Many colleges and universities in the United States are attempting to continue undergraduate onsite learning and residential living during the COVID-19 pandemic. Modeling the outcomes, cost, and cost-effectiveness of mitigation strategies, such as social distancing, masking, and laboratory testing, can inform these efforts.
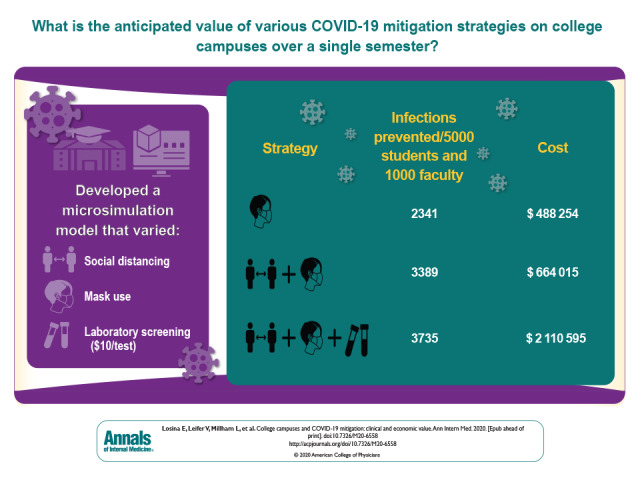
Visual Abstract. COVID-19 Mitigation on College Campuses.
Many colleges and universities in the United States are attempting to continue undergraduate onsite learning and residential living during the COVID-19 pandemic. Modeling the outcomes, cost, and cost-effectiveness of mitigation strategies, such as social distancing, masking, and laboratory testing, can inform these efforts.
Abstract
Background:
Colleges in the United States are determining how to operate safely amid the coronavirus disease 2019 (COVID-19) pandemic.
Objective:
To examine the clinical outcomes, cost, and cost-effectiveness of COVID-19 mitigation strategies on college campuses.
Design:
The Clinical and Economic Analysis of COVID-19 interventions (CEACOV) model, a dynamic microsimulation model, was used to examine alternative mitigation strategies. The CEACOV model tracks infections accrued by students and faculty, accounting for community transmissions.
Data Sources:
Data from published literature were used to obtain parameters related to COVID-19 and contact-hours.
Target Population:
Undergraduate students and faculty at U.S. colleges.
Time Horizon:
One semester (105 days).
Perspective:
Modified societal.
Intervention:
COVID-19 mitigation strategies, including social distancing, masks, and routine laboratory screening.
Outcome Measures:
Infections among students and faculty per 5000 students and per 1000 faculty, isolation days, tests, costs, cost per infection prevented, and cost per quality-adjusted life-year (QALY).
Results of Base-Case Analysis:
Among students, mitigation strategies reduced COVID-19 cases from 3746 with no mitigation to 493 with extensive social distancing and masks, and further to 151 when laboratory testing was added among asymptomatic persons every 3 days. Among faculty, these values were 164, 28, and 25 cases, respectively. Costs ranged from about $0.4 million for minimal social distancing to about $0.9 million to $2.1 million for strategies involving laboratory testing ($10 per test), depending on testing frequency. Extensive social distancing with masks cost $170 per infection prevented ($49 200 per QALY) compared with masks alone. Adding routine laboratory testing increased cost per infection prevented to between $2010 and $17 210 (cost per QALY gained, $811 400 to $2 804 600).
Results of Sensitivity Analysis:
Results were most sensitive to test costs.
Limitation:
Data are from multiple sources.
Conclusion:
Extensive social distancing with a mandatory mask-wearing policy can prevent most COVID-19 cases on college campuses and is very cost-effective. Routine laboratory testing would prevent 96% of infections and require low-cost tests to be economically attractive.
Primary Funding Source:
National Institutes of Health.
Colleges and universities in the United States are trying to mitigate the effect of coronavirus disease 2019 (COVID-19) on their campuses. More than 2000 colleges, with more than 20 million students and 3.6 million employees, constitute this $671-billion-per-year industry (1, 2). Since the pandemic began, there have been more than 320 000 COVID-19 cases and 80 deaths at more than 1700 colleges, highlighting the consequences of various mitigation strategies (3). Because students live in close contact, which increases the likelihood of transmission, and more than one third of college faculty (about 500 000 persons) are older than 55 years, which increases the risk for morbidity and mortality from COVID-19 (4, 5), evaluating mitigation strategies is critical. These strategies have major implications for laboratory testing and hospital capacity in the towns and cities where colleges are located.
The tradeoffs of different strategies must be weighed. Although closing campus and offering fully remote education might reduce transmissions, doing so could reduce education quality, graduation rates, and revenue (6). Frequent laboratory testing may be costly and requires isolation strategies for those who test positive. Schools have considered combinations of nonpharmacologic interventions (NPIs) and screening of asymptomatic students with laboratory testing to balance these factors.
Such NPIs include hybrid (in-person and online) education, social distancing, designated isolation locations for symptomatic students or asymptomatic students who test positive, and required mask wearing (7, 8). Testing strategies vary in frequency and test sensitivity.
Data about the efficacy of social distancing and masks, the accuracy and cost of testing, and the feasibility of isolation strategies have evolved over the fall; therefore, we examined the clinical and economic effect of alternative strategies for COVID-19 mitigation in college settings (9, 10).
Methods
Analytic Overview
We used the calibrated and validated Clinical and Economic Analysis of COVID-19 interventions (CEACOV) model, a dynamic microsimulation of the natural history of COVID-19 built on susceptible–infected–recovered principles (11) (Supplement). We considered contacts among students, faculty, and the surrounding community and assessed clinical outcomes among students and faculty, including prevalent and incident infections, isolation unit use, laboratory tests, and hospital and intensive care unit (ICU) use. CEACOV models infections to students and faculty occurring from students, faculty, and the community. We focused on undergraduate students because most live on campus or near it in surrounding communities and because they exhibit a unique social profile and activities. In addition, many colleges focus on undergraduate education and do not offer graduate programs. We modeled college and university staff as members of the community, assuming that they exhibit social behaviors more similar to those of surrounding community members (work, dining, shopping, and errands) than to those of undergraduate students (class and on-campus social activities) or faculty (teaching and office hours).
Transmission rates within and across groups are based on estimated contact-hours for each and the infectivity rate for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) per contact-hour (12). Costs included NPIs, testing, and hospital-related expenses. Using quality of life (QoL) decrements for similar illnesses, we modeled QoL decrements for COVID-19 (13–15). We accounted for the daily proportion of individuals with influenza-like illness unrelated to SARS-CoV-2 infections (16). Outcomes included the projected clinical effect, cost, budget impact, and cost-effectiveness of mitigation strategies over 1 semester (105 days). We calculated incremental cost-effectiveness ratios (ICERs), the difference in costs divided by the difference in quality-adjusted life-years (QALYs) between strategies, and determined the cost per infection prevented (17). We describe results for 5000 students and 1000 faculty within a surrounding community of 100 000 persons.
Strategies
We considered 2 “background” strategies for comparison where the campus remains closed with only online education (CampusClosed) and where the campus operates as it did before COVID-19 without any mitigation interventions (NoIntervention).
We examined 24 mitigation strategies based on the following 4 approaches: social distancing (SocDist), mask-wearing policies (Masks), isolation, and laboratory testing (LT). Laboratory testing ranged from no testing of asymptomatic students or faculty to routine LT (RLT) of asymptomatic students and faculty at 14-, 7-, or 3-day intervals. Because administrative actions implemented by colleges aim to reduce or eliminate larger gatherings, we modeled 2 social distancing programs: minimal social distancing (MinSocDist), including canceling sports and university-sponsored concerts, and extensive social distancing (ExtSocDist), where 100% of large classes and 50% of smaller classes were delivered online.
We also considered a strategy that combined the ExtSocDist and Masks strategies (ExtSocDist+Masks). Social distancing reduced contact-hours with infected persons, and masks reduced infectivity of infected individuals. All 24 strategies used symptom screening. Positive results from symptom screening and laboratory tests led to isolation, which further reduced contact between infected and susceptible persons.
We examined 2 isolation strategies for students with positive results on symptom screening or laboratory tests: residence-based isolation (ResIsol) and designated spaces for isolation (DesigIsol). Both strategies reduced contact-hours between infected and susceptible persons; DesigIsol reduced contact-hours more than ResIsol.
CEACOV Model Structure
Disease States and Progression
The CEACOV model is a dynamic microsimulation of SARS-CoV-2 (18–20). Susceptible persons have a daily probability of becoming infected. Infected persons have a daily probability of advancing in COVID-19 severity, which increases with age and includes risk for hospitalization, ICU admission, and death. The model includes 6 COVID-19 disease states: preinfectious latency, asymptomatic, mild or moderate, severe, critical, and recuperation, all as defined by current clinical and epidemiologic data. The latency period for COVID-19 lasts 5 days on average, and neither symptom screening nor laboratory testing is positive during this stage (21, 22). Asymptomatic disease can be detected only with laboratory screening. Masks can reduce the infectiousness of asymptomatic and symptomatic individuals. In this analysis, we assumed that all persons recovered from COVID-19 are immune to reinfection for the remainder of the semester.
Transmissions
The CEACOV model captures the heterogeneity of viral transmission among students, faculty, and the community. The overall force of infection depicting transmission risk from infected to susceptible individuals is distributed across the 3 transmission groups, weighted by group size and contact-hours within and across the groups. The transmission rate is based on contact-hours per day and a derived infectivity rate per contact-hour. Social distancing reduces contact-hours within and between groups. Masks reduce the infectivity rate (9).
Costs and QoL
We included the costs of NPIs, isolation units, testing, and hospitalization. Costs of NPIs include implementation and maintenance of online learning platforms, masks, and cleaning and disinfecting measures. Strategy-specific costs depend on the NPIs in place. College-sponsored DesigIsol costs include the cost per day of designated isolation units. Although mild to moderate COVID-19 symptoms are assumed to resolve with over-the-counter or no medications, severe or critical disease results in hospitalization and potentially ICU costs. We report costs in 2020 U.S. dollars.
For mild and moderate COVID-19, we estimated QoL losses based on utility decrements from influenza (14). For all students, regardless of symptom state, we modeled decreased QoL for time spent in isolation to account for the effects of isolation on mental health (15). We derived QoL decrements for hospitalized individuals using data for complicated pneumonia (13). The effect of mortality on QALYs lost is described in the Supplement. We did not model any long-term complications from COVID-19.
Input Parameters
Cohort Characteristics
We derived demographic characteristics of students, faculty, and community members using data from colleges and their surrounding typical college towns (Supplement).
Contact-Hours
We derived contact-hours, defined as a single hour spent with a single person, within and across transmission groups (Table 1)<(23–37)>. We estimated average contact-hours before the COVID-19 pandemic as the basis for reductions in contact-hours resulting from social distancing strategies.
Table 1. Input Parameters for an Analysis of COVID-19 Mitigation Strategies on U.S. College Campuses.
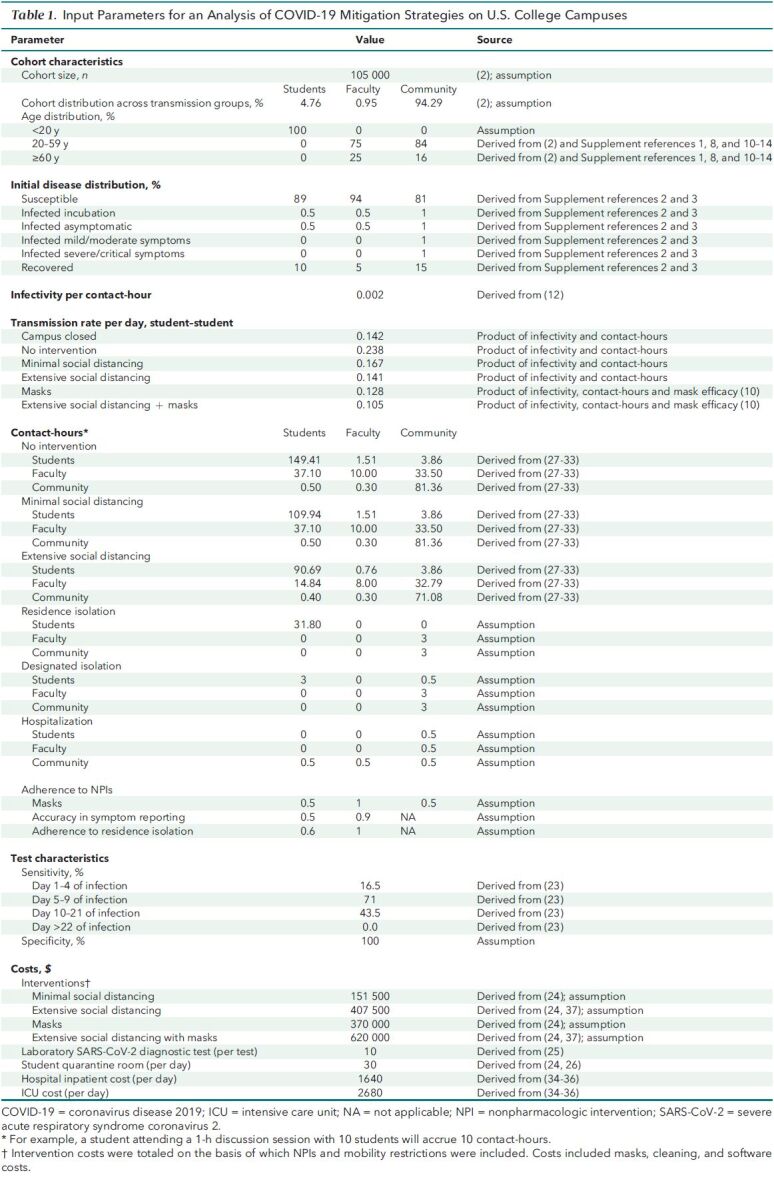
Contact-hours for students include time spent with roommates; in group study; in office hours with faculty; in lectures; and in recreational, sports, work-for-pay, shopping, and social activities. We estimated that each student on average spends 149 contact-hours per day with other students, 1.5 contact-hours per day with faculty, and 3.9 contact-hours per day with community members.
We estimated that each faculty member on average spends 10 contact-hours per day with other faculty, 37 contact-hours per day with students (25 of which are spent teaching), and 33 contact-hours per day with community members (including family).
We estimated that each community member on average spends 81 contact-hours per day interacting with other community members, including time with family, work, shopping, and socializing.
SARS-CoV-2 Infectivity
We derived the rate of infectivity per contact-hour from a study of household infections in Wuhan, China (0.002 infections per contact-hour) (12) (Supplement). Following guidelines from the Centers for Disease Control and Prevention, we assumed an infectivity duration of 10 days (38).
Efficacy of NPIs
The MinSocDist strategy decreased student–student contact-hours by 26% and reduced the overall daily transmission rate from 0.238 (reproduction number [Rt] = 2.38) to 0.167 (Rt = 1.67) (Table 1). The ExtSocDist strategy decreased student–student contact-hours by 39%, student–faculty contact-hours by 50%, and faculty–student contact-hours by 60%; it reduced the overall daily transmission rate to 0.141 (Rt = 1.41).
The published efficacy of masks in reducing infectivity ranges from 44% to 82% (10). Recognizing that students may use different types of masks and may not wear them at all times, we used a base-case infectivity reduction for masks of 50% and adherence of 50%, and we varied these parameters in sensitivity analyses (9). The overall daily transmission rates for the Masks and ExtSocDist+Masks strategies were 0.128 (Rt = 1.28) and 0.105 (Rt = 1.05), respectively.
To capture potential “fatigue” that students, faculty, and community members might experience over time in adhering to NPIs, we used “transmission rate multipliers” to increase transmission rates by 25% for the second month of the semester and 50% for the last 2 months.
Self-screening and Laboratory Test Characteristics
We assumed that the accuracy of reporting COVID-19–associated symptoms in a self-screening procedure was 50% for students and 90% for faculty. We also assumed that those with positive results on symptom screening have a 60% chance of adhering to the ResIsol strategy and 100% adherence to the DesigIsol strategy. We stratified the sensitivity of LT by days after infection using published polymerase chain reaction test data (Table 1) (23). We assumed 100% laboratory test specificity and modeled a 1-day delay in receiving test results.
COVID-19 Clinical Characteristics
We derived the probability of progressing to more severe COVID-19 disease stages from published literature (Supplement Table 1).
Costs
We considered costs from a modified societal perspective, including costs associated with implementing mitigation strategies and the resulting costs of COVID-19 treatment. We included costs within the formal health care system (hospital costs) and outside the health care system (those incurred by the college). Utility measures captured lost productivity due to COVID-19–related isolation. For all 24 NPI-based strategies, we increased prepandemic cleaning costs by about 50% ($31.50 per student per semester) to account for additional cleaning (24). For the Masks and ExtSocDist+Masks strategies, we included the cost of masks (one $2 cloth mask per week and one $0.10 disposable mask per day for each student and faculty member; $212 500 per semester in total). Total NPI costs per semester were $151 500 for MinSocDist, $407 500 for ExtSocDist, and $620 000 for ExtSocDist+Masks. In the base-case analysis, we assumed that colleges would negotiate a SARS-CoV-2 test cost of $10 (about 25% of the lowest published price) (25). We used data from the Healthcare Cost and Utilization Project to derive costs per day for hospital and ICU care ($1640 and $2680, respectively) (Table 1). We estimated the cost of college-sponsored DesigIsol at $30 per day, between the maintenance cost per student per day ($5) (24) and the daily cost of room and board ($55) (26).
Sensitivity Analyses
In sensitivity analyses, we varied the efficacy of masks (50% to 67% infectivity reduction), students' adherence to wearing masks (50% to 80%), and the sensitivity of laboratory tests (50% to 90%). We varied the costs of LT ($1 to $51), a daily DesigIsol unit ($5 to $55), and online educational software ($100 000 to $500 000) for 1 semester for 5000 students and 1000 faculty (37). We also did a threshold analysis to determine the percentage of students who would need to defer for a semester (that is, not pay tuition and room and board) to make the CampusClosed strategy clinically and economically worse than the other strategies. We also determined the laboratory test cost that produced an ICER less than $100 000 per QALY (39).
Role of the Funding Source
The National Institutes of Health had no role in the design or conduct of this study or in the decision to submit this work for publication.
Results
Clinical Outcomes: Cumulative Infections
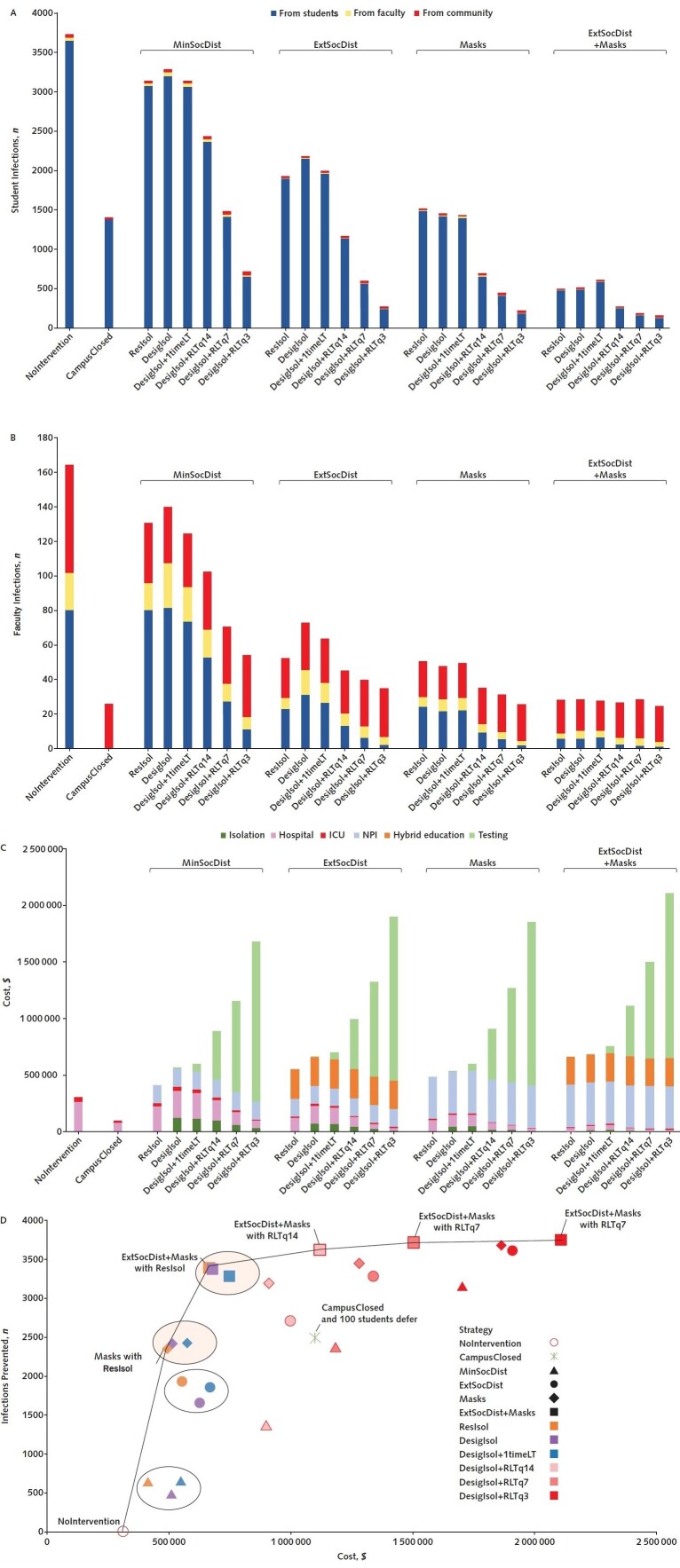
We estimate that the NoIntervention strategy would lead to infections among 75% of students and 16% of faculty, or 3699 incident and 154 prevalent infections per 5000 students and 47 incident and 10 prevalent infections per 1000 faculty (Table 2 and Figure [A and B]). The CampusClosed strategy would reduce student infections by 63% and faculty infections by 84%, with most student infections coming from other students living off campus. The MinSocDist strategy with self-screening or 1-time laboratory screening at the semester start would reduce student infections by 16% relative to NoIntervention. Adding laboratory screening of asymptomatic students every 3 days (RLTq3) to MinSocDist would reduce student infections by 77% to 78% and faculty infections by 59% to 61% relative to MinSocDist alone. Adding RLTq3 to ExtSocDist would reduce student infections by 86% to 87% and faculty infections by 33% to 52% relative to ExtSocDist alone. Without laboratory screening, the Masks strategy would be more effective than either MinSocDist or ExtSocDist, reducing student and faculty infections by 53% to 56% and 64% to 66%, respectively, relative to MinSocDist, and by 31% to 33% and 30% to 34%, respectively, relative to ExtSocDist. Adding RLTq3 to the Masks strategy would reduce infections by 85% to 86% among students and 46% to 49% among faculty relative to Masks alone. Adding RLTq3 to ExtSocDist+Masks would reduce infections by 69% to 70% among students and 11% to 14% among faculty relative to ExtSocDist+Masks alone. The percentage by which adding RLTq3 would reduce the number of infections depends on the isolation strategy (ResIsol vs. DesigIsol).
Table 2. Clinical Outcomes Among Students and Faculty, by Strategy (Results Reported per 5000 Students and 1000 Faculty).
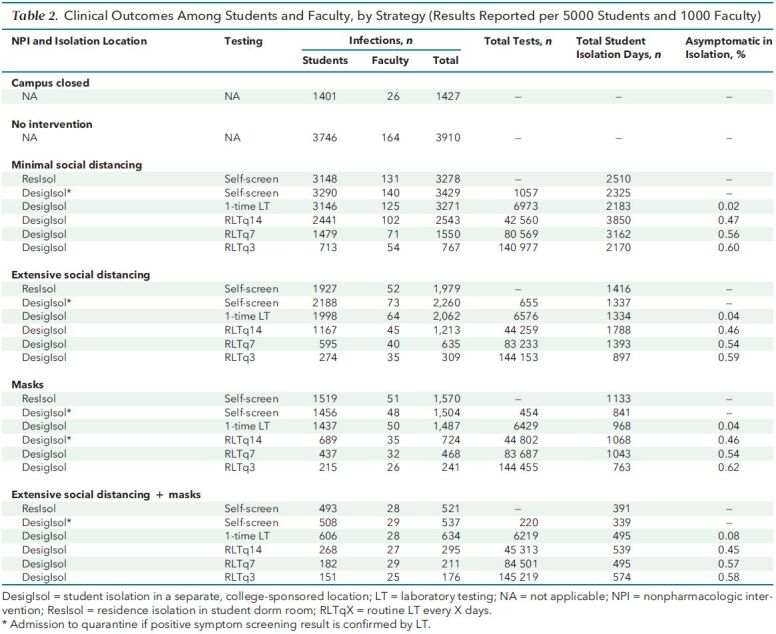
Figure. Infections, costs, and economic efficiency, by COVID-19 mitigation strategy.
1timeLT = 1-time laboratory testing; CampusClosed = campus remains closed with only online education; COVID-19 = coronavirus disease 2019; DesigIsol = student isolation in a separate, college-sponsored location; ExtSocDist = extensive social distancing; ICU = intensive care unit; LT = laboratory testing; Masks = mask-wearing policies; MinSocDist = minimal social distancing; NoIntervention = campus operates as it did before COVID-19 without any mitigation interventions; NPI = nonpharmacologic intervention; ResIsol = residence isolation in student dorm room; RLT = routine LT; RLTqX = RLT every X days. A-C. The number and source of infections among students (A) and faculty (B) for each strategy, and total costs (C). On the left are the NoIntervention and CampusClosed strategies. The 4 broad NPI strategies (MinSocDist, ExtSocDist, Masks, and combined ExtSocDist and Masks) are further stratified by the use and frequency of LT, ranging from no LT, where those who report symptoms associated with COVID-19 are asked to isolate in their residence for 10 d; to 1 test for those who report symptoms to confirm placement in isolation; to RLT for all students and faculty at the start of the semester; to RLT among asymptomatic students and faculty at 3-, 7-, or 14-d intervals. Infections decrease as strategies increase in intensity, from MinSocDist to the ExtSocDist+Masks strategy. In each case, adding LT further decreases infections. Among students, most infections are from other students (A). Among faculty, depending on the strategy, most infections are from the community and other faculty (B). In strategies without RLT, hospital and ICU costs account for >50% of total costs (C). In strategies with RLT, testing accounts for >50% of total costs. Cost per test was $10. D. The efficiency frontier (cost per infection prevented) for COVID-19 mitigation strategies. The efficiency frontier represents the relationship between infections prevented (vertical axis) and total costs (horizontal axis). NoIntervention is shown in the open red circle on the lower left. Without RLT or testing at the semester start, regardless of isolation approach, there is clustering (ovals) of strategies involving MinSocDist (triangles), ExtSocDist (circles), Masks (diamonds), and ExtSocDist+Masks (squares). Unshaded ovals represent strategies where masks are not incorporated, and beige ovals represent clustering of strategies where masks are incorporated. More infections are prevented when masks are used. Symbols on the solid black line represent economically efficient strategies. The slope of the solid line represents the incremental cost per infection prevented for each strategy, compared with the next less costly efficient strategy. Testing at 14-, 7-, or 3-d intervals prevents additional infections, but at a substantially increased cost per infection prevented.
Clinical Outcomes
We estimate that the NoIntervention strategy would lead to 217 hospital days and 8 ICU days among students and 40 hospital days and 12 ICU days among faculty. The ExtSocDist+Masks strategy would reduce the number of hospital days by 87% among students (to 29 hospital days) and by 95% among faculty (to 2 hospital days).
The incidence of new infections varied greatly across strategies. Maximum daily rates of new infection were highest with the MinSocDist strategy, ranging from 582 cases per day in the absence of laboratory screening to 131 per day when frequent laboratory screening (every 3 days) was implemented. The additional value of screening in the presence of extensive social distancing and masks was lower: Maximum daily incidence of new infections ranged from 115 per day without LT to 47 per day with RLT.
Economic Evaluation
Budgetary Impact
The CampusClosed strategy cost $1 099 181 if 100 students (2%) took a “gap semester” (Table 3). Without RLT, MinSocDist cost $414 749 to $546 927, ExtSocDist cost $551 693 to $667 518, the Masks strategy cost $448 254 to $576 108, and ExtSocDist+Masks cost $664 015 to $747 829. Adding RLTq3 to ExtSocDist+Masks led to a total cost of $2 110 595, and adding it to MinSocDist cost $1 702 406.
Table 3. Cost-Effectiveness of COVID-19 Mitigation Strategies on U.S. College Campuses.
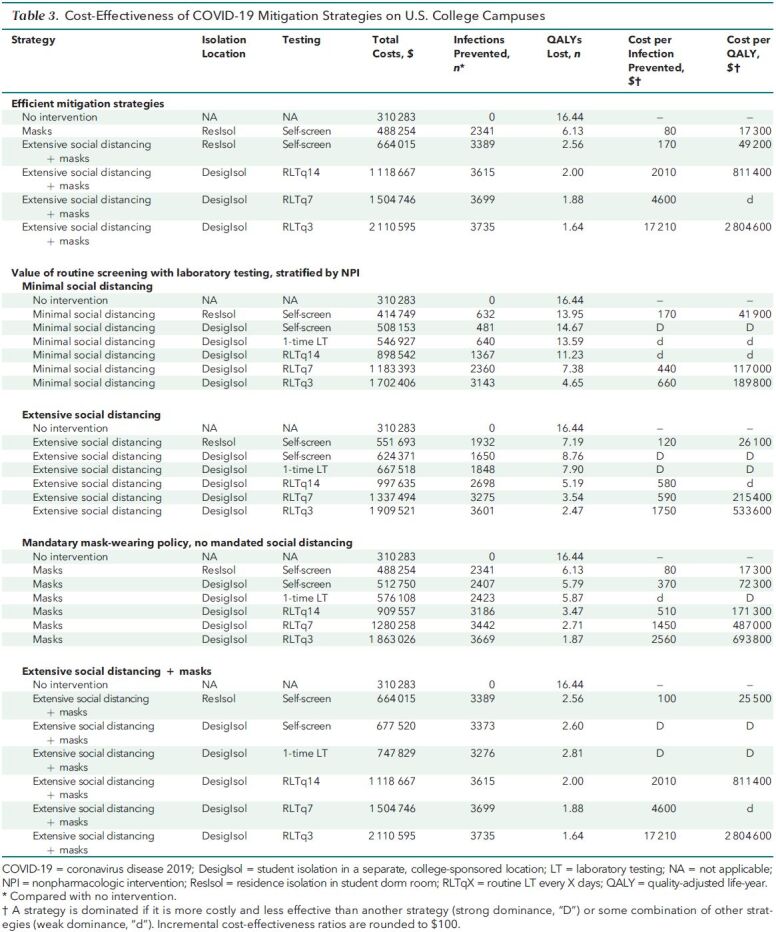
Cost-Effectiveness
Different strategies led to substantially different cost per infection prevented and cost per QALY. The Figure (D) presents the overall results of the cost-effectiveness analysis and highlights the efficient strategies by connecting them in an efficiency frontier. The numerical values used to calculate ICERs are presented in Table 3 (top).
The MinSocDist strategy was never economically efficient relative to ExtSocDist, assuming that the number of students taking a gap semester did not differ between the 2 strategies. Masks alone cost $80 per infection prevented ($17 300 per QALY). We estimated the incremental value of ExtSocDist+Masks to be $170 per infection prevented (ICER, $49 200 per QALY). Adding RLT every 14 days (RLTq14) to ExtSocDist+Masks led to a cost of $2010 per infection prevented (ICER, $811 400 per QALY). Adding more frequent testing to ExtSocDist+Masks prevented more infections but cost much more, at $4600 per infection prevented for RLT every 7 days (RLTq7) and $17 210 per infection prevented for RLTq3, both with ICERs above $1 million per QALY.
Table 3 (bottom) stratifies the cost-effectiveness results by underlying NPI strategy (MinSocDist, ExtSocDist, Masks, and ExtSocDist+Masks). This table indicates the cost and amount of testing required to prevent a certain number of infections for each NPI strategy. For example, to prevent at least 3000 infections, each strategy would cost and require the following amount of testing: MinSocDist would require RLTq3 for $1.7 million, ExtSocDist would require RLTq7 for $1.3 million, Masks would require RLTq14 for $900 000, and ExtSocDist+Masks would require the least amount of testing (1-time LT) and cost the least ($750 000).
Sensitivity Analyses
Without RLT, the value of ExtSocDist depended on its cost components. If the implementation cost of ExtSocDist doubled from $250 000 to $500 000, ExtSocDist+ResIsol cost $250 per infection prevented ($53 000 per QALY). Lowering the cost of designated isolation spaces from $30 to $5 per room per day reduced total costs attributable to COVID-19 mitigation by 0.7% to 1.7% ($8500 to $14 300), depending on the strategy. If the number of students electing to take a gap semester increased even minimally as a result of the more restrictive social distancing measures associated with ExtSocDist compared with MinSocDist, then MinSocDist would be a more favorable strategy. However, neither MinSocDist nor ExtSocDist was as economically efficient as Masks alone.
Increasing the sensitivity of the polymerase chain reaction test to 90% did not qualitatively change the cost-effectiveness of the screening strategies, which included routine polymerase chain reaction testing.
The most influential factors affecting the value of RLT were test costs and frequency. If test costs were lowered to $1 per test, then adding RLTq3 to Masks led to a favorable cost of $160 per infection prevented ($42 700 per QALY) and adding RLTq14 to ExtSocDist+Masks led to $210 per infection prevented ($83 600 per QALY). The full results are presented in Supplement Table 3.
Discussion
We conducted a model-based evaluation of the effect of COVID-19 mitigation strategies on college campuses, considering heterogeneous transmission across students and faculty and transmission from the surrounding community. Despite increased caseload throughout the country, the reported statistics indicate that the prevalence of COVID-19–susceptible individuals has not decreased substantially, making our analysis timely and relevant. This analysis provides insights to college administrators (isolation capacity and cost of mitigation strategies), as well as to public health officials, about the health consequences of specific mitigation strategies (infections, hospital days, and ICU days). This dual emphasis is recommended by the Second Panel on Cost-Effectiveness in Health and Medicine (17).
We examined the value of social distancing, mask-wearing policies, and routine laboratory testing of asymptomatic students and faculty. We had 4 major findings. First, even if campuses remain closed, there will likely be many infections among faculty from the community and among students who return to live off campus in and around the college town. Second, although minimal social distancing (such as canceling large college-sponsored events) would reduce infections, and extensive social distancing with hybrid education would lead to even fewer infections, a mandatory mask-wearing policy alone would reduce infections the most. Combining a mask-wearing policy with extensive social distancing would prevent 87% of infections among students and faculty and would cost $170 per infection prevented ($49 200 per QALY saved). Third, although adding testing every 14 days to a strategy combining social distancing and a mask-wearing policy would also reduce infections, it would cost much more per infection prevented, even at $10 per test (25% of the lowest available price), relative to the same strategy without testing. Reducing test costs to $1 per test would yield a much better value for strategies involving testing every 3 days. Fourth, although most infections among students were from other students, most faculty infections were not from students because most faculty live off campus and spend a substantial amount of time in the community.
As noted earlier, adding routine testing to a policy involving extensive social distancing and mask wearing reduced infections the most, but at a high cost per infection prevented. Even if colleges can support the financial and operational burden of testing, other factors, such as laboratory capacity and the availability of testing supplies, may affect its feasibility. In Massachusetts, where more than 100 colleges have a combined student population of more than 500 000, RLTq14 would require 36 000 tests per day for students alone (40). This would divert resources away from symptomatic, nonstudent populations and those in close contact with persons with confirmed COVID-19. Considering these tradeoffs, it is critical to implement mitigation programs, such as extensive social distancing and mask-wearing policies, that do not rely primarily on testing capacity.
Our results suggest that although routine screening with laboratory testing among asymptomatic students and faculty reduces infections, the economic value of such testing at current test prices is above willingness-to-pay thresholds that are frequently used in the United States. As a result, many colleges could not afford routine laboratory screening for mitigation. It might be manageable for some small and medium-sized private colleges, but it may be less economically feasible for large, publicly funded colleges. Less costly tests could alleviate this problem, making routine laboratory screening of higher value and more affordable for both private and public colleges. Our results highlight that if colleges invested less in NPIs, they would need to rely more on routine laboratory screening, at higher cost, to prevent the spread of COVID-19. These results could help college administrators with decision making regarding laboratory testing and in negotiations on test costs.
Two recent studies have examined COVID-19 mitigation strategies for U.S. colleges. Paltiel and colleagues (41) examined routine surveillance screening under several epidemic scenarios, defined by an Rt of 1.5 to 3.5. Consistent with our analysis, they found that more frequent testing prevented more infections. Our MinSocDist strategy, resulting in an Rt between 1.7 and 2.6, yielded a cost of $660 per infection prevented, which is similar to the cost of $600 per infection prevented that Paltiel and colleagues reported for their base-case analysis, in which the Rt was 2.5. In our analysis, we report the incremental value of NPIs and the added value of routine laboratory screening under alternative NPI scenarios. Differences in the apparent value of routine laboratory testing between these 2 analyses likely result from our explicit modeling of rigorous social distancing and mask-wearing policies, which led to a lower added value of testing.
A report from Cornell University (42) also found that routinely testing asymptomatic students would prevent the most infections. Although this report suggested pooling specimens to reduce costs, no explicit economic analysis was presented. Similar to our analysis, this report suggests that keeping campuses closed may yield more infections than bringing students back with NPIs because a closed campus would not have structured programs or oversight to promote students' adherence to mask wearing and social distancing.
Our results should be viewed in the context of several limitations. First, although we tried to capture the major COVID-19 mitigation strategies that colleges are considering, we examined only a limited number of strategies. We did not capture all externalities that institutions might face, such as lost sports revenue and the effect of social distancing on students' QoL, nor did we examine the effect of contact tracing on transmission. Although we modeled heterogeneity across 3 groups (students, faculty, and community), we did not account for the heterogeneity of transmission within each group (for example, students living off campus vs. on campus), which would have required additional and unavailable data. We were also unable to track or quarantine close contacts of infected individuals because CEACOV is a dynamic, population-based model.
We could not find reliable data on the accuracy of self-reported symptom screening among students and therefore assumed a low rate of accuracy because it may not be in students' self-interest to report mild symptoms. We did not include lost revenue from not receiving room and board payment because we could not find data on the proportion of students electing to study from home stratified by whether their school mandated social distancing. Finally, there is uncertainty about many aspects of COVID-19 testing and the immune response. We used the best currently available data and limited our analysis to 1 semester.
In conclusion, extensive social distancing and mandatory mask-wearing policies would enable higher education institutions to have the greatest effect in reducing COVID-19 infections among students and faculty. Routine laboratory testing would further reduce infections but would require lower-cost tests combined with markedly increased capacity to be feasible for many colleges.
Supplementary Material
Footnotes
This article was published at Annals.org on 21 December 2020
* Drs. Kazemian and Freedberg contributed equally to this work.
References
- 1. UnivStats. Total number of employees at U.S. colleges by occupation. 2020. Accessed at www.univstats.com/staffs on 2 December 2020.
- 2. National Center for Education Statistics. College Navigator. Accessed at https://nces.ed.gov/collegenavigator on 2 December 2020.
- 3. The New York Times. Tracking the coronavirus at U.S. colleges and universities. Updated 19 November 2020. Accessed at www.nytimes.com/interactive/2020/us/covid-college-cases-tracker.html on 2 December 2020.
- 4. McChesney J, Bichsel J. The aging of tenure-track faculty in higher education: implications for succession and diversity. College and University Professional Association for Human Resources. 2020. Accessed at www.cupahr.org/wp-content/uploads/CUPA-HR-Brief-Aging-Faculty.pdf on 2 December 2020.
- 5. Clark A , Jit M , Warren-Gash C , et al; Centre for the Mathematical Modelling of Infectious Diseases COVID-19 working group. Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. Lancet Glob Health. 2020;8:e1003-e1017. [PMID: ] doi: 10.1016/S2214-109X(20)30264-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. DePietro A. Here's a look at the impact of coronavirus (COVID-19) on colleges and universities in the U.S. Forbes. 30 April 2020. Accessed at www.forbes.com/sites/andrewdepietro/2020/04/30/impact-coronavirus-covid-19-colleges-universities/?sh=52861a4161a6 on 2 December 2020.
- 7. Hadden J. What the top 25 colleges and universities in the US have said about their plans to reopen in fall 2020, from postponing the semester to offering more remote coursework. Business Insider. 8 May 2020. Accessed at www.businessinsider.in/international/news/what-the-top-25-colleges-and-universities-in-the-us-have-said-about-their-plans-to-reopen-in-fall-2020-from-postponing-the-semester-to-offering-more-remote-coursework/slidelist/75631798.cms on 2 December 2020.
- 8. Logan T. Dorm rooms at the Westin? Hotels and universities are teaming up to offer socially distanced student housing. Boston Globe. 26 July 2020. Accessed at www.bostonglobe.com/2020/07/26/business/dorm-rooms-westin-hotels-universities-are-teaming-up-offer-socially-distanced-student-housing on 2 December 2020.
- 9. Stutt ROJH , Retkute R , Bradley M , et al. A modelling framework to assess the likely effectiveness of facemasks in combination with ‘lock-down' in managing the COVID-19 pandemic. Proc Math Phys Eng Sci. 2020;476:20200376. [PMID: ] doi: 10.1098/rspa.2020.0376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chu DK , Akl EA , Duda S , et al; COVID-19 Systematic Urgent Review Group Effort (SURGE) study authors. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395:1973-1987. [PMID: ] doi: 10.1016/S0140-6736(20)31142-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hethcote HW. The mathematics of infectious diseases. SIAM Rev Soc Ind Appl Math. 2000;42:599-653. doi:10.1137/S0036144500371907
- 12. Li W , Zhang B , Lu J , et al. Characteristics of household transmission of COVID-19. Clin Infect Dis. 2020;71:1943-1946. [PMID: ] doi: 10.1093/cid/ciaa450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Andrade LF , Saba G , Ricard JD , et al. Health related quality of life in patients with community-acquired pneumococcal pneumonia in France. Health Qual Life Outcomes. 2018;16:28. [PMID: ] doi: 10.1186/s12955-018-0854-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yang J , Jit M , Zheng Y , et al. The impact of influenza on the health related quality of life in China: an EQ-5D survey. BMC Infect Dis. 2017;17:686. [PMID: ] doi: 10.1186/s12879-017-2801-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kolovos S , Bosmans JE , van Dongen JM , et al. Utility scores for different health states related to depression: individual participant data analysis. Qual Life Res. 2017;26:1649-1658. [PMID: ] doi: 10.1007/s11136-017-1536-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Centers for Disease Control and Prevention. Percentage of visits of ILI by age group reported by a subset of ILINet providers. Updated 21 August 2020. Accessed at www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/08212020/percent-ili-visits-age.html on 2 December 2020.
- 17. Carias C , Chesson HW , Grosse SD , et al. Recommendations of the Second Panel on Cost Effectiveness in Health and Medicine: a reference, not a rule book. Am J Prev Med. 2018;54:600-602. [PMID: ] doi: 10.1016/j.amepre.2017.11.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Reddy KP , Shebl FM , Foote JHA , et al. Cost-effectiveness of public health strategies for COVID-19 epidemic control in South Africa: a microsimulation modelling study. Lancet Glob Health. 2020. [PMID: ] doi: 10.1016/S2214-109X(20)30452-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Neilan AM , Losina E , Bangs AC , et al. Clinical impact, costs, and cost-effectiveness of expanded SARS-CoV-2 testing in Massachusetts. Clin Infect Dis. 2020. [PMID: ] doi: 10.1093/cid/ciaa1418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Baggett TP, Scott JA, Le MH, et al. Management strategies for people experiencing sheltered homelessness during the COVID-19 pandemic: clinical outcomes and costs. JAMA Netw Open. 2020. [Forthcoming.] [DOI] [PMC free article] [PubMed]
- 21. Wang D , Hu B , Hu C , et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061-1069. [PMID: ] doi: 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lauer SA , Grantz KH , Bi Q , et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172:577-582. doi: 10.7326/M20-0504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kucirka LM , Lauer SA , Laeyendecker O , et al. Variation in false-negative rate of reverse transcriptase polymerase chain reaction-based SARS-CoV-2 tests by time since exposure. Ann Intern Med. 2020;173:262-267. doi: 10.7326/M20-1495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Agron J. 38th annual Maintenance & Operations Cost Study for colleges. American School & University. 1 April 2009. Accessed at www.asumag.com/research/article/20851272/38th-annual-maintenance-operations-cost-study-for-colleges on 2 December 2020.
- 25. Centers for Medicare & Medicaid Services. Medicare Administrative Contractor COVID-19 test pricing. 19 May 2020. Accessed at www.cms.gov/files/document/mac-covid-19-test-pricing.pdf on 2 December 2020.
- 26. Tufts University Undergraduate Admissions. Cost and aid. Accessed at https://admissions.tufts.edu/tuition-and-aid/tuition-and-aid on 12 December 2020.
- 27. Marzell M , Bavarian N , Paschall MJ , et al. Party characteristics, drinking settings, and college students' risk of intoxication: a multi-campus study. J Prim Prev. 2015;36:247-58. [PMID: ] doi: 10.1007/s10935-015-0393-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. U.S. Bureau of Labor Statistics. Databases, tables & calculators by subject. 2020. Accessed at www.bls.gov/data on 2 December 2020.
- 29. Fosnacht K, McCormick AC, Lerma R. First-year students' time use in college: a latent profile analysis. Res High Educ. 2018;59:958-78. doi:10.1007/s11162-018-9497-z
- 30. Bronkema R. Campus Friends, Gender, and College Student Success. Dissertation. Bowling Green State University; 2014. Accessed at https://scholarworks.bgsu.edu/he_diss/61 on 2 December 2020.
- 31. U.S. Census Bureau. Datasets. Accessed at www.census.gov/data/datasets.html on 2 December 2020.
- 32. Mossong J , Hens N , Jit M , et al. Social contacts and mixing patterns relevant to the spread of infectious diseases. PLoS Med. 2008;5:e74. [PMID: ] doi: 10.1371/journal.pmed.0050074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Google. COVID-19 community mobility reports. 2020. Accessed at www.google.com/covid19/mobility on 2 December 2020.
- 34. Cox C, Rudowitz R, Neuman T, et al. How health costs might change with COVID-19. Peterson-KFF Health System Tracker. 15 April 2020. Accessed at www.healthsystemtracker.org/brief/how-health-costs-might-change-with-covid-19 on 2 December 2020.
- 35. Rae M, Claxton G, Kurani N, et al. Potential costs of COVID-19 treatment for people with employer coverage. Peterson-KFF Health System Tracker. 13 March 2020. Accessed at www.healthsystemtracker.org/brief/potential-costs-of-coronavirus-treatment-for-people-with-employer-coverage on 2 December 2020.
- 36. FAIR Health. COVID-19: the projected economic impact of the COVID-19 pandemic on the US healthcare system. 25 March 2020. Accessed at https://s3.amazonaws.com/media2.fairhealth.org/brief/asset/COVID-19%20-%20The%20Projected%20Economic%20Impact%20of%20the%20COVID-19%20Pandemic%20on%20the%20US%20Healthcare%20System.pdf on 2 December 2020.
- 37.Zoom business price plan. Accessed at www.zoom.us on 2 December 2020.
- 38. Centers for Disease Control and Prevention. Duration of isolation and precautions for adults with COVID-19. Updated 19 October 2020. Accessed at www.cdc.gov/coronavirus/2019-ncov/hcp/duration-isolation.html on 2 December 2020.
- 39. Neumann PJ , Cohen JT , Weinstein MC . Updating cost-effectiveness—the curious resilience of the $50,000-per-QALY threshold. N Engl J Med. 2014;371:796-7. [PMID: ] doi: 10.1056/NEJMp1405158 [DOI] [PubMed] [Google Scholar]
- 40. UnivStats. Student population at Massachusetts colleges. 2020. Accessed at www.univstats.com/states/massachusetts/student-population on 2 December 2020.
- 41. Paltiel AD , Zheng A , Walensky RP . Assessment of SARS-CoV-2 screening strategies to permit the safe reopening of college campuses in the United States. JAMA Netw Open. 2020;3:e2016818. [PMID: ] doi: 10.1001/jamanetworkopen.2020.16818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Cashore JM, Duan N, Janmohamed A, et al. COVID-19 mathematical modeling for Cornell's fall semester. Cornell University. 15 June 2020. Accessed at https://covid.cornell.edu/_assets/files/covid_19_modeling_main_report.pdf on 2 December 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.