Abstract
Objective:
Many high school students experience a high degree of anxiety and perceived stress. This study examined whether a classroom-based mindfulness program or a wellness program were acceptable and effective as anxiety and stress reduction interventions based on students’ self-reports.
Design, setting, and participants:
Thirteen health education classes (n=285 students, aged 14–16 years) were randomized by classroom to one of three conditions: mindfulness, wellness, or usual health class only (passive control/ waitlist), for 8 weeks.
Outcomes:
Pre- and post-intervention scores compared self-reported measures of depression, anxiety and stress.
Results:
Complete data were available from nine classes (n=202 students). Post-intervention anxiety scores were reduced in students who received the mindfulness intervention compared to those who received only their usual health class (β=−0.07, SE=0.03, P≤0.001; 95% CI=−0.12, −0.02). No significant between group differences were found for depression or stress (P>0.4). Students’ satisfaction with the mindfulness intervention they received withstood baseline credibility and expectancy effects: r=0.21, n=67, P=0.17 for credibility; r=−0.001, n=67, P=0.99 for expectancy. However, students’ satisfaction with the wellness intervention they received was positively correlated with their pre-intervention expectations, r=0.42, n=47, P>0.001. Fifty-two percent of the 68 students assigned to mindfulness (n=35) used the iPad app for mindfulness home practice at least once; of those, 10% used it 10 or more times.
Conclusion:
Eight weeks of classroom-based mindfulness, with limited home practice, reduced self-reported anxiety compared to usual health class, and withstood baseline expectancy effects in this group of high school students, a majority who come from high income families.
Clinical implications:
School- or community-based mindfulness may be an appropriate recommendation for adolescents who experience anxiety.
Keywords: Mindfulness, Stress reduction, Wellness, Anxiety, Adolescents, High school
INTRODUCTION
Adolescence is a developmental period often accompanied by depression, anxiety, and stress.1 In addition to the physical and mental changes of puberty, the burgeoning complexity of adolescents’ social relationships combined with the increasing academic pressure of high school add layers of potential stress and anxiety to an adolescent’s life.2, 3 Teenagers report more stress during the school year than most adults during the same time period.4 Although excessive stress negatively affects adolescents and adults similarly by worsening sleep and appetite, among other effects,4 adolescents may be at risk for additional adverse effects given that this is a period for rapid brain development.5
Frontal-limbic neural networks are developing asynchronously during this period, making teens potentially more sensitive to social cues and responsive to emotional signals, while regulation is still immature.1 This developmental phase leaves them arguably more vulnerable to the negative effects of excessive stress and anxiety.5 Teenage stress has been associated with behavioral problems,6 poor eating habits,7 risky sexual behavior,6 smoking,8 substance abuse, self-harm,9 depression,10 and suicidality6.
Mindfulness, which involves bringing one’s attention to the present moment, in a non-judgmental way, noticing thoughts, sensations and experiences with a non-reactive, curious and open perspective,11 has shown some benefit for symptoms of depression, anxiety and stress.12 While some mindfulness practices are associated with eastern religions as part of their origin, mindfulness training, as offered in this study, was focused on a cognitive and breathing practice without religious symbolism.
While mindfulness training with individuals, or in small groups, appears to have benefit for stress and anxiety reduction in adults,13 far less is known about its value in adolescents, particularly within the school setting. In a preliminary uncontrolled study of elementary school children (n=409), mindfulness training improved in-class behavior, as rated by the teachers who delivered the daily curriculum.14 In a study of adolescent boys (n=155), mindfulness, delivered by the teacher as part of religious education class for 4 weeks, did not show differences in self-reported well-being or resilience when compared to usual religious class. However, among those who received mindfulness, greater well-being was associated with the amount of mindfulness practice.15 In a non-randomized study, among 129 public high school students who received eighteen 15–25 minute sessions of mindfulness delivered as part of choir class, lower levels of perceived stress and psychosomatic complaints were reported compared to (n=87) students in choir class as usual.16 In an uncontrolled study of a 6-week mindfulness intervention combined with sleep hygiene for adolescents with poor sleep quality at baseline (n=10), improvements were reported on a number of sleep-related domains. However, no controlled studies with an active control were found.
Within a small clinical population, a pilot study of mindfulness for adolescents and adults (n=8 and 24, respectively) with attention-deficit/hyperactivity disorder (ADHD) found improvements in attentional skills and mood.17 In youth with substance use problems (n=18), 6 weeks of mindfulness increased reported total sleep time.18
While evidence suggests that mindfulness may improve anxiety- and stress-related symptoms for adolescents,19 few studies have investigated the benefit of mindfulness provided as part of a regular high school curriculum, which may offer a time- and cost-effective strategy for helping adolescents cope effectively with anxiety and stress. To address the gap, this study enrolled a large student sample, and compared mindfulness to an active and a passive control.
The primary aims of this three-arm study were to (1) evaluate the acceptability of mindfulness, delivered by an outside provider as part of a regular high school health class, compared to an active control intervention control (wellness education), or passive control/waitlist (usual health class), and, (2) to measure the interventions’ effects on depression, anxiety, and stress.
METHODS
DESIGN
This cluster-randomized study of students who attended a private, college-preparatory high school used a repeated measures, experimental design, utilizing within- and between-subject comparisons of the participants. A detailed description of the study design may be found in Johnstone, Roake20 and is explained briefly below.
PARTICIPANTS
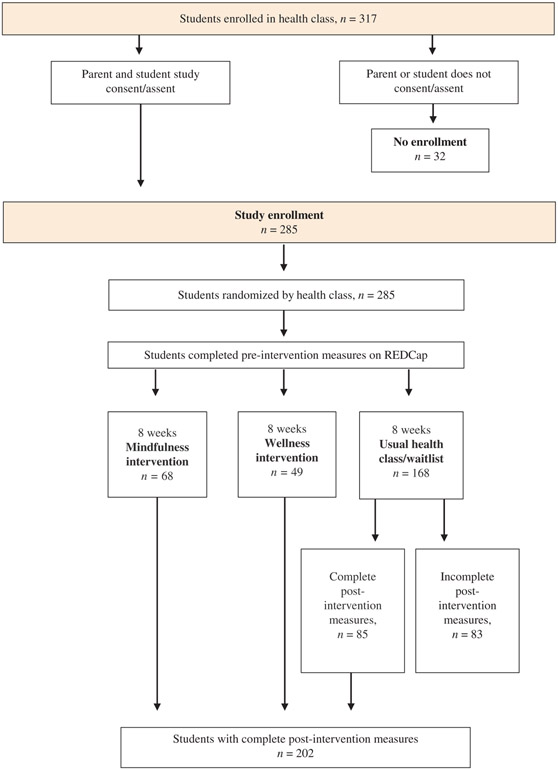
All students taking a non-elective 10th grade health class (students ages 14–16 years) at a Catholic high school were recruited to participate in the study. Of 317 eligible students, 285 (90%) provided parent and child consent/assent and were enrolled. Students were randomized by classroom to one of three study arms: mindfulness, n=68 in three classrooms; wellness, n=49 in two classrooms; or usual health class (passive control/waitlist) n=168 in eight classrooms. The number of classrooms that received one of the two interventions was based on available resources and teaching schedules. Four of the usual health classes (waitlist) n=83, were unable to complete post-intervention measures due to scheduling constraints, reducing the total number of usual health class only students with complete outcome data to n=85, for a total number of students with complete data as n=202. One student within the mindfulness classes, and two students within the wellness classes appeared to use the same answer for all responses, so their data were removed from analyses, leaving n=67 for mindfulness and n=47 for wellness. Removal did not change results. See CONSORT diagram for study flow (Figure 1).
Figure 1:
CONSORT diagram of study flow.
INCLUSION/EXCLUSION CRITERIA
High School students who (1) were enrolled in 10th grade health class, (2) had access to an iPad or computer, and (3) stated they were willing to abide by randomization process and to commit to daily practice of mindfulness or wellness activities for the duration of the study, (4) both student and parent agreed to study with informed assent/consent respectively.
COMPLIANCE WITH ETHICAL STANDARDS
All procedures performed in this study were approved by the University’s Institutional Review Board, and in accordance with the ethical standards as laid down in the 1964 Helsinki declaration and its later amendments. The study was prospectively registered with clinicaltrials.gov, NCT02629016.
PROCEDURES
Following parent consent and student assent, students were enrolled in the study using the Research Electronic Data Capture (REDCap) system.21 REDCap was also used to electronically collect students’ responses to questionnaires pre- and postintervention, during one class period before and after the study. After completing pre-intervention questionnaires, students were randomized by classroom to one of the three study conditions using an Excel random number generator. Both of the active interventions (mindfulness and wellness) were delivered during one of the four health periods each week, for 8 weeks, by a psychologist resident (first author, JJ). The remaining three health periods each week comprised the usual curriculum and were taught by the regular classroom teacher. Waitlisted students received their usual health curriculum four periods per week, taught by the regular classroom teacher. See Figure 2 for details of the usual health class curriculum. Students who completed the study, defined a priori by attending at least 6 of the 8 intervention classes and completing the pre- and post-questionnaires, were entered into a drawing for one $20 Visa gift card per classroom.
Figure 2:
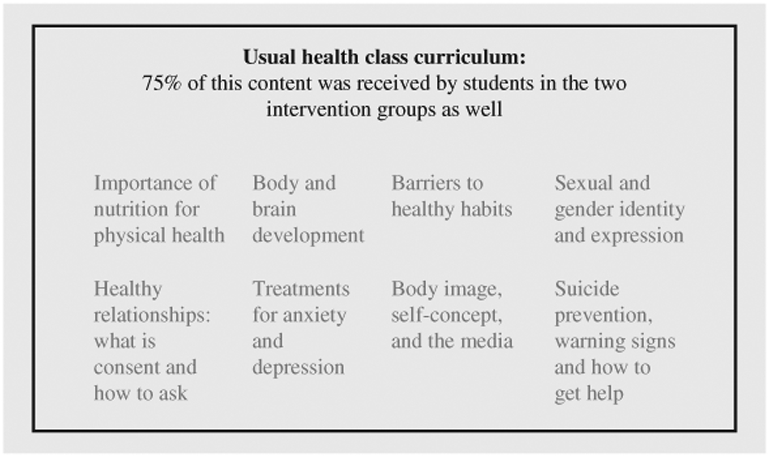
Topics covered in usual health class in four periods per week during the 8-week study.
INTERVENTIONS
Both of the active interventions were delivered by a psychologist resident (first author, JJ) who completed a certified Mindfulness Based Stress Reduction (MBSR)11 course taught by a certified teacher (co-author, HW) and has practiced yoga for more than a decade. She has trained in and used the contemplative therapy practice, Acceptance and Commitment Therapy (ACT)22 for 6 years.
Mindfulness Class
The mindfulness curriculum was specifically created for this study population, based on previously tested programs. Students were taught mindfulness principles based on a combination of: MBSR,11 shortened in length to fit the 1-hour-per-week, 8-week format, reinforced by experiential activities from the mindful therapy practice, ACT, using the book, Get Out of Your Mind and Into Your Life For Teens23 and the school-based curriculum for teaching mindfulness in schools, The MindUP Curriculum: Brain-Focused Strategies for Learning and Living,24 which was adapted for use with adolescents. Classroom activities and discussion followed the MBSR model and encouraged the incorporation of focused awareness, non-judgemental noticing of thoughts and their transient nature (mindfulness), and the practice of these skills in every life (e.g. mindful eating or walking). Each class began and ended with 5–10 minutes of mindfulness meditation during which the students were guided through the practice of mindful breathing, noticing physical sensations and thoughts, and gently guiding themselves back to noticing their breathing when their mind wandered. Depending on personal preference, students sat at their desks, or laid on mats on the floor for the guided mindfulness meditation. See Table 1 for specific elements of the mindfulness intervention. To encourage daily mindfulness practice outside the classroom, students were provided with Headspace© (https://www.headspace.com), an app that they downloaded onto their school-assigned iPads. Students were instructed to use the app for 10 minutes of guided mediation, daily. The students’ use of the Headspace app was tracked electronically by Headspace, based on the unique code provided to each student. Following study completion, these usage data (student code and usage time in minutes) were sent to the researchers for analyses. No other student details were collected or accessed via this tracking system and Headspace did not receive any protected health or identifying information. Students were aware that their usage was tracked.
Table 1:
Core components of the mindfulness and wellness classes
| Session | Mindfulnessa | Wellnessb |
|---|---|---|
| 1 | Mindfulness overviewa,c Acting mindfully vs. being on autopilota,g |
Wellness overviewb,d Types of stress: eustress and distress |
| 2 | Body awareness, body scana Noticing the wandering minda Present moment awarenessa,c |
Causes of stress Circle of influence and controlb The power of proactive peopleb |
| 3 | Yoga, acting mindfully to guide behaviorg
Mindfulness and the brain: amygdala, prefrontal cortex, hippocampush |
Goal setting and creating purposee Finding one’s voice: talent, passione Creating a personal mission statemente |
| 4 | Mindful awareness of breatha Having a thought vs. being a thoughtg Thoughts and the nervous system: internal and external threatsg,h |
Time managementb,f Prioritizing tasks using quadrantsb,f Big vs. Little Rocks: the impact of tasks and activitiesb |
| 5 | Mindful walkinga Emotions as passing experiencesc,g |
Reducing procrastinationb,f Begin with the end in mindb |
| 6 | Mindful listening and speakinga Responding vs. reactinga Acceptance and willingnessg |
Successful relationship buildingb Think Win-Win: less competition in relationshipsb |
| 7 | Mindful eatinga Perspective takinga Developing self and other compassiona |
Lifestyle choices to reduce stressi Importance of good sleep hygiene, exercise, being outdoors i |
| 8 | Integrating mindfulness into daily lifea,h Cultivating gratitudea |
Body postures for confidencej The physiological influence of smilingk,l |
Kabat-Zinn J, Hanh TN. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. Delta; 2009.11
Covey, S. The 7 Habits of Highly Effective Teens: the Ultimate Teenage Success Guide. New York: Touchstone; 2014.25
Mindfulness class asked to use the Headspace App© for 10 minutes of daily guided mindfulness.
Wellness class asked to watch 10 minutes of pre-selected YouTube or TEDtalk videos.
Finding your voice: http://seancovey.com/teens.html.
Covey, SR, Merrill, AR, Merrill, RR. First Things First. New York: Fireside; 1995.42
Ciarrochi J, Hayes L, Bailey A. Get Out of Your Mind & Into Your Life for Teens. Oakland, CA: New Harbinger Publications; 2012.23
The Hawn Foundation (2011). The MindUP Curriculum: Grades 6–8: Brain-Focused Strategies for Learning—and Living, 1st edn. The MindUP Curriculum, Scholastic Teaching Resources.24
Stress management and teens. American Acadamy of Child & Adolescent Psychiatry. Retreived from: https://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFGuideHelpingTeenagers-With-Stress-066.aspx. November, 2015.
Cuddy A. Your body language may shape who you are. Retrieved from: https://www.youtube.com/watch?v=Ks-_Mh1QhMc, November, 2015.
Gutman R. The hidden power of smiling. Retrieved from: https://www.youtube.com/watch?v=U9cGdRNMdQQ. November 2015.
There’s magic in your smile: how smiling affects your brain. Retrieved from: https://www.psychologytoday.com/us/blog/cutting-edgeleadership/201206/there-s-magic-in-your-smile. November 2015.
Wellness Class
Students were taught time management and conflict resolution strategies based on the 7 Habits of Highly Effective Teens25 by the same instructor who delivered mindfulness. Class discussion and activities focused on incorporating principles from the book and other stress reducing concepts into everyday life. See Table 1 for specific elements of the wellness intervention. To control for the 10 minutes of daily home practice assigned to students in the mindfulness classes, students in the wellness classes were asked to watch 10 minutes of preselected TED talks and YouTube videos daily. The videos, specifically chosen as stress reducers, featured humor and inspirational entertainment. While students’ viewing of the videos was not monitored, students were asked to log whether they watched the videos; class discussion incorporated video content. A list of the assigned videos is available by request. Completion of the mindfulness or wellness home practice was not graded.
Usual Health Class (Passive Control/Waitlist)
In lieu of receiving mindfulness or wellness during one class per week, students randomized to the waitlist received their usual health class curriculum for all four periods each week, taught by the usual classroom teacher, with content based on Oregon’s Health Education curriculum.26 All students, including those in the intervention classes, received at least 75% of the usual health class curriculum. Topics included mental and emotional health, body systems, nutrition, self-care, communication skills, and dealing with peer pressure. See Figure 2 for additional detail.
INTERVENTION EQUALITY
To retain the study’s internal validity, the focus on mindfulness as the hypothesized ‘active’ intervention was minimized and the ‘control’ intervention, “wellness,” was presented as a logical and equal alternative. This balanced view of the two active interventions was reflected in the use of “stress reduction” as the reported purpose of the study. While the two interventions types were named in the materials provided to parents and students, the potential benefit of one intervention over the other was not discussed or implied. All students had access to the materials from the other group once the study finished.
OUTCOMES
The two primary outcome domains were intervention acceptability and improvement in three symptom areas – stress, anxiety, and mood.
Acceptability
Acceptability was measured by correlating the students’ reported satisfaction with the intervention they received with their perception of the intervention’s credibility at baseline. Acceptability also included class attendance and the number of out-ofclass “home practice” assignments completed.
Credibility and Expectancy Questionnaire (CEQ)
Credibility and expectancy are considered two nonspecific intervention components that may impact outcome differences between the interventions.27 Prior to randomization, the students’ perceptions of the two interventions, were measured the by the six-item Credibility/Expectancy Questionnaire (CEQ).27 The CEQ contains four “thinking” questions that ask the student to cognitively assess the legitimacy of the intervention, and two “feeling” questions that rely on an affective assessment of the intervention’s potential benefit. The credibility score is derived from the first three “thinking” questions, and the expectancy score is derived from the fourth “thinking” question and both “feeling” questions. The CEQ demonstrated adequate test-retest reliability: 0.75 for credibility, and 0.82 for expectancy.27 Reliability in the current sample was good: α=0.86 for credibility, α=0.93 for expectancy.
Prior to the class being assigned to an intervention group, students received one sentence descriptions of the two interventions and then completed the CEQ. The mindfulness intervention was described as a “way of paying attention to your thoughts, feelings and experiences, in the present moment, without judgment,” and the wellness intervention was described as a “wellness program focused on aspects of healthy living with an emphasis on the 7 Habits of Highly Effective Teens.” While many of the students reported familiarity with the terms “wellness” and “mindfulness,” only one student had practiced mindfulness, and one had previously used the 7 Habits material.
Satisfaction
The students’ satisfaction with the intervention they received was measured, post-intervention, by the eight-item Client Satisfaction Questionnaire (CSQ-8),28 designed to measure an individual’s satisfaction with a health care intervention using answers on a 4-point Likert scale where “1” indicates the lowest degree of satisfaction and “4,” the highest. CSQ-8 scores have been correlated with symptom reduction.28
Attendance and Adherence
Attendance was recorded as the number of classes each student attended. The number of times a student logged in to use the Headspace app for guided mindfulness practice comprised adherence. These data were provided by the Headspace statistical team after the study, with the students’ knowledge. In the wellness classes, adherence was measured by watching the assigned videos, and recorded by student self-report in a written log, and through discussion of videos during class.
Symptom Change
Self-reported levels of depression, anxiety, and stress were measured by the Depression Anxiety and Stress Scale – 21 (DASS-21).29 The DASS-21, an abbreviated 21-item version of the original DASS, is a reliable and valid measure of depression (α=0.88), anxiety (α=0.82), and stress (α=0.90).29 Participants were asked to rate the extent to which they have experienced each of the items over the last week with responses: 0=did not apply to me at all, 1=applied to me to some degree, or some of the time, 2=applied to me to a considerable degree, or a good part of time, 3=applied to me very much, or most of the time. DASS internal consistency was in this sample: DASS total: pre/post α=0.92, 0.91; depression: pre/post α=0.85, 0.77; anxiety: pre/post α=0.80, 0.80; stress: pre/post α=0.80, 0.79.
Mindfulness
The Five Facet Mindfulness Questionnaire (FFMQ)30 assessed levels of mindfulness pre- and post-intervention. The FFMQ is a self-report measure that is used to assess five domains of mindfulness in everyday life: observing, describing, acting with awareness, nonreactivity, and nonjudging.31 An a priori decision was made not to use the describing subscale, which measures one’s ability to label internal experiences with words,31 based on the last author’s findings that this subscale did not change in studied populations, and in an effort to relieve student response burden. The measure has high internal consistency within each facet (α=0.86–0.93).31,32 Internal consistency was good in the current study for the subscales used (α=0.82–0.90).
DATA REDUCTION AND ANALYSIS
IBM SPSS Statistics for Windows, Version 24 (Armonk, NY:IBM Corp. 2016) was used to compute descriptive statistics and compare groups using ANOVA, t-tests and χ2 tests. To test Aim 1 (evaluating the acceptability of mindfulness), we used using ANOVA, t-tests and χ2 tests to examine mean differences on baseline credibility and expectancy, and post-intervention, on their satisfaction with the intervention received, also the frequency of home practice comparing the wellness and the mindfulness groups. As described above, in place of the home practice exercises, the wellness group was asked to watch YouTube videos. However, non-compliance among these students (on average, they viewed videos <10% of the time) undermined our ability to make comparisons between groups. Thus, the wellness group was not included in the home practice acceptability analyses.
To test for intervention group differences in symptom change after intervention (Aim 2), a series of multiple regressions were estimated using Mplus version 7.2 (Los Angeles, CA: Muthén & Muthén, 2012) with the robust maximum likelihood estimator. Non-independence of observations (i.e. the nesting of children within classrooms) was handled with the Mplus cluster command, where classroom was treated as the clustering variable.
Separate models were used to test the effect of group assignment after adjusting for the baseline values of the outcome. If the omnibus analyses were significant, then subgroup analyses were used to compare mindfulness to both of the two controls (wellness, usual health class). In these models, the students’ post-intervention score was regressed on their preintervention score, as well as on their intervention group. Controlling for baseline provides a conservative test of observed difference, and allows for approximation of change following the intervention.
Missing data were handled using full information maximum likelihood. Separate sets of models were run for each of the primary outcomes (DASS subscales: Depression, Stress, and Anxiety) and, due to the exploratory nature of the study, uncorrected P-values are reported.
RESULTS
SAMPLE DEMOGRAPHICS
Among the 317 students taking 10th grade health class, 90% enrolled in the study (n=285). Due to scheduling conflicts, four regular health/waitlisted classes were unable to provide post-intervention data, yielding a sample of 202 students from nine classes for analysis. Demographic and baseline clinical information is reported for the original 285 students, with the students who completed postintervention measures designated as “included waitlist,” and those without, as “excluded waitlist” (see Table 2).
Table 2:
Participant demographic data, as reported by parent, for the 285 high school students in the stress reduction study.
| Total n=285 n (%) |
Mindfulness n=68 n (%) |
Wellness n=49 n (%) |
Included waitlist n=85 n (%) |
Excludeda waitlist n=83 n (%) |
|
|---|---|---|---|---|---|
| Female gender | 138 (48.4) | 35 (51.5) | 28 (57.1) | 37 (43.5) | 38 (45.8) |
| Mean age in years | 15.7 | 15.7 | 15.6 | 15.6 | 15.7 |
| Ethnicity | |||||
| Hispanic | 14 (4.9) | 2 (2.9) | 5 (10.2) | 4 (4.7) | 3 (3.6) |
| Non-Hispanic | 177 (63.2) | 41 (60.3) | 28 (57.1) | 61 (71.8) | 47 (56.6) |
| Other/did not specify | 94 (33.0) | 25 (36.8) | 16 (32.7) | 20 (23.6) | 33 (39.8) |
| Race | |||||
| American Indian/Alaska Native | 3 (1.1) | 0 (0.0) | 1 (2.0) | 1 (1.2) | 1 (1.2) |
| Asian/East Indian* | 25 (8.8) | 10 (14.7) | 1 (2.0) | 11 (12.9) | 3 (3.6) |
| Native Hawaiian/Pacific Islander | 3 (1.1) | 0 (0.0) | 1 (2.0) | 2 (2.4) | 0 (0.0) |
| Black/African-American | 8 (2.8) | 4 (5.9) | 3 (6.1) | 0 (0.0) | 1 (1.2) |
| White/Middle Eastern† | 134 (47.0) | 26 (38.2) | 22 (44.9) | 53 (62.4) | 33 (39.8) |
| Other/did not specify | 82 (29.3) | 27 (39.8) | 17 (34.7) | 23 (27.0) | 15 (18.1) |
| Diagnoses | |||||
| Autism | 1 (0.4) | 0 (0.0) | 0 (0.0) | 1 (1.2) | 0 (0) |
| Anxiety | 11 (3.9) | 3 (1.5) | 1 (0.5) | 4 (2.0) | 3 (1.5) |
| Depression | 2 (0.7) | 0 (0.0) | 1 (2.0) | 1 (1.2) | 0 (0.0) |
| Medications | |||||
| Stimulant medication | 5 (1.8) | 1 (2.0) | 1 (2.0) | 1 (2.0) | 2 (2.4) |
| Non-stimulant ADHD medication | 2 (0.7) | 0 (0.0) | 1 (2.0) | 1 (2.0) | 0 (0.0) |
| Antidepressants | 1 (0.4) | 0 (0.0) | 0 (0.0) | 1 (2.0) | 0 (0.0) |
Four classes without post-treatment measures.
P<0.05 for difference between wellness and mindfulness, included waitlist.
P<0.05 for difference between mindfulness and included waitlist.
Demographically, the sample comprised high socioeconomic status families: among the 153 participant families who provided income data, 86% reported an annual household income of over $100,000, with an average annual income between $130,000-$150,000.
Clinically, the intervention groups did not differ significantly from one another on any of baseline variables (all P-values >0.12). Overall, females tended to report higher baseline symptoms of anxiety and stress, as measured by the DASS subscales, compared to males (t(199)=−3.03, P<0.01 for anxiety, and t(199)=−3.55, P<0.01 for stress). However, post hoc analyses showed that the effect of the interventions on DASS scores did not differ by gender: P>0.16 for all gender × group interactions.
CLASS ATTENDANCE
One hundred percent (n=68) of the students assigned to the mindfulness intervention and 98% of the students assigned to the wellness intervention (n=48) attended all eight classes. While attendance was not formally tracked for students in the usual health class, teachers reported that these students had attendance rates comparable to the intervention groups.
AIM 1: ACCEPTABILITY
Credibility, Expectancy and Satisfaction
At baseline, students who were later randomized to the wellness intervention rated both interventions (mindfulness and wellness) higher in terms of perceived credibility and expectancy, relative to students who were later randomized to the mindfulness intervention (all P-values <0.03). There were no significant differences between the classes that received the same intervention, in terms of the students’ baseline rating of credibility for the interventions. See Table 3.
Table 3:
Baseline mean scores for the credibility and expectancy rating of the two interventions, prior to randomization, and for students’ satisfaction after receiving the intervention.
| Scales | Intervention received |
|||
|---|---|---|---|---|
| Mindfulness 3 classes (n=67) |
Wellness 2 classes (n=47) |
|||
| Pre-intervention |
Post-intervention |
Pre-intervention |
Post-intervention |
|
| Credibility and Expectancy Questionnaire (CEQ)a | ||||
| Credibility of mindfulnessa | 197.2 ± 44.7 | n/a | 215.5 ± 43.9 | n/a |
| Credibility of wellnessa | 189.0 ± 44.2 | n/a | 214.5 ± 49.4 | n/a |
| Expectancy of mindfulnessa | 169.5 ± 50.3 | n/a | 199.4 ± 52.4 | n/a |
| Expectancy of wellnessa | 161.3 ± 54.1 | n/a | 195.3 ± 51.3 | n/a |
| Client Satisfaction Questionnaire (CSQ)b | n/a | 22.0 ± 4.1** | n/a | 17.4 ± 4.6 |
Rated for both interventions prior to randomization.
Rated after study completion on the intervention received.
P<0.01 compared to wellness.
After the study, the students who received the mindfulness intervention reported a higher level of satisfaction than the students who received the wellness intervention, M=22 versus 17, t (97)=5.3, P<0.01 (two-tailed). However, the students’ increased satisfaction with the mindfulness intervention was not correlated with their baseline credibility rating, r=0.21, n=67, P=0.17; or expectancy of the intervention: r=−0.001, n=67, P=0.99.
In contrast, among students who received the wellness intervention, their expectancy for the wellness intervention at baseline was associated with their post-intervention satisfaction of wellness, showing a positive correlation with their baseline expectancy rating, r=0.42, n=47, P<0.001.
Adherence
In terms of mindfulness home practice, measured by students’ use of Headspace on their iPad devices, 52% (n=35) used the application at least once over the 8-week period. Of those, 20% used it 1–3 times; 70% used it 4–10 times and 10% used it 11+ times. Less than 10% of the students in the wellness classes reported viewing the assigned TED talks and YouTube videos for any length of time each night.
AIM 2: EFFECTIVENESS
Depression, Anxiety, and Stress
To test for effectiveness, we used regression models that controlled for pre-intervention values, and took into account classroom assignment; however, in Table 4 we present raw mean scores, pre- and post-intervention, in order to provide context for the outcomes.
Table 4:
Baseline and post-intervention mean scores for depression, anxiety, stress; and facets of mindfulness*
| Scales | Intervention received |
|||||
|---|---|---|---|---|---|---|
| Mindfulness 3 classes (n=67) |
Wellness 2 classes (n=47) |
Usual health elass/Waitlist 4 classes (n=85) |
||||
| Pre- intervention |
Post- intervention |
Pre- intervention |
Post- intervention |
Pre- Intervention |
Post- Intervention |
|
| Depression Anxiety and Stress Scale (DASS) | ||||||
| Depression scale | 4.0 ± 3.1 | 3.6 ± 3.3 | 4.3 ± 3.4 | 4.1 ± 3.6 | 5.2 ± 4.1 | 4.6 ± 4.1 |
| Anxiety scale | 3.8 ± 3.0 | 3.3 ± 3.0 | 4.7 ± 4.1 | 3.9 ± 3.8 | 4.3 ± 3.8 | 4.2 ± 3.8 |
| Stress scale | 6.1 ± 3.0 | 5.9 ± 3.8 | 7.3 ± 3.4 | 6.3 ± 3.8 | 6.4 ± 3.9 | 5.9 ± 3.1 |
| DASS total | 14.0 ± 7.6 | 12.7 ± 8.8 | 16.3 ± 9.6 | 14.4 ± 10.1 | 15.9 ± 10.6 | 14.7 ± 9.5 |
| Five Facet Mindfulness Questionnaire (FFMQ) | ||||||
| Observing | 23.2 ± 5.0 | 23.4 ± 6.5 | 23.6 ± 5.0 | 20.7 ± 6.9 | 23.0 ± 6.8 | 23.0 ± 6.9 |
| Acting with awareness | 25.9 ± 5.6 | 25.1 ± 5.2 | 26.1 ± 5.0 | 28.3 ± 6.3 | 26.3 ± 6.1 | 26.5 ± 6.7 |
| Non-reactivity | 19.9 ± 4.5 | 19.5 ± 4.6 | 19.6 ± 4.1 | 17.9 ± 5.5 | 19.0 ± 5.9 | 19.6 ± 5.8 |
| Non-judging | 28.8 ± 5.9 | 28.2 ± 6.9 | 28.8 ± 6.5 | 30.8 ± 7.5 | 29.3 ± 6.8 | 29.6 ± 6.5 |
A11 P-values >0.05.
Students in the mindfulness group reported fewer symptoms of anxiety, post-intervention, than students who received only their usual health curriculum/waitlist, controlling for the students’ baseline anxiety scores (α=−0.07, SE=0.03, P <0.01; 95% CI=−0.12, −0.02). This effect was above and beyond the influence of students’ baseline anxiety scores (β=0.67, SE=0.06, P≤0.001; 95% CI=0.55, 0.80), suggesting that students’ self-reported anxiety decreased more during the 8-week mindfulness intervention period than students’ anxiety in the usual health/waitlist classrooms. (See Figure 3.) While the students in the wellness group also reported a reduction in anxiety symptoms compared to the usual health/waitlist classes, there was no intervention effect; (P=0.50). The mindfulness groups’ scores were not significantly different compared with usual health/waitlist classrooms on depression, (β=−0.03, SE=0.07, P=0.61; 95% CI=−0.16, 0.10), or stress (β=0.05, SE=0.06, P=0.37; 95% CI=−0.06, 0.16). In fact, the students’ intervention group status was not associated with any of the other primary outcomes.
Figure 3:
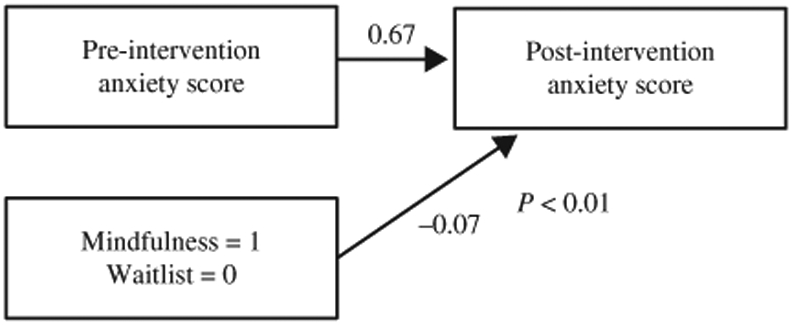
Impact of mindfulness on decrease in DASS anxiety scores after intervention compared usual health class/waitlist.
Level of Mindfulness
Among the FFMQ subscales, acting with awareness was higher in the wellness group after the study than the mindfulness group, after controlling for baseline scores (β=−0.22 P<0.01), but was not different between either group or the passive control/waitlist. See Table 4 for pre- and post-intervention mean scores.
DISCUSSION
This study examined the acceptability and effectiveness of a classroom-based mindfulness intervention among a group of largely affluent students attending a college-preparatory high school, compared to an active control intervention (wellness), or passive control (usual health class), for depression, anxiety and stress. Two key findings emerged in relation to mindfulness. First, while there were no differences between the two active interventions, after controlling for students’ baseline anxiety levels, students who received the mindfulness intervention reported reduced anxiety compared to students who received only their usual health class (passive control/waitlist). Although lower, the anxiety levels reported in the wellness classes were not significantly different from the levels reported in the usual health class/waitlist. Second, students who received mindfulness reported a higher level of satisfaction with their intervention than the students who received the wellness intervention.
Comparing mindfulness to usual health class provided a realistic comparison to judge the benefit of mindfulness in the context of classroom-based delivery. Although mindfulness did not outperform the wellness intervention on self-reported measures, the mindful skills that were at the least introduced, if not fully incorporated into the students’ lives, may positively influence the students, and are not typically taught in other curricula.
The reported reduction in anxiety symptoms among this largely non-clinical student population is supported by findings in adult clinical populations where mindfulness was also found to reduce anxiety symptoms, compared to waitlist in a 39-study meta-analysis,33 and in an RCT of adult patients with anxiety (n=76).12 Further, the reduction in post-intervention anxiety in both of the active conditions in this study, without group differences, mirrored findings from an RCT of mindfulness or hatha yoga in adolescents.34 The findings that depression and stress did not differ between the intervention groups may be related to a floor effect in that the student’s reported symptoms were low at baseline. Ninety-seven percent of students reported normal to mild symptoms of depression, 3% reported moderate levels; for stress 99% reported normal to mild levels, with 1% reporting moderate stress. In contrast, 10% of students reported moderate to severe levels of anxiety. Supporting these reports, 5% of the students had an anxiety disorder at baseline, according to parent reports, underscoring the finding that anxiety was the one area where enough students reported sufficient symptoms to notice a change after the study. Examining the possible benefit of mindfulness in high school students who have mental health symptoms at baseline, lower socioeconomic status, or have been affected by trauma, may produce other results.
The students who received mindfulness reported higher satisfaction after receiving the intervention for the 8 weeks compared to the students who received wellness. Among students who received wellness, satisfaction with the intervention was influenced by their expectations of the intervention prior to receiving it. In contrast, even after controlling for the expectancy and credibility ratings prior to randomization, students rated the mindfulness intervention as significantly more satisfying postinvention compared to the students who received the wellness intervention. These results suggest that students’ satisfaction with mindfulness withstood their preconceived ideas about the intervention, while students’ satisfaction with wellness was positively correlated with their baseline expectations.
Another important finding was the adolescents’ limited home practice. Only 52% used it once; 10% (n=6) of students used the app to practice mindfulness at a frequency that approached the expectation of using it daily. Despite efforts to make the guided mindful practice readily accessible to students by asking them to download it on to their iPads, app usage was limited. When asked, students’ top three reasons for not using the app were, (1) being too busy, (2) getting home too late, and (3) having too much homework, suggesting that the students’ academic and extracurricular activities may have created time barriers to practicing mindfulness at home. Several students suggested that app usage would have occurred more frequently if they had been graded on its use. Similarly, students in the wellness intervention did not watch the assigned videos at home. Other researchers have found that outside practice is limited in adolescent samples, and that the amount of outside practice impacts study outcomes, notably,15 found an association between the amount of home practice and level of well-being. Interestingly, in this study, students reported reduced anxiety from mindfulness without home practice.
A standardized “dose” of mindfulness has not been established, but many studies follow an eight-session 90-minute format with the expectation of 30+ minutes daily home practice.11 School day time constraints meant this duration was not possible, and may be unrealistic for many high school students. In hindsight, students’ at-home practice might increase if they were encouraged to practice informally (e.g. doing regular activities mindfully) or be more evident if asked to record observations of their internal processes, an idea used by others.34,35 Anecdotally, a number of students in this study volunteered that the mindfulness practice helped them cope with stress—in preparing for a test, a play performance, or sporting event—but these effects were not evident quantitatively. Similarly, the students who received the wellness intervention reported enjoying the intervention, but did not specifically report stress reduction benefits. A qualitative assessment of the interventions’ effects may capture these data.
One of the FFMQ subscales, acting with awareness, was different between the two active intervention groups, but not the waitlist. Among students who received wellness, higher levels of acting with awareness were reported compared to those who received mindfulness. This increase may be related to the topics and skills taught as part of the wellness intervention (e.g. sleep hygiene, time management, and power postures for self-confidence), which encouraged premeditated, planned behavior, resulting in noticeable differences to the students themselves. For example, the sleep hygiene curriculum included the importance of a creating a dark bedroom for sleep. Among students who actively took steps to darken their bedroom (e.g. covering up computer monitor lights), several reported a qualitative improvement in their ability to go to sleep, an example of acting with awareness.
STUDY LIMITATIONS AND STRENGTHS
The characteristics of the students who participated in this study may be distinct from other high school populations and these student features may have impacted intervention home practice. The school’s college-preparatory curriculum may attract students with high achievement standards, not just academically, but also in sports and other extracurricular activities. The students’ busy schedules impacted the time available for home practice, and in the absence of being graded, mindfulness practice was not prioritized over other homework. The school’s Jesuit foundation, evident throughout its culture and daily activities, may bias the students, positively or negatively, to the concept of a contemplative practice such as mindfulness. Finally, many students came from affluent families with more than 85% of parents reporting an annual household income of over $100,000. The specific features of this student population may limit the generalizability of the study findings. Another limitation is the validity of using the same intervention provider for both the mindfulness and wellness interventions. Although specific class plans were created in advance, and adhered to during the sessions, the lack of a third party fidelity rating is a limitation.
This study builds upon the current literature by enrolling a large number of students and using a three-arm design to compare mindfulness to an active and a passive control. Previous studies showing the benefit of mindfulness in child and adolescent populations enrolled fewer participants,36,37 and lacked a comparison to an active control.38 In terms of limitations, students were not blind to the intervention they received, however, the expectation that one intervention or the other was “superior” or active was mitigated by emphasizing that “stress reduction” was the study focus. Fidelity to the intervention is another possible limitation. Although a fidelity measure denoting specific components for each session was created for both interventions, the third-party rater attended only the first few sessions due to limited co-facilitator support. The larger classroom format may have been a limiting factor. With an average of 21 students per class, mindfulness may have seemed like a school subject or technique to learn, rather than a personal practice to develop, a distinction that results in different outcomes.39 Finally, some research suggests preference for online or individual mindfulness training rather than group delivery.40,41
CLINICAL CONSIDERATIONS
Even with limited practice at home, mindfulness demonstrated benefit for self-reported symptoms of anxiety, when compared to usual health class. Clinicians may consider referring adolescents to school- or community-based mindfulness programs for anxiety.
CONCLUSIONS
Two encouraging conclusions may be drawn from this study. First, despite limited practice outside of the classroom, students who received the mindfulness intervention in class reported fewer symptoms of anxiety at the end of the 8 weeks compared to students who received only their usual health class. Second, students’ satisfaction with mindfulness withstood expectancy effects meaning that their expectations of mindfulness, before they received the intervention, did not influence their reported satisfaction at the end of the intervention. Delivering a mindfulness intervention in the group context of a high school class was feasible and acceptable, suggesting that adding mindfulness to an already existing curriculum of health may be of value in reducing anxiety, even with limited home practice. Novel ways to encourage students to practice outside the classroom are needed for future studies.
ACKNOWLEDGMENTS AND FUNDING
The authors wish to thank the students, parents and staff of Jesuit High School for their participation, and to the administration for allowing the study to be conducted on campus. For assistance with study implementation, many thanks to Ashlie Mole, Bethany Sutro, Ifrah Sheik, Lodi Rice, and Hayden Forster; to Zayne Vacheresse, Andrew Bontemps, Julia Fonk, and Libby Nousen for REDCap database creation and maintenance; to Jessica Tipsord, PhD and Doug Hanes, PhD for statistical consultation.
This research was funded by the National Institutes of Health (NIH) NCCIH T32 AT002688 (Johnstone); as well as through support from the Division of Child and Adolescent Psychiatry, Oregon Health & Science University and Oregon Clinical & Translational Research, through the NIH’s National Center for Advancing Translational Sciences, UL1TR000128. Dr. Johnstone’s time completing the manuscript was funded by NIH-NCCIH 5R90AT00892403. Dr. Nigg’s time was funded by NIH R37MH59105.
Footnotes
COMPETING INTERESTS
The authors report no competing interests.
REFERENCES
- 1.Andersen SL, Teicher MH. Stress, sensitive periods and maturational events in adolescent depression. Trends Neurosci. 2008;31(4):183–91. [DOI] [PubMed] [Google Scholar]
- 2.Chandra A, Batada A. Exploring stress and coping among urban African American adolescents: the Shifting the Lens Study. Prev Chronic Dis. 2006;3(2):A40. [PMC free article] [PubMed] [Google Scholar]
- 3.O’Keeffe GS, Clarke-Pearson K. The impact of social media on children, adolescents, and families. Pediatrics. 2011;127(4):800–4. [DOI] [PubMed] [Google Scholar]
- 4.American Psychological Association. Stress in America 2014. Available from: http://www.apa.org/news/press/releases/2014/02/teen-stress.aspx.
- 5.Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci. 2009;10(6):434–45. [DOI] [PubMed] [Google Scholar]
- 6.LaRue DE, Herrman JW. Adolescent stress through the eyes of high-risk teens. Pediatr Nurs. 2008;34(5):375. [PubMed] [Google Scholar]
- 7.Cartwright M, Wardle J, Steggles N, Simon AE, Croker H, Jarvis MJ. Stress and dietary practices in adolescents. Health Psychol. 2003;22(4):362. [DOI] [PubMed] [Google Scholar]
- 8.Finkelstein DM, Kubzansky LD, Goodman E. Social status, stress, and adolescent smoking. J Adolesc Health. 2006;39(5):678–85. [DOI] [PubMed] [Google Scholar]
- 9.Gould MS, Greenberg T, Velting DM, Shaffer D. Youth suicide risk and preventive interventions: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2003;42(4):386–405. [DOI] [PubMed] [Google Scholar]
- 10.Kendall PC, Peterman JS. CBT for adolescents with anxiety: mature yet still developing. Am J Psychiatry. 2015;172(6):519–30. [DOI] [PubMed] [Google Scholar]
- 11.Kabat-Zinn J, Hanh TN. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. New York: Random House Publishing Group; 2009. [Google Scholar]
- 12.Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. J Consult Clin Psychol. 2010;78(2):169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.de Vibe M, Bjørndal A, Fattah S, Dyrdal GM, Halland E, Tanner-Smith EE. Mindfulness-based stress reduction (MBSR) for improving health, quality of life and social functioning in adults: a systematic review and metaanalysis. Campbell Syst Rev. 2017;13(1):1–264. [Google Scholar]
- 14.Black DS, Fernando R. Mindfulness training and classroom behavior among lower-income and ethnic minority elementary school children. J Child Fam Stud. 2014;23(7):1242–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huppert FA, Johnson DM. A controlled trial of mindfulness training in schools; the importance of practice for an impact on well-being. J Posit Psychol. 2010;5(4):264–74. [Google Scholar]
- 16.Metz SM, Frank JL, Reibel D, Cantrell T, Sanders R, Broderick PC. The effectiveness of the learning to BREATHE program on adolescent emotion regulation. Res Hum Dev. 2013;10(3):252–72. [Google Scholar]
- 17.Zylowska L, Ackerman DL, Yang MH, Futrell JL, Hale TS, Pataki C, et al. Mindfulness meditation training in adults and adolescents with ADHD. J Attent Disord. 2008;11(6):737–46. [DOI] [PubMed] [Google Scholar]
- 18.Britton WB, Bootzin RR, Cousins JC, Hasler BP, Peck T, Shapiro SL. The contribution of mindfulness practice to a multicomponent behavioral sleep intervention following substance abuse treatment in adolescents: a treatment-development study. Substance Abuse. 2010;31(2):86–97. [DOI] [PubMed] [Google Scholar]
- 19.Meiklejohn J, Phillips C, Freedman ML, Griffin ML, Biegel G, Roach A, et al. Integrating mindfulness training into K-12 education: fostering the resilience of teachers and students. Mindfulness. 2012;3(4):291–307. [Google Scholar]
- 20.Johnstone JM, Roake C, Sheikh I, Mole A, Nigg JT, Oken B. School-based mindfulness intervention for stress reduction in adolescents: design and methodology of an open-label, parallel group, randomized controlled trial. Contemp Clin Trials Commun. 2016;4:99–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hayes SC, Strosahl KD, Wilson KG. Acceptance and Commitment Therapy: the Process and Practice of Mindful Change. New York, NY: Guilford Press; 2011. [Google Scholar]
- 23.Ciarrochi J, Hayes L, Bailey A. Get Out of Your Mind & Into Your Life for Teens. Oakland, CA: New Harbinger Publications; 2012. [Google Scholar]
- 24.The Hawn Foundation. The MindUP Curriculum: Grades 6–8: Brain-Focused Strategies for Learning—and Living, 1st edn. Scholastic Teaching Resources; 2011. [Google Scholar]
- 25.Covey S. The 7 Habits of Highly Effective Teens: The Ultimate Teenage Success Guide. New York: Touchstone; 2014. [Google Scholar]
- 26.Oregon Department of Education. Oregon Health Education Standards and Performance Indicators, K-12 2016. Available from: https://www.oregon.gov/ode/educator-resources/standards/health/Pages/default.aspx.
- 27.Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. J Behav Ther Exp Psychiatry. 2000;31(2):73–86. [DOI] [PubMed] [Google Scholar]
- 28.Attkisson CC, Zwick R. The client satisfaction questionnaire: psychometric properties and correlations with service utilization and psychotherapy outcome. Eval Program Plan. 1982;5(3):233–7. [DOI] [PubMed] [Google Scholar]
- 29.Henry JD, Crawford JR. The short-form version of the Depression Anxiety Stress Scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br J Clin Psychol. 2005;44(2):227–39. [DOI] [PubMed] [Google Scholar]
- 30.Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. [DOI] [PubMed] [Google Scholar]
- 31.Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, et al. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008;15(3):329–42. [DOI] [PubMed] [Google Scholar]
- 32.Bohlmeijer E, ten Klooster PM, Fledderus M, Veehof M, Baer R. Psychometric properties of the five facet mindfulness questionnaire in depressed adults and development of a short form. Assessment. 2011;18(3):308–20. [DOI] [PubMed] [Google Scholar]
- 33.Vollestad J, Sivertsen B, Hostmark Nielsen G. Mindfulness-based stress reduction for patients with anxiety disorders: evaluation in a randomized controlled trial. Behav Res Ther. 2011;49:281–8. [DOI] [PubMed] [Google Scholar]
- 34.Quach D, Mano KEJ, Alexander K. A randomized controlled trial examining the effect of mindfulness meditation on working memory capacity in adolescents. J Adolesc Health. 2016;58(5):489–96. [DOI] [PubMed] [Google Scholar]
- 35.Finkelstein-Fox L, Park CL, Riley KE. Mindfulness and emotion regulation: promoting well-being during the transition to college. Anxiety Stress Coping. 2018;31(6):639–53. [DOI] [PubMed] [Google Scholar]
- 36.Britton WB, Lepp NE, Niles HF, Rocha T, Fisher NE, Gold JS. A randomized controlled pilot trial of classroom-based mindfulness meditation compared to an active control condition in sixth-grade children. J School Psychol. 2014;52(3):263–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Broderick PC, Metz S. Learning to BREATHE: a pilot trial of a mindfulness curriculum for adolescents. Adv School Mental Health Promot. 2009;2(1):35–46. [Google Scholar]
- 38.MacCoon DG, Imel ZE, Rosenkranz MA, Sheftel JG, Weng HY, Sullivan JC, et al. The validation of an active control intervention for Mindfulness Based Stress Reduction (MBSR). Behav Res Ther. 2012;50(1):3–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Melbourne Academic Mindfulness Interest Group. Mindfulness-based psychotherapies: a review of conceptual foundations, empirical evidence and practical considerations. Aust N Z J Psychiatry. 2006;40(4):285–94. [DOI] [PubMed] [Google Scholar]
- 40.Wahbeh H, Lane JB, Goodrich E, Miller M, Oken BS. One-on-one mindfulness meditation trainings in a research setting. Mindfulness. 2014;5(1):88–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wahbeh H, Goodrich E, Oken BS. Internet mindfulness meditation for cognition and mood in older adults: a pilot study. Altern Ther Health Med. 2016;22(2):46–55. [PMC free article] [PubMed] [Google Scholar]
- 42.Covey SR, Merrill AR, Merrill RR. First Things First. New York: Fireside; 1995. [Google Scholar]