Abstract
Children with Reactive Attachment Disorder (RAD) have special educational needs that are challenging for teachers in early education. In the current contribution, we will discuss a large body of research suggesting that stimulating these children’s attachment development is feasible for teachers and potentially a successful strategy to ensure that these children thrive better in the classroom and socially. The current overview discusses research and theory on RAD and RAD treatment and results in the formulation of specific recommendations for the successful management of children with RAD in the classroom.
Keywords: attachment, treatment, teacher, dynamic model of the insecure cycle
Current Perspectives on the Management of Reactive Attachment Disorder in Early Education
Not many childhood mental health disorders have sparked more debate than Reactive Attachment Disorder1 (RAD). RAD refers to children’s difficulties with engaging in meaningful relationships with primary caregivers.2 While the DSM-IV distinguished two types of RAD, the inhibited and disinhibited type,3 the latter has been renamed in the DSM-5 as Disinhibited Social Engagement Disorder (DSED), and is no longer considered to be an attachment disorder.2 Therefore, in the current contribution, we will use the term RAD to refer to what was initially considered the inhibited subtype. According to the DSM 5, children have RAD if they show (A) a consistent pattern of inhibited, emotionally withdrawn behavior toward adult caregivers, manifested by both of the following: (1) The child rarely or minimally seeks comfort when distressed and (2) The child rarely or minimally responds to comfort when distressed. There should be (B) a persistent social or emotional disturbance characterized by at least two of the following: (1) Minimal social and emotional responsiveness to others; (2) Limited positive affect; (3) Episodes of unexplained irritability, sadness, or fearfulness that are evident even during non-threatening interactions with adult caregivers. In addition, (C), the child must have experienced a pattern of extremes of insufficient care as evidenced by at least one of the followings: (1) Social neglect or deprivation in the form of persistent lack of having basic emotional needs for comfort, stimulation, and affection met by caring adults; (2) Repeated changes of primary caregivers that limit opportunities to form stable attachments (eg, frequent changes in foster care); (3) Rearing in unusual settings that severely limit opportunities to form selective attachments (eg, institutions with high child to caregiver ratios). Also, (D) the care in Criterion C is presumed to be responsible for the disturbed behavior in Criterion A (eg, the disturbances in Criterion A began following the lack of adequate care) and, (E-G) the criteria are not met for autism spectrum disorder; the disturbance is evident before age 5 years and the child has a developmental age of at least nine months.
The fact that the definition and criteria changed substantially across different versions of the DSM illustrates that much is still unknown about the disorder and little is understood about the most adequate treatment strategies. As suggested by the name, children with RAD are considered to have disordered attachment development. This means that they either experienced traumatizing ruptures in their trust in the availability and support of their attachment figures due to maltreatment and neglect early in life, or never had the opportunity to develop attachment relationships at all (eg, in some institutionalized children). RAD symptoms can be clearly differentiated from symptoms of both internalizing and externalizing disorders in factor analysis4,5 and are associated with a wide range of co-occurring internalizing and externalizing diagnoses.4,6,7 Although RAD is, apparently, a rare condition in the community,8 a RAD diagnosis appears to be assigned substantially more often than can be expected from prevalence by professionals working with children in adoptive/foster placements. Aggressive behavior, in particular, seems to increase children’s risk of being overdiagnosed with RAD:9 once diagnosed, an overvalued link in professionals’ minds between RAD and aggression might prime teachers and other professional caregivers’ expectation that children with a RAD label are going to exhibit externalizing behavior that will be extremely difficult to manage.
Yet, we suspect RAD might also remain underidentified in early education settings, particularly in children who do not have severe externalizing problems.8 Despite the rarity of RAD in the general population, it is less rare in high-risk adolescents in social care10 and criminal justice settings.7 In these older populations a wide range of associated psychopathology, including aggression, is common.10 There have as yet been no population studies following up children diagnosed with RAD in early life, but a recent systematic review and case series of three boys with RAD that had persisted since early childhood suggested that withdrawn behavior and lack of comfort-seeking may not be noticed in the early years and that problems may not present until externalizing behaviors have emerged later in life.11
If children with RAD are not identified, this may be problematic, as they have specific interpersonal needs12 which, if unrecognized, could result in children not receiving the support they need resulting in children becoming stressed and even dysregulated in the classroom. This implies that children with RAD may not fulfill their educational potential and their dysregulation could impair both their own learning and that of their classmates and could lead to out-of-school placement. However, if teachers can be supported to meet the interpersonal needs of children with RAD, these children’s wellbeing and performance at school could improve.13 This is already important in early education when children are between birth and primary school age. Therefore, the current contribution aims to equip early education teachers with more confidence in understanding how RAD might manifest in the classroom and to propose strategies that could help to optimally manage these children. However, because research on the topic on early education and RAD is scarce, the current review will also take into account findings from research in older samples. Before moving on to give some specific recommendations on what teachers might do to support children with RAD in early education, we will address some controversies about RAD and the current state of the art.
Reactive Attachment Disorder and Attachment Theory
One of the major controversies related to the RAD diagnosis is the implied link to children’s attachment development. To date, this link remains difficult to establish empirically, which has raised the question what the exact nature of RAD might be.14,15 Because establishing the etiology of a disorder is critical to designing effective interventions, we will discuss attachment theory, research on the link between RAD and attachment, and provide an updated view on attachment development and links with the development of psychopathology from which we will derive concrete suggestions for the management of RAD in early education.
Attachment Theory
According to attachment theory, children are born with a behavioral system (the attachment system) that is activated during distress with the purpose of eliciting their primary caregivers’ support and protection to promote survival.16 Through the resulting care-related interactions, children establish an attachment relationship with these caregivers. According to attachment theory, such a relationship is characterized by mental representations that children develop about these caregivers (called internal working models; IWMs). The quality of these interactions determines whether IWMs are secure or insecure.16 Children who experience their caregivers as consistently available and supportive become securely attached, which means that they develop trust in their availability and more easily seek and benefit from support during new distressing experiences. Conversely, children who become insecurely attached have less trust in their caregiver’s availability. They either revert to more anxious (also called “anxious-ambivalent”) or to more avoidant interpersonal coping styles. Anxiously attached children continue to seek support in spite of their relative lack of trust. Consequently, they become preoccupied and angry with caregivers as they continue to fear and experience rejection. Avoidantly attached children no longer rely on the untrustworthy caregivers; however, they can only achieve this goal by suppressing negative emotions and avoiding situations that elicit such emotions.17 Finally, some children show a disorganized attachment.18 These children appear insecurely attached but fail to organize their behavior in either an avoidant or an anxious way. They display intense fear for the caregiver combined with stereotypic, asymmetric, misdirected, or jerky movements; or freezing and apparent dissociation.19 These behaviors suggest “motivational conflict”, ie, they do not know whether to approach or avoid the caregiver.20
The caregivers about whom children develop such IWMs are typically parents, but any caregiver (eg, adoptive parents, foster parents, extended family members) can become an attachment figure depending on the emotional relevance of the relationship and the duration of the relationship. Bowlby suggested that IWMs could remain open for updating throughout life, yet for many years the general assumption was that attachment IWMs developed during the first three years of life and then remained a stable construct throughout life.21 However, the latter assumption has found very mixed support,22 suggesting that subsequent experiences still have significant impact on children’s attachment development.23 This observation is also true for children who developed in extremely adversive relational circumstances early in life. Adoption research shows that after adoption, attachment development significantly catches-up and differences with never-adopted peers appear small to non-existent a few years after adoption into more caring environments.24 Hence, changing the quality of children’s caregiving environment remains relevant throughout life and teachers can play an important role to further stimulate insecurely attached children’s catch-up.25
Teacher–Child Relationships and Attachment
Scholars have argued that although most teacher–child relationships cannot be considered full-fledged attachment bonds, teacher–child relationships generally do have an attachment component, especially in early education.26 When entering school, for instance, kindergartners have been found to show high security seeking behavior with their teacher, which sharply decreases later on.27 These and other findings have led attachment researchers to conclude that, especially for young children, teachers can be considered temporary or ad hoc attachment figures, that may serve as a secure base and safe haven for children at school26,28.
Consistent with expectations from attachment theory, research has also revealed that children with secure parent–child attachments tend to be better equipped to maintain a smooth balance between seeking support and independent exploration from teachers.29 Studies showed, for instance, that teachers reported less close and warm relationships with children who were less securely attached to their mother.30,31 Also, less securely attached children have been found to show more overdependent behavior toward their kindergarten teacher, indicating a lack of secure base use of the teacher.29
Teacher–child relationships of children with RAD have been studied far less. Given their consistent pattern of inhibited, emotionally withdrawn behavior toward adult caregivers, and the persistent social or emotional disturbances, children with RAD will most likely have even more problems in forming high-quality affective relationship with their teacher than children who are insecurely attached. In support of that assumption, Bosmans and colleagues found that, compared with other children with severe behavioral and emotional disorders, children with symptoms of RAD showed less trust in their teachers.32 This was evidenced both in their observed behavior toward the teacher and in their representations of the relationship.
In sum, the limited available research suggests that children with RAD are at risk for developing relationship problems with teachers. This is worrisome, as research indicates that teacher–child relationship problems tend to increase children’s initial emotional and behavioral problems, thus installing a negative vicious cycle.33,34 It is important that teachers are aware of this risk, and their potential role in maintaining or enhancing these problems.
Search for a Link Between Attachment and Reactive Attachment Disorder
In spite of the straightforward prediction that attachment disordered children should have insecure IWMs, this association has proven surprisingly difficult to establish. Studies conducted in the DSM-IV era (when RAD was one subtype of the disorder next what is now described as DSED), showed that insecure attachment was neither necessary nor sufficient for RAD/DSED.35,36 In the Bucharest Early Intervention Study, there was a modest correlation between a continuous measure of attachment security and what we would now call RAD.36 A lack of – or reduction in – attachment behavior (ie, failure to seek or accept comfort) is the core of Criterion A in the DSM 5 classification of RAD, so, although it is now accepted that abnormalities in the attachment system are necessary for a diagnosis of RAD, it appears that attachment abnormalities cannot be sufficient for RAD to develop.37 Minnis and colleagues argued that the fundamental problem in RAD might be one of “intersubjectivity”, the broad process whereby infant development is “supported by the intuitive responses of parents and other human companions”38 - and that problems with attachment might be one of a range of downstream processes affected by this broader problem.39 Rutter suggested that RAD symptoms reflect general emotional and behavioral dysregulation instead of the unique dysregulation of children’s attachment system.40 Other scholars found that RAD symptoms reflect hyperarousal linked to post traumatic stress disorder (PTSD) or similar anxiety-related disorders.41–44 In a study of young people in foster care, Lehman and colleagues found that RAD Criterion A (failure to seek and accept comfort) and RAD Criterion B (social or emotional disturbance including unexplained irritability, sadness or fearfulness) were distinct in factor analysis.43 Only Criterion B was associated with traumatic events suggesting that, while Criterion A is attachment-related, Criterion B might have an aetiological link with PTSD.43 Finally, research suggests that, alongside maltreatment, the child’s genetics is an important element in the aetiology of RAD.5 Heritable neurodevelopmental factors have been suggested as potentially increasing the risk of RAD developing in the context of maltreatment.11 Taken together, RAD symptoms seem not solely be attachment-related, but seem to result from a complex interplay between environmental (maltreatment), relational (including attachment and broader intersubjective processes) and child (genetic, temperamental) factors.
The Dynamic Model of the Insecure Cycle
Understanding the role of attachment in the development (and treatment) of RAD requires understanding how attachment develops. This has long been poorly understood due to the vagueness of the theory.45,46 Of relevance is a recent theory suggesting that attachment development can be understood as the result of a social learning process.47 Specifically, although the attachment system is innate and requires no learning,16 this theory proposes that the development of differences in (in)secure attachment occurs according to the principles of safety conditioning. For a thorough introduction to this Learning Theory of Attachment or LTA, see Appendix 1. In short, children’s view of primary caregivers seems to shift as the result of safety conditioning. Safety conditioning occurs over single learning events – events during which the child’s distress is followed by caregivers’ comfort. Comfort positively affects children’s endocrinological systems. For example, cortisol levels decrease resulting in a sense of relief, oxytocin levels increase resulting a sense of safety and care, and dopamine levels increase which has a reinforcing effect. Such learning trials result in secure state attachment: children feel, in the moment, that they can trust in their caregivers’ support. In a similar vein, Bosmans and colleagues have argued that children’s attachment behavior develops through operant conditioning and the same reinforcing stimuli.47
This LTA implies that attachment should not be merely considered a stable trait that develops early in life and remains largely unchanged throughout life. Instead, attachment consists of both trait- and state-like components. State attachment responds dynamically to changes in the context. Repeatedly activated attachment states that contradict expectations at trait level can eventually result in shifts at trait level.48 This way, the LTA explicitly proposes a potential mechanism for previous findings regarding the limited stability of attachment over time22 and is also in line with observations in adoption studies showing post-adoption catch-up after exposure to adverse caregiver environments early in life.24
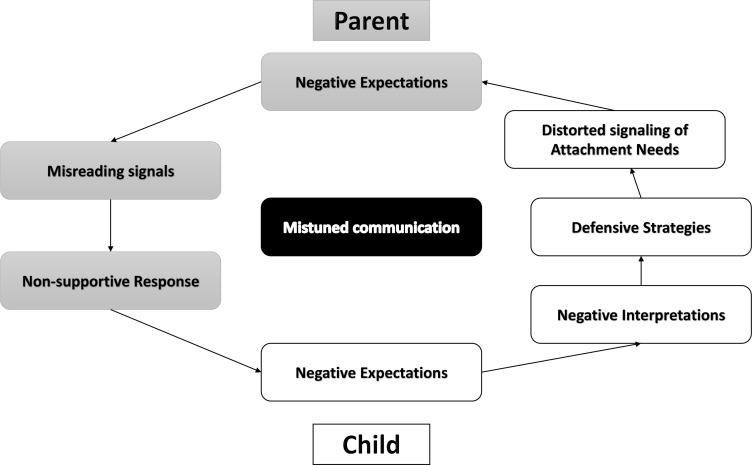
The LTA further suggests that every singular support-related interaction is relevant to understanding children’s attachment development. To understand the relational dynamics during these singular interactions that eventually foster insecure attachment, Kobak and Bosmans proposed the dynamic model of the insecure cycle49 (Figure 1). This model builds on the evolutionary theory that all children are born with an innate system that activates the need to be cared for during distress (the attachment system) and that all parents have an innate desire to be a loved and competent caregiver of their children (the caregiving system).16,47 Further, this model builds on learning research showing that what is once learned, can never be unlearned.50,51 At best, these memories can be deactivated and replaced by novel knowledge until the moment that the old knowledge gets reactivated by related contextual cues.52 Because all children are assumed to have a relational learning history that by definition entails both positive and negative attachment-related learning experiences, current interpersonal interactions can activate (or “prime”) both positive and negative attachment memories and associated states.47
Figure 1.
The dynamic model of the insecure cycle applied to the parent–child relationship.
Kobak and Bosmans argued that a learning event elicits an insecure cycle if a child signals distress to a parent and has the experience that the parent’s response is mistuned (mistuned communication).49 This primes or activates negative memories about past relational disappointments, which results in more negative expectations about the parent’s ability to sensitively respond to the child’s basic need for care during distress. The resulting reduction in state trust negatively affects how children interpret their parent’s behavior. Thus, in spite of their need of support, they will mainly experience the expectation or fear that their need will be frustrated and/or that they will be hurt by the parent. To protect themselves against this anticipated frustration or pain, children rely on defensive strategies. Concretely, instead of support-seeking behavior, they will rely on more anxious or more avoidant interpersonal coping strategies. As a result, they display anxious/angry or avoidant behaviors – or a mixture of both - which in reality are distorted signals of their underlying attachment needs.
In turn (again Figure 1), these behaviors prime the parents’ own negative experiences related to feeling rejected, which activates negative expectations about the child (eg, my child sees me as a failing parent, my child does not love me). They only see their child’s apparently unloving or negative behavior and not the child’s underlying fear or frustrated expectations. As a result, the parents misread the child’s distorted signaling of their attachment needs: they see the behavior as inappropriate behavior that needs to be stopped as soon as possible. These attempts to stop the child’s distorted signals can result in parental responses which child will again will experience as non-supportive. As a result, the parental responses strengthen the child’s negative experiences which further intensify the insecure cycle leading to the development of trait-like insecure attachment.
Attachment and the Development of Psychopathology
An increasing number of meta-analyses has shown that an association exists between insecure attachment and internalizing and externalizing psychopathology, but that this association is rather modest.53,54 Hence, there is a growing recognition that not all insecurely attached children develop psychopathology. Instead, research shows that secure attachment increases children’s resilience against the development of psychopathology,55 while insecure attachment interferes with support seeking during distress and receiving comfort and care to help cope with distress. This, in turn, increases their risk of developing psychopathology, but does not make this inevitable.56 This aligns with predictions from the LTA on the insecure cycle: the more children rely on distorted signaling of their attachment needs, the more they become vulnerable to develop psychopathology as the resulting interaction deprives them from the support they need to be protected against the impairing effects of distress – but future, repeated, singular support-related interactions in which parental responses are more optimal can gradually shift the developmental trajectory towards one in which the child once again builds trust in the parent.57
Thus, although the direct links between insecure attachment and psychopathology are weak, insecure attachment remains a transdiagnostic risk factor for several disorders. Specifically, insecure attachment aggravates the effects of environment, and of child-related risk factors, on the development of child psychopathology. Specifically, if insecurely attached children experience distress, they are at higher risk of developing emotional and behavioral problems because these children engage in distorted attachment behaviors that missignal their attachment needs – and their parents are likely to respond in a less than optimal manner. These repeatedly sub-optimal support-related interactions mean that the child’s ongoing distress is more likely to elicit psychopathology.56,58,59 Research suggests that individuals vulnerable to developing severe psychopathologies like psychosis have less severe psychotic symptoms if they are more securely attached.60,61 Again, this is likely explained by lack of (perceived) support during the regulation of distress which leads to enhanced expression of psychopathology symptoms.62
Revisiting the Association Between Attachment and RAD
Because the RAD literature suggests that insecure attachment is not necessarily the defining characteristic of RAD, and because the attachment literature suggests that children develop psychopathology if their distorted attachment needs-signals deprive them from the care they need to cope adequately with distress, we propose an alternative role for attachment in RAD. Specifically, we argue that RAD development is precipitated by a cascade of genetically inherited child traits and severe deprivation and/or traumatizing events. The extent to which these children, in addition, develop attachment (in)security with primary and ad-hoc caregivers will subsequently determine the effects of their RAD symptoms. This hypothesis was directly tested by Cuyvers and colleagues who found that children with more RAD symptoms displayed more prosocial behavior if they were more securely attached, suggesting that attachment (in)security modulates the severity of RAD-related outcomes.62 To summarise this developmental cascade, children with (a) particular heritable temperamental traits who have also (b) experienced extremes of parenting characterized by repeated single learning events that are either frustrating (in the case of neglect) or frightening/hurtful (in the case of abuse) are likely to have developed (c) an entrenched lack of trust that manifests in a marked reduction in comfort-seeking and comfort-acceptance. As Prior and Glaser noted, this is essentially a turning off of the attachment system with inevitably dire developmental consequences, since babies and young children need to have their attachment needs recognized and addressed in order to survive and thrive.63
Relevant for the current review is that the dynamic nature of this cascade might mean that children with RAD can benefit from relationships that nurture secure attachment IWMs. This more process-based understanding of the mechanisms underlying the development of RAD provides a promising avenue for the successful management of these children in the classroom.
Managing RAD in Early Education
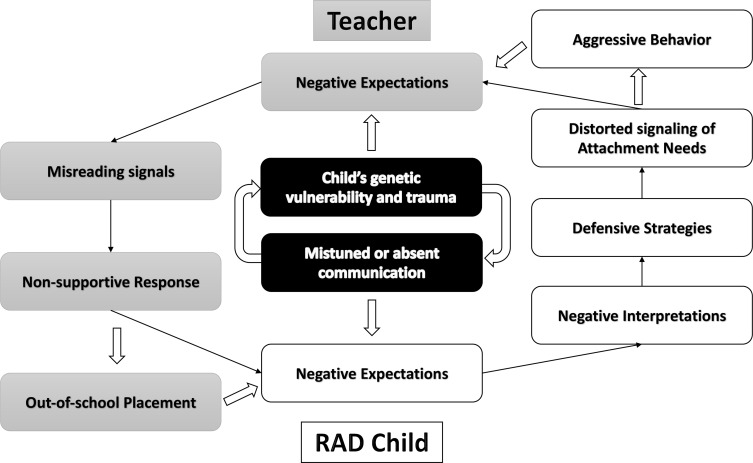
The observation that even after severe deprivation insecurely attached children catch-up in their attachment development when their parenting environment becomes safer and more supportive,24 suggests that even children with RAD will benefit significantly from supportive interpersonal relationships in the classroom. However, managing children with RAD in early education is a challenging endeavor.64 When teachers report children to show more inhibited RAD symptoms they also report more internalizing and externalizing problem behavior.64 According to the dynamic model of the insecure cycle, these behaviors reflect children’s distorted signals about their need for support. These missignals have the potential to come across just as intrusive for ad hoc attachment figures (ie, teachers) as they are for attachment figures. Thus, these missignals in RAD likely set off insecure cycles in the teacher–child relationship. These cycles risk eventually culminating in out-of-school placement which imply physical ruptures from ad hoc attachment figures (see Figure 2).
Figure 2.
THe dynamic model of the insecure cycle applied to the teacher – RAD child relationship.
Specifically, inhibited RAD children have been observed to appear initially problem free in the classroom as they typically make few demands. However, since these children do not seek help when feeling distressed, at the point that their stress becomes overwhelming they might either “boil over” and burst into aggressive behavior or become even more withdrawn or frozen. It is easy to see how aggressive responses can elicit insecure attachment cycles, but withdrawn or frozen responses to stress can also set off these insecure cycles whereby such child behavior can stimulate teachers to try even harder to stimulate the child’s social participation. Because, in healthy attachment cycles, it is the child’s communicative lead that ordinarily elicits the communication,56 the teacher’s efforts to lead the communication might be perceived by the child as intrusive. This well-intentioned teacher behavior is likely to activate or increase the child’s negative expectations about support, setting off an insecure cycle that stimulates the child to further shield him/herself from the teacher.65 Both aggressive and shielding behaviors can, in turn, activate pain and disappointment in the teacher who might start responding more harshly or who might withdraw from communication. The more these cycles stimulate teachers to interpret a RAD child’s observable behaviors as rejection, the more the teacher can develop the idea that these children either do not fit in the classroom, or that these children would thrive better in the hands of more competent teachers or school-settings. Although these decisions are taken in the best interests of the child, they lead to physical ruptures with (ad hoc) attachment figures that further nurture these children’s negative expectations about the availability of support and the untrustworthiness of adults.
Indeed, it is well described that children with RAD often experience a cascade of ruptures as they are often removed from, for example, schools, families, institutions, foster families because of escalating social, oppositional, and behavioral problems, or because putative attachment figures feel a sense of failure in being unable to achieve emotional intimacy with the child. Children’s bodies are evolutionarily equipped with biological systems that flag any imminent danger to survival. For children, separation from even insensitive (ad hoc) attachment figures signifies a new aversive event – contradicting the idea that out-of-school placement is in the best interest of the child. In the context of each new disappointment, the attachment system gets hyperactivated in order to repair the rupture and find safety again. If this again increases children’s defensive strategies and distorted signaling (they will want to avoid re-experiencing this much pain), an out-of-school placement will only set off new insecure cycles with the new caregivers which jeopardizes the development of these novel relationships.
How to Restore or Strengthen Attachment Relationships?
This raises the question of what is known about strategies that can be successfully employed to interrupt insecure cycles, to avoid physical ruptures, and to restore trust. An increasing number of clinical interventions have begun to demonstrate improvements in relationships between attachment figures (mostly parents) and children displaying severely disrupted behavior. Although many programmes still lack robust randomized controlled trial evidence,66 literature suggests that potentially effective strategies might differ in congruence with the age of the children, implying the need for different, age-specific intervention programs (eg, Video-feedback Intervention to promote Positive Parenting and Sensitive Discipline, VIPP-SD;67 Middle Childhood Attachment-focused Therapy;68 Attachment-based Family Therapy69). However, what all these programs share is that they aim to help caregivers recognize and understand that the child is missignaling their underlying attachment needs and that it is critical that parental responses to these missignals do not simply entail direct responses to these missignals (eg, using reward/punishment systems or setting clear rules and limits), but also entail attachment-focussed responses. According to these programs, purely pedagogical strategies remain important in direct response to children’s transgressions but, at the same time, these programs aim to support parents in also responding to the underlying dynamic insecure cycle. Subsequently, they learn to provide support to these underlying attachment needs and to children’s related fears.
Experience with two interventions supports the idea that such an approach is even helpful for children with RAD. First, the Attachment and Biobehavioral Catch-up (ABC) intervention70 helps caregivers look beyond the observable (missignaling) behavior of the child, helps attachment figures develop strategies aimed to override their automatic responses to children’s missignals, and stimulates parents to respond to children’s basic needs. Dozier makes the case that, for traumatized children to catch-up attachment learning, caregivers should not merely follow children’s limits, but should be “gently challenging”65 This advice is in line with learning and attachment research that shows that information processing biases decrease the likelihood that incongruent information (eg, the parent responding more sensitively to the child) is noticed and thus allows children to update their attachment-related expectations.57 In other words, children should be able to notice that something happens that goes beyond their expectations. This gentle challenge differs from intrusive interventions like holding therapy (which means that therapists or parents firmly hold or lay upon aggressive or dysregulated children until they regain their calm). The latter is typically described as “attachment therapy”, but should not be used in the treatment of RAD as holding has resulted in the death of six children.12 Further supporting the adequacy of this approach is research that shows that it improves children’s attachment and decreases their behavior problems.71
Second, Dyadic Developmental Psychotherapy72 was developed to improve attachment relationships in children that experienced trauma in early caregiving environments.73 Although not as extensively studied as ABC, preliminary data suggest that helping children to express their negative relational experiences with caregivers in a safe and controlled way might be a valuable strategy for restoring children’s trust in the caregiver - and a randomized controlled trial is underway (ClinicalTrials.gov Identifier: NCT04187911). Third, a good example of attempts to incorporate both attachment and social learning concepts into a single therapeutic intervention is VIPP-SD,67 which, as a treatment for RAD, is also currently undergoing a randomized controlled trial.74
Towards an Attachment-Sensitive Management of RAD Children in Early Education
The present overview leads to concrete recommendations that can be incorporated in teachers’ management of RAD children in early education. Despite the continuity of relationship problems between the home and school environment, research also indicates that teachers can break this continuity. Buyse, Verschueren and Doumen, for instance, found that when teachers showed high sensitivity in class, being responsive to the children’s needs and providing reassurance and encouragement, less securely attached children were no longer at risk for developing a less close relationship with their teacher.25 Moreover, this higher teacher-child closeness protected less securely attached children from showing aggressive behavior.
In the case of children with RAD, it will undoubtedly be more challenging for teachers to compensate for a lack of adequate parental care because these children’s lack of trust will be more entrenched. However, compared to children who simply have insecure attachment, children with RAD will undoubtedly reap even greater benefits from developing a positive attachment relationship with a teacher. Even for children with RAD, promising indications for teachers’ buffering role have been found. A study by Spilt and colleagues showed that children with RAD symptoms showed more overt and relational aggression, but only when teacher sensitivity was low.13 With highly sensitive teachers, levels of aggression were found to decrease. As of yet, it is unclear if these buffering effects extend over school years and contexts. However, case reports suggest that even singular experiences with highly sensitive teachers can make a difference for (some) children later in life.75 Thus, the limited available evidence suggests that for children with RAD, sensitivity of teachers could be a key protective strategy that might help these children find a more positive developmental trajectory.
To date, there is a substantial gap in the literature and research concerning interventions that aim to improve relationships between teachers and children with RAD in early education. However, the current literature review provides promising leads towards the development of interventions that target to increase teacher sensitivity to provide a nurturing context for children with RAD. Specifically, teacher sensitivity implies that teachers are aware of and responsive to the emotional and relational needs of children. And these needs may differ considerably. Some children may need physical comfort from their teacher, whereas other children may prefer more subtle signs of being available, providing time and space when they need it.
With regard to recognizing the attachment needs and related fears of children with RAD, teachers will likely struggle to recognize that the child’s tendency to make few demands is actually a manifestation of missignaled attachment needs. Accurately recognizing and understanding RAD-related missignals is challenging because these children largely express their attachment needs through absent behavior. Absent support seeking, absent social and emotional responsiveness to others, or absent positive affect do not tend to draw teachers’ attention. Instead teachers are more aware of, or more directly triggered by, children’s unexplained irritability.76 Yet the “boiling over” externalizing behavior that can occur in some children with RAD is also unlikely to be recognized by teachers as a manifestation of attachment-related processes. Raising teachers’ awareness that children have an innate desire for care during distress can help teachers understand that low demandingness, being distant and frozen, or being just irritated and aggressive during distress are behaviors that can reflect a distorted signaling of attachment needs. Such a better understanding of the insecure cycle can stimulate teachers to employ strategies that offer a more sensitive or gently challenging response to these children’s underlying needs, instead of relying solely on children’s overt behavior (which then sets off new/reinforces existing insecure cycles).
With regard to stimulating teachers’ responsive reactions to RAD children’s needs, interventions have been developed to improve teacher sensitivity. Examples are Banking Time,77 Teacher–Child Interaction Theory,78 and Playing-2-Gether.79 In these interventions, teachers are trained to observe the child, follow the child’s lead, narrate his or her actions and label his or her feelings, thus conveying acceptance and sensitivity.79,80 Although these interventions have shown positive effects on the behavior and teacher–child relationship quality of at-risk children, their effectiveness among children with RAD needs to be examined.
Modifications, perhaps involving gentle challenge, may be necessary in order for these promising interventions to be effective for children with RAD, especially if the child’s attachment signals are absent or much reduced. Building on the components of the abovementioned attachment-focused interventions for severely deprived and/or traumatized children, one may assume that merely avoiding challenging the child’s fears of rejection will be insufficient to interrupt the entrenched pattern of repeated insecure attachment cycles that have developed in RAD. Instead, if ad hoc attachment relationships between teachers and children RAD are to be restored or strengthened, then training teachers to gently challenge these children’s defensive strategies is likely to be necessary. Specifically, if a teacher has a good understanding that this child has a signalling problem, it seems reasonable to assume that there is potential for the teacher to set off an alternative, more secure, attachment cycle. This could be achieved when the teacher persists with gentle challenge and gradually gets a positive attachment-cycle going as the child experiences the behavioral rewards that result from signalling their needs65 and, eventually, begins to develop a positive safety conditioning cycle as the child gradually develops trust in the teacher. Also, interventions that support teachers’ reflection on the relationship with a particular child and their related feelings may prove helpful in improving teachers’ sensitivity.13
A Research Agenda for the Optimal Management of RAD in Early Education
Given the importance of the teacher–child relationship as a protective factor in RAD children’s development, it is important to understand how this relationship unfolds and can be stimulated. The current literature review can be a valuable step towards the development of a relevant intervention, but much more research is needed before we can formulate evidence-based direct recommendations for teachers in early education. More research is needed on the characteristics of a positive relationship between teachers and RAD children. More research is needed on the extent to which the dynamic model of the insecure attachment cycle applies to the development of children’s attachment relationship with their teachers in the context of RAD. Finally, more research is needed on the extent to which gently challenging a child’s RAD symptoms is a promising avenue towards strengthening their relationship with the teacher.
For now, the current literature review suggests that increasing teacher sensitivity and encouraging/training teachers in gentle challenge, according to the insights of the insecure cycle, is unlikely to be harmful for any child and promises to be beneficial for children with RAD. This strategy could serve to maintain/build relationships, protect children from school-ruptures and therefore help restore children’s social and emotional resilience.
Acknowledgment
The authors are grateful to the FWO and KU Leuven for the support (grants G075718N; G049419N; C14/16/040) of the research that has allowed writing this literature review.
Disclosure
The authors report no conflicts of interest for this work.
References
- 1.Allen B. A radical idea: a call to eliminate “Attachment Disorder” and “Attachment Therapy” from the clinical lexicon. Evid-Based Pract Child Adolesc Mental Health. 2016;1(1):60–71. doi: 10.1080/23794925.2016.1172945 [DOI] [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC; 2013. [Google Scholar]
- 3.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC; 2000. [Google Scholar]
- 4.Lehmann S, Breivik K, Heiervang ER, Havik T, Havik OE. Reactive attachment disorder and disinhibited social engagement disorder in school-aged foster children - a confirmatory approach to dimensional measures. J Abnorm Child Psychol. 2016;44:445–457. doi: 10.1007/s10802-015-0045-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Minnis H, Reekie J, Young D, et al. Genetic, environmental and gender influences on attachment disorder behaviours. Br J Psychiatry. 2007;190:490–495. [DOI] [PubMed] [Google Scholar]
- 6.Atkinson L. Reactive attachment disorder and attachment theory from infancy to adolescence: review, integration, and expansion. Attach Hum Dev. 2019;21(2):205–217. doi: 10.1080/14616734.2018.1499214 [DOI] [PubMed] [Google Scholar]
- 7.Moran K, McDonald J, Jackson A, Turnbull S, Minnis H. A study of attachment disorders in young offenders attending specialist services. Child Abuse Negl. 2017;65:77–87. doi: 10.1016/j.chiabu.2017.01.009 [DOI] [PubMed] [Google Scholar]
- 8.Minnis H, Macmillan S, Pritchett R, et al. Prevalence of reactive attachment disorder in a deprived population. Br J Psychiatry. 2013;202(5):342–346. doi: 10.1192/bjp.bp.112.114074 [DOI] [PubMed] [Google Scholar]
- 9.Allen B, Schuengel C. Attachment disorders diagnosed by community practitioners: a replication and extension. Child Adolesc Ment Health. 2020;25:4–10. doi: 10.1111/camh.12338 [DOI] [PubMed] [Google Scholar]
- 10.Kay C, Green J. Reactive attachment disorder following early maltreatment: systematic evidence beyond the institution. J Abnorm Child Psychol. 2013;41:571–581. doi: 10.1007/s10802-012-9705-9 [DOI] [PubMed] [Google Scholar]
- 11.Nelson R, Chadwick G, Bruce M. Can reactive attachment disorder persist in nurturing placements? A systematic review and clinical case series. Developmental Child Welfare. 2020;2(2):110–131. doi: 10.1177/2516103220940326 [DOI] [Google Scholar]
- 12.Zeanah CH, Chesher T, Boris NW. American academy of child and adolescent psychiatry (AACAP) committee on quality issues (CQI). Practice parameter for the assessment and treatment of children and adolescents with reactive attachment disorder and disinhibited social engagement disorder. J Am Acad Child Adolesc Psychiatry. 2016;55(11):990–1003. doi: 10.1016/j.jaac.2016.08.004 [DOI] [PubMed] [Google Scholar]
- 13.Spilt JL, Vervoort E, Koenen A, Bosmans G, Verschueren K. The socio-behavioral development of children with symptoms of attachment disorder: an observational study of teacher sensitivity in special education. Res Dev Disabil. 2016;56:71–82. doi: 10.1016/j.ridd.2016.05.014 [DOI] [PubMed] [Google Scholar]
- 14.Zilberstein K. Reactive attachment disorder In: Levesque R, editor. Encyclopedia of Adolescence. Cham: Springer; 2016. [Google Scholar]
- 15.Zimmermann P, Soares I. Recent contributions for understanding inhibited reactive attachment disorder. Attach Hum Dev. 2019;21(2):87–94. doi: 10.1080/14616734.2018.1499207 [DOI] [PubMed] [Google Scholar]
- 16.Bowlby J. Attachment and loss In: Basic Books Vol. 3 New York; 1969. [Google Scholar]
- 17.Cassidy J. The nature of the child’s ties In: Cassidy J, Shaver PR, editors. Handbook of Attachment: Theory, Research, and Clinical Applications. 2nd ed. New York: The Guilford Press; 2008. [Google Scholar]
- 18.Main M, Solomon J. Discovery of an insecure–disorganized/disoriented attachment pattern In: Affective Development in Infancy. West-port, CT: Ablex; 1986:95–124. [Google Scholar]
- 19.Duschinsky R. The emergence of the disorganized/disoriented (D) attachment classification, 1979–1982. Hist Psychol. 2015;18(1):32–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reisz S, Duschinsky R, Siegel DJ. Disorganized attachment and defense: exploring John Bowlby’s unpublished reflections. Attach Hum Dev. 2018;20(2):107–134. doi: 10.1080/14616734.2017.1380055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grossmann KE, Grossmann K, Waters E, eds. Attachment from Infancy to Adulthood: The Major Longitudinal Studies. Guilford Press; 2005. [Google Scholar]
- 22.Pinquart M, Feußner C, Ahnert L. Meta-analytic evidence for stability in attachments from infancy to early adulthood. Attach Hum Dev. 2013;15:189–218. doi: 10.1080/14616734.2013.746257 [DOI] [PubMed] [Google Scholar]
- 23.Waters TEA, Facompré CR, Dujardin A, et al. Taxometric analysis of secure base script knowledge in middle childhood reveals categorical latent structure. Child Dev. 2019;90:694–707. doi: 10.1111/cdev.13229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Finet C, Vermeer HJ, Juffer F, Bijttebier P, Bosmans G. Remarkable cognitive catch-up in Chinese Adoptees nine years after adoption. J Appl Dev Psychol. 2019;65:1010–1071. doi: 10.1016/j.appdev.2019.101071 [DOI] [Google Scholar]
- 25.Buyse E, Verschueren K, Doumen S. Preschoolers’ attachment to mother and risk for adjustment problems in kindergarten: can teachers make a difference? Soc Dev. 2011;20(1):33–50. [Google Scholar]
- 26.Verschueren K, Koomen HM. Teacher-child relationships from an attachment perspective. Attach Hum Dev. 2012;14(3):205–211. doi: 10.1080/14616734.2012.672260 [DOI] [PubMed] [Google Scholar]
- 27.Koomen HMY, Hoeksma JB. Regulation of emotional security by children after entry to special and regular kindergarten classes. Psychol Rep. 2003;93:1319–1334. doi: 10.2466/pr0.2003.93.3f.1319 [DOI] [PubMed] [Google Scholar]
- 28.Zajac K, Kobak R. Attachment In: Bear GG, Minke KM, editors. Children’s Needs III: Development, Prevention and Intervention. Washington, DC: National Association of School Psychologists; 2006:379–389. [Google Scholar]
- 29.Verschueren K, Spilt JL. Understanding the origins of child-teacher dependency: mother-child attachment security and temperamental inhibition as antecedents. Attach Hum Dev. 2020;1–19. doi: 10.1080/14616734.2020.1751988 [DOI] [PubMed] [Google Scholar]
- 30.O’Connor E, McCartney K. Attachment and cognitive skills: an investigation of mediating mechanisms. J Appl Dev Psychol. 2007;28:458–476. [Google Scholar]
- 31.Sabol TJ, Pianta RC. Recent trends in research on teacher–child relationships. Attach Hum Dev. 2012;14(3):213–231. doi: 10.1080/14616734.2012.672262 [DOI] [PubMed] [Google Scholar]
- 32.Bosmans G. The link between middle childhood attachment and late adolescent early maladaptive schemas. 2020.
- 33.Doumen S, Verschueren K, Buyse E, Germeijs V, Luyckx K, Soenens B. Reciprocal relations between teacher-child conflict and aggressive behavior in kindergarten: a three-wave longitudinal study. J Clin Child Adolesc Psychology. 2008;37:588–599. doi: 10.1080/15374410802148079 [DOI] [PubMed] [Google Scholar]
- 34.Roorda DL, Verschueren K, Vancraeyveldt C, Van Craeyevelt S, Colpin H. Teacher-child relationships and behavioral adjustment: transactional links for preschool boys at risk. J Sch Psychol. 2014;52:495–510. doi: 10.1016/j.jsp.2014.06.004 [DOI] [PubMed] [Google Scholar]
- 35.Minnis H, Green J, O’Connor TG, et al. An exploratory study of the association between reactive attachment disorder and attachment narratives in early school-age children. J Child Psychol Psychiatry. 2009;50(8):931–942. doi: 10.1111/j.1469-7610.2009.02075.x [DOI] [PubMed] [Google Scholar]
- 36.Zeanah CH, Smyke AT, Koga SF, Carlson E; Bucharest Early Intervention Project Core Group. Attachment in institutionalized and community children in Romania. Child Dev. 2005;76(5):1015–1028. doi: 10.1111/j.1467-8624.2005.00894.x [DOI] [PubMed] [Google Scholar]
- 37.Zeanah CH, Gleason MM. Annual research review: attachment disorders in early childhood-clinical presentation, causes, correlates, and treatment. J Child Psychol Psychiatry. 2015;56:207–222. doi: 10.1111/jcpp.12347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Trevarthen C, Aitkin KJ. Infant intersubjectivity: research, theory, and clinical applications. J Child Psychol Psychiatry. 2001;42:3–48. doi: 10.1111/1469-7610.00701 [DOI] [PubMed] [Google Scholar]
- 39.Minnis H, Everett K, Pelosi AJ, Dunn J, Knapp M. Children in foster care: mental health, service use and costs. Eur Child Adolesc Psychiatry. 2006;15:336–342. doi: 10.1007/s00787-006-0539-2 [DOI] [PubMed] [Google Scholar]
- 40.Rutter M, Kreppner J, Sonuga-Barke E. Emanuel Miller Lecture: attachment insecurity, disinhibited attachment, and attachment disorders: where do research findings leave the concepts? J Child Psychol Psychiatry. 2009;50:529–543. [DOI] [PubMed] [Google Scholar]
- 41.Bakermans-Kranenburg MJ, Steele H, Zeanah CH, et al. Attachment and emotional development in institutional care: characteristics and catch-up. Monogr Soc Res Child Dev. 2011;76:62–91. doi: 10.1111/j.1540-5834.2011.00628.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hinshaw‐Fuselier S, Boris NW, Zeanah CH. Reactive attachment disorder in maltreated twins [Special issue]. Infant Ment Health J. 1999;20:42–59. [Google Scholar]
- 43.Lehmann S, Breivik K, Monette S, Minnis H. Potentially trau- matic events in foster youth, and association with DSM-5 trauma- and stressor related symptoms. Child Abuse Negl. 2020;101:1043–1074. doi: 10.1016/j.chiabu.2020.104374 [DOI] [PubMed] [Google Scholar]
- 44.O’Connor MJ, Kogan N, Findley R. Prenatal alcohol exposure and attachment behavior in children. Alcoholism: Clin Exp Res. 2002;26:1592–1602. doi: 10.1111/j.1530-0277.2002.tb02460.x [DOI] [PubMed] [Google Scholar]
- 45.Rutter M. Commentary: attachment is a biological concept - a reflection on Fearon et al. (2014). J Child Psychol Psychiatry. 2014;55:1042–1043. doi: 10.1111/jcpp.12301 [DOI] [PubMed] [Google Scholar]
- 46.Thompson RA. Early attachment and later development: reframing the questions In: Cassidy J, Shaver PR, editors. Handbook of Attachment: Theory, Research and Clinical Applications. 3rd ed. New York, NY: The Guilford Press; 2016:330–348. [Google Scholar]
- 47.Bosmans G, Bakermans-Kranenburg MJ, Vervliet B, Verhees MWFT, van IJzendoorn MH. A learning theory of attachment: unraveling the black box of attachment development. Neurosci Biobehav Rev. 2020;113:287–298. doi: 10.1016/j.neubiorev.2020.03.014 [DOI] [PubMed] [Google Scholar]
- 48.Fraley C, Hudson NW. The development of attachment styles In: Personality Development Across the Lifespan. Academic Press; 2017:275–292. [Google Scholar]
- 49.Kobak R, Bosmans G. Attachment and psychopathology: a dynamic model of the insecure cycle. Curr Opin Psychol. 2019;25:76–80. doi: 10.1016/j.copsyc.2018.02.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bouton ME. A learning theory perspective on lapse, relapse, and the maintenance of behavior change. Health Psychol. 2000;19:57–63. doi: 10.1037/0278-6133.19.Suppl1.57 [DOI] [PubMed] [Google Scholar]
- 51.Uner O, Roediger HL. Are encoding/retrieval interactions in recall driven by remembering, knowing, or both? J Mem Lang. 2018;103:44–57. doi: 10.1016/j.jml.2018.07.002 [DOI] [Google Scholar]
- 52.Tulving E. Cue-dependent forgetting. Am Sci. 1974;62:74–82. [Google Scholar]
- 53.Fearon RP, Bakermans-Kranenburg MJ, Van Ijzendoorn MH, Lapsley A, Roisman GI. The significance of insecure attachment and disorganization in the development of children’s externalizing behavior: a meta‐analytic study. Child Dev. 2010;81:435–456. doi: 10.1111/j.1467-8624.2009.01405.x [DOI] [PubMed] [Google Scholar]
- 54.Madigan S, Brumariu LE, Villani V, Atkinson L, Lyons-Ruth K. Representational and questionnaire measures of attachment: A meta-analysis of relations to child internalizing and externalizing problems. Psychol Bull. 2016;142(4):367–399. doi: 10.1037/bul0000029 [DOI] [PubMed] [Google Scholar]
- 55.Scott V, Verhees MWFT, De Raedt R, et al. Gratitude: a resilience factor for more securely attached children. J Child Fam Stud. 2020:1–15. [Google Scholar]
- 56.Dujardin A, Santens T, Braet C, et al. Middle childhood support-seeking behavior during stress: links with self-reported attachment and future depressive symptoms. Child Dev. 2016;87:326–340. doi: 10.1111/cdev.12491 [DOI] [PubMed] [Google Scholar]
- 57.Verhees MWFT, Ceulemans E, Van IJzendoorn MH, Bakermans-Kranenburg MJ, Bosmans G. State attachment variability across distressing situations in middle childhood. Soc Dev. 2020;29(1):196–216. doi: 10.1111/sode.12394 [DOI] [Google Scholar]
- 58.Bosmans G, Braet C, Heylen J, De Raedt R. Children’s attentional processing of mother and proximity seeking. PLoS One. 2015;10(4):e0124038. doi: 10.1371/journal.pone.0124038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Houbrechts M, Bosmans G, Calders F. Cumulative family stress and externalizing problems: secure base script knowledge as a protective factor. 2020. [DOI] [PubMed]
- 60.Berry K, Barrowclough C, Wearden A. Attachment theory: a framework for understanding symptoms and interpersonal relationships in psychosis. Behav Res Ther. 2008;46:1275–1282. doi: 10.1016/j.brat.2008.08.009 [DOI] [PubMed] [Google Scholar]
- 61.MacBeth A, Gumley A, Schwannauer M, Fisher R. Attachment states of mind, mentalization, and their correlates in a first-episode psychosis sample. Psychol Psychother. 2011;84(1):42–57. [DOI] [PubMed] [Google Scholar]
- 62.Cuyvers B, Vervoort E, Bosmans G. Reactive attachment disorder symptoms and prosocial behavior in middle childhood: the role of secure base script knowledge. BMC Psychiatry. 2020;20. doi: 10.1186/s12888-020-02931-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Prior V, Glaser D. Understanding attachment and attachment disorders: theory, evidence and practice. J Can Acad Child Adolesc Psychiatry. 2007;16(4):184–185. [Google Scholar]
- 64.Vervoort E, De Schipper JC, Bosmans G, Verschueren K. Screening symptoms of reactive attachment disorder: evidence for measurement invariance and convergent validity. Int J Methods Psychiatr Res. 2013;22(3):256–265. doi: 10.1002/mpr.1395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dozier M. Attachment-based treatment for vulnerable children. Attach Hum Dev. 2003;5(3):253–257. doi: 10.1080/14616730310001596151 [DOI] [PubMed] [Google Scholar]
- 66.Wright B, Edginton E. Evidence-based parenting interventions to promote secure attachment: findings from a systematic review and meta-analysis. Glob Pediatr Health. 2016;3:1–14. doi: 10.1177/2333794X16661888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Van Zeijl J, Mesman J, Van IJzendoorn MH, et al. Attachment-based intervention for enhancing sensitive discipline in mothers of 1- to 3-year-old children at risk for externalizing behavior problems: a randomized controlled trial. J Consult Clin Psychol. 2006;74:994–1005. doi: 10.1037/0022-006X.74.6.994 [DOI] [PubMed] [Google Scholar]
- 68.Van Vlierberghe L, Bosmans G. Middle childhood script attachment therapy. [DOI] [PubMed]
- 69.Diamond G, Russon J, Levy S. Attachment-based family therapy: a review of the empirical support. Fam Process. 2016;55:595–610. doi: 10.1111/famp.12241 [DOI] [PubMed] [Google Scholar]
- 70.Dozier M, Meade E, Bernard K. Attachment and biobehavioral catch-up: an intervention for parents at risk of maltreating their infants and toddlers In: Timmer S, Urquiza A, editors. Evidence-Based Approaches for the Treatment of Maltreated Children. Child Maltreatment (Contemporary Issues in Research and Policy). Vol. 3 Dordrecht: Springer; 2014. [Google Scholar]
- 71.Facompré CR, Bernard K, Waters TEA. Effectiveness of interventions in preventing disorganized attachment: a meta-analysis. Dev Psychopathol. 2018;30(1):1–11. doi: 10.1017/S0954579417000426 [DOI] [PubMed] [Google Scholar]
- 72.Hughes D. Dyadic developmental psychotherapy (DDP): an attachment‐focused family treatment for developmental trauma. Aust N Z J Fam Ther. 2017;38(4):595–605. doi: 10.1002/anzf.1273 [DOI] [Google Scholar]
- 73.Becker-Weidman A. Treatment for children with reactive attachment disorder: dyadic developmental psychotherapy. Child Adolesc Ment Health. 2008;13(1):52–60. doi: 10.1111/j.1475-3588.2006.00428.x [DOI] [PubMed] [Google Scholar]
- 74.Comyn J. Exploring Stakeholders’ Perceptions of the Impact, Acceptability and Feasibility of a Video-Feedback Intervention to Promote Positive Parenting in Foster Care (VIPP-FC) [doctoral thesis]. University College London. [Google Scholar]
- 75.Emerick LJ. Academic underachievement among the gifted: students’ perceptions of factors that reverse the pattern. Gifted Child Q. 1992;36:140–146. doi: 10.1177/001698629203600304 [DOI] [Google Scholar]
- 76.Pearcy MT, Clopton JR, Pope AW. Influences on teacher referral of children to mental health services: gender, severity, and internalizing versus externalizing problems. J Emot Behav Disord. 1993;1:165–169. doi: 10.1177/106342669300100304 [DOI] [Google Scholar]
- 77.Hamre BK, Pianta RC. Early teacher–child relationships and the trajectory of children’s school outcomes through eighth grade. Child Dev. 2001;72(2):625–638. doi: 10.1111/1467-8624.00301 [DOI] [PubMed] [Google Scholar]
- 78.McIntosh DE, Rizza MG, Bliss L. Implementing empirically supported interventions: teacher‐child interaction therapy. Psychol Sch. 2000;37(5):453–462. doi: [DOI] [Google Scholar]
- 79.Vancraeyveldt C, Verschueren K, Wouters S, Van Craeyevelt S, Van Den Noortgate W, Colpin H. Improving teacher-child relationship quality and teacher-rated behavioral adjustment amongst externalizing preschoolers: effects of a two-component intervention. J Abnorm Child Psychol. 2015;43(2):243–257. [DOI] [PubMed] [Google Scholar]
- 80.Driscoll KC, Pianta RC. Banking time in head start: early efficacy of an intervention designed to promote supportive teacher-child relationships. Early Educ Dev. 2010;21:38–64. doi: 10.1080/10409280802657449 [DOI] [Google Scholar]