Abstract
Coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory coronavirus 2 (SARS-COV-2) is a significant threat to global health security. Till date, no completely effective drug or vaccine is available to cure COVID-19. Therefore, an effective vaccine against SARS-COV-2 is crucially needed. This study was conducted to design an effective multiepitope based vaccine (MEV) against SARS-COV-2. Seven highly antigenic proteins of SARS-COV-2 were selected as targets and different epitopes (B-cell and T-cell) were predicted. Highly antigenic and overlapping epitopes were shortlisted. Selected epitopes indicated significant interactions with the HLA-binding alleles and 99.93% coverage of the world’s population. Hence, 505 amino acids long MEV was designed by connecting 16 MHC class I and eleven MHC class II epitopes with suitable linkers and adjuvant. MEV construct was non-allergenic, antigenic, stable and flexible. Furthermore, molecular docking followed by molecular dynamics (MD) simulation analyses, demonstrated a stable and strong binding affinity of MEV with human pathogenic toll-like receptors (TLR), TLR3 and TLR8. Finally, MEV codons were optimized for its in silico cloning into Escherichia coli K-12 system, to ensure its increased expression. Designed MEV in present study could be a potential candidate for further vaccine production process against COVID-19. However, to ensure its safety and immunogenic profile, the proposed MEV needs to be experimentally validated.
Introduction
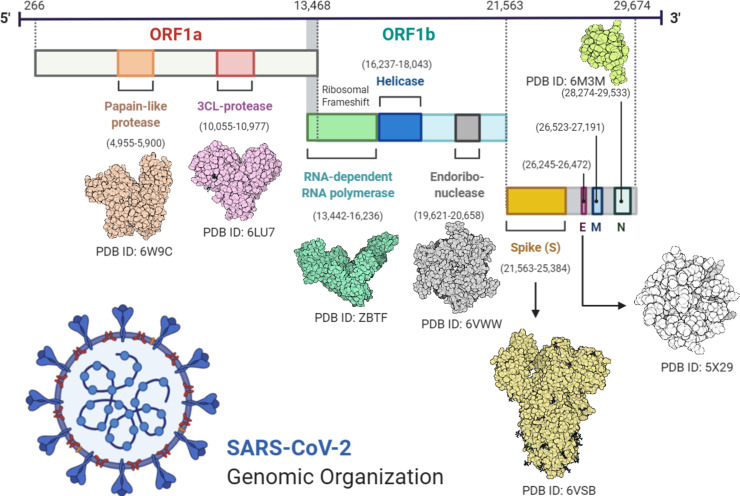
Viruses are dangerous pathogens and can cause irreversible losses to human lives and economy. The world hardly learns to deal with a virus when new emerges and threatens the future of humanity [1]. A similar situation arises when a new strain of coronavirus (CoV) not previously identified in humans was reported last year (2019). Positive-sense RNA viruses called corona viruses belong to the Coronaviridae family that are distributed broadly among human and mammals. In the last two decades there have been more than 10,000 reported infections of two types of coronaviruses: severe acute respiratory coronavirus (SARS-COV) or Middle East Coronavirus (MERS-COV) [2]. Last year December (2019), few cases of unknown viral based pneumonia were reported. Later it was identified that, this pneumonia is linked with a novel type of CoV outbreak. World Health Organization (WHO) named the virus SARS-CoV-2 and linked disease as coronavirus disease 2019 (COVID-19). The COVID-19 widespread around the globe and claimed thousands of human lives. WHO announced global health emergency and recognized COVID-19 as pandemic [3–5]. SARS-CoV-2 was indicated root cause of COVID-19 through deep sequencing analysis from lower respiratory tract samples of patients [6]. SARS-COV-2 genome sequence is almost 70% similar to SARS-COV, and 40% similar to the MERS-COV [7]. Symptoms of SARS-COV-2 may arise within 2 days or up-to 14 days of exposure. Symptoms such as fever, diarrhea and respiratory disorder are found in infected patients [4]. According to latest research SARS-CoV-2 has an identical genomic organization as of beta-coronaviruses (Fig 1); 5’-untranslated region (UTR), orf1ab (replicas complex), nsps (encoding non-structural proteins), S (spike) protein, E (envelope) protein, M (membrane) protein, Oraf6, orf7a, orf8, N (nucleocapsid) protein, orf10, 3’-UTR and several unknown non-structural open reading frames [3,8].
Fig 1. Diagram representing the genomic organization of SARS-CoV-2.
Figure was created using BioRender (https://biorender.com/).
There is currently no approved vaccine or drug treatment for COVID-19. Few traditional Chinese medicine such as Shufengjiedu capsules and Lianhuaqingwen capsules were reported effective against COVID-19 [9,10]. Nonetheless, no clinical trials support the safety and efficacy of these medicinal products. Similarly, clinical trials are in process for few experimental drugs, including remdesivir and chloroquine which were found effective in vitro against COVID-19 [11]. Few candidate vaccines are also in their final trials for COVID-19 [12]. However, there is no clinical trial-based drug or completely effective vaccine reported yet. To prevent viral diseases, vaccine is the most effective approach. Now a days, availability of genomic information, advance software and immunological data sets could greatly facilitate researchers to identify the effective epitopes from pathogens’ proteins that can be used to develop active sub-unit vaccines [13–16]. The subunit vaccine contains the fragments of antigenic proteins of pathogen that can trigger an immune response against the target pathogen [17,18]. In recent studies, candidate vaccine constructs were reported against different viruses including: MERS-CoV [19], RSV [20], Chikungunya virus [21], Ebola virus [22], Zika virus [23], HCV [24], Flavivirus [25], Cytomegalovirus [26], HIV [27], BK virus [28] and Norovirus [29] with promising results. The in silico methods reduce the number of in vitro experiments and save time, overcome cost obstacles and increase the potential for successful vaccine design [30–32].
In present study, SARS-CoV-2 proteome was explored to determine the potent antigenic proteins and their further screening for B-cell and T-cell epitopes prediction with their MHC (major histocompatibility complex) alleles. Antigenicity, conserveness and global coverage of predicted epitopes were analyzed. Multiepitope based vaccine (MEV) construct was designed by using the most potential and interacting epitopes, with the addition of suitable linkers and an adjuvant. MEVs are more advantageous in comparison with single-epitope vaccines or conventional vaccines, due to their cost effective, time saving, stability and specificity properties. Additionally, they are believed to induce significant humoral and cellular immune responses, simultaneously because of the presence of T-cell as well as B-cell epitopes [33,34]. As MEVs consist of adjuvants, they believed to developed long-lasting immune responses and increased immunogenicity. Adjuvants are generally defined as molecules that may increase or modulate the intrinsic immunogenicity of an antigen [35]. Adjuvants are essential to reduce the amount of antigen and the number of injections, as they help to induce effective and persistent immune responses [36]. Several in silico approaches were utilized to validate the antigenicity, immunogenicity, allergenicity, toxicity, structural stability/flexibility and physiochemical properties of designed MEV. Furthermore, molecular docking and MD simulations analyses were carried out to investigate binding interaction and stability of the MEV with human pathogenic receptors. At the end, the MEV codons were optimized for E. coli system and in silico cloning was performed to ensure its expression profiling.
Material and methods
Sequence retrieval and analysis of antigenic proteins
In the first step, whole proteome of SARS-CoV-2 was retrieved from GENBANK [37]. After that, individual protein sequences were extracted and stored as FASTA format for further analysis.
Antigenicity and physiochemical properties evaluation
The Expassy Protparam tool was used to determine the physical and chemical properties of selected proteins [38]. To check protein antigenicity, the Vaxijen 2.0 software was used [39]. The threshold value was held at 0.5, and the secondary structure of proteins was predicted by using SOPMA tool [40].
Tertiary structure prediction and refinement of target proteins
Tertiary structures of most of SARS-CoV-2 proteins are not reported yet. Therefore, combinations of different approaches were employed to predict good quality structures for further analysis. Online tools such as Swiss model which work on homology based modeling algorithms and Raptor X which work on deep learning modules, were primarily used for the tertiary structure prediction of SARS-COV-2 proteins [41–43]. Predicted Models were then refined by galaxy refine server and validated by Ramachandran plot analysis.
Epitopes prediction and validation
B-cell epitope prediction
In immune system the B-Cell epitope helps to detect viral infection and activities. B-cells provide humoral immunity by secreting immunoglobulins which can neutralize antigen upon binding. A surface receptor of B-cell recognizes B-cell epitopes, resulting the generation of antigen-specific immunoglobulins [44]. B-cell epitopes are two types, linear (continuous) and conformational (discontinuous). An online database of ABCPred was used to predict linear B-cell epitopes [45,46]. Conformational epitopes were predicted by Ellipro server [47].
T-cell Epitope prediction
T-cells express TCRs (T-cell receptors), that could recognize specific antigens and can generate cellular and humoral immune response against them [48]. The Immune Epitope Database (IEDB) consensus method [49,50] was used to predict MHC classes I and MHC II epitopes with consensus score less than 2 filter cut.
Immunogenicity prediction of epitopes
To evaluate the antigenicity of B-cell and T-cell epitope, Vaxijen v2.0 was used. The filtering criteria 0.5 was used. Only filtered highly antigenic epitopes were selected for further studies.
Conservation analysis of epitopes
IEDB conservancy analysis tool [51] was used, to monitor the degree of conservation in the sequence of B-cell and T-cell epitopes. Epitopes showing 100 percent conservation were shortlisted for further analysis.
Interferon-γ inducing epitopes prediction
IFN-γ is acknowledged to elicit intrinsic safe responses and can directly detain viral duplication [52,53]. Besides, they can trigger the versatile immune reactions by preparing cytotoxic T lymphocyte (CTL) and Helper T lymphocyte (HTL). IFN epitope server was used to calculate the IFN-γ inducing potential of selected epitopes using SVM hybrid algorithms along with Motif [34].
Epitopes modeling and molecular docking
Epitopes which show favorable strong binding affinities with a common experimentally validated allele, are good choice to design MEV construct. Therefore, molecular docking between screened epitopes and human allele was performed. Molecular docking is an in silico approach which determined the binding affinity between ligand and its target proteins, and also highlight the important residues involve in the interaction [54]. 3D structures of overlapping, highly antigenic and conserved epitopes with corresponding common alleles were predicted using PEPFOLD [55]. The X-ray crystallographic structure of a common human allele (HLA-B7) was retrieved from protein data bank (PDB ID: 3VCL). Molecular docking was performed using same protocol of our previously published studies [19–21,34]. To visualize the docked complexes and draw figures, the PyMOL educational version was used [56].
Population coverage analysis of selected epitopes
The selected epitopes for MEV construct should effectively cover major populations across the globe. For population coverage, overlapping, antigenic, conserved and strongly interacting with their corresponding HLA-binding alleles (MHC class-I and II), epitopes were selected and further analyzed combine using the IEDB population coverage analysis tool by maintaining the default analysis parameters [51]. This tool is designed to estimate the population coverage of epitopes from diverse countries based on the distribution of their MHC-binding alleles. As SARS-CoV-2 is global pandemic, therefore, worldwide analysis has been performed.
Construction of multi epitope vaccine
To construct a sub-unit vaccine, the epitopes with following properties are usually preferred: (i) highly antigenic, (ii) 100% conserved, (iii) overlapping, (iv) with significant population coverage, (v) having strong binding affinity with common human allele and (vi) have no similarity with the human proteins. Therefore, only those epitopes were further selected that passed all the six above parameters to construct SARS-CoV-2 MEV. To boost the immune response an adjuvant was attached with the first CTL epitope with the EAAAK linker, while other epitopes were connected using AAY and GPGPG linkers to preserve their independent immunogenic activities after their inter-interaction compatibility validation.
Immunogenic and physicochemical properties evaluation of the vaccine construct
The vaccine construct should be stable, highly antigenic, non-allergic and non-toxic. The ProtParam tool [57] was used to evaluate the physicochemical properties of MEV. It analyzes different physical and chemical features of proteins including grand average hydropathy, half-life, stability/instability index, theoretical pI and aliphatic index hydropathy. The MEV properties were further verified using VaxiJen 2.0 and AllerTOP V2.0 servers [58]. Moreover, PSIPRED was used to analyzed the secondary structure of MEV [59].
Tertiary structure prediction of vaccine construct
As vaccine construct is combination of different epitopes, therefore, the RaptorX server was used to develop good quality MEV 3D tertiary structure [41].
Refinement and validation of vaccine construct
Galaxy Refine server MD simulation approach was used to refine the MEV predicted 3D structure [60]. To verify refined MEV structure quality, Ramachandran plot analysis was performed using RAMPAGE server [61], followed by structural validation analysis using ProSA-web server [62]. The quality scores outside the normal range of natural proteins during structure validation process reveal potential defects in the protein structure model. Therefore, ERRAT server was further used to evaluate the statistics of non-bonded interactions in MEV construct [63]. Furthermore, MEV structural flexibility was also analyzed using CABS-Flex 2.0 server [64]. The flexibility of vaccine is an important aspect for its functionating, and CABS-Flex server provides a detail overview of flexibility and stability of query protein by simulating its residues [65].
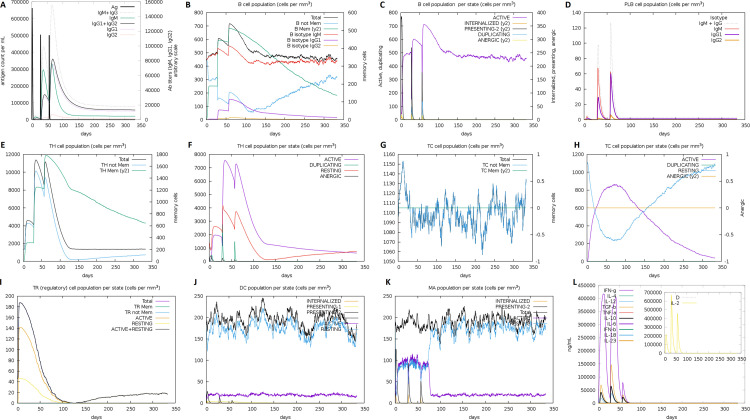
Immunogenicity evaluation of the vaccine construct
An in silico immune simulation was performed using C-ImmSim 10.1 server [66], in order to validate immunological response of constructed MEV. This server simulates the three major functional mammal system components (bone marrow, thymus and lymph node) [66]. The MEV has been tested for the ability to simulate various types of immune cells such as HTL, CTL, B-cells, NK cells, dendritic cells, Immunoglobulins and cytokines. Clinically the minimum recommended interval between two doses of vaccines is four weeks [26,48,67,68]. Consequently, three injections (each injection contain a thousand units of MEV) were administered using C-ImmSim immunostimulatory, with the recommended interval of four weeks (1, 84 and 168 time-steps parameters were set as 1 time-step is equal to eight hours of real life) for a total of 1000 steps of simulation. Other parameters were kept as default.
Molecular docking of vaccine construct with human immune receptor
The host produces an efficient immune response if an antigen / vaccine interacts properly with the target immune cells. Therefore, molecular docking analysis was performed to analyze integrations between the MEV and the human immune receptors. TLR3 and TLR8 have been extensively studied and researchers found their vital roles in the generation of antiviral immune response. HADDOCK was used for the MEV docking with TLR3 (PDB ID: 1ZIW) and TLR8 (PDB ID: 3W3G). To visualize the docked complex and draw figures, the PyMOL educational version was used [56]. In addition, the online database PDBsum was used to demonstrate the interacting residues of docked complexes [69].
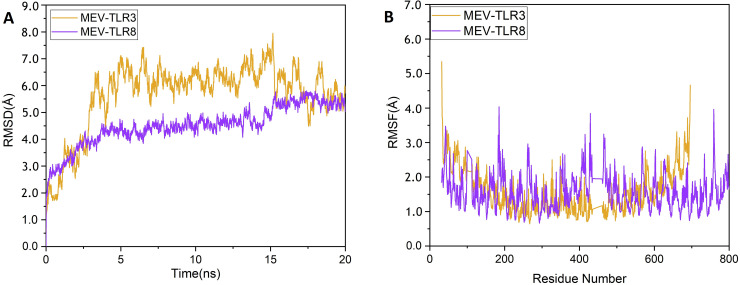
Molecular dynamics simulation analysis of vaccine construct and receptors complexes
MD simulation is an important approach to analyse the stability of the receptor-ligand complex [48,70]. Complexes of MEV with TLR3 and TLR8 were simulated at 20 ns using GROMACS 5.1.4 [71] by following the same protocol of our previously published studies [5,7,20,72,73]. The trajectories were saved for each complex after every 2 fs and root mean square deviation (RMSD) and root mean square fluctuations (RMSF) analysis were performed using GROMCAS tools. MM/PBSA has been extensively used to estimate binding free energies of protein-ligand systems [20,33]. Therefore, using the MMPBSA module, the binding free energies of the docked receptor-vaccine complexes were calculated. The binding free energy calculation was done on 100 frames extracted from complete length of MD simulation. Total energy of binding for both the complexes was calculated using equation given below:
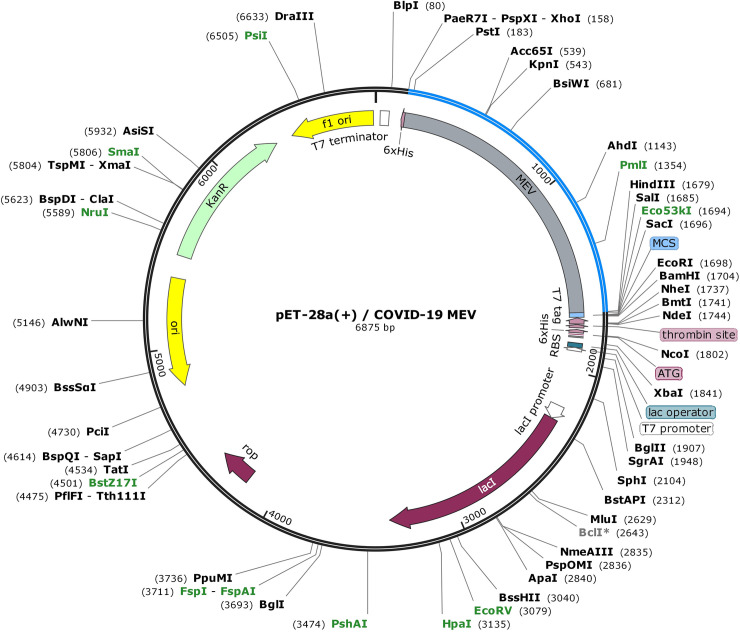
Codon optimization and in silico cloning
Codon adaptation is a way of increasing the translation efficacy of external genes in the host if the use of codon in both species varies. After carefully evaluating MEV properties and immune response, its codon optimization was performed followed by in silico cloning. The Java Codon Adaptation Tool (JCAT) server [74] was used for codon optimization of MEV to make it compatible with widely used prokaryotic expression system; E. coli K12 [75]. The available additional options were selected to evade (a) rho-independent transcription termination, (b) prokaryote ribosome binding site and (c) restriction enzymes cleavage sites. The GC (guanine and cytosine) contents together with codon adaptation index (CAI) [76] were evaluated. Furthermore, to facilitate restriction and cloning, sticky ends restriction sites of XhoI and HindIII restriction enzymes were introduced at the start/N-terminal and end/C-terminal of the optimized MEV sequence, respectively. Finally, the adapted nucleotide sequence of MEV was cloned into the E. Coli pET28a(+) vector with SnapGene 4.2 tool (https:/snapgene.com/) to ensure the in vitro expression.
Results
Target proteins sequence and structural analysis
The amino acid sequences of SARS-CoV-2 important vaccine target proteins (ORF1 [QHD43415.1], S [QHD43416.1], ORF3a [QHD43417.1], E [QHD43418.1], M [QHD43419.1], ORF6 [QHD43420.1], ORF7a [QHD443421.1], ORF8 [QHD43422.1], N [QHD43423.2] and ORF10 [QHI42199.1]) were evaluated for the antigenicity screening using Vaxijen server. Total 7 highly antigenic proteins were detected. The most antigenic protein found was ORF10, followed by E, M, ORF6, ORF7a, ORF8, and N, with antigenic values 0.7185, 0.6502, 0.6441, 0.6131, 0.6025, 0.5102 and 0.5059 respectively. ORF1, S, and ORF3 proteins had antigenic values less than 0.5, therefore they were excluded from further analysis. Among selected 7 highly antigenic SARS-CoV-2 proteins for further analysis, 5 were non-structural proteins (M, N, ORF6, ORF7a, and ORF10) and 2 were structural proteins (E, ORF8). Other physicochemical characteristics of selected proteins including theoretical pI, molecular weight, half-life, stability profile, aliphatic index, etc were analyzed using ProtParam server (S1 Table) and their secondary structures was predicted using SOPMA tool (S2 Table).
The 3D structures of E and N proteins were downloaded from protein data bank (PDB), using PDB IDs 5X29 and 6M3M, respectively. While, 3D models of other selected proteins tertiary structures were predicted using Swiss model tool and Raptor X tool, and in order to select best quality models, predicted structures were further refined by galaxy refine server followed by Ramachandran plot validation. The most of structures predicted using Swiss model were of better quality than Raptor X predicted structures, except for Orf7a protein. There was no suitable structure predicted for ORF10 because of small number of residues. So, its structure was predicted by PEPFOLD server [55] (S3 Table).
Prediction of B-cell and T-cell epitopes
Screened out B-cell epitopes were 100% conserved in all protein sequences and were highly antigenic. All the target proteins were predicted to have a total 55 linear epitopes (E-4, M-12, ORF6-1, ORF7a- 6, ORF8-9, N- 22, and ORF10-1). Moreover, a total of 24 (E-4, M-2, ORF6-3, ORF7a- 4, ORF8-4, NC- 4, and ORF10-3) conformational epitopes were predicted in all target proteins.
As mentioned before, epitopes that can bind to multiple alleles because of their strong defense capabilities are considered the most appropriate epitopes. Therefore, total 31 MHC class I (E-9, M-4, ORF6-2, ORF7a-3, ORF8-7, N-4, ORF10-2) and 40 MHC class II (E-4, M-5, ORF6-4, ORF7a-7, ORF8-12, N-4, ORF10-4) epitopes, 100% conserved among target protein sequences and highly antigenic were chosen for further study.
The HTLs helps to activate CTLs together with other immune cells upon various types of cytokines release i.e., IFN-γ, interleukin-4 and interleukin-10 [18,77]. Thus, HTL epitopes that induce cytokines are vital for the progress of vaccines or immunotherapy. A total of 178 IFN-γ inducing epitopes from target proteins (E-8, M-39, ORF6-4, ORF7a-8, ORF8-28, N-82, ORF10-9) were obtained.
Interaction analysis of epitopes with HLA-B7 allele
As stated before, to construct a sub-unit vaccine, the chosen epitopes should be 100% conserved, overlapping and antigenic. Therefore, total 50 conserved/antigenic/overlapping epitopes from selected proteins were selected for subsequent validation of their interactions with a common human allele. The 3D structures of selected epitopes were predicted using PEPFOLD. The binding patterns of selected epitopes with a common conserved allele HLA-B7 were analyzed through molecular docking and it was found that only 27 epitopes bind deep inside in the HLA-B7 binding pocket (S1 and S2 Figs). Each bound epitope to HLA-B7 depict stronger than -10.00 Kcal/mol docking affinity. Docking binding energy scores together with their detail information is mentioned in Table 1. All the 27 selected epitopes ensured their binding efficiency as well as their suitability to be used in multiple epitope-based vaccine construct.
Table 1. Final selected epitopes from SARS-CoV-2 antigenic proteins used to design MEV construct.
| Sr. No. | Epitopes | Protein | Position | Antigenicity | Binding score (Kcal/mol) of epitopes with HLA-B7 |
|---|---|---|---|---|---|
| MHC Class I | |||||
| 1 | FLLVTLAILTAL | E | 26–37 | 0.8 | -11.95 |
| 2 | FRLFARTRSMWS | M | 100–111 | 0.71 | -11.50 |
| 3 | RLFARTRSMWSF | M | 101–112 | 0.5 | -12.95 |
| 4 | LFARTRSMWSFN | M | 102–113 | 0.9 | -12.89 |
| 5 | FHLVDFQVTIAE | orf6 | 2–13 | 1.5 | -11.60 |
| 6 | GTYEGNSPFHPL | orf7a | 38–49 | 0.6 | -10.22 |
| 7 | HPLADNKFALTC | orf7a | 58–12 | 1.3 | -12.23 |
| 8 | STQFAFACPDGV | orf7a | 61–71 | 0.9 | -14.19 |
| 9 | HQPYVVDDPCPI | orf8 | 28–39 | 0.5 | -10.79 |
| 10 | DDPCPIHFYSKW | orf8 | 34–45 | 0.8 | -10.54 |
| 11 | PIHFYSKWYIRV | orf8 | 38–49 | 0.7 | -11.20 |
| 12 | GNYTVSCLPFTI | orf8 | 77–88 | 1.7 | -10.48 |
| 13 | LPFTINCQEPKL | orf8 | 84–95 | 1.1 | -11.10 |
| 14 | KMKDLSPRWYFY | N | 100–111 | 1.4 | -10.78 |
| 15 | DPNFKDQVILLN | N | 343–354 | 1.3 | -10.04 |
| 16 | CRMNSRNYIAQV | orf10 | 19–30 | 0.6 | -12.43 |
| MHC Class II | |||||
| 1 | FLLVTLAILTALRLC | E | 26–40 | 0.6 | -14.23 |
| 2 | LEQWNLVIGFLFLTW | M | 7–31 | 1.0 | -14.41 |
| 3 | PVTLACFVLAAVYRI | M | 59–73 | 0.8 | -10.71 |
| 4 | ESELVIGAVILRGHL | M | 135–149 | 0.5 | -11.60 |
| 5 | MFHLVDFQVTIAEIL | orf6 | 1–15 | 1.0 | -11.80 |
| 6 | DGVKHVYQLRARSVS | orf7a | 69–83 | 0.7 | -12.41 |
| 7 | VVDDPCPIHFYSKW | orf8 | 3–17 | 0.5 | -11.98 |
| 8 | PKLGSLVVRCSFYED | orf8 | 93–107 | 0.7 | -11.65 |
| 9 | ALLLLDRLNQLESKM | N | 220–234 | 0.5 | -13.38 |
| 10 | FFGMSRIGMEVTPSG | N | 314–328 | 0.9 | -11.72 |
| 11 | CRMNSRNYIAQVDV | orf10 | 8–22 | 0.6 | -11.91 |
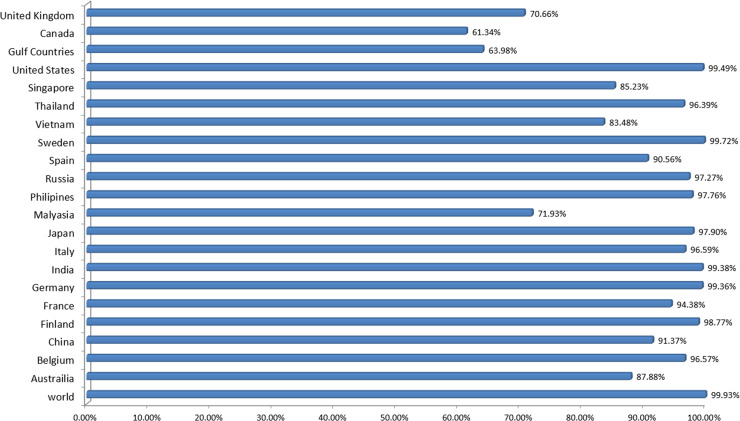
Population coverage
The distribution and expression of HLA alleles vary by ethnic groups and regions of the world. Therefore, it affects the successful development of an epitope-based vaccine. The IEDB population tool was used to check the population coverage of selected epitopes and their suitability for vaccine construct. Selected epitopes showed the 99.93% world population coverage. The highest coverage of population found within a country Sweden 99.79%. The population coverage for worst COVID-19 hit countries; United States, Italy, Spain, France and India were 99.49%, 96.59%, 90.56%, 94.38% and 99.38%, respectively (Fig 2). Likewise, significant population coverage was identified for other seriously affected countries with SARS-CoV-2 including United Kingdom, China and Australia. The result suggested that MEV designed using these selected epitopes could help to combat against COVID-19 in most of the regions around the globe.
Fig 2. Worldwide population coverage of MEV epitopes based on their respective HLA binding alleles.
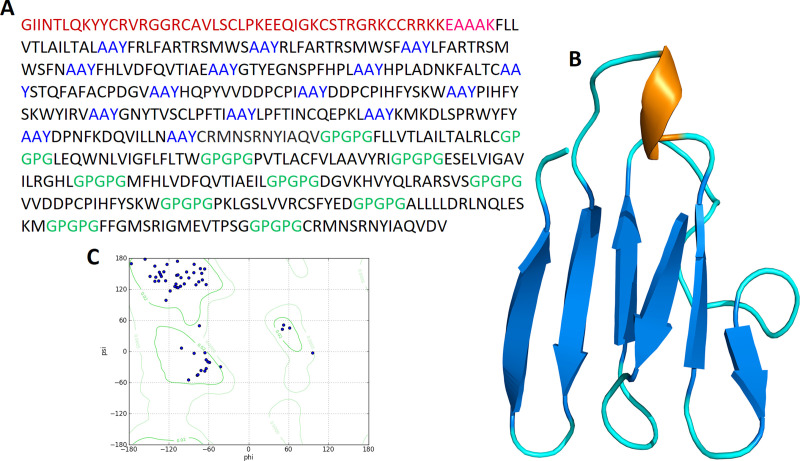
Construction of multiepitope based vaccine
All 27 selected epitopes (E-2, M-15, ORF6-2, ORF7a-4, ORF8-7, N-5, ORF10-2) were validated for their inter-interactions and next used to develop an MEV construct. An adjuvant (45 amino acid long β-defensin) was linked with the help of EAAAK linker at the start (to the N-terminal of the MEV). EAAAK linker reduce interaction with other protein regions with efficient separation and increase stability [78,79]. The vaccine's immunogenicity may increase with an adjuvant. Epitopes were merge together based on their interaction’s compatibility in sequential manner with AAY and GPGPG linkers respectively. AAY and GPGPG prevents the generation of junctional epitopes, which is a major concern in the design of multiepitope vaccines; On the other hand, they facilitates the immunization and presentation of epitopes [80,81]. The final vaccine construct comprises 505 amino acid residues (Fig 3).
Fig 3. Schematic diagram of MEV construct: An adjuvant (Maroon) linked at N-terminal with the help of EAAAK linker (Pink).
CTL epitopes are joined by AAY linkers (Blue) while HTL epitopes are joined by GPGPG linkers (Green).
Evaluation of multiepitope based vaccine
First, Blast-p analysis was performed against Homo sapiens proteome with default parameters to validate that MEV is non-homologous. Protein with less than 37% identity generally considered as non-homologous protein. However, MEV showed no similarity (higher or equal to 37%) with the human proteins.
Next, allergenicity, antigenicity and toxicity of the vaccine construct were evaluated. Results described that MEV is highly antigenic (0.6741 at 0.5% threshold), non-allergenic and non-toxic.
Next, the physiochemical properties of the SARS-CoV-2 MEV construct were determined using Protparam. It contains 505 amino acids with 55426.35 KDa molecular weight, indicating good antigenic nature. The isoelectric point (pI) of MEV was 9.12 which show its negative. Negatively charged MEV showed the value of pI less than 7. MEV was categorized as stable as instability index computed by the Protparam was 33.41. The aliphatic index was 82.75, which represents the idea of the proportional volume of the aliphatic side chains. The protein sequence has a GRAVY value of 0.105, indicating the hydrophobic nature of the MEV. Total time taken for a protein to disappear after it has been synthesized in cell depicted as the half-life of the protein which was computed as > 20 h for yeast, 30 h for mammalian-reticulocytes and > 10 h for Escherichia coli. MEV computed formula wa C2549H3850N666O669S28, depicting the cumulative numbers of Carbon (C), Oxygen (O), Nitrogen (N), Hydrogen (H) and Sulfur (S). Above results indicated MEV as a suitable potential vaccine candidate.
Structural analysis of multiepitope based vaccine
Secondary structure of MEV was predicted by PSIPRED. Among the 505 amino acids, the formation of α-helix is comprised of 176 amino acids representing 35.20%, 109 amino acids in β-strands representing 21.59% and 215 amino acids forms the coils which are 42.58% of the whole MEV construct (S3 Fig).
To determine the tertiary structure of vaccine RaptorX server was used. Structure was refined by Galaxy refine server (Fig 4). The improved model depicted that 96.3% of residues in favorable region, 3.7% of residues in permitted region and 0.0% in outer region according to Ramachandran plot analysis. Further analyses revealed qRMSD is 0.428, poor rotamers are 0%, MolProbity is 1.889, clash score is 13.6, and Z score is −2.25 Z. In addition, the refined model showed 0 errors with PROCHECK validation. The refined model score was 85.7143 in quality check analysis through ERRAT. These results show that the refined model is of good quality.
Fig 4.
(A) A 505 amino acid long MEV sequence consisting an adjuvant (Maroon) linked at N-terminal with the help of EAAAK linker (Pink). CTL epitopes are joined by AAY linkers (Blue) while HTL epitopes are joined by GPGPG linkers (Green). (B) The predicted three-dimensional structure of the MEV vaccine construct (Alpha helixes: Brown; Beta sheets: Blue; Loops: Cyan). (C) Ramachandran plot analysis result of predicted MEV structure where 96.3% of residues present in the most favorable region.
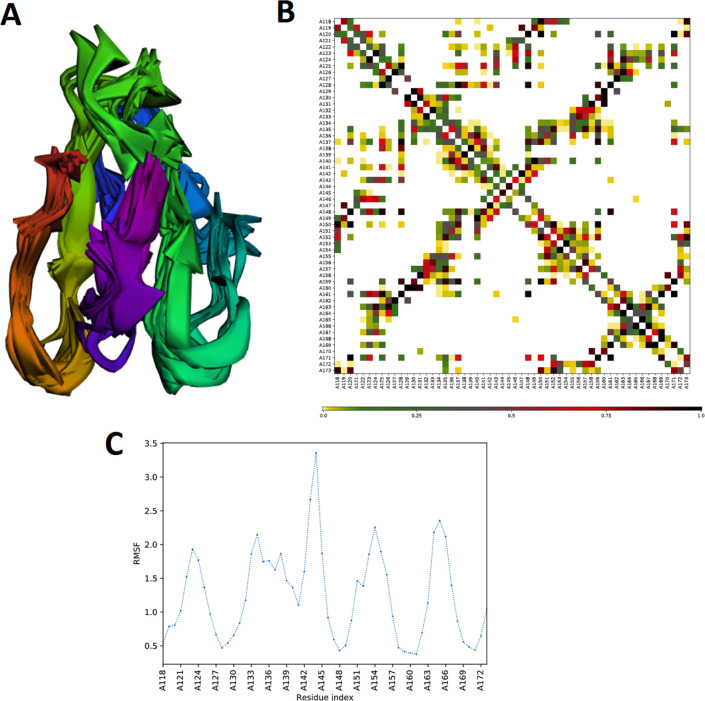
In addition, flexibility of MEV structure was evaluated using CABS-flex 2.0 server with 50 cycles simulation at 1.4°C temperature. Among the 10 final retrieved 3D structures, regions near to N-terminal depicted lesser fluctuation compared with the regions near the C-terminal (Fig 5A). Resultant contact-map presented the residue-residue interaction pattern for all the 10 final retrieved models (Fig 5B). In addition, root mean square fluctuation (RMSF) plot revealed the fluctuation of each of the amino acid of MEV model ranging from 0.0 Å to 3.5 Å. The presence of fluctuations in the MEV structure, indicated its high flexibility and endorse it as a potential vaccine construct (Fig 5C).
Fig 5. MEV structural flexibility results.
(A) Cartoon representation of top 10 final models showing obvious fluctuation throughout. (B) MEV residue-residue interaction/contact map. The interactive area is represented in the central panel. (C) RMSF plot representing the obvious fluctuations of MEV residues during simulation.
Prediction of B-cell epitopes in multiepitope based vaccine
B-lymphocytes besides secreting cytokines, also produce antigens, which in return provide humoral immunity [82]. Therefore, MEV ideally should have B-cell epitopes with its domains. Three conformational/discontinuous and 92 linear/continuous B-cell epitopes from the MEV were predicted without altering the prediction parameters of Ellipro and ABCPred 2.0 (S4 and S5 Tables).
Immunogenicity evaluation of multiepitope based vaccine
The in silico immune system simulation against MEV showed significant activity of B-cells and T-cells, which was consistent with the actual immune responses. Primary immune response was observed with the increased levels of IgM in the start. Later, secondary and tertiary immune responses were observed comparatively higher than the primary response. The immunoglobulin activity (i.e., IgG1 + IgG2, IgM, and IgG + IgM antibodies) was normally at high levels with a consistent decrease in MEV concentration. The high levels of triggered B-cells and memory B-cell formation was observed, that is indicator of an effective long-lasting immune response produced by the MEV (Fig 6A–6D). Similarly, higher levels of HTL and CTL as well as development of memory Th and Tc were observed which is vital for triggering the immune response (Fig 6E–6H). The significant levels of T regulatory cells and the continuous and increased proliferation of macrophages and dendritic cells were observed during introduction of MEV. The higher levels of cytokines like IL-2, and IFN-γ were also observed (Fig 6I–6L). These observations indicated the generation of promising antiviral response by the proposed MEV construct.
Fig 6.
In silico simulation of immune response against MEV as an antigen: (A) Antigen and immunoglobulins, (B) B-cell population, (C) B-cell population per state, (D) Plasma B-cell population, (E) Helper T-cell population, (F) Helper T-cell population per state, (G) Cytotoxic T-cell population, (H) Cytotoxic T-cell population per state, (I) Reduced levels of T regulatory cells, (J) Dendritic cell population per state, (K) Macrophage population per state, and (L) Different levels of cytokine and interleukins with Simpson index (D) of immune response.
Molecular docking of multiepitope based vaccine with TLR3 and TLR8
An appropriate association between immune receptor molecules and the antigen molecule is essential to activate an immune responsiveness. HADDOCK server has thus been used to perform the docking of the MEV with human immune receptors TLR3 and TLR8. TLR3 and TLR8 can efficiently induce the immune response after virus recognition. The docking analysis showed good interactions between the MEV and TLR3/TLR8. The binding scores of MEV-TLR3 and MEV-TLR8 were -293.90 Kcal/mol and -283.20 Kcal/mol, respectively. TLR3 is shown in the orange color, while the MEV is shown in the blue color, respectively, in Fig 7A. It was observed that MEV made 11 hydrogen bond interactions within range of 3.00 Å with TLR3 Fig 7B and 7C. MEV interacting amino acids with hydrogen bonding to TLR3 shown in green color stick representation, while similarly TLR3 amino acids interacting through hydrogen bonding with MEV shown in red color stick representation.
Fig 7.
MEV construct docking with human TLR3: (A) MEV-TLR3 docked complex in cartoon representation. TLR3 displayed with brown color and MEV vaccine construct displayed with blue color. (B) Interacting residues illustration between MEV and TLR3 complex. Interacting residues of MEV are highlighted with green color stick representation, while interacting residues of TLR3 are highlighted with red color stick representation. Hydrogen bonds are represented with yellow color dotted lines. (C) All interacting residues of MEV and TLR3. Hydrogen bonds are shown with blue color lines. The colors of interacting residues are representing properties of amino acids (Positive: Blue, Negative: Red, Neutral: Green, Aliphatic: Grey, Aromatic: Pink, Pro&Gly: Orange and Cys: Yellow).
In case of TLR8, it is shown in the grey color, while the MEV is shown in the blue color, respectively, in Fig 8A. It was observed that MEV made 9 hydrogen bond interactions within range of 3.00 Å with TLR8 Fig 8B and 8C. Similar to TLR3, MEV interacting amino acids with hydrogen bonding to TLR8 shown in green color stick representation, while TLR8 amino acids interacting through hydrogen bonding with MEV shown in red color stick representation. These results indicated that this MEV is best suitable candidate for vaccine production.
Fig 8.
MEV construct docking with human TLR8: (A) MEV-TLR8 docked complex in cartoon representation. TLR8 displayed with grey color and MEV vaccine construct displayed with blue color. (B) Interacting residues illustration between MEV and TLR8 complex. Interacting residues of MEV are highlighted with green color stick representation, while interacting residues of TLR8 are highlighted with red color stick representation. Hydrogen bonds are represented with yellow color dotted lines. (C) All interacting residues of MEV and TLR8. Hydrogen bonds are shown with blue color lines. The colors of interacting residues are representing properties of amino acids (Positive: Blue, Negative: Red, Neutral: Green, Aliphatic: Grey, Aromatic: Pink, Pro&Gly: Orange and Cys: Yellow).
MD simulation of TLR3-MEV and TLR8-MEV complexes
MD simulation is a common approach used to analyze the micro-interactions between ligand/vaccine and protein/receptor structures [70]. In order to further assess MEV dynamics and stability, its docking complexes with TLR3 and TLR8 were simulated by 20 ns MD followed by Root Mean Square Deviations (RMSD) and Root Mean Square Fluctuations (RMSF) analysis. The values of RMSD of backbone atoms were computed to monitor the structural stability of MEV and immune receptor complexes (Fig 9A). The RMSD average values for both complexes TLR3-MEV and TLR8-MEV are 4.5 ± 0.02 Å and 5.6 ± 0.02 Å, respectively. There were no significant variations noticed in both docked complexes. Both the systems remain stable throughout 20 ns simulation. To further compute, the residual and side-chain flexibility, RMSF over 20 ns time were computed. Little fluctuations at the terminal constituent residues of both complexes were observed, while middle residues depicted stable behavior with an average 1.5 ± 0.02 Å RMSF (Fig 9B). In general, both complexes were stable without obvious fluctuations. These results validate the docking interaction analysis and endorsed that MEV can strongly bind with immune receptors to generate significant immune response against SARS-CoV-2.
Fig 9.
MD simulation at 20 ns results: (A) The RMSD plot of the MEV-TLR3 and MEV-TLR8 complexes. MEV-TLR3 complex RMSD represented with purple color line while MEV-TLR8 complex RMSD is represented with orange color line. (B) The RMSF plot of the MEV-TLR3 and MEV-TLR8 complexes. MEV-TLR3 complex RMSF represented with purple color line while MEV-TLR8 complex RMSF is represented with orange color line.
MM/PBSA binding free energy calculations
Further, the binding affinity of the vaccine-receptor complexes was validated using MM/PBSA calculations. As shown in Table 2, the total binding energies (ΔTOTAL) of TLR3-MEV and TLR8-MEV complexes are −57.67 kcal/mol and −66.09 kcal/mol, respectively. The MMPBSA net binding energy demonstrates both systems interaction energies significantly favorable and stable. The intermolecular interactions are dominated by both vanderWaals (VDWAALS) and electrostatic energies (EEL).
Table 2. Binding free energies statistics for the TLR3-MEV and TLR8-MEV complexes.
| Energy Components (Kcal/mol) | TLR3-MEV | TLR8-MEV |
|---|---|---|
| VDWAALS | -170.66 | -183.91 |
| EEL | -321.93 | -297.77 |
| EPB | 457.36 | 439.71 |
| ENPOLAR | -22.44 | -24.12 |
| ΔG gas | -492.59 | -481.68 |
| ΔG solv | 434.92 | 415.59 |
| ΔTOTAL | -57.67 | -66.09 |
In silico cloning
In silico cloning was performed to ensure expression of SARS-CoV-2 derived MEV in commonly used E. coli host. First, codons of MEV construct were adapted as per codon usage of E. coli expression system. JCAT server was used to optimize the MEV codons according to E. coli (strain K12). The optimized MEV construct contained 1515 nucleotides (S6 Table), an ideal range of GC content 56.30% (30–70%) and CAI value 0.93 (0.8–1.0), and showing the high possibility of positive protein expression and reliability. In next step, buffer compatible restriction enzymes XhoI and HindIII restriction sites were added to both ends of MEV optimized nucleotide sequence to aid the cloning/purification process. Finally, refined MEV sequence was cloned between XhoI and HindIII restriction sites at the multiple cloning site of pET28a (+) vector (Fig 10). The total length of the clone was 6.875 kbp.
Fig 10. MEV codon optimized nucleotide sequence for E. coli expression system, in silico cloned at multiple cloning site (MCS) of pET28a(+) vector, shown with blue color in vector backbone (black color) and with grey color functional annotation.
MEV cloned sequence is surrounded by XhoI (158) and HindIII (1679) restriction enzyme site, and 6-histidine residues.
Discussion
Vaccination has many useful effects for improving people health at a low-cost and best aid to inhibit transmission of diseases around the world. However, the development and production of the vaccine is labor-intensive and costly. Immunoinformatics approaches can reduce this burden. Today researchers are searching methods for the development of subunit vaccines from complete genome/proteome of pathogens [83]. Epitope prediction for antibodies becomes more significant with the advancement of the computational tools for designing a vaccine [84]. In the field of bioinformatics, Immuno-informatics is a sub-branch that includes a lot of tools & databases. Immunological datasets prediction and in silico analysis are done with the help of those tools. With the advancement of tools and a variety of data availability like genomic, proteomic, and different algorithms made it more effective for scientists to accurately predict epitopes that are much effective in the development of the sub-unit vaccines [13,14,85].
An outbreak of SARS-COV-2 in late December 2019 that later turned into a global pandemic resulted in thousands of deaths around the globe [6]. After the outbreak, remarkable progress has been made towards the structural genomics, proteomics and drug repurposing against the SARS-CoV-2, yet there is no exact cure has been identified for COVID-19. Till date, no completely effective vaccine is available against SARS-CoV-2. Therefore, COVID-19 vaccine needs to be designed so that global pandemic situation could be controlled effectively.
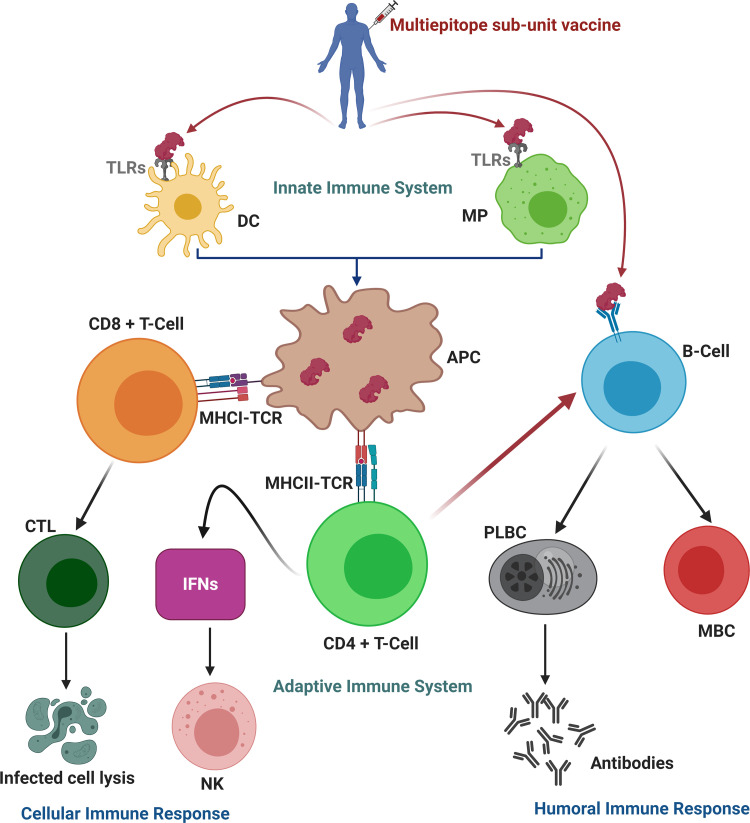
The recent study was conducted to design a multiepitope based vaccine (MEV) against SARS-COV-2 by using immunoinformatics and in silico approaches. Multiepitope based sub-unit vaccine presented in this study, is advantageous compared to monovalent vaccine because it can elicit humoral, innate and cellular immunity responses together (Fig 11) [86]. To date, various studies reported several epitopes for COVID-19 vaccine development. Sohail et al., recently compared 65 reviewed studies related to SARS-CoV-2 epitopes prediction [87]. They reported that a high percentage of experimentally determined epitopes are identical to the epitopes reported using in silico methods [87]. This offers proof of the practical significance of immunoinformatics. Similarly, various studies reported MEV constructs for SARS-CoV-2 using one or multiple proteins [33,34,88–95]. But none of them used all anti-genic proteins of SARS-CoV-2 both structure and non-structure collectively to screen a pool of conserved/overlapping epitopes to design a comprehensive MEV construct. Since vaccines have high failure rates, we are presenting a novel MEV construct which is very promising candidate to fight against COVID-19. In this study, amino acid sequences of all ten vaccine target proteins of SARS-COV-2 were taken from Genbank and their antigenicity was checked. Only highly antigenic proteins were selected for downward analysis. After the complete physiochemical analysis of antigenic proteins, B-cell and T-cell with IFN-γ inducing potential were predicted. Antigenic and overlapped T-cell epitopes with B-cells were further validated using molecular docking with HLA-B7 allele and their population coverage was estimated. After All, MEV was designed with the help of linkers and adjuvant. An adjuvant was added to the N-terminal of the MEV and epitopes were linked with the help of AAY and GPGPG linkers. Adjuvant was added to increase the immunogenicity of the vaccine [96]. Linkers were added to help maintain the function of each epitope, so that after being imported into the human body, they can function independently/properly [42,97].
Fig 11. Proposed immunity pathway in host simulated in response to multiepitope based sub-unit vaccine.
The vaccine enters into cell, attached to dendritic cells (DC) and macrophages (MP) via toll like receptors (TLRs), and thus in turn trigger innate immune response. Then, antigen-presenting cells (APC) processed the vaccine’s epitopes and presented it to the T-cell which in turn trigger adaptive immune response. The T-cell prompt other immune cells or directly kills the infected cells (cellular immune response), whereas plasma B-cells (PLBC) produced antibodies to neutralize the viruses and memory B-cells (MBC) store all the information to trigger robust immune response in the case of re-infection (humoral immune response). (CD: cluster of differentiation; MHC: major histocompatibility complex; TCR: T-cell receptors; CTL: cytotoxic T lymphocytes; IFNs: Interferons; NK: natural killer cells). Figure was created using BioRender (https://biorender.com/).
MEV was found to be highly antigenic, immunogenic, non-toxic and non-allergenic indicating an epitope-based vaccine’s potential to cause robust immune responses. During in silico immunological validation analysis, higher B and T-cell activity was observed that is rationally identical with typical immune responses. B and T-cell memory formation was evident, and results depicted it last for several months. Molecular docking analysis followed by MD simulation and binding free energy analysis revealed that the MEV is potentially able to properly/firmly occupy the TLR3/TLR8 receptors with minimal energy. Furthermore, the expression of MEV construct inside the host E. coli K12 was improved through codon optimization. The results of recent study suggest that the MEV being designed is a potential candidate to undergo in vivo and in vitro experimental analysis to develop a potential vaccine against COVID-19.
Conclusions
Recent global pandemic of SARS-CoV-2 claimed hundreds of precious lives in various regions of the world and crumble the economies of several countries. There is no approved drug or completely effective vaccine reported against SARS-CoV-2 yet. In this study, a successful attempt was made to design a sub-unit MEV against SARS-COV-2. Immunoinformatics and in silico approaches were used to develop a potential and safe MEV that could trigger three types of the immune responses: humoral, innate and cellular. A highly immunogenic, safe, stable and strongly interacting with human receptors, MEV has been reported in present study that could be a potential candidate for vaccine production. However, current research is the result of an integrated vaccinomics approach. Therefore, further experimental research by the vaccinologists is required to demonstrate the efficacy of the designed vaccine.
Supporting information
Hydrogen bond interactions are highlighted with yellow color dotted lines. Numbering 1–16 is consistent with the Table 1 of main text.
(DOCX)
Hydrogen bond interactions are highlighted with yellow color dotted lines. Numbering 1–11 is consistent with the Table 1 of main text.
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Green color bold sequence at 5`site (N-terminal) is representing XhoI restriction enzyme site, while maroon color bold sequence at 3`site (C-terminal) is representing HindIII restriction enzyme site.
(DOCX)
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
This work was supported by the Starting Research Grant for High-level Talents from Guangxi University (L.L.C.) and Postdoctoral project from Guangxi University (M.T.Q.). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Tripp RA, Tompkins SM. Roles of Host Gene and Non-coding RNA Expression in Virus Infection: Springer; 2018. [Google Scholar]
- 2.Xu X, Chen P, Wang J, Feng J, Zhou H, Li X, et al. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci China Life Sci. 2020;63(3):457–460. 10.1007/s11427-020-1637-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. 10.1056/NEJMoa2001017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tahir ul Qamar M, Alqahtani SM, Alamri MA, Chen L-L. Structural Basis of SARS-CoV-2 3CLpro and Anti-COVID-19 Drug Discovery from Medicinal Plants. Journal of Pharmaceutical Analysis. 2020;10(4):313–319. 10.1016/j.jpha.2020.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hui DS, I Azhar E, Madani TA, Ntoumi F, Kock R, Dar O, et al. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health—The latest 2019 novel coronavirus outbreak in Wuhan, China. International Journal of Infectious Diseases. 2020;91:264–266. 10.1016/j.ijid.2020.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alamri MA, Tahir ul Qamar M, Usman Mirza M, Bhadane R, Alqahtani SM, Muneer I, et al. Pharmacoinformatics and molecular dynamics simulation studies reveal potential covalent and FDA-approved inhibitors of SARS-CoV-2 main protease 3CLpro. Journal of Biomolecular Structure and Dynamics. 2020. 10.1080/07391102.2020.1782768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahmed T, Noman M, Almatroudi A, Shahid M, Khurshid M, Tariq F, et al. Coronavirus Disease 2019 Assosiated Pneumonia in China: Current Status and Future Prospects. Preprints. 2020;2020020358. [Google Scholar]
- 9.Lu H. Drug treatment options for the 2019-new coronavirus (2019-nCoV). Biosci Trends. 2020;14(1):69–71. 10.5582/bst.2020.01020 [DOI] [PubMed] [Google Scholar]
- 10.Abdelmageed MI, Abdelmoneim AH, Mustafa MI, Elfadol NM, Murshed NS, Shantier SW, et al. Design of multi epitope-based peptide vaccine against E protein of human 2019-nCoV: An immunoinformatics approach. BioRxiv. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang M, Cao R, Zhang L, Yang X, Liu J, Xu M, et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020;30(3):269–271. 10.1038/s41422-020-0282-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Amanat F, Krammer F. SARS-CoV-2 Vaccines: Status Report. Immunity. 2020;52(4):583–589. 10.1016/j.immuni.2020.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.De Gregorio E, Rappuoli R. Vaccines for the future: learning from human immunology. Microb Biotechnol. 2012;5(2):149–155. 10.1111/j.1751-7915.2011.00276.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patronov A, Doytchinova I. T-cell epitope vaccine design by immunoinformatics. Open Biol. 2013;3(1):120139 10.1098/rsob.120139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gupta N, Regar H, Verma VK, Prusty D, Mishra A, Prajapati VK. Receptor-ligand based molecular interaction to discover adjuvant for immune cell TLRs to develop next-generation vaccine. Int J Biol Macromol. 2020;152:535–545. 10.1016/j.ijbiomac.2020.02.297 [DOI] [PubMed] [Google Scholar]
- 16.Kalita P, Lyngdoh DL, Padhi AK, Shukla H, Tripathi T. Development of multi-epitope driven subunit vaccine against Fasciola gigantica using immunoinformatics approach. International journal of biological macromolecules. 2019;138:224–233. 10.1016/j.ijbiomac.2019.07.024 [DOI] [PubMed] [Google Scholar]
- 17.Saadi M, Karkhah A, Nouri HR. Development of a multi-epitope peptide vaccine inducing robust T cell responses against brucellosis using immunoinformatics based approaches. Infection, Genetics and Evolution. 2017;51:227–234. 10.1016/j.meegid.2017.04.009 [DOI] [PubMed] [Google Scholar]
- 18.Nain Z, Karim MM, Sen MK, Adhikari UK. Structural Basis and Designing of Peptide Vaccine using PE-PGRS Family Protein of Mycobacterium ulcerans–An Integrated Vaccinomics Approach. bioRxiv. 2019:795146. [DOI] [PubMed] [Google Scholar]
- 19.Tahir Ul Qamar M, Saleem S, Ashfaq UA, Bari A, Anwar F, Alqahtani S. Epitope-based peptide vaccine design and target site depiction against Middle East Respiratory Syndrome Coronavirus: an immune-informatics study. J Transl Med. 2019;17(1):362 10.1186/s12967-019-2116-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tahir ul Qamar M, Shokat Z, Muneer I, Ashfaq UA, Javed H, Anwar F, et al. Multiepitope-Based Subunit Vaccine Design and Evaluation against Respiratory Syncytial Virus Using Reverse Vaccinology Approach. Vaccines. 2020;8(2):288 10.3390/vaccines8020288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tahir Ul Qamar M, Bari A, Adeel MM, Maryam A, Ashfaq UA, Du X, et al. Peptide vaccine against chikungunya virus: immuno-informatics combined with molecular docking approach. J Transl Med. 2018;16(1):298 10.1186/s12967-018-1672-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ahmad B, Ashfaq UA, Rahman MU, Masoud MS, Yousaf MZ. Conserved B and T cell epitopes prediction of ebola virus glycoprotein for vaccine development: An immuno-informatics approach. Microb Pathog. 2019;132:243–253. 10.1016/j.micpath.2019.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shahid F, Ashfaq UA, Javaid A, Khalid H. Immunoinformatics guided rational design of a next generation multi epitope based peptide (MEBP) vaccine by exploring Zika virus proteome. Infect Genet Evol. 2020;80:104199 10.1016/j.meegid.2020.104199 [DOI] [PubMed] [Google Scholar]
- 24.Ikram A, Zaheer T, Awan FM, Obaid A, Naz A, Hanif R, et al. Exploring NS3/4A, NS5A and NS5B proteins to design conserved subunit multi-epitope vaccine against HCV utilizing immunoinformatics approaches. Sci Rep. 2018;8(1):16107 10.1038/s41598-018-34254-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pandey RK, Dahiya S, Mahita J, Sowdhamini R, Prajapati VK. Vaccination and immunization strategies to design Aedes aegypti salivary protein based subunit vaccine tackling Flavivirus infection. Int J Biol Macromol. 2019;122:1203–1211. 10.1016/j.ijbiomac.2018.09.071 [DOI] [PubMed] [Google Scholar]
- 26.Chauhan V, Singh MP. Immuno-informatics approach to design a multi-epitope vaccine to combat cytomegalovirus infection. Eur J Pharm Sci. 2020;147:105279 10.1016/j.ejps.2020.105279 [DOI] [PubMed] [Google Scholar]
- 27.Pandey RK, Ojha R, Aathmanathan VS, Krishnan M, Prajapati VK. Immunoinformatics approaches to design a novel multi-epitope subunit vaccine against HIV infection. Vaccine. 2018;36(17):2262–2272. 10.1016/j.vaccine.2018.03.042 [DOI] [PubMed] [Google Scholar]
- 28.Kesherwani V, Tarang S. An immunoinformatic approach to universal therapeutic vaccine design against BK virus. Vaccine. 2019;37(26):3457–3463. 10.1016/j.vaccine.2019.04.096 [DOI] [PubMed] [Google Scholar]
- 29.Azim KF, Hasan M, Hossain MN, Somana SR, Hoque SF, Bappy MNI, et al. Immunoinformatics approaches for designing a novel multi epitope peptide vaccine against human norovirus (Norwalk virus). Infect Genet Evol. 2019;74:103936 10.1016/j.meegid.2019.103936 [DOI] [PubMed] [Google Scholar]
- 30.Mirza MU, Rafique S, Ali A, Munir M, Ikram N, Manan A, et al. Towards peptide vaccines against Zika virus: Immunoinformatics combined with molecular dynamics simulations to predict antigenic epitopes of Zika viral proteins. Sci Rep. 2016;6:37313 10.1038/srep37313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khan A, Junaid M, Kaushik AC, Ali A, Ali SS, Mehmood A, et al. Computational identification, characterization and validation of potential antigenic peptide vaccines from hrHPVs E6 proteins using immunoinformatics and computational systems biology approaches. PloS one. 2018;13(5). 10.1371/journal.pone.0196484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Katalani C, Nematzadeh G, Ahmadian G, Amani J, Kiani G, Ehsani P. In silico design and in vitro analysis of a recombinant trivalent fusion protein candidate vaccine targeting virulence factor of Clostridium perfringens. Int J Biol Macromol. 2020;146:1015–1023. 10.1016/j.ijbiomac.2019.09.227 [DOI] [PubMed] [Google Scholar]
- 33.Ahmad S, Waheed Y, Ismail S, Abbasi SW, Najmi MH. A computational study to disclose potential drugs and vaccine ensemble for COVID-19 conundrum. Journal of molecular liquids. 2020:114734 10.1016/j.molliq.2020.114734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tahir ul Qamar M, Shahid F, Aslam S, Ashfaq UA, Aslam S, Fatima I, et al. Reverse vaccinology assisted designing of multiepitope-based subunit vaccine against SARS-COV-2. Infectious Diseases of Poverty. 2020. 10.1186/s40249-020-00752-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hunter RL. Overview of vaccine adjuvants: present and future. Vaccine. 2002;20 Suppl 3:S7–12. 10.1016/s0264-410x(02)00164-0 [DOI] [PubMed] [Google Scholar]
- 36.Guy B. The perfect mix: recent progress in adjuvant research. Nat Rev Microbiol. 2007;5(7):505–517. 10.1038/nrmicro1681 [DOI] [PubMed] [Google Scholar]
- 37.Benson DA, Karsch-Mizrachi I, Lipman DJ, Ostell J, Sayers EW. GenBank. Nucleic acids research. 2008;37(suppl_1):D26–D31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Walker JM. The proteomics protocols handbook: Springer; 2005. [Google Scholar]
- 39.Doytchinova IA, Flower DR. VaxiJen: a server for prediction of protective antigens, tumour antigens and subunit vaccines. BMC Bioinformatics. 2007;8(1):4 10.1186/1471-2105-8-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Deléage G. ALIGNSEC: viewing protein secondary structure predictions within large multiple sequence alignments. Bioinformatics. 2017. 10.1093/bioinformatics/btx521 [DOI] [PubMed] [Google Scholar]
- 41.Kallberg M, Wang H, Wang S, Peng J, Wang Z, Lu H, et al. Template-based protein structure modeling using the RaptorX web server. Nat Protoc. 2012;7(8):1511–1522. 10.1038/nprot.2012.085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pandey RK, Bhatt TK, Prajapati VK. Novel Immunoinformatics Approaches to Design Multi-epitope Subunit Vaccine for Malaria by Investigating Anopheles Salivary Protein. Sci Rep. 2018;8(1):1125 10.1038/s41598-018-19456-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Waterhouse A, Bertoni M, Bienert S, Studer G, Tauriello G, Gumienny R, et al. SWISS-MODEL: homology modelling of protein structures and complexes. Nucleic Acids Res. 2018;46(W1):W296–W303. 10.1093/nar/gky427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cooper MD. The early history of B cells. Nat Rev Immunol. 2015;15(3):191–197. 10.1038/nri3801 [DOI] [PubMed] [Google Scholar]
- 45.Zheng J, Lin X, Wang X, Zheng L, Lan S, Jin S, et al. In Silico Analysis of Epitope-Based Vaccine Candidates against Hepatitis B Virus Polymerase Protein. Viruses. 2017;9(5). 10.3390/v9050112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kolaskar AS, Tongaonkar PC. A semi-empirical method for prediction of antigenic determinants on protein antigens. FEBS Lett. 1990;276(1–2):172–174. 10.1016/0014-5793(90)80535-q [DOI] [PubMed] [Google Scholar]
- 47.Ponomarenko J, Bui HH, Li W, Fusseder N, Bourne PE, Sette A, et al. ElliPro: a new structure-based tool for the prediction of antibody epitopes. BMC Bioinformatics. 2008;9(1):514 10.1186/1471-2105-9-514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nain Z, Abdulla F, Rahman MM, Karim MM, Khan MSA, Sayed SB, et al. Proteome-wide screening for designing a multi-epitope vaccine against emerging pathogen Elizabethkingia anophelis using immunoinformatic approaches. Journal of Biomolecular Structure and Dynamics. 2019:1–18. 10.1080/07391102.2019.1692072 [DOI] [PubMed] [Google Scholar]
- 49.Vita R, Overton JA, Greenbaum JA, Ponomarenko J, Clark JD, Cantrell JR, et al. The immune epitope database (IEDB) 3.0. Nucleic Acids Res. 2015;43(Database issue):D405–412. 10.1093/nar/gku938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fleri W, Paul S, Dhanda SK, Mahajan S, Xu X, Peters B, et al. The Immune Epitope Database and Analysis Resource in Epitope Discovery and Synthetic Vaccine Design. Front Immunol. 2017;8:278 10.3389/fimmu.2017.00278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bui HH, Sidney J, Li W, Fusseder N, Sette A. Development of an epitope conservancy analysis tool to facilitate the design of epitope-based diagnostics and vaccines. BMC Bioinformatics. 2007;8(1):361 10.1186/1471-2105-8-361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sarkar SN, Sen GC. Novel functions of proteins encoded by viral stress-inducible genes. Pharmacol Ther. 2004;103(3):245–259. 10.1016/j.pharmthera.2004.07.007 [DOI] [PubMed] [Google Scholar]
- 53.Fuse S, Molloy MJ, Usherwood EJ. Immune responses against persistent viral infections: possible avenues for immunotherapeutic interventions. Crit Rev Immunol. 2008;28(2):159–183. 10.1615/critrevimmunol.v28.i2.40 [DOI] [PubMed] [Google Scholar]
- 54.Morris GM, Lim-Wilby M. Molecular docking: Springer; 2008. 365–382 p. [DOI] [PubMed] [Google Scholar]
- 55.Lamiable A, Thevenet P, Rey J, Vavrusa M, Derreumaux P, Tuffery P. PEP-FOLD3: faster de novo structure prediction for linear peptides in solution and in complex. Nucleic Acids Res. 2016;44(W1):W449–454. 10.1093/nar/gkw329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.DeLano WLJCNopc. Pymol: An open-source molecular graphics tool. CCP4 Newsletter on protein crystallography. 2002;40(1):82–92. 10.1053/ajkd.2002.33916 [DOI] [PubMed] [Google Scholar]
- 57.Gasteiger E, Hoogland C, Gattiker A, Wilkins MR, Appel RD, Bairoch A. Protein identification and analysis tools on the ExPASy server: Springer; 2005. 571–607 p. [DOI] [PubMed] [Google Scholar]
- 58.Dimitrov I, Flower DR, Doytchinova I. AllerTOP-a server for in silico prediction of allergens. BMC bioinformatics. 2013;14(6):S4 10.1186/1471-2105-14-S6-S4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.McGuffin LJ, Bryson K, Jones DT. The PSIPRED protein structure prediction server. Bioinformatics. 2000;16(4):404–405. 10.1093/bioinformatics/16.4.404 [DOI] [PubMed] [Google Scholar]
- 60.Heo L, Park H, Seok C. GalaxyRefine: Protein structure refinement driven by side-chain repacking. Nucleic Acids Res. 2013;41(Web Server issue):W384–388. 10.1093/nar/gkt458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lovell SC, Davis IW, Arendall WB III, De Bakker PI, Word JM, Prisant MG, et al. Structure validation by Cα geometry: ϕ, ψ and Cβ deviation. Proteins: Structure, Function, and Bioinformatics. 2003;50(3):437–450. [DOI] [PubMed] [Google Scholar]
- 62.Wiederstein M, Sippl MJ. ProSA-web: interactive web service for the recognition of errors in three-dimensional structures of proteins. Nucleic Acids Res. 2007;35(Web Server issue):W407–410. 10.1093/nar/gkm290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lengths M, Angles M. Limitations of structure evaluation tools errat. Quick Guideline Comput Drug Des. 2018;16:75. [Google Scholar]
- 64.Kuriata A, Gierut AM, Oleniecki T, Ciemny MP, Kolinski A, Kurcinski M, et al. CABS-flex 2.0: a web server for fast simulations of flexibility of protein structures. Nucleic Acids Res. 2018;46(W1):W338–W343. 10.1093/nar/gky356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kurcinski M, Oleniecki T, Ciemny MP, Kuriata A, Kolinski A, Kmiecik S. CABS-flex standalone: a simulation environment for fast modeling of protein flexibility. Bioinformatics. 2019;35(4):694–695. 10.1093/bioinformatics/bty685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rapin N, Lund O, Bernaschi M, Castiglione F. Computational immunology meets bioinformatics: the use of prediction tools for molecular binding in the simulation of the immune system. PLoS One. 2010;5(4). 10.1371/journal.pone.0009862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kroger AT. General recommendations on immunization. US Department of Health and Human Services, Public Health Service, Centers for Disease Control. 2013. [Google Scholar]
- 68.Castiglione F, Mantile F, De Berardinis P, Prisco A. How the interval between prime and boost injection affects the immune response in a computational model of the immune system. Computational and mathematical methods in medicine. 2012;2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Laskowski RA. PDBsum new things. Nucleic Acids Res. 2009;37(Database issue):D355–359. 10.1093/nar/gkn860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hansson T, Oostenbrink C, van Gunsteren W. Molecular dynamics simulations. Curr Opin Struct Biol. 2002;12(2):190–196. 10.1016/s0959-440x(02)00308-1 [DOI] [PubMed] [Google Scholar]
- 71.Abraham MJ, Murtola T, Schulz R, Páll S, Smith JC, Hess B, et al. GROMACS: High performance molecular simulations through multi-level parallelism from laptops to supercomputers. SoftwareX. 2015;1:19–25. [Google Scholar]
- 72.Alamri MA, Tahir ul Qamar M, Mirza MU, Alqahtani SM, Froeyen M, Chen L-L. Discovery of human coronaviruses pan-papain-like protease inhibitors using computational approaches. Journal of Pharmaceutical Analysis. 2020. 10.1016/j.jpha.2020.08.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tahir Ul Qamar M, Maryam A, Muneer I, Xing F, Ashfaq UA, Khan FA, et al. Computational screening of medicinal plant phytochemicals to discover potent pan-serotype inhibitors against dengue virus. Sci Rep. 2019;9(1):1433 10.1038/s41598-018-38450-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Grote A, Hiller K, Scheer M, Munch R, Nortemann B, Hempel DC, et al. JCat: a novel tool to adapt codon usage of a target gene to its potential expression host. Nucleic Acids Res. 2005;33(Web Server issue):W526–531. 10.1093/nar/gki376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Smith CL, Econome JG, Schutt A, Klco S, Cantor CR. A physical map of the Escherichia coli K12 genome. Science. 1987;236(4807):1448–1453. 10.1126/science.3296194 [DOI] [PubMed] [Google Scholar]
- 76.Sharp PM, Li WH. The codon Adaptation Index—a measure of directional synonymous codon usage bias, and its potential applications. Nucleic Acids Res. 1987;15(3):1281–1295. 10.1093/nar/15.3.1281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Luckheeram RV, Zhou R, Verma AD, Xia B. CD4+ T cells: differentiation and functions. Clinical and developmental immunology. 2012;2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Arai R, Ueda H, Kitayama A, Kamiya N, Nagamune T. Design of the linkers which effectively separate domains of a bifunctional fusion protein. Protein engineering. 2001;14(8):529–532. 10.1093/protein/14.8.529 [DOI] [PubMed] [Google Scholar]
- 79.Pandey RK, Narula A, Naskar M, Srivastava S, Verma P, Malik R, et al. Exploring dual inhibitory role of febrifugine analogues against Plasmodium utilizing structure-based virtual screening and molecular dynamic simulation. J Biomol Struct Dyn. 2017;35(4):791–804. 10.1080/07391102.2016.1161560 [DOI] [PubMed] [Google Scholar]
- 80.Nezafat N, Karimi Z, Eslami M, Mohkam M, Zandian S, Ghasemi Y. Designing an efficient multi-epitope peptide vaccine against Vibrio cholerae via combined immunoinformatics and protein interaction based approaches. Comput Biol Chem. 2016;62:82–95. 10.1016/j.compbiolchem.2016.04.006 [DOI] [PubMed] [Google Scholar]
- 81.Livingston B, Crimi C, Newman M, Higashimoto Y, Appella E, Sidney J, et al. A rational strategy to design multiepitope immunogens based on multiple Th lymphocyte epitopes. J Immunol. 2002;168(11):5499–5506. 10.4049/jimmunol.168.11.5499 [DOI] [PubMed] [Google Scholar]
- 82.Lund FE. Cytokine-producing B lymphocytes—key regulators of immunity. Current opinion in immunology. 2008;20(3):332–338. 10.1016/j.coi.2008.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Khatoon N, Pandey RK, Prajapati VK. Exploring Leishmania secretory proteins to design B and T cell multi-epitope subunit vaccine using immunoinformatics approach. Sci Rep. 2017;7(1):8285 10.1038/s41598-017-08842-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Dubey KK, Luke GA, Knox C, Kumar P, Pletschke BI, Singh PK, et al. Vaccine and antibody production in plants: developments and computational tools. Brief Funct Genomics. 2018;17(5):295–307. 10.1093/bfgp/ely020 [DOI] [PubMed] [Google Scholar]
- 85.Yang X, Yu X. An introduction to epitope prediction methods and software. Rev Med Virol. 2009;19(2):77–96. 10.1002/rmv.602 [DOI] [PubMed] [Google Scholar]
- 86.Amanna IJ, Slifka MK. Contributions of humoral and cellular immunity to vaccine-induced protection in humans. Virology. 2011;411(2):206–215. 10.1016/j.virol.2010.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sohail MS, Ahmed SF, Quadeer AA, McKay M. In Silico T Cell Epitope Identification for SARS-CoV-2: Progress and Perspectives. Available at SSRN 3720371. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ahmad S, Navid A, Farid R, Abbas G, Ahmad F, Zaman N, et al. Design of a Novel Multi Epitope-Based Vaccine for Pandemic Coronavirus Disease (COVID-19) by Vaccinomics and Probable Prevention Strategy against Avenging Zoonotics. Eur J Pharm Sci. 2020;151:105387 10.1016/j.ejps.2020.105387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ka T, Narsaria U, Basak S, De D, Castiglion F, Mueller DM, et al. A Candidate multi-epitope vaccine against SARS-CoV-2. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Bhattacharya M, Sharma AR, Patra P, Ghosh P, Sharma G, Patra BC, et al. Development of epitope‐based peptide vaccine against novel coronavirus 2019 (SARS‐COV‐2): Immunoinformatics approach. Journal of medical virology. 2020;92(6):618–631. 10.1002/jmv.25736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Chen H-Z, Tang L-L, Yu X-L, Zhou J, Chang Y-F, Wu X. Bioinformatics analysis of epitope-based vaccine design against the novel SARS-CoV-2. Infectious diseases of poverty. 2020;9(1):1–10. 10.1186/s40249-019-0617-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Samad A, Ahammad F, Nain Z, Alam R, Imon RR, Hasan M, et al. Designing a multi-epitope vaccine against SARS-CoV-2: an immunoinformatics approach. Journal of Biomolecular Structure and Dynamics. 2020:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rahman MS, Hoque MN, Islam MR, Akter S, Rubayet-Ul-Alam A, Siddique MA, et al. Epitope-based chimeric peptide vaccine design against S, M and E proteins of SARS-CoV-2 etiologic agent of global pandemic COVID-19: an in silico approach. PeerJ. 2020;8:e9572 10.7717/peerj.9572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kalita P, Padhi A, Zhang KY, Tripathi T. Design of a peptide-based subunit vaccine against novel coronavirus SARS-CoV-2. Microbial Pathogenesis. 2020:104236 10.1016/j.micpath.2020.104236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Waqas M, Haider A, Sufyan M, Siraj S, Sehgal SA. Determine the potential Epitope based Peptide Vaccine against novel SARS-CoV-2 targeting structural proteins using immunoinformatics approaches. Frontiers in molecular biosciences. 2020;7 10.3389/fmolb.2020.00227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Pashine A, Valiante NM, Ulmer JB. Targeting the innate immune response with improved vaccine adjuvants. Nat Med. 2005;11(4 Suppl):S63–68. 10.1038/nm1210 [DOI] [PubMed] [Google Scholar]
- 97.Shamriz S, Ofoghi H, Moazami N. Effect of linker length and residues on the structure and stability of a fusion protein with malaria vaccine application. Comput Biol Med. 2016;76:24–29. 10.1016/j.compbiomed.2016.06.015 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Hydrogen bond interactions are highlighted with yellow color dotted lines. Numbering 1–16 is consistent with the Table 1 of main text.
(DOCX)
Hydrogen bond interactions are highlighted with yellow color dotted lines. Numbering 1–11 is consistent with the Table 1 of main text.
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Green color bold sequence at 5`site (N-terminal) is representing XhoI restriction enzyme site, while maroon color bold sequence at 3`site (C-terminal) is representing HindIII restriction enzyme site.
(DOCX)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.