamorano JL. SARS‐CoV‐2, a novel virus with an unusual cardiac feature: inverted takotsubo syndrome. Eur Heart J. 2020; ehaa390 10.1093/eurheartj/ehaa390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Minhas AS, Scheel P, Garibaldi B, Liu G, Horton M, Jennings M, Jones SR, Michos ED, Hays AG. Takotsubo syndrome in the setting of COVID‐19. JACC Case Rep. 2020; 2: 1321–1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Meyer P, Degrauwe S, Van Delden C, Ghadri J‐R, Templin C. Typical takotsubo syndrome triggered by SARS‐CoV‐2 infection. Eur Heart J 2020; 41: 1860–1860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L. Clinical course and risk factors for mortality of adult inpatients with COVID‐19 in Wuhan, China: a retrospective cohort study. The Lancet 2020; 395: 1054–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lozano Á, Bastante T, Salamanca J, Aguilar R, Montes de Oca R, Rodríguez D, Alfonso F. Tako‐tsubo cardiomyopathy triggered by Influenza A virus infection. Int J Cardiol 2014; 174: e52–e53. [DOI] [PubMed] [Google Scholar]
- 11. Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, Mehra MR, Schuepbach RA, Ruschitzka F, Moch H. Endothelial cell infection and endotheliitis in COVID‐19. The Lancet. 2020; 395: 1417–1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Peretto G, Sala S, Caforio ALP. Acute myocardial injury, MINOCA, or myocarditis? Improving characterization of coronavirus‐associated myocardial involvement. Eur Heart J. Published online May 3 2020: ehaa396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sala S, Peretto G, Gramegna M, Palmisano A, Villatore A, Vignale D, de Cobelli F, Tresoldi M, Cappelletti AM, Basso C, Godino C, Esposito A. Acute myocarditis presenting as a reverse Tako‐Tsubo syndrome in a patient with SARS‐CoV‐2 respiratory infection. Eur Heart J 2020; 41: 1861–1862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ghadri JR, Cammann VL, Jurisic S, Seifert B, Napp LC, Diekmann J, Bataiosu DR, D'Ascenzo F, Ding KJ, Sarcon A, Kazemian E, Birri T, Ruschitzka F, Lüscher TF, Templin C, InterTAK co‐investigators . A novel clinical score (InterTAK Diagnostic Score) to differentiate takotsubo syndrome from acute coronary syndrome: results from the International Takotsubo Registry: diagnostic score for takotsubo syndrome. Eur J Heart Fail 2017; 19: 1036–1042. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video S1. Supporting information
Video S2. Supporting information
Table S1. Supporting information


