Abstract
Background
In late December 2019, a cluster of pneumonia cases due to a novel betacoronavirus, SARS-CoV-2 was reported in China. The so-called COVID 19 is responsible not only for respiratory symptoms, from mild up to pneumonia and even acute respiratory distress syndrome, but also for extrapulmonary involvement.
Cases presentation
Here we present two cases of spontaneous muscle hematoma in patients with SARS-CoV-2 infection, both on therapeutic LMWH for atrial fibrillation: the first one was an 86-year-old Caucasian female with a history of hypertensive cardiomyopathy and the second one was an 81-year-old Caucasian male with a history of hypertension, diabetes and ischemic heart disease. Blood tests revealed a considerable drop of hemoglobin and alterations of coagulation system. In both cases, embolization of femoral artery was performed. A few other cases of bleeding manifestations are reported in literature, while a lot has been published about the hypercoagulability related to COVID-19.
Conclusions
Our reports and literature review highlight the need of active surveillance for possible hemorrhagic complications in patients with SARS-CoV-2 infection.
Keywords: COVID-19, Endothelial dysfunction, Vascular disease, Muscle haematoma, Case report
Background
In late December 2019, a cluster of pneumonia cases of unknown etiology was reported in the city of Wuhan in Hubei Province, China. A novel betacoronavirus, SARS-CoV-2, spread by inter-human transmission, is considered as the etiological agent of this disease [1, 2]. The World Health Organization (WHO) officially named the coronavirus disease “COVID-19” and declared a global pandemic in 2020. The spectrum of clinical manifestations of SARS-Cov-2 infection ranges from fever, fatigue, myalgia, cough and dyspnoea to pneumonia and even acute respiratory distress syndrome. Extrapulmonary involvement, such as gastrointestinal (diarrhea, nausea/vomiting, abdominal pain), cardiovascular (arrhythmias, myocardial injury) and renal (acute renal injury) have been reported as well. There is emerging evidence of the role of vascular disease in COVID-19 and clinical reports increasingly suggest a confluence of endothelial dysfunction, thrombosis and dysregulated inflammation [3]. Here we present two cases of older patients with SARS-Cov-2 infection, who presented spontaneous muscle hematoma on anticoagulation therapy with heparin in therapeutic dose.
Cases presentation
Case 1
The first patient was an 86-year-old woman with a history of hypertensive cardiomyopathy with severe mitral regurgitation and atrial fibrillation on anticoagulant therapy with warfarin. She presented to the Emergency Department after experiencing a sudden onset of shortness of breath on mild exertion and peripheral edema.
At admission, the patient was afebrile, eupneic in oxygen therapy at rest. Thoracic physical examination revealed decreased breath sounds and crackles in the lower lung lobes, bilaterally.
Blood investigations revealed a total leucocyte count of 9140/mcL (normal 4000–11,000/mcL), Hb 11 g/dL (normal 13–18 g/dL), C-reactive protein (CRP) 15.8 mg/dL (normal < 0.50 mg/dL), Procalcitonin (PCT) 0.32 ng/L (normal < 0.5 ng/L), fibrinogen 707 mg/dL (normal 200–400 mg/dL), creatinine 1.23 mg/dL (normal 0.7–1.20 mg/dL), INR 2.36 (normal 0.82–1.19). Chest CT revealed bilateral pleural effusion with passive atelectasis of the lower lobes. Patient was diagnosed with COVID-19 on April the 8th, 2020, on the basis of RT-PCR testing that detected SARS-CoV-2. The patient was admitted to our Geriatric department and began to receive hydroxychloroquine, intravenous ceftriaxone and doxycycline, as per local protocol, observing a good clinical response and the decrease of inflammation markers. Weaning and discontinuation of oxygen therapy was possible once the patient was stable with satisfactory oxygen saturation. The anticoagulation (AC) therapy was maintained, however, we decided to switch AC therapy from warfarin to low molecular-weight heparin (LMWH) enoxaparin 6000 U BID.
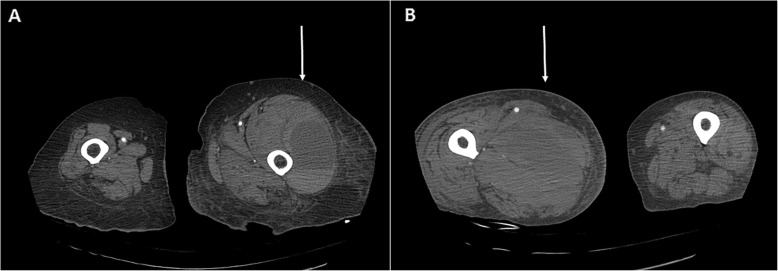
Suddenly, 5 days after admission, she started complaining of pain and loss of movement of her left leg, which appeared swollen. Venous compression ultrasound (CUS) and evaluation of D-dimer excluded deep vein thrombosis, but a Chest computed tomography (CT) scan with contrast revealed an 11 × 8 × 14 cm hematoma in the left thigh (Fig. 1). Laboratory tests showed a fall in hemoglobin from 11 g/dL to 7.8 g/dL and, despite the absence of active arterial extravasation, prophylactic embolization of small branches of superficial and deep femoral artery was performed. Blood tests at that time also showed alterations of coagulation system, with reduced prothrombin time, increased fibrinogen and international normalized ratio (INR), despite a platelet count within normal limits. Interleukin-6 levels were 67,9 pg/mL (normal < 12.7 pg/mL). Overall, the patient was transfused 3 unit of packed blood cells, which raised her hemoglobin to 10.1 g/dL. Table 1 shows the patient’s routine blood test during the hospitalization. In the following days, the patient’s hemoglobin remained stable and the hematoma showed no evidence of further expansion. The patient recovered completely and was discharged shortly after the event.
Fig. 1.
Computed Tomography images of the two patients’ hematomas. This image shows the 11 x 8 x 14 cm hematoma in the Case 1’s left thigh (a) and the 12 x 10 x 25 cm Case 2’s hematoma in the right thigh (b) (white arrows)
Table 1.
Blood investigations of both patients
| Case 1 | Case 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| Blood tests | DAY 1 | DAY 4 | DAY 19 | DAY 23 | DAY 1 | DAY 2 | DAY 10 | DAY 14 |
| RBC IU/mcL | 4.310.000 | 4.710.000 | 2.970.000 | 3.710.000 | 3.7400.00 | 3.090.000 | 3.460.000 | 2.740.000 |
| Hb g/dL | 11,0 | 11,9 | 7,80 | 9.9 | 12,5 | 10,3 | 11,10 | 8,50 |
| HCT % | 33 | 38 | 24,30 | 30.7 | 36,6 | 29,9 | 34,10 | 25,2 |
| MCV fL | 77 | 80 | 81,80 | 82,7 | 97,9 | 96,4 | 98,60 | 92 |
| WBC IU/mcL | 9140 | 8800 | 13.360 | 8300 | 15.640 | 9390 | 12.600 | 17.120 |
| N % | 83 | 74 | 82 | 77,9 | 88,5 | 90,3 | 91,00 | 90,7 |
| L % | 9 | 17 | 10 | 12,5 | 5,7 | 3,6 | 2,90 | 4,2 |
| M % | 8 | 9 | 7,4 | 9 | 5,6 | 6,1 | 6 | 5 |
| E % | 0 | 0 | 0,3 | 0,5 | 0,1 | 0 | 0,10 | 0,1 |
| B % | 0 | 0 | 0 | 0 | 0,1 | 0 | 0,00 | 0 |
| PLT IU/mcL | 155.000 | 167.000 | 301.000 | 233.000 | 327.000 | 256,000 | 290.000 | 211.000 |
| PT % | 17 | 66 | 75,00 | 36 | 49 | 59 | ||
| INR | 4,00 | 1,34 | 1,19 | 2,1 | 1,67 | 1,43 | ||
| aPTT sec. | 40,3 | 30,4 | 32,4 | 28,5 | 23,4 | 36,70 | ||
| aPTT Ratio | 1,40 | 1,06 | 1,13 | 0,99 | 0,82 | 1,27 | ||
| Fibrinogen mg/dL | 707 | 805 | 421 | 350 | ||||
| D-dimer mg/L | 0,3 | 0,47 | 1,95 | |||||
| CRP mg/dL | 15,88 | 13,04 | 11,37 | 16,69 | 11,41 | 1,64 | ||
| PCT ng/mL | 0,32 | 0,32 | 0,9 | 0,9 | ||||
| BNP pg/mL | 571 | 945 | 907 | 2523 | 1367 | 229 | ||
| IL-1 pg/mL | 3,5 | |||||||
| IL-6 pg/mL | 67,9 | 6,1 | ||||||
| IL-10 pg/mL | 0,5 | |||||||
| TNF-α pg/mL | 1,8 | |||||||
| MCP-1 pg/mL | 356 | 228 | ||||||
| Creatinine mg/dL | 1,23 | 1,07 | 1,53 | 0,81 | 1,92 | 1,56 | 1,82 | 1,58 |
Abbreviations: RBC red blood cells, Hb haemoglobin, HCT hematocrit, MCV mean corpuscular volume, WBC white blood cells, N neutrophils, L lymphocytes, M monocytes, E eosinophils, B basophils, PLT platelets, INR international normalized ratio, PT prothrombin time, aPTT activated partial thromboplastin time, CRP C-reactive protein, PCT procalcitonin, BNP brain natriuretic peptide, IL-1 interleukin 1, IL-6 interleukin 6, IL-10 interleukin 10, TNF-α tumor necrosis factor α, MCP-1 monocyte chemoattractant protein-1
Case 2
Another patient with similar findings was seen at our Geriatric department. The patient was an 81-year-old man with a history of hypertension, diabetes, ischemic heart disease and dilated cardiomyopathy with reduced left ventricular ejection fraction on echocardiogram, who presented to the Emergency Department with cough and shortness of breath. At admission the patient was oriented, febrile and had a respiratory rate of 15 breaths per minute and oxygen saturation of 97% while he was receiving oxygen therapy (10 L/min). He was tachycardic and ECG detected atrial fibrillation.
Laboratory tests showed a total leucocyte count of 15,640/mcL (N 88.5%, L 5.7%), Hb 12.5 g/dL, C-reactive protein (CRP) 16.69 mg/dL, PCT 0.95 ng/mL, fibrinogen 350 mg/dL, creatinine 1.92 mg/dL, Brain Natriuretic Peptide (BNP) 2523 pg/mL (normal < 100 pg/mL), INR 2.1. CT scan revealed bilateral ground-glass opacities and crazy-paving pattern with thickened interlobular septae and intralobular lines, with bilateral consolidations and thoracic lymphadenopathy. Serological tests detected the presence of serum IgM antibodies against SARS-Cov-2. Once admitted to our Geriatric ward, blood tests were repeated; INR dropped to 1.56 and creatinine values dropped to 1.67 mg/dL (CKD-EPI 41 mL/min/1.73 m2), therefore, accounting for the patient’s body weight of 83 Kg, anticoagulation therapy with LMWH (enoxaparin 8000 U BID) was administered. Blood cultures were collected (gram-positive cocci positivity detected), antimicrobial broad-spectrum therapy was started, observing a good clinical response and the decrease of inflammation markers.
On the ninth day of admission, similarly to the first case we reported, the patient presented right thigh hematoma causing pain and loss of movement. X-ray showed no sign of hip fracture. Laboratory investigations at the time revealed a drop in hemoglobin from 12,5 g/dL to 6,6 g/dL and showed alterations of coagulation system, with decreased prothrombin time, increased partial thromboplastin time and INR, despite a platelet count within normal limits. A CT scan with contrast detected a 12 × 10 × 25 cm hematoma in the right thigh with four foci of active arterial extravasation (i.e. active bleeding) (Fig. 1). Transcatheter angiography directly identified arterial injury and the source of the bleeding, so that coil and gelfoam embolization of branches of deep femoral artery was performed (Fig. 2). The patient was transfused 2 unit of packed blood cells. Table 1 shows the patient’s routine blood test during the hospitalization. Although the procedure was successful and there was no evidence of further arterial extravasation, the patient died in the following days.
Fig. 2.
Selective catheterism and coil embolization of hematoma’s arterial afferences.
The image shows the catheterized and embolized arterial afferences of Case 2’s hematoma
The patients described in the current manuscript have not been reported in any other submission. Written informed consent for publication was obtained from the first patient and from the next of keen of the second one.
Discussion
There are several cases in the recent literature of different patterns of vascular disease in patients with SARS-CoV-2 infection, most of which point towards the hypercoagulability related to COVID-19.
Melissano et al. reported a high number of cases hospitalized for pneumonia SARS-CoV-2 induced, associated with ischemia of lower and upper limbs and a significant number of deep venous thrombosis among both ventilated and unventilated patients. Most of the patients were already receiving antithrombotic prophylaxis [3]. In a retrospective study performed in two French intensive care units, Llitjos et al. found a high rate of venous thromboembolism in anticoagulated patients with COVID-19-related ARDS, supported with mechanical ventilation[4]. The possible link between thromboembolic events and the respiratory failure in COVID-19 has been widely reported. Gattinoni et al. observed a discrepancy between the well-preserved lung compliance and the severity of hypoxemia in patients with COVID-19 pneumonia. A possible explanation for such severe hypoxemia occurring in compliant lungs, in contrast to expectations for severe ARDS, could be a loss of lung perfusion regulation and hypoxic vasoconstriction [5]. This atypical presentation of ARDS seems to be associated to complement-mediated microvascular injury and thrombosis, as shown in recent autoptic studies [6]. Compared to the growing attention given to hypercoagulability associated to COVID-19, a little has been reported about the hemorrhagic problems in patients with SARS-CoV-2 infection. Even though muscle hematomas have always been recognized as a possible complication of LMWH treatment of older adults [7–9], attention should be driven to possible hemorrhagic complications COVID19-related during LMWH treatment [10].
In a group of 41 Thai patients (4 males and 37 females, age between 7 and 74 years) affected by COVID-19, Joob et al.. reported only one patient presenting with bleeding manifestation (petechiae) and he was firstly misdiagnosed as dengue fever [11]. Guotao et al.. described the case of an 83-year-old man with SARS-CoV-2 infection presenting hematochezia, with no source of bleeding identified by colonoscopy or abdominal CT scan. The authors considered the possibility that manifestations including hematochezia may be secondary to an alternate point of entry of SARS-CoV-2 virus [12]. Zulfiqar et al.. described the case of a 65-year-old woman with COVID-19 presenting with immune thrombocytopenic purpura complicated by subarachnoid microhemorrhage [13]. Sharifi-Razavi et al.. reported the case of a 79-year-old man affected by COVID-19, with a history of fever and cough and acute loss of consciousness; brain CT revealed a massive intracerebral hemorrhage. He was not hypertensive nor on anticoagulant therapy. The authors suggested that brain ACE2 could be involved in SARS-CoV-2 infection and its dysfunction could lead to disruption of vascular autoregulation [14]. Conti et al.. reported two cases of spontaneous ileo-psoas hematomas in hospitalized patients for SARS-CoV-2-related bilateral interstitial pneumonia and supported with C-PAP ventilation. They were a 76-year-old man and a 72-year-old woman, both treated with LMWH but at different dosages: the first one with prophylactic LMWH, the second one with therapeutic dosage because of concomitant deep venous femoral thrombosis. Blood investigations revealed normal PLT, PT and PTT; they both received radiological embolization of the epigastric inferior artery. The cause of the bleeding remained unclear; the authors suggested a possible connection with the presence of cough and the use of C-PAP ventilation other than the emerging disorders of the coagulation system [15]. Recently, Mattioli et al. published a case report of neck and upper chest spontaneous hematoma in an 84-year-old patient prescribed with prophylactic dose of LMWH [16].
Finally, our Interventional Radiology team reported other four cases of spontaneous bleeding in patients with COVID-19, all treated with therapeutic dosage of LMWH: a 74-year-old woman with rupture of superior thoracic artery complicated by left pectoral muscle hematoma, a 71-year-old man with left iliopsoas muscle hematoma, a 71-year-old woman with a rectus sheath hematoma due to both right and left inferior epigastric arteries injury and a 81-year-old man with a large left thigh hematoma. They all underwent coil embolization. The authors suggested a traumatic mechanism underlying the bleeding in two cases (mobilization in the prone position in the first one, electrical cardioversion in the second one) [17].
No evidence of trauma was found in the two cases we described. Although hemorrhagic complications in soft tissues, muscles, retroperitoneum [18, 19], are quite common even in absence of SARS-CoV-2 infection in patients treated with LMWH or anticoagulants, in our reports the temporal sequence suggests that COVID-19 was a contributing factor in the development of spontaneous muscle hematoma.
Conclusions
In conclusion, emerging data confirm the broad range of COVID-19 complications, above the respiratory ones. Among them, vascular involvement in COVID-19 appears to be related not only to hypercoagulability features, but also to bleeding ones. We recommend caution and active surveillance for possible hemorrhagic complications in patients with SARS-CoV-2 infection, in particular in those treated with LMWH or at higher hemorrhagic risk.
Acknowledgements
Not applicable.
Abbreviations
- COVID
Corona virus disease
- CRP
C-reactive protein
- PCT
Procalcitonin
- CT
Computed tomography
- RT-PCR
Real-time polymerase chain reaction
- LMWH
Low molecular-weight heparin
- CUS
Venous compression ultrasound
- INR
International normalized ratio
- BNP
Brain natriuretic peptide
- ARDS
Acute respiratory distress syndrome
- ACE2
Angiotensin-converting enzyme-2
- RAS
Reninangiotensin system
- RBC
Red blood cells
- Hb
Haemoglobin
- HCT
Hematocrit
- MCV
Mean corpuscular volume
- WBC
White blood cells
- N
Neutrophils
- L
Lymphocytes
- M
Monocytes
- E
Eosinophils
- B
Basophils
- PLT
Platelets
- PT
Prothrombin time
- aPTT
Activated partial thromboplastin time
- IL-1
Interleukin 1
- IL-6
Interleukin 6
- IL-10
Interleukin 10
- TNF-α
Tumor necrosis factorα
- MCP-1
Monocyte chemoattractant protein-1
Authors’ contributions
SR provided the patients with medical care, collected the data, reviewed the literature and prepared the draft of the manuscript. VC supervised the literature search and revision, and proof read the manuscript, approving the final version. RF provided the patients with medical care, collected the data, reviewed the literature and prepared the draft of the manuscript. AMC provided the patients with medical care, collected the data, reviewed the literature and prepared the draft of the manuscript. CO supervised the literature search and revision, and proof read the manuscript, approving the final version. FM conceptualized the manuscript, supervised the literature search and read/approved the final version. All authors have read and approved the manuscript.
Funding
The authors did not receive fundings to prepare the manuscript.
Availability of data and materials
The presented data are available under request, as anonymized files. To have access to the data, please contact Prof F. Monzani, Director of the Geriatrics Unit (Department of Clinical and Experimental Medicine, University of Pisa), Email: fabio.monzani@med.unipi.it, Phone: +393337733135.
Ethics approval and consent to participate
Not applicable.
Consent for publication
We obtained written informed consent to publish the case report from patients or legal representative. In case of deceased patient, the consent for publication was obtained by the next of keen.
The patients described in the current manuscript have not been reported in any other submission. Nonetheless, these patients are included in a multicentre national register endorsed by the Italian Society of Gerontology and Geriatrics thus, in the future, they could be reported as part of that database but only with epidemiological purposes without any relation to their own clinical outcome, specifically the haemorrhagic complication.
Competing interests
The authors do not have competing interest to declare.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sara Rogani and Valeria Calsolaro contributed equally as first author.
References
- 1.Chan JF, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–23. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li Q, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199–207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Melissano G, et al. Pattern of vascular disease in Lombardy, Italy, during the first month of the COVID-19 outbreak. J Vasc Surg. 2020;72(1):4–5. doi: 10.1016/j.jvs.2020.04.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Llitjos JF, et al. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients. J Thromb Haemost. 2020;18(7):1743–6. doi: 10.1111/jth.14869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gattinoni L, et al. COVID-19 does not lead to a “typical” acute respiratory distress syndrome. Am J Respir Crit Care Med. 2020;201(10):1299–300. doi: 10.1164/rccm.202003-0817LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Magro C, et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res. 2020;220:1–13. doi: 10.1016/j.trsl.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Di Ascenzo L, et al. Major rectus abdominis hematoma complicating low molecular weight heparin therapy. J Cardiovasc Med (Hagerstown) 2008;9(7):758–9. doi: 10.2459/JCM.0b013e3282f45787. [DOI] [PubMed] [Google Scholar]
- 8.Manckoundia P, et al. [Muscle hematoma in the very elderly receiving low-molecular-weight heparins] Presse Med. 2000;29(13):702. [PubMed] [Google Scholar]
- 9.Nourbakhsh E, Anvari R, Nugent K. Abdominal wall hematomas associated with low-molecular-weight heparins: an important complication in older adults. J Am Geriatr Soc. 2011;59(8):1543–5. doi: 10.1111/j.1532-5415.2011.03529.x. [DOI] [PubMed] [Google Scholar]
- 10.Dorgalaleh A. Bleeding and bleeding risk in COVID-19. Semin Thromb Hemost. 2020;46(7):815–8. doi: 10.1055/s-0040-1713434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joob B, Wiwanitkit V. Hemorrhagic problem among the patients with COVID-19: clinical summary of 41 Thai infected patients. Clin Appl Thromb Hemost. 2020;26:1076029620918308. doi: 10.1177/1076029620918308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guotao L, et al. SARS-CoV-2 infection presenting with hematochezia. Med Mal Infect. 2020;50(3):293–6. doi: 10.1016/j.medmal.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zulfiqar AA, et al. Immune thrombocytopenic purpura in a patient with Covid-19. N Engl J Med. 2020;382(18):e43. doi: 10.1056/NEJMc2010472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sharifi-Razavi A, Karimi N, Rouhani N. COVID-19 and intracerebral haemorrhage: causative or coincidental? New Microbes New Infect. 2020;35:100669. doi: 10.1016/j.nmni.2020.100669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Conti CB, et al. Bleeding in COVID-19 severe pneumonia: the other side of abnormal coagulation pattern? Eur J Intern Med. 2020;77:147–9. doi: 10.1016/j.ejim.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mattioli M, et al. Atypical spontaneous hematomas in a patient with severe coronavirus disease 2019 (COVID-19) Semin Thromb Hemost. 2020;46(7):856–8. doi: 10.1055/s-0040-1715092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bargellini I, et al. Spontaneous bleedings in COVID-19 patients: an emerging complication. Cardiovasc Intervent Radiol. 2020;43(7):1095–6. doi: 10.1007/s00270-020-02507-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sahu KK, et al. Clinical spectrum, risk factors, management and outcome of patients with retroperitoneal hematoma: a retrospective analysis of 3-year experience. Expert Rev Hematol. 2020;13(5):545–55. doi: 10.1080/17474086.2020.1733963. [DOI] [PubMed] [Google Scholar]
- 19.Sahu KK, Mishra AK, Zhang P. Femoral neuropathy: a rare presentation of retroperitoneal hematoma with review of literature. Indian J Hematol Blood Transfus. 2020;36(1):174–7. doi: 10.1007/s12288-019-01126-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The presented data are available under request, as anonymized files. To have access to the data, please contact Prof F. Monzani, Director of the Geriatrics Unit (Department of Clinical and Experimental Medicine, University of Pisa), Email: fabio.monzani@med.unipi.it, Phone: +393337733135.